Abstract
A 28-year-old, hypertensive and hypercholesterolaemic patient, was referred to our emergency unit with a mild thoracic pain, productive cough and a body temperature of 37.3°C. Laboratory examinations showed normal white cell count and moderate elevation of C reactive protein (CRP). Later, the thoracic pain increased accompanied by shortness of breath. High D-dimer was detected. Positive lupic anticoagulant factor and anticardiolipin and antibodies anti-Mycoplasma pneumoniae were present and high titres of antinuclear factor. Recombinant tissue-type plasminogen activator plus heparin and vancomycin were administered due the high possibility of mycoplasma pneumonia associated with pulmonary thromboembolism. CRP increased to very high levels with very mild modification of white blood cells during the evolution. Thoracic tomography and pulmonary scintigraphy of the lungs confirmed the diagnosis. The patient responded well and he was discharged after 25 days medicated with hydroxychloroquine sulphate, warfarin and aspirin. At present date he is well (150 days).
Background
We deem this case interesting because of disease evolution where we had a connection between infection, thromboembolism and antiphospholipid syndrome. The event occurred during the hospitalisation and therefore was subjected to a close follow-up during his complete recovery.
Case presentation
A 28-year-old-man, previously diagnosed as hypertensive and hypercholesterolaemic, was referred to an emergency unit in a Hospital in São Paulo, Brazil, with a mild right thoracic pain, productive cough and a body temperature of 37.3°C. The medical team suspected an infectious disease as further suggested by moderately elevated C reactive protein (CRP, 47mg/l). After a few hours, thoracic pain increased and after being transferred to the intensive care unit, the patient started to have shortness of breath.
Investigations
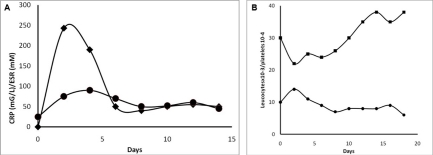
Clinical laboratory tests showed the presence of antibodies against Mycoplasma pneumoniae, positive lupic anticoagulant factor and anticardiolipin antibodies (IgG and IgM), antinuclear factor –1/1320 and a titre of D-dimer of 1450 ng/ml (ref), considered high. CRP increased to a very high level (298 mg/l) (figure 1) during the first week of hospitalisation, suggesting a severe evolution of the clinical picture. The subsequent examinations included pulmonary scintigraphy (figure 2) with ventilation/perfusion images. Pulmonary scintigraphy showed a lack of ventilation/perfusion in the inferior portion of the right lung, suggesting together with the D-dimer presence of pulmonary embolism. Thoracic tomography (figure 3) further confirmed images compatible with thromboembolism in the same pulmonary area and a right-sided pulmonary effusion (figure 4). All these data suggested, in addition to the clinical data, the presence of a severe infection in the same side.
Figure 1.
(A) Significative increase of CRP and ESR, reflecting an acute inflammatory status secondary to a very severe pneumonia and pulmonary thromboembolism. (B) Leucocytes showed a small increase in the initial phase due to inflammatory/infectious disease and rapidly returned to normal levels. Platelets showed an initial reduction due to the combined therapy of rTPA plus heparin.
Figure 2.
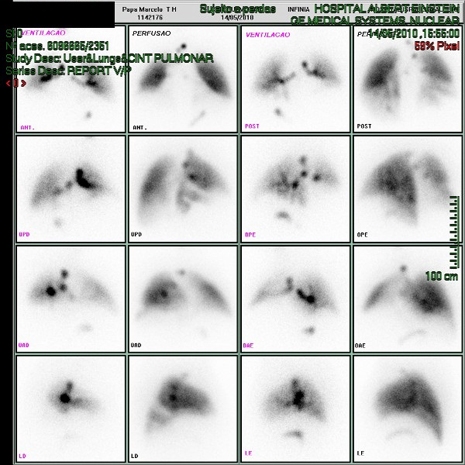
Images showing a lack of ventilation/perfusion in the inferior portion the right lung.
Figure 3.
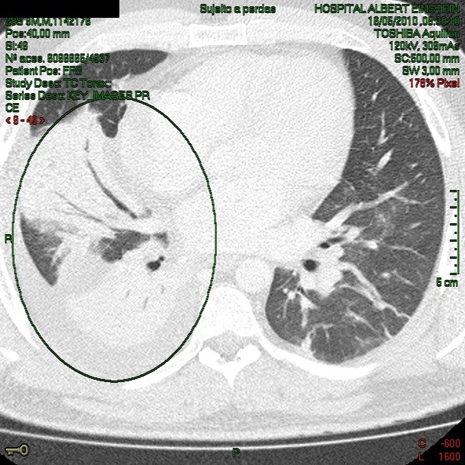
Thoracic tomography with the right lung compromised by pulmonary embolism and pneumonia.
Figure 4.
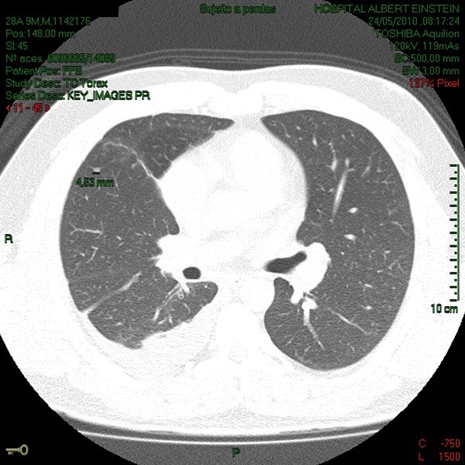
Pleural effusion in the inferior portion of the right lung.
Differential diagnosis
-
▶
Common pneumonia
-
▶
Myocardial infarction
-
▶
Myocarditis
-
▶
Common pulmonary thromboembolism.
Treatment
Initially, the patient was medicated with vancomycin (ABL Laboratories, Luxembourg, Luxembourg ) 500 mg intravenously 6/6 h. In the intensive care unit the patient was infused with recombinant tissue-type plasminogen activator 100 mg (Boehringer Ingelheim, Ingelheim am Rhein, Germany) intravenously, for 2 h, together with heparin 1000 IU/h. He was discharged with hydroxychloroquine sulphate (400 mg/day), aspirin and varfarin ‘per os’ as pharmacological therapy.
Outcome and follow-up
After 25 days the patient showed good clinical evolution, and was discharged with hydroxycloroquine sulphate, aspirin and varfarin ‘per os’ for the pharmacological therapy.
Discussion
We consider that this is a rare case that presents a M pneumoniae infection associated with pulmonary thromboembolism and signs of antiphospholipid syndrome. The patient had intensified chest pain and difficulties in breathing suggesting a very rapid and potentially severe evolution of a pneumonia infection. Antiphospholipid syndrome has been associated with increased risk for cardiovascular complications.1–8 The patient had antiphospholipid antibodies and, in this case, Phospholipid species (eg, PAF) generated by inflammation (detected by the presence of autoantibodies), which are potent mediators of acute inflammation.
Learning points.
-
▶
Acute pulmonary infections, associated with involvement of the cardiovascular system in addition to autoimmune components has to be thoroughly investigated and during the acute phase be subjected to close follow-up by the clinicians.
Acknowledgments
This work was financially supported by FAPESP, CNPq, CAPES and INCT-INAMI.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Espinosa G, Cervera R. Antiphospholipid syndrome: frequency, main causes and risk factors of mortality. Nat Rev Rheumatol 2010;6:296–300 [DOI] [PubMed] [Google Scholar]
- 2.Tincani A, Casu C, Cartella S, et al. Antiphospholipid antibody: laboratory, pathogenesis and clinical manifestations. Reumatismo 2010;62:65–75 [DOI] [PubMed] [Google Scholar]
- 3.Cohen D, Berger SP, Steup-Beekman GM, et al. Diagnosis and management of the antiphospholipid syndrome. BMJ 2010;340:c2541. [DOI] [PubMed] [Google Scholar]
- 4.Ieko M, Naito S, Yoshida M. Laboratory examinations in antiphospholipid syndrome. Rinsho Byori 2010;58:343–51 [PubMed] [Google Scholar]
- 5.Ford HJ, Roubey RA. Pulmonary manifestations of the antiphospholipid antibody syndrome. Clin Chest Med 2010;31:537–45 [DOI] [PubMed] [Google Scholar]
- 6.Sherer Y, Blank M, Shoenfeld Y. Antiphospholipid syndrome (APS): where does it come from? Best Pract Res Clin Rheumatol 2007;21:1071–8 [DOI] [PubMed] [Google Scholar]
- 7.Shoenfeld Y, Meroni PL, Cervera R. Antiphospholipid syndrome dilemmas still to be solved: 2008 status. Ann Rheum Dis 2008;67:438–42 [DOI] [PubMed] [Google Scholar]
- 8.Pabinger I, Ay C. Biomarkers and venous thromboembolism. Arterioscler Thromb Vasc Biol 2009;29:332–6 [DOI] [PubMed] [Google Scholar]