Abstract
The aim of this study was to examine the association between serum apolipoprotein B (apoB) and the risk of coronary heart disease (CHD) using Framingham risk score (FRS) in healthy Korean men. A total of 13,523 men without medication history of diabetes and hypertension were enrolled in this study. The FRS is based on six coronary risk factors. FRS ≥ 10% was defined as more-than-a-moderate risk group and FRS ≥ 20% as high risk group, respectively. The logistic regression analyses were conducted. When quartile 1 (Q1) set as a reference, in unadjusted analyses, the Q2, Q3, Q4 of apoB level had increased odds ratio (OR) for the risk of CHD in both more-than-a-moderate risk and high risk group, respectively. After adjusting for confounding variables, multivariable-adjusted logistic regression analyses showed a strong relationship between the quartiles of apoB level and more-than-a-moderate risk and high risk group, respectively. These associations were attenuated, but still remained statistically significant. ApoB is found to be independently related to the risk of CHD using FRS in healthy Korean men, and the link between apoB and the risk of CHD is dose-depedent.
Keywords: Framingham Risk Score, Apolipoproteins B, Coronary Disease
INTRODUCTION
Apolipoproteins (Apo) are the protein components of plasma lipoproteins and also known to determine the structural stability and metabolism of lipoproteins. ApoB and apoA-I are the main structural proteins of low-density lipoprotein (LDL) and high-density lipoprotein (HDL) particles, respectively. ApoB puts together the precursors of LDL and very-low-density lipoprotein (VLDL) in the liver (1).
Until now, diabetes mellitus, hypertension, and dyslipidemia have been regarded as established predictors of cardiovascular disease. Life style risk factors, including dietary habits, physical inactivity, smoking, alcohol intake, stress and obesity strongly affect the established cardiovascular risk factors (2-4). The reduction of risk factors for cardiovascular disease can prevent the incidence of the cardiovascular diseases (5). The assessment, treatment, monitoring and prevention of these risk factors are major emphases of clinical care, research investigation and treatment guidelines. The Framingham risk prediction model was based on the 12 yr of follow-up of 5,573 members of the Framingham Heart Study, aged 35-74 yr free from symptomatic cardiovascular diseases at baseline (6). The Framingham risk score (FRS) has been a traditionally used algorithm in primary prevention strategies for the assessment of 10-yr risk for coronary heart disease (CHD) events in middle-aged, asymptomatic individuals (7). Recently, several studies have reported that other risk factors for CHD were associated with the FRS (8-10).
However, there have been few reports on the relationship between apoB and risk of CHD using FRS. Furthermore, no reliable data obtained by healthy men without diabetic and hypertensive medication are available regarding the risk of CHD development with apoB level. Therefore, we conducted the large scaled cross-sectional study. The aim of this study was to determine whether plasma concentrations of apoB have an elevated 10-yr risk of developing CHD using FRS in healthy Korean men.
MATERIALS AND METHODS
Study subjects
A cross-sectional study was conducted to examine the association between serum apoB and risk for CHD in healthy Korean men who were employed at various companies in Korea. All employees participated in an annual health examination, as was required by Korea's Industrial Safety and Health law. A total of 25,594 men participated in the comprehensive health examinations at a university hospital in Seoul, from January to December in 2007. Among them, 3,828 were excluded for various reasons: 14 had a past history of a malignancy; 2,375 were taking medication for diabetes; 1,688 were taking medication for hypertension at their initial examinations. Because some individuals had more than one exclusion criterion, the total number that was eligible for the study was 21,766. We excluded an additional 1,075 from our study subjects not calculating FRS, 7,087 not possessing information about apoB variables and 81 aged less than 30 yr old. FRS should be applied to individuals who are over 30 yr old (2), because FRS may less accurately predict the risk of CHD in younger individuals. Ultimately, 13,523 men, aged 30 to 77 yr old, were enrolled in the analysis and were observed the relationship between apoB and the risk of CHD using FRS.
Clinical and laboratory measurements
The initial health examinations that were performed in 2007 included a medical history, a physical examination, a questionnaire about health-related behavior, anthropometric measurements, and biochemical measurements. The medical history and the history of drug prescription were assessed by the examining physicians. All the participants were asked to respond to a questionnaire on health-related behavior. Questions about alcohol intake included the frequency of alcohol consumption on a weekly basis and the usual amount that was consumed on a daily basis (≥ 20 g/day). We considered persons reporting that they smoked at that time to be current smokers. Overweight and obesity was defined as a body mass index (BMI) ≥ 25 kg/m2 for all subjects as an index of obesity because this cut-off has been proposed for the diagnosis of obesity in Asian people (11).
