Abstract
Percutaneous endoscopic gastrostomy tube feeding is widely used for patients with swallowing dysfunction and a history of repeated aspiration pneumonitis. However, liquid nutrient feeding via percutaneous endoscopic gastrostomy is not effective enough to prevent aspiration pneumonitis and related inflammatory responses. We performed this prospective multi-centre study to clarify the efficacy of half-solidification of nutrients to prevent fever possibly caused by aspiration pneumonitis in elderly patients with percutaneous endoscopic gastrostomy. The study subjects were 42 elderly patients undergoing percutaneous endoscopic gastrostomy feeding (mean age 85.8 years). All subjects were fed half-solid as well as liquid nutrients for 8 weeks respectively in a cross over design. We counted the number of days with fever caused by pneumonitis and unidentified origin. Thirty-two of 42 patients were successfully observed in both nutrient periods. Fever was frequently observed in both nutrient periods, however, the percentage of observational days with fever during half-solid nutrient feeding was significantly lower than that during liquid nutrient feeding (15.3 ± 0.3 vs 19.8 ± 0.4%, p = 0.030). The percentage of observational days when patients had diarrhea was not significantly different (10.1 ± 3.8 vs 7.2 ± 3.2%, p = 0.357). In conclusion, half-solid nutrient feeding was determined to be effective for reducing fever in patients with percutaneous endoscopic gastrostomy feeding.
Keywords: aspiration pneumonitis, half-solidification, nutrient, percutaneous endoscopic gastrostomy
Introduction
Percutaneous endoscopic gastrostomy (PEG) tube feeding is widely used for patients with swallowing dysfunction caused by a number of disease conditions or a history of repeated aspiration pneumonitis. Aspiration pneumonitis caused by reflux of gastric contents including nutrients fed via PEG is one of the most frequent and life-threatening inflammatory events during long-term PEG feeding.(1–4) Solidification of nutrients is considered to be an effective method to prevent gastro-esophageal reflux (GER) of fed nutrients, and several studies have demonstrated that increased viscosity of nutrients reduces the risk of GER of nutrients in infants by mainly counting the occurrences of regurgitation and vomiting.(5–7) However, the efficacy of solidification of nutrients for the prevention of aspiration pneumonitis in elderly patients with PEG feeding was not yet fully investigated. Kanie and coworkers previously demonstrated that half-solidification of nutrients was useful for decreasing GER of nutrients. They used computed tomography scan to study the presence of nutrients mixed with water-soluble contrast agent in the esophagus.(8) It was, however, demonstrated that there was a zone of apparently unbuffered, highly acidic gastric juice above the ingested food at as early as 15 min after a meal, a phenomenon termed an “acid pocket”.(9) The presence of an acid pocket above the nutrients calls into question the effectiveness of solidification for preventing aspiration pneumonitis, since it is well-known that the aspiration of acidic gastric contents induces more severe pneumonitis.
We recently demonstrated that half-solidification of nutrients could not significantly decrease the frequency of GER events by using the esophageal multichannel intraluminal impedance (MII) and pH (MII-pH) monitoring method, which can detect any types of GER.(10) However, the volume of GER of gastric contents, which the MII-pH monitoring system couldn’t measure, is considered to affect the occurrence of aspiration pneumonitis. We, therefore, performed this prospective multi-centre study to test the efficacy of half-solidification of nutrients for preventing aspiration pneumonitis in elderly patients with tube feeding via PEG.
