Recent studies have reported that low serum vitamin D levels are associated with a variety of diseases, including cardiovascular disease and in particular ischemic heart disease (IHD). Possible mechanisms underlying this association include increased inflammation, renin-angiotensin system upregulation, insulin resistance, altered lipid metabolism, and altered vascular smooth muscle growth and function that lead to hypertension, diabetes, dyslipidemia and atherosclerosis.[1][2]
However, few longitudinal studies have explored the association between vitamin D levels and incident IHD. A nested case-control study of male health care professionals found an approximately doubled risk of incident myocardial infarction associated with lower vitamin D levels.[3] Other studies have identified trends between vitamin D levels and incident myocardial infarction but no statistically significant associations, [4][5][6] at least in part due to small sample sizes or short follow-up.
The association between vitamin D levels and recurrent IHD has been studied even less frequently. A cohort study among patients referred for coronary angiography for suspected coronary artery disease found a statistically significant association between low vitamin D levels and risk of cardiovascular mortality.[7] A cohort study among patients with a history of IHD found no significant association between vitamin D levels and risk of secondary cardiovascular disease including IHD, ischemic stroke, or other cardiovascular disease.[8] No study has specifically tested the population-based relation between vitamin D levels and ischemic heart disease among patients with prior cardiovascular disease. In the current study, we hypothesized that an inverse association exists between vitamin D level and risk of IHD would be detected in patients with established cardiovascular disease.
We studied a randomly selected, population-based sample of participants in the Canadian Nova Scotia Health Survey 1995 (NSHS95) who underwent plasma vitamin D quantification, consented for linkage of their NSHS95 data and subsequent hospitalization or death data, and had a prior history of cardiovascular disease – IHD, peripheral vascular disease, or stroke. To identify these conditions, the following International Classification of Disease (ICD) codes were included: ICD-9 codes V12.5, V45.81, V49.7x, 250.70, 410-414.xx, 415.05, 430-432, 433-435.xx, 440.xx, 441-442.xx, 443.21, 444.xx, 447.xx, 459.9, 593.81, 707.xx, 785.4; or ICD-10 codes E11.5, E10.5, E13.5, E14.5, G45.xx, L98.4, L97, N28.0, R02, T82.3, Z86.7, Z89.x, Z95.x, 120-125.xx, 160-166.xx, 167.0, 170-174.x, 177.x, 179.2, 199. The design of and data collection for NSHS95 has been described elsewhere. [9]
25-hydroxyvitamin D (25(OH)D)quantification of serum is the established method of determining a patient’s vitamin D status.[10] and was measured with the Diasorin radioimmunoassay method (Stillwater, MN). [11]
Data for IHD events during the 10-year period beginning with a subject’s baseline NSHS95 interview date were provided by the provincial health care registry (hospitalization data) and Statistics Canada (mortality data, including deaths outside of a hospital). Time to event is days from NSHS enrollment to IHD event.
Cox regression analyses were performed to evaluate the association between vitamin D level and IHD events. Covariates in the analyses included season during which plasma was collected (for vitamin D quantification), age, and cigarette smoking. The analyses were sex-stratified. Diabetes, hypertension, obesity, and cholesterol were not included as covariates because they are hypothesized to be in the causal pathway.
In the NSHS95 database of 1844 patients, 244 subjects met our selection criteria.
25(OH)D level was not transformed given its normal distribution as ascertained during exploratory analysis. 25(OH)D level was divided into three categories for analysis: <15 ng/mL, 15 to <30 ng/mL, and ≥30 ng/mL. The 30 ng/mL cutoff distinguishes between vitamin D sufficiency and insufficiency or deficiency.[12][13] A 25(OH)D level above this cutoff is considered optimal for several health outcomes.[14][15] 25(OH)D levels below this cutoff are associated with elevated parathyroid hormone(PTH) levels, [16] indicating vitamin D insufficiency. Although several different cutoffs have been used to distinguish vitamin D insufficiency and deficiency, 15 ng/mL has been used in multiple studies.[17][3][18]
13 subjects (5.3%) had vitamin D levels of <15 ng/mL, 140 (57.4%) had levels of 15 to <30 ng/mL, and 91 (37.3%) had levels of ≥30 ng/mL. The subjects’ characteristics are detailed in Table 1.
Table 1.
Baseline Characteristics of the Patients According to Vitamin D Level
| Characteristic | Vitamin D Level |
|||
|---|---|---|---|---|
| <15 ng/mL | 15 to <30 ng/mL | >=30 ng/mL | p-value | |
| Age | 72.1 ± 11.0 | 65.6 ± 14.5 | 66.2 ± 15.4 | 0.315 |
| % Female | 53.8% | 47.9% | 37.4% | 0.228 |
| % Smokers | 23.1% | 27.9% | 26.4% | 0.919 |
| % Diabetic | 23.1% | 10.0% | 13.2% | 0.340 |
| Systolic Blood Pressure (mmHg) | 137.1 ± 17.0 | 134.5 ± 18.0 | 138.3 ± 20.8 | 0.331 |
| Body Mass Index (kg/m2) | 26.5 ± 6.3 | 28.1 ± 6.0 | 27.4 ± 5.6 | 0.520 |
| Cholesterol (total:HDL) | 4.7 ± 1.6 | 5.1 ± 1.5 | 5.1 ± 1.4 | 0.514 |
| % Previous IHD | 69.2% | 55.7% | 62.6% | 0.434 |
| % Previous stroke | 15.4% | 17.1% | 15.4% | 0.936 |
| % Previous PVD | 41.7% | 45.7% | 34.1% | 0.215 |
| Season (quarter of plasma collection) | 0.492 | |||
| January 1 – March 31 | 23.1% | 11.4% | 6.6% | 0.146 |
| April 1 – June 30 | 53.8% | 53.6% | 50.6% | 0.900 |
| July 1 – September 30 | 7.7% | 16.4% | 33.0% | *0.005 |
| October 1 – December 31 | 15.4% | 18.6% | 9.9% | 0.201 |
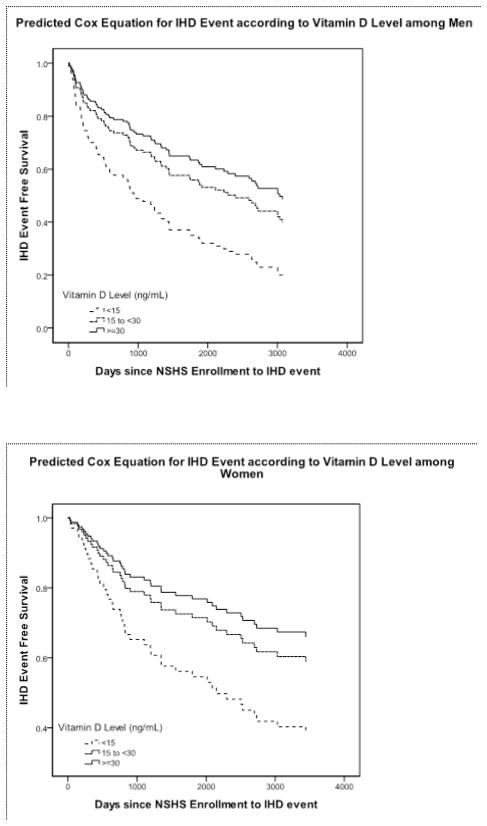
114 IHD events occurred during the 10-year follow-up. The figure below show the predicted Cox regression equations for IHD events according to vitamin D level. In men and women combined, levels of <30 ng/mL were associated with a hazard ratio of 1.33 (p=.172) for IHD events compared to levels ≥30 ng/mL. Levels of <15 ng/mL were associated with a hazard ratio of 2.30 (p=.035) for IHD events compared to levels ≥30 ng/mL (see Figures 1a and 1b).
Fig. 1.
Our study’s objective was to expand on the thus far limited literature exploring the association between vitamin D levels and incident or recurrent IHD. We have shown that among patients with prior cardiovascular disease (including IHD, peripheral vascular disease, or stroke), marked vitamin D deficiency is associated with an increased risk of IHD events.
Growing evidence indicates that low vitamin D levels may underlie established cardiovascular risk factors, perhaps making it in and of itself a cardiovascular risk factor. Early hypotheses relating vitamin D and IHD stemmed from ecological studies showing increased IHD incidence or mortality at increased latitude,[19][20] during winter months [21][22][23], and lower altitude [24] – presumably due to decreased sun exposure and thus lower vitamin D levels. Indeed, two case-control studies found lower vitamin D levels among myocardial infarction patients versus controls, with the greatest differences existing according to season. [25][26]
Specific mechanisms underlying the vitamin D--IHD association have since been explored. The pathophysiology initially became evident in studies of end-stage renal disease patients.[27][28] This population’s high IHD burden has been attributed to decreased production of the active metabolite 1,25-dihydroxyvitamin D (calcitriol) as well as consequent secondary hyperparathyroidism, both of which lead to atherosclerosis via altered lipoprotein metabolism and altered vascular smooth muscle growth and function.[1] Low vitamin D levels may also lead to increased vessel calcification via increased PTH,[1] which would help explain associations even in non-renal failure populations between low vitamin D levels and more extensive vascular calcification[29] including incident coronary artery calcification.[30]
Additional mechanisms have been elucidated. Inflammation and hypertension are both risk factors for IHD. Low vitamin D levels lead to increased inflammation via increased TNF-α and IL-6[31] and decreased IL-10.[32] Low vitamin D levels result in upregulation of the renin-angiotensin system, increasing blood pressure.[2] In fact, low vitamin D levels are associated with hypertension[33][34][35][18] and vitamin D supplementation has been shown to decrease systolic blood pressure.[36] Low vitamin D levels are also associated with other IHD risk factors, including diabetes, obesity, and dyslipidemia.[33][34][18] Mechanisms underlying these associations include increased insulin resistance and altered lipid metabolism leading to decreased high-density lipids and increased very low-density lipids.[1]
It is important to understand how the association found in our study could influence clinical practice. Once the association is confirmed in larger, more diverse populations, the effect of vitamin D supplementation on IHD in cardiovascular disease patients should be explored. A recent meta-analysis of randomized controlled trials involving various patient populations found that vitamin D supplementation caused decreased total mortality.[37] In cohort studies, dialysis patients receiving vitamin D supplementation have had decreased mortality from cardiovascular disease, including IHD;[38][39] the caveat being that dialysis patients receive a different vitamin D formulation compared to that typically given to the non-renal failure population. Therefore, the potential for vitamin D to provide health benefits, and specifically to reduce the incidence of IHD events in cardiovascular disease patients, may exist.
Limitations of this study include its observational design and its geographically limited population. Not all NSHS survey participants underwent vitamin D quantification or consented for linkage of their survey and subsequent hospitalization or death data, introducing further selection bias. Also, this analysis relies on medical records in which ICD-9/10 coding may not always be accurate; however, obtaining data from a universal healthcare system for the general population is more representative and complete than other methods. It is also conceivable that vitamin D status simply reflects outdoor physical activity, making it a surrogate marker for exercise rather than an independent risk factor for IHD.
The authors of this manuscript have certified that they comply with the Principles of Ethical Publishing in the International Journal of Cardiology.[40]
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Lauren Taggart Wasson, New York Presbyterian Hospital-Columbia University Medical Center, 177 Fort Washington Avenue, 6th Floor, Center Room 12, New York, NY 10024.
Daichi Shimbo, Center for Behavioral Cardiovascular Health, Division of General Medicine, Department of Medicine (Columbia University Medical Center).
Mishaela R. Rubin, Metabolic Bone Disease Unit, Department of Medicine (Columbia University College of Physicians & Surgeons).
Jonathan A. Shaffer, Center for Behavioral Cardiovascular Health (Columbia University Medical Center).
Joseph E. Schwartz, Center for Behavioral and Cardiovascular Health (Columbia University Medical Center); Department of Psychiatry and Behavioral Sciences (Stony Brook University).
Karina W. Davidson, Center for Behavioral Cardiovascular Health (Columbia University Medical Center).
References
- 1.Rostand SG, Drueke TB. Parathyroid hormone, vitamin D, and cardiovascular disease in chronic renal failure. Kidney Int. 1999;56(2):383–392. doi: 10.1046/j.1523-1755.1999.00575.x. [DOI] [PubMed] [Google Scholar]
- 2.Zittermann A, Schleithoff SS, et al. Putting cardiovascular disease and vitamin D insufficiency into perspective. British Journal of Nutrition. 2005;94(04):483–492. doi: 10.1079/bjn20051544. [DOI] [PubMed] [Google Scholar]
- 3.Giovannucci E, Liu Y, et al. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Archives of Internal Medicine. 2008;168(11):1174–80. doi: 10.1001/archinte.168.11.1174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Vik T, Try K, et al. Tromso Heart Study: vitamin D metabolism and myocardial infarction. British Medical Journal. 1979;2:176. doi: 10.1136/bmj.2.6183.176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marniemi J, Alanen E, et al. Dietary and serum vitamins and minerals as predictors of myocardial infarction and stroke in elderly subjects. Nutrition, Metabolism and Cardiovascular Diseases. 2005;15(3):188–197. doi: 10.1016/j.numecd.2005.01.001. [DOI] [PubMed] [Google Scholar]
- 6.Bolland MJ, Bacon CJ, et al. Vitamin D insufficiency and health outcomes over 5 years in older women. American Journal of Clinical Nutrition. 2010;91(1):82–89. doi: 10.3945/ajcn.2009.28424. [DOI] [PubMed] [Google Scholar]
- 7.Dobnig H, Pilz S, et al. Independent association of low serum 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D levels with all-cause and cardiovascular mortality. Archives of Internal Medicine. 2008;168(12):1340–1349. doi: 10.1001/archinte.168.12.1340. [DOI] [PubMed] [Google Scholar]
- 8.Grandi NC, Breitling LP, et al. Serum vitamin D and risk of secondary cardiovascular disease events in patients with stable coronary heart disease. American Heart Journal. 1010;159(6):1044–1051. doi: 10.1016/j.ahj.2010.03.031. [DOI] [PubMed] [Google Scholar]
- 9.MacLean D, Scott J, et al. D o Health. Halifax; Nova Scotia: 1996. The 1995 Nova Scotia Health Survey. [Google Scholar]
- 10.Holick MF. Vitamin D Status: Measurement, Interpretation, and Clinical Application. Annals of Epidemiology. 2009;19(2):73–78. doi: 10.1016/j.annepidem.2007.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Roth HJ, Schmidt-Gayk H, et al. Accuracy and clinical implications of seven 25-hydroxyvitamin D methods compared with liquid chromatography-tandem mass spectrometry as a reference. Ann Clin Biochem. 2008;45(2):153–159. doi: 10.1258/acb.2007.007091. [DOI] [PubMed] [Google Scholar]
- 12.Holick MF. Vitamin D deficiency. N Engl J Med. 2007;357(3):266–281. doi: 10.1056/NEJMra070553. [DOI] [PubMed] [Google Scholar]
- 13.Lee JH, O’Keefe JH, et al. Vitamin D deficiency: an important, common, and easily treatable cardiovascular risk factor? Journal of the American College of Cardiology. 2008;52(24):1949–1956. doi: 10.1016/j.jacc.2008.08.050. [DOI] [PubMed] [Google Scholar]
- 14.Bischoff-Ferrari HA, Giovannucci E, et al. Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. American Journal of Clinical Nutrition. 2006;84(1):18–28. doi: 10.1093/ajcn/84.1.18. [DOI] [PubMed] [Google Scholar]
- 15.Dawson-Hughes B, Heaney RP, et al. Estimates of optimal vitamin D status. Osteoporos Int. 2005;6:713–716. doi: 10.1007/s00198-005-1867-7. [DOI] [PubMed] [Google Scholar]
- 16.Chapuy MC, Preziosi P, et al. Prevalence of vitamin D insufficiency in an adult normal population. Osteoporosis International. 1997;7(5):439–443. doi: 10.1007/s001980050030. [DOI] [PubMed] [Google Scholar]
- 17.Wang TJ, Pencina MJ, et al. Vitamin D deficiency and risk of cardiovascular disease. Circulation. 2008;117(4):503–511. doi: 10.1161/CIRCULATIONAHA.107.706127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Anderson JL, May HT, et al. Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. American Journal of Cardiology. 2010;106(7):963–968. doi: 10.1016/j.amjcard.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 19.Elford J, Phillips AN, et al. Migration and geographic variations in ischemic heart disease in Great Britain. Lancet. 1989;333:343–6. doi: 10.1016/s0140-6736(89)91722-4. [DOI] [PubMed] [Google Scholar]
- 20.Fleck A. Latitude and ischemic heart disease. The Lancet. 1989;333(8638):613–613. doi: 10.1016/s0140-6736(89)91634-6. [DOI] [PubMed] [Google Scholar]
- 21.Dunnigan MG, Harland WA, et al. Seaonal incidence and mortality of ischaemic heart-disease. The Lancet. 1970;296(7677):793–797. doi: 10.1016/s0140-6736(70)91460-1. [DOI] [PubMed] [Google Scholar]
- 22.Douglas AS, Allan TM, et al. Composition of seasonality of disease. Scott Med J. 1991;36:76–82. doi: 10.1177/003693309103600304. [DOI] [PubMed] [Google Scholar]
- 23.Douglas AS, Dunnigan MG, et al. Seasonal variation in coronary heart disease in Scotland. Journal of Epidemiology and Community Health. 1995;49(6):575–582. doi: 10.1136/jech.49.6.575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Voors AW, Johnson WD. Altitude and arteriosclerotic heart disease mortality in white residents of 99 of the 100 largest cities in the united states. Journal of Chronic Diseases. 1979;32(1–2):157–162. doi: 10.1016/0021-9681(79)90044-4. [DOI] [PubMed] [Google Scholar]
- 25.Lund B, Badskjaer J, et al. Vitamin D and ischaemic heart disease. Hormone & Metabolic Research. 1978;10(6):553–6. doi: 10.1055/s-0028-1093390. [DOI] [PubMed] [Google Scholar]
- 26.Scragg R, Sowers M, et al. Serum 25-hydroxyvitamin D, Ethnicity, and Blood Pressure in the Third National Health and Nutrition Examination Survey. Am J Hypertens. 2007;20(7):713–719. doi: 10.1016/j.amjhyper.2007.01.017. [DOI] [PubMed] [Google Scholar]
- 27.Zittermann A. Vitamin D and disease prevention with special reference to cardiovascular disease. Progress in Biophysics & Molecular Biology. 2006;92(1):39–48. doi: 10.1016/j.pbiomolbio.2006.02.001. [DOI] [PubMed] [Google Scholar]
- 28.Nemerovski CW, Dorsch MP, et al. Vitamin D and cardiovascular disease. Pharmacotherapy. 2009;29(6):691–708. doi: 10.1592/phco.29.6.691. [DOI] [PubMed] [Google Scholar]
- 29.Watson KE, Abrolat ML, et al. Active serum vitamin D levels are inversely correlated with coronary calcification. Circulation. 1997;96(6):1755–60. doi: 10.1161/01.cir.96.6.1755. [DOI] [PubMed] [Google Scholar]
- 30.de Boer IH, Kestenbaum B, et al. 25-hydroxyvitamin D levels inversely associate with risk for developing coronary artery calcification. Journal of the American Society of Nephrology. 2009;20(8):1805–12. doi: 10.1681/ASN.2008111157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Muller K, Haahr PM, et al. 1,25-Dihydroxyvitamin D3 inhibits cytokine production by human blood monocytes at the post-transcriptional level. Cytokine. 1992;4:506–12. doi: 10.1016/1043-4666(92)90012-g. [DOI] [PubMed] [Google Scholar]
- 32.Canning M, Grotenhuis K, et al. 1-alpha,25-Dihydroxyvitamin D3 (1,25(OH)(2)D(3)) hampers the maturation of fully active immature dendritic cells from monocytes. Eur J Endocrinol. 2001;145(3):351–357. doi: 10.1530/eje.0.1450351. [DOI] [PubMed] [Google Scholar]
- 33.Scragg R, Sowers M, et al. Serum 25-hydroxyvitamin D, diabetes, and ethnicity in the third National Health and Nutrition Examination Survey. Diabetes Care. 2004;27(12):2813–2818. doi: 10.2337/diacare.27.12.2813. [DOI] [PubMed] [Google Scholar]
- 34.Martins D, Wolf M, et al. Prevalence of cardiovascular risk factors and the serum levels of 25-hydroxyvitamin D in the United States: data From the third National Health and Nutrition Examination Survey. Archives of Internal Medicine. 2007;167(11):1159–1165. doi: 10.1001/archinte.167.11.1159. [DOI] [PubMed] [Google Scholar]
- 35.Scragg R, Jackson R, et al. Myocardial infarction is inversely associated with plasma 25-hydroxyvitamin D3 levels: a community-based study. International Journal of Epidemiology. 1990;19(3):559–63. doi: 10.1093/ije/19.3.559. [DOI] [PubMed] [Google Scholar]
- 36.Pfeifer M, Begerow B, et al. Effects of a short-term vitamin D3 and calcium supplementation on blood pressure and parathyroid hormone levels in elderly women. J Clin Endocrinol Metab. 2001;86(4):1633–1637. doi: 10.1210/jcem.86.4.7393. [DOI] [PubMed] [Google Scholar]
- 37.Autier P, Gandini S. Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med. 2007;167(16):1730–1737. doi: 10.1001/archinte.167.16.1730. [DOI] [PubMed] [Google Scholar]
- 38.Shoji T, Shinohara K, et al. Lower risk for cardiovascular mortality in oral 1{alpha}-hydroxy vitamin D3 users in a haemodialysis population. Nephrol Dial Transplant. 2004;19(1):179–184. doi: 10.1093/ndt/gfg513. [DOI] [PubMed] [Google Scholar]
- 39.Teng M, Wolf M, et al. Activated injectable vitamin D and hemodialysis survival: a historical cohort study. Journal of the American Society of Nephrology. 2005;16(4):1115–1125. doi: 10.1681/ASN.2004070573. [DOI] [PubMed] [Google Scholar]
- 40.Shewan LG, Coats AJ. Ethics in the authorship and publishing of scientific articles. Int J Cardiol. 2010;144:1–2. [Google Scholar]