Blood samples were collected after more than 12 hr of fasting and were drawn from an antecubital vein. The total cholesterol, triglycerides, LDL-cholesterol, HDL-cholesterol, alanine aminotransferase (ALT) and aspartate aminotransferase (AST) were measured enzymatically with an automatic analyzer (Advia 1650 Autoanalyzer, Bayer Diagnostics; Leverkusen, Germany). The fasting serum glucose was measured with the hexokinase method. Insulin levels were measured with immunoradiometric assays (Biosource, N. velles, Belgium). Insulin resistance was assessed with the Homeostasis Model Assessment of insulin resistance (HOMA-IR): Fasting serum insulin (µU/mL) × fasting blood glucose (mg/dL)/22.5. High sensitivity-C reactive protein (hsCRP) was measured by immunonephelometry (Dade Behring Co., Marburg, Germany), and apoA-I and apoB measured by rate nephelometry (Beckman Instruments, Fullerton, CA, USA). Distribution of values was assessed by the Kolmogorov-Smirnov test for normality of distribution. Because the values of hsCRP were skewed to the right, its log-transformed data were used in analysis. Trained nurses obtained sitting blood pressure (BP) levels with a standard mercury sphygmomanometer. The first and fifth Korotkoff sounds were utilized in order to estimate the systolic BP and the diastolic BP. Height and weight were measured after an overnight fast with the subjects wearing a light-weight hospital gown and no shoes. The BMI was calculated as the weight (kg) divided by the square of the height (m).
Framingham risk score assessment
The FRS was calculated from the National Cholesterol Education Program (NCEP) Adult Treatment Panel (ATP) III algorithm, based on six coronary risk factors: gender, age, total cholesterol, HDL-cholesterol, systolic BP and smoking habit (7). Among these factors, age, BP, and cholesterol levels were categorized according to their values and smoking status was classified as either "current smoker" or "non-smoker". Finally, the corresponding point was given to each man and then the total score was used as the individual's CHD risk level. The FRS has been used to predict the 10-yr risk of coronary events (fatal/nonfatal myocardial infarction or sudden death) (12). The FRS for CHD over 10 yr was calculated for each man (12), and divided into three levels of risk < 10% (low), 10%-19% (intermediate) and ≥ 20% (high) (7). In this study, we defined FRS ≥ 10% as more-than-a-moderate CHD risk group and FRS ≥ 20% as a high CHD risk group, respectively.
Statistical analyses
The one-way ANOVA and chi-squared test were used to analyze the statistical differences across the characteristics of the study participants in relation to the quartiles of apoB level and 10 yr-predicted-risk groups of the FRS. More-than-a-moderate risk (FRS ≥ 10%) and high risk (FRS ≥ 20%) were considered as dependent variable. The logistic regression analyses were conducted to calculate the odds ratio (OR) and 95% confidence interval (CI). The data were first unadjusted, then adjusted for the multiple covariates. In multivariable model, we included apoB/apoA-I, BMI, diastolic BP, LDL-cholesterol, triglyceride, ALT, HOMA-IR, log (hsCRP) and alcohol intake. The statistical analysis for the data was performed with SAS version 9.1 (SAS Institute Inc., Cary, NC, USA). All the reported P values were two-tailed, and those < 0.05 were considered to be statistically significant.
Ethics statement
This study was approved by the institutional review board of Kangbuk Samsung Hospital, Sungkyunkwan University, School of Medicine in Seoul, Korea (IRB number: KBC09100). All participants gave their written informed consent.
RESULTS
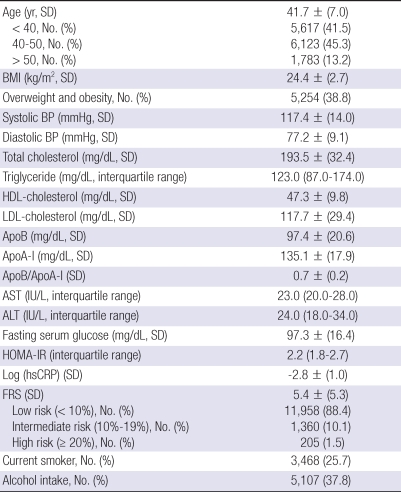
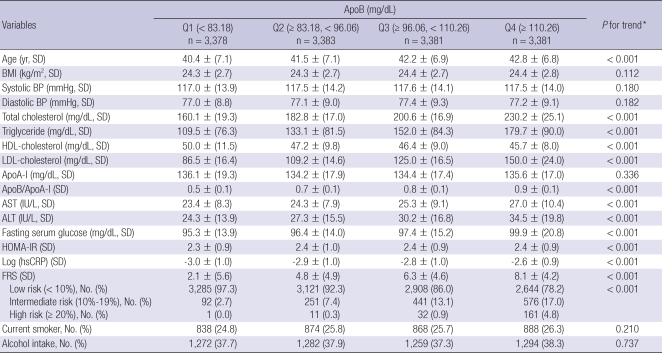
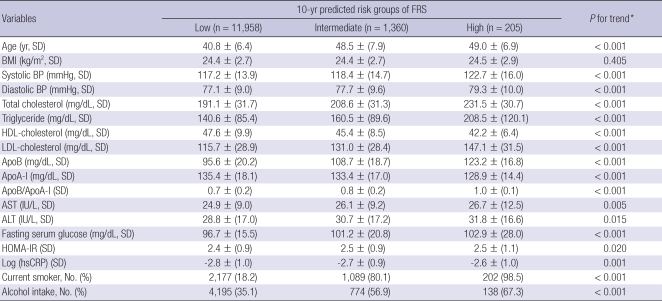