Subjects and Methods
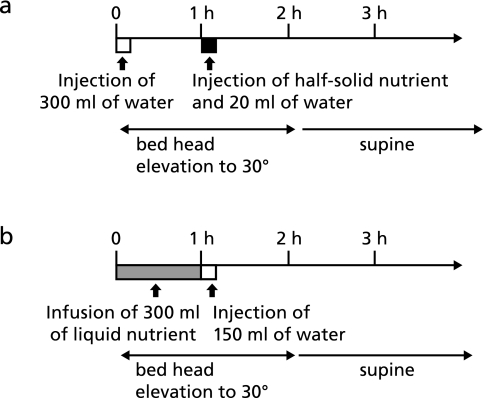
The subjects were 42 elderly patients undergoing PEG feeding (female: 31, mean age: 85.8 year, range: 56–100 year) in 8 hospitals in Shimane Prefecture, Japan. PEG feeding was started in these patients due to swallowing dysfunction caused by cerebral infarction, and almost all patients had a history of repeated aspiration pneumonitis. In all cases, feeding of liquid nutrients via PEG had been performed for over 3 months before study enrollment. After enrollment in this study, all subjects were fed by half-solid nutrients for 8 weeks and by liquid nutrients for 8 weeks in a random order. Medication for each patient was not changed between the periods of feeding. In this study, we used commercially available half-solid nutrients (150 or 200 g of MEDI-F PUSHCARE® from Ajinomoto Pharma Co., Inc., Tokyo, Japan). The volume of half-solid nutrients was determined by the total calories of the nutrients used in each patient before the study enrollment. Standard liquid nutrients were used for liquid feeding. Both types of nutrients were fed 3 times per day. The viscosity of MEDI-F PUSHCARE® is about 2000 mPas. The total calories, protein and lipids in 150 g of MEDI-F PUSHCARE® are 300 kcal, 14.0 g and 8.4 g, respectively. The volume of liquid nutrients was adjusted to equal the total calories, protein and lipids to those of MEDI-F PUSHCARE®. The quantity of basic minerals and vitamins was almost equal between the two kinds of nutrients. The water contents of MEDI-F PUSHCARE® and liquid nutrients were markedly different (81.3 g vs approximately 250 g). Therefore, total water volume in one meal was adjusted to 400 g by modifying the volume of water administered with the meals. Feeding of half-solid nutrients and liquid nutrients was done according to the schedule shown in Fig. 1. Half-solid nutrients were infused into stomach by the hands of medical staffs, and liquid nutrients were fed by gravity. Three hundred millilitres of water was given via the PEG feeding tube in 10 min before administration of the half-solid nutrient. One hour after giving 300 ml water, half-solid nutrients and 20 ml of water were delivered through the PEG tube in 10 min. Patients were instructed to remain supine, and the bed head was elevated to 30° for 2 h. For administration of the liquid nutrient, 300 ml of nutrient was infused via the PEG feeding tube in 1 h, followed by delivery of 150 ml water in 10 min. Patients were instructed to remain supine, and the bed head was elevated to 30° for 2 h.
Fig. 1.
Nutrient administration schedule (a: feeding schedule of half-solid nutrients, and b: feeding schedule of liquid nutrients).
Feeding time for each patient and the days when fever, defecation and diarrhea were observed, were carefully recorded on sheets during the 16-week study period. The time necessary for feeding included the time for preparing nutrients and for administering nutrients and water, since medical staff frequently needed to observe the patients during nutrient feeding. We counted the number of days with fever caused by pneumonitis and unidentified origin to detect possible aspiration pneumonitis, since fever observed in elderly patients with PEG feeding and a history of repeated pneumonitis is highly speculated to be caused by aspiration pneumonitis. In this study, fever was defined as a body temperature of over 37°C, and watery or muddy stool was defined as diarrhea. The time necessary for feeding and the days with fever, defecation and diarrhea were compared between half-solid and liquid nutrient feeding periods. We used the percentages in all the observed days to compare the number of days with fever, defecation and diarrhea because some patients could not complete the study protocol for various reasons. The data of patients with at least a 4-week-long observation period using both half-solid nutrient and liquid nutrient were taken for analysis in this study.
Data were expressed as mean ± SE. Statistical analysis was performed using the Wilcoxon signed rank test, and differences at p<0.05 were considered statistically significant.
This study was performed in accordance with the declaration of Helsinki. The study protocol was approved by the ethics committee of Shimane University, Faculty of Medicine, and written informed consent was obtained from all study subjects or their family members.
Results
Twenty-six of 42 study subjects completed the 16-week study protocol. Sixteen patients could not complete the 16-week study protocol due to: transfer to another hospital or home (n = 4), life threatening pneumonitis which necessitates fasting over several days (n = 7), continuous severe diarrhea which necessitates a change of nutrients (n = 4), or acute renal failure of unknown origin (n = 1). Of the 16 patients who could not complete the 16-week study, 6 completed at least the 4-week observational period in both types of nutrients. In this study, these 6 patients plus the 26 who completed the whole 16-week protocol were the 32 patients we analyzed.
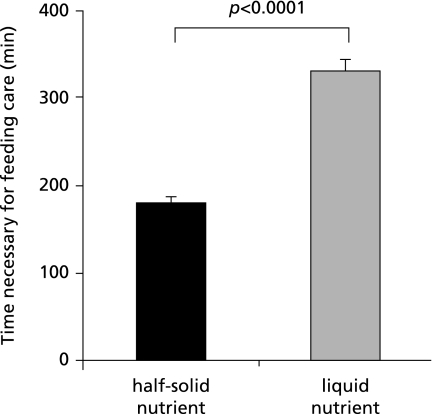
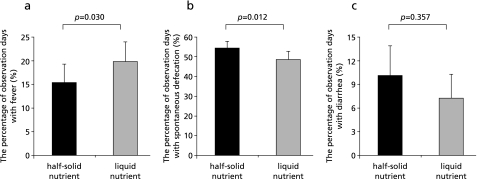
The necessary time for feeding half-solid nutrients was significantly shorter than that for feeding liquid nutrients (180.4 ± 8.1 vs 329.7 ± 14.8 min/day, p<0.0001), as shown in Fig. 2. The numbers of patients who did not show fever during the observational period of half-solid feeding and liquid feeding were only 5 and 7, respectively. Thus, fever was frequently observed during both feeding periods. However, the percentage of days with fever during the half-solid nutrient feeding period was significantly lower than that during the liquid nutrient feeding period (15.3 ± 0.3 vs 19.8 ± 0.4%, p = 0.030). The percentage of days with spontaneous defecation during the half-solid nutrient feeding period was significantly higher than that during the liquid nutrient feeding period (54.6 ± 3.5 vs 48.7 ± 4.2%, p = 0.013). However, the number of patients who did not develop diarrhea during the half-solid nutrient feeding period was similar to that during the liquid nutrient feeding (15 vs 19 cases). The percentage of days with diarrhea was also not significantly different between the half-solid nutrient and liquid nutrient feeding periods (10.1 ± 3.8 vs 7.2 ± 3.2%, p = 0.357) (Fig. 3).
Fig. 2.
Time necessary for feeding care during half-solid nutrient feeding and that during liquid feeding.
Fig. 3.
The percentage of observational days with fever (a), spontaneous defecation (b), and diarrhea (c) during half-solid nutrient feeding and during liquid nutrient feeding.
Discussion
The feeding of nutrients via PEG is widely used for patients with swallowing dysfunction. Aspiration pneumonitis induced by GER of gastric contents is an important and serious problem for patients with long-term PEG feeding.(1–4) The degree of GER during PEG feeding is reported to be related to esophageal motor function, volume or rate of gastric infusion, gastric emptying, posture during feeding, accompanying diseases such as diabetes or scleroderma, and usage of drugs that affect esophageal motor function.(1) Solidification of nutrients is considered to be one of the most effective method to prevent gastro-esophageal reflux (GER) of nutrient itself. However, a zone of apparently unbuffered highly acidic gastric juice above the ingested food was observed after meals, and this was considered an important cause of postprandial acidic GER.(9) The zone of acidic gastric juice after the administration of solid nutrients may be wider than that after liquid nutrients, since gastric juice could be easily mixed with liquid nutrients. Recently, we demonstrated that half-solidification of nutrients could not decrease the number of GER events and half-solidification tends to increase acidic GER in patients with PEG feeding using the esophageal MII-pH monitoring method.(10) However, the results of this prospective multi-centre study showed that the usage of half-solid nutrients significantly decreases the percentage of days with fever in elderly patients with PEG feeding. Since fever in patients with PEG feeding is mainly caused by aspiration of refluxed gastric contents, the result of this study seems not to fit with the results of our previous MII-pH monitoring study, which could not demonstrate the reduction of GER events during half-solid nutrient feeding. The larger volume of GER of gastric contents, which the MII-pH monitoring system could not investigate, may be more important as a risk factor of aspiration pneumonitis. Although the half-solid nutrients were effective to decrease the number of days with fever, it did not completely prevent the occurrence of aspiration pneumonitis in patients with PEG feeding. The therapeutic effect of anti-secretory therapy in combination with half-solidification of nutrients, which can decrease the zone of highly acidic gastric juice above ingested food, should be further investigated.
Half-solidification of nutrients is considered to have several advantages other than decreasing GER of nutrients. It could prevent the leakage of nutrients from the gaps between PEG fistula and tubing. It may prevent diarrhea caused by rapid delivery of high-osmolar liquid nutrient into the small intestine.(11,12) The results of this study clearly demonstrated that the usage of half-solid nutrient could decrease the workload of medical staff, since it can be easily administered in a short period. The shorter necessary time of feeding could also reduce the duration of bed head elevation of patients, and this might be effective for the prevention of pressure ulcers.(13) The percentage of days with spontaneous defecation during half-solid nutrient feeding was significantly higher than that during liquid nutrient feeding, although we found no significant difference in the percentage of days with diarrhea in this study. The occurrence of diarrhea is considered to correlate with the speed of nutrient and water administration. Although the solidification of nutrients has an advantage for preventing diarrhea, the increased frequency in defecation during half-solid nutrient feeding might be caused by the rapid infusion of 300 ml of water before the feeding of half-solid nutrients.
The limitations of this study are the small number of enrolled cases and the uncertainty in the diagnosis of aspiration pneumonitis as a cause of fever. In the future, a large-scale study using more realistic diagnostic markers of aspiration pneumonitis is considered necessary to confirm the results of this study.
In conclusion, this prospective multi-centre study demonstrated that half-solidification of nutrition is effective for a reduction of the days with fever in elderly patients using PEG feeding.
Acknowledgment
This study was supported by the funding from the Grants-in-Aid from Science Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan, No. 22590681. None of the authors had a personal or financial conflict of interest.
References
- 1.Coben RM, Weintraub A, DiMarino AJ, Jr., Cohen S. Gastroesophageal reflux during gastrostomy feeding. Gastroenterology. 1994;106:13–18. doi: 10.1016/s0016-5085(94)93969-1. [DOI] [PubMed] [Google Scholar]
- 2.Marik PE. Aspiration pneumonitis and aspiration pneumonia. N Engl J Med. 2001;344:665–671. doi: 10.1056/NEJM200103013440908. [DOI] [PubMed] [Google Scholar]
- 3.Sanders DS, Carter MJ, D’Silva J, McAlindon ME, Willemse PJ, Bardham KD. Percutaneous endoscopic gastrostomy: a prospective analysis of hospital support required and complications following discharge to the community. Eur J Clin Nutr. 2001;55:610–614. doi: 10.1038/sj.ejcn.1601197. [DOI] [PubMed] [Google Scholar]
- 4.Carnes ML, Sabol DA, DeLegge M. Does the presence of esophagitis prior to PEG placement increase the risk for aspiration pneumonia? Dig Dis Sci. 2004;49:1798–1802. doi: 10.1007/s10620-004-9573-4. [DOI] [PubMed] [Google Scholar]
- 5.Penna FJ, Norton RC, Carvalho AS, et al. Comparison between pre-thickened and home-thickened formulas in gastroesophageal reflux treatement. J Pediatr (Rio J) 2003;79:49–54. [PubMed] [Google Scholar]
- 6.Wenzl TG, Schneider S, Scheele F, Silny J, Heimann G, Skopnik H. Effects of thickened feeding on gastroesophageal reflux in infants: a placebo-controlled crossover study using intraluminal impedance. Pediatrics. 2003;111(4 Pt 1):e355–e359. doi: 10.1542/peds.111.4.e355. [DOI] [PubMed] [Google Scholar]
- 7.McPherson V, Wright ST, Bell AD. Clinical inquiries. What is the best treatment for gastroesophageal reflux and vomiting in infants? J Fam Pract. 2005;54:372–375. [PubMed] [Google Scholar]
- 8.Kanie J, Suzuki Y, Iguchi A, Akatsu H, Yamamoto T, Shimokata H. Prevention of gastroesophageal reflux using an application of half-solid nutrients in patients with percutaneous endoscopic gastrostomy feeding. J Am Geriatr Soc. 2004;52:466–467. doi: 10.1111/j.1532-5415.2004.52125_1.x. [DOI] [PubMed] [Google Scholar]
- 9.Fletcher J, Wirz A, Young J, Vallance R, McColl KE. Unbuffered highly acidic gastric juice exists at the gastroesophageal junction after a meal. Gastroenterology. 2001;121:775–783. doi: 10.1053/gast.2001.27997. [DOI] [PubMed] [Google Scholar]
- 10.Adachi K, Furuta K, Morita T, et al. Half-solidification of nutrient does not decrease gastro-esophageal reflux events in patients fed via percutaneous endoscopic gastrostomy. Clin Nutr. 2009;28:648–651. doi: 10.1016/j.clnu.2009.05.006. [DOI] [PubMed] [Google Scholar]
- 11.Guenter PA, Settle RG, Perlmutter S, Marino PL, DeSimone GA, Rolandelli RH. Tube feeding-related diarrhea in acutely Ill patients. JPEN J Parenter Enteral Nutr. 1991;15:277–280. doi: 10.1177/0148607191015003277. [DOI] [PubMed] [Google Scholar]
- 12.Bhatnagar S, Bhandari N, Mouli UC, Bhan MK. Consensus statement of IAP national task force: status report on management of acute diarrhea. Indian Pediatr. 2004;41:335–348. [PubMed] [Google Scholar]
- 13.Dini V, Bertone M, Romanelli M. Prevention and management of pressure ulcers. Dermatol Ther. 2006;19:356–364. doi: 10.1111/j.1529-8019.2006.00094.x. [DOI] [PubMed] [Google Scholar]