Abstract
Exenteration of the orbital contents as well as removal of a part of maxilla with an ablative surgery for the removal of a malignant tumor can severely affect a person in terms of function, esthetics and psychological trauma. A well-retained, user-friendly, removable maxillofacial prosthesis is the key to successful prosthetic rehabilitation in such cases. Various retentive techniques include using spectacle frame, conformers, adhesives, osseointegrated implants, magnets or buttons. This paper describes a novel technique for retention of silicone orbital prosthesis using acrylic resin base attached to maxillary obturator with the help of pin and socket of an electric plug wherein the latter is attached to the eye prosthesis with the help of a mechanical undercut. This helps in better retention of both the prostheses.
Keywords: Orbital prosthesis, Silicone eye prosthesis
Introduction
Acquired mid facial defects often present with severe disfigurement and functional impairment. Large defects that result from cancer treatment rarely are rehabilitated by surgical reconstruction alone; they usually require a facial prosthesis to restore function and appearance. In addition, an intraoral prosthesis such as an obturator is often needed to restore speech and swallowing [1]. Providing comfort and protection to the remaining soft and hard tissues should be the paramount feature of rehabilitation. Technique used for retaining maxillofacial prostheses plays an important role in the success of treatment. This allows the patient to be accepted in society without being a victim of unwanted sympathy [2]. Various methods of auxiliary retention for facial prostheses have been described in the literature; they include eye patches [3], prosthesis fastened to spectacle frame [4] extensions from the denture [5], magnets [6], adhesives [7–9], and osseointegrated implants [10, 11].
Use of spectacle frame is an easy and economical treatment option but the method is not user friendly as the frame becomes heavy and patient has to wear the spectacle unconditionally. Modern prosthetic replacements are secured with adhesives that are readily available, easily applied, and provide satisfactory retention, but for a limited period of time. However, continual use of adhesives may cause allergic response or irritation [9]. With few or missing undercuts, mimic motion and sneezing can cause adhesive failure. Thus, the orbital prosthesis may be attached to the obturator with magnets or buttons [12]. Besides being an expensive option, there may be loss of magnetism with time or, corrosion of magnets may occur. Osseointegrated implants are well documented for retaining the orbital prosthesis [8, 9]. Although osseointegrated implants may provide the most reliable prosthesis retention, additional surgeries, expenses, inadequate bone, and prior radiation to the area may contraindicate this type of treatment [13]. So, it is not a treatment option for all. Use of anatomic retention can help to retain an orbital prosthesis by using a flexible conformer in the defect space. The orbital prosthesis is constructed in the usual manner with an extension into the conformer engaging the circumferential groove undercut to provide mechanical retention [9]. However, there should be an adequate anatomic undercut to use this technique. This case report describes a procedure in which a pin of electrical plug was attached to the orbital prosthesis, which was fitted into the socket attached to the bulb of obturator. This helps in better retention of both the intraoral and extraoral prostheses and, silicone eye prosthesis also fulfils the esthetic requirements of the patient.
Case Report
A 55-year-old male patient had reported to the Department of Prosthodontics, AIIMS, with a chief complaint of missing right eye since 3 months and regurgitation of food from the defect site. Patient gave the history of diabetes and histopathological diagnosis revealed Rhinocerebral mucormycosis. Surgical exenteration of the right eye and right side hemimaxillectomy was done to treat Rhinocerebral mucormycosis, and was followed by protocol of maintenance chemotherapy. Extraoral examination of the patient showed a large orbital defect on right side which was continuous with intraoral maxillary defect (Fig. 1). Extra orally, tissue was healthy but no definite bony or soft tissue undercut was found to help in the retention of the prosthesis. For complete prosthetic rehabilitation of the patient, a hollow closed bulb obturator and a silicone orbital prosthesis were planned. As the intraoral and extraoral defects were continuous, so to retain the orbital prosthesis, it was plugged with the help of pin of electric plug into the socket attached to the bulb of maxillary obturator (like a patrix and matrix).
Fig. 1.
Orbital defect continuous with intraoral maxillary defect
Method
Recording the Impressions
The patient was draped for impression procedures and patient’s eyebrows and eyelashes were lubricated with petroleum jelly in order to facilitate removal of the impression material and minimize discomfort to the patient. Lines were marked on the patient’s face with an indelible pencil for symmetrical placement of the orbital prosthesis. Impressions of the orbital defect and the maxillary defect were made using irreversible hydrocolloid (Zelgan, Dentsply India Ltd.) and individual casts were poured in dental stone for better surface details and strength.
Fabrication of Conformer and Attachment of Pin and Socket
A conformer of orbital defect was made with the autopolymerising resin (DPI cold cure, Dental Product of India, Mumbai, India) and was tried on patients face. A 5 mm thick sprue wax was attached to the acrylic base to provide a mechanical undercut for the retention of silicone eye prosthesis. An obturator plate was also made in cold cure acrylic resin and adjusted in patient’s mouth. A pin of electric plug was attached on the rear side of the conformer and a corresponding socket pin was attached to the bulb of the maxillary obturator plate. Both parts were snuggly fitted into each other like a matrix and patrix part of a semi precision attachment and adjusted to attain a path of insertion and removal without interference, so that the orbital prosthesis could be retained with the obturator in the absence of anatomic undercuts. The pin and socket were stabilized with sticky wax to the acrylic conformer and obturator plate, respectively. Conformer and obturator plate were flasked and dewaxed and packing was done in heat cure acrylic resin (high impact heat cure acrylic, Travelon) (Fig. 2). Pigments were added to the resin used for packing of orbital defect to match the patient’s skin color. The heat cure bases were checked on the patient for the adaptation and retentive potential (Fig. 3).
Fig. 2.
Flasking of acrylic base
Fig. 3.
Try-in of acrylic base on patients face
Fabrication of Silicone Orbital Prosthesis
The right eye prosthesis was carved in modeling wax using a prefabricated eye shell button selected according to the color of the left eye. It was tried on the patient’s face to check the orientation of pupil, color, size and volume of sclera visible as compared to the contra lateral eye. Once the trial was found satisfactory, flasking, dewaxing and packing were done as per Prosthodontic protocols and processed in RTV (room temperature vulcanizing) silicone material. Silicone-specific colors were used to match the color of the patient’s skin. Try-in of definitive obturator was done. It was flasked in a conventional manner and was delivered to the patient after finishing and polishing (Fig. 4a, b). Eye prosthesis was retrieved, characterized and was delivered to the patient (Figs. 5, 6). Patient could wear the prosthesis with or without spectacle (Figs. 7, 8).
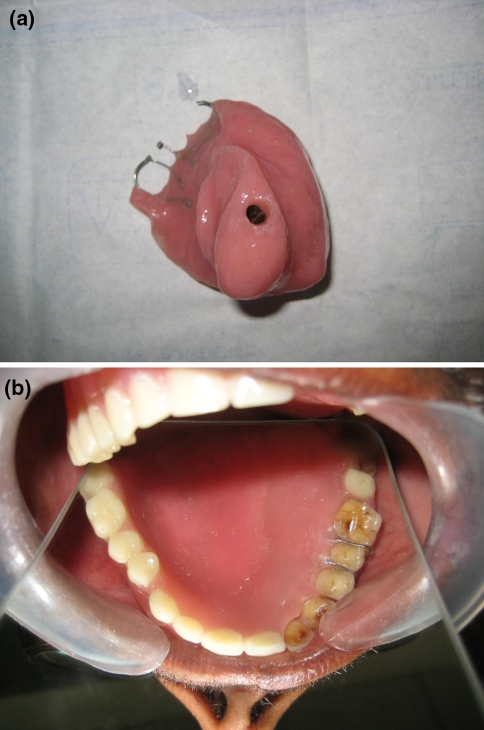
Fig. 4.
a Definitive obturator with socket pin. b Intraoral view of definitive obturator
Fig. 5.
a Orbital prosthesis with socket pin. b Acrylic conformer and silicone prosthesis
Fig. 6.
Final eye prosthesis
Fig. 7.
Final prosthesis on patients face with spectacle
Fig. 8.
Final prosthesis on patients face without spectacle
Discussion
Total orbital exenteration is a radical surgical procedure which typically involves the removal of the entire contents of the orbit, including periorbita. Consequently, it results in a deep orbital deformity with devastating cosmetic and functional implications that require expensive and technically challenging oculoplastic intervention, not to mention associated psychological effects. Orbital prosthesis presents an attractive and viable alternative when esthetic and functional demands are beyond the capacity of local reconstructive efforts [14].
Selection of a reasonable maxillofacial prosthetic material and economically feasible retentive aid should be the goal of rehabilitating such patients. Ablative surgical procedure incurs major financial burden, and hence the patient may seek a prosthetic treatment that is economical. Therefore, selection of a reasonable maxillofacial prosthetic material and economically feasible retentive aid should be the goal of rehabilitating such patients. Since silicone has better marginal adaptation and life-like appearance, it has been used for the fabrication of orbital prostheses [15]. A limitation of silicone orbital prostheses is its lack of chemical/mechanical bonding with the eyeglass frame, making it difficult to retain the prosthesis [16].
In this case report, a novel idea of retention with the help of very economical household electrical plug was used, which helped in the better retention of both the obturator and the orbital prosthesis. If it would have been only an orbital defect, the other methods of retention like spectacle retained, use of adhesive or osseointegrated implants, could be considered. But in this case, as the defect was continuous, the attachment of both the prostheses was possible with the help of magnets or electric pin and socket method.
Advantages of using this particular method include adequate retention, economical, comfortable, and noninvasive unlike implants. Because of this non rigid attachment, slight movement produced in the eye prosthesis with the movement of obturator gave a slight life like appearance to the orbital prosthesis. The silicone eye prosthesis provided all the advantages of being light weight, better esthetics than acrylic prosthesis and a life like appearance. But, use of adhesive was not required as the prosthesis was attached to the conformer with a self made undercut. So, the chances of allergic reaction caused due to the use of adhesives or silicone was also overcome, as in this case, more of tissue contact was with acrylic. Use of spectacle was also optional for the patient as it was not used as the method of retention.
Summary
Exenteration of the orbital contents as well as removal of a part of maxilla with an ablative surgery for the removal of a malignant tumor can severely affect a person in terms of function, esthetics and psychological trauma. A well-retained, user-friendly, removable maxillofacial prosthesis is the key to successful prosthetic rehabilitation in such cases. A simple procedure of fabricating a pin and socket retained silicone orbital prosthesis has been presented above. The method used acrylic resin base for attaching the silicone prosthesis to the maxillary obturator with the help of pin and socket of electric plug which is easily available. The advantages of this method are its better retention, restoration of function, cost-effectiveness, tissue tolerance, esthetics, and comfort for use and wear.
Contributor Information
Gunjan Pruthi, Email: gunjan_prostho@yahoo.co.in.
Swati Sikka, Phone: +919971625576, Email: tellswati@yahoo.com.
References
- 1.Brignoni R, Dominici JT. An intraoral–extraoral combination prosthesis using an intermediate framework and magnets: a clinical report. J Prosthet Dent. 2001;85:7–11. doi: 10.1067/mpr.2001.113030. [DOI] [PubMed] [Google Scholar]
- 2.Dhiman R, Arora V, Kotwal N. Rehabilitation of a Rhinocerebral mucormycosis patient. J Indian Prosthodont Soc. 2007;7:88–91. doi: 10.4103/0972-4052.34003. [DOI] [Google Scholar]
- 3.Tautin FS, Schoemann D. Retaining a large facial prosthesis. J Prosthet Dent. 1975;34:342–345. doi: 10.1016/0022-3913(75)90115-8. [DOI] [PubMed] [Google Scholar]
- 4.McClelland RC. Facial prosthesis following radical maxillofacial surgery. J Prosthet Dent. 1977;38:327–330. doi: 10.1016/0022-3913(77)90310-9. [DOI] [PubMed] [Google Scholar]
- 5.Fattore L, Edmonds DC. A technique for the obturation of anterior maxillary defects with accompanying midfacial tissue loss. J Prosthet Dent. 1987;58:203–205. doi: 10.1016/0022-3913(87)90177-6. [DOI] [PubMed] [Google Scholar]
- 6.Dumbrigue HB, Fyler A. Minimizing prosthesis movement in a midfacial defect: a clinical report. J Prosthet Dent. 1997;78:341–345. doi: 10.1016/S0022-3913(97)70040-4. [DOI] [PubMed] [Google Scholar]
- 7.Amnuay SK, Khan Z, Goldsmith LJ. Effect of adhesive retention on maxillofacial prostheses. Part I: skin dressings and solvent removers. J Prosthet Dent. 2000;84:335–340. doi: 10.1067/mpr.2000.109507. [DOI] [PubMed] [Google Scholar]
- 8.Wolfaardt JF, Tam V, Faulkner MG, Prasad N. Mechanical behavior of three maxillofacial prosthetic adhesive systems: a pilot project. J Prosthet Dent. 1992;68:943–949. doi: 10.1016/0022-3913(92)90556-P. [DOI] [PubMed] [Google Scholar]
- 9.Parel SM. Diminishing dependence on adhesives for retention of facial prosthesis. J Prosthet Dent. 1980;43:552–560. doi: 10.1016/0022-3913(80)90330-3. [DOI] [PubMed] [Google Scholar]
- 10.Chang TL, Garrett N, Roumanas E, Beumer J., III Treatment satisfaction with facial prosthesis. J Prosthet Dent. 2005;94:275–280. doi: 10.1016/j.prosdent.2005.06.002. [DOI] [PubMed] [Google Scholar]
- 11.Nishimura RD, Roumanas E, Moy PK, Sugai T. Nasal defects and osseointegrated implants: UCLA Experience. J Prosthet Dent. 1996;76:597–602. doi: 10.1016/S0022-3913(96)90436-9. [DOI] [PubMed] [Google Scholar]
- 12.Lemon JC, Chambers MS. Locking retentive attachment for an implant-retained auricular prosthesis. J Prosthet Dent. 2002;87:336–338. doi: 10.1067/mpr.2002.122016. [DOI] [PubMed] [Google Scholar]
- 13.Arcuri M, LaVelle WE, Fyler E, Jons R. Prosthetic complications of extraoral implants. J Prosthet Dent. 1993;69:289–292. doi: 10.1016/0022-3913(93)90108-Z. [DOI] [PubMed] [Google Scholar]
- 14.Konstantinidis L, Scolozzi P, Hamedani M. Rehabilitation of orbital cavity after total orbital exenteration using oculofacial prostheses anchored by osseointegrated dental implants posed as a one step surgical procedure. Klin Monbl Augenheilkd. 2006;223:400–404. doi: 10.1055/s-2006-926565. [DOI] [PubMed] [Google Scholar]
- 15.Rodrigues S, Shenoy VK, Shenoy K. Prosthetic rehabilitation of a patient after partial rhinectomy: a clinical report. J Prosthet Dent. 2005;93:125–128. doi: 10.1016/j.prosdent.2004.10.021. [DOI] [PubMed] [Google Scholar]
- 16.Guttal SS, Patil NP, Nadiger RK, et al. Use of acrylic resin base as an aid in retaining silicone orbital prosthesis. J Indian Prosthodont Soc. 2008;8:112–115. doi: 10.4103/0972-4052.43615. [DOI] [Google Scholar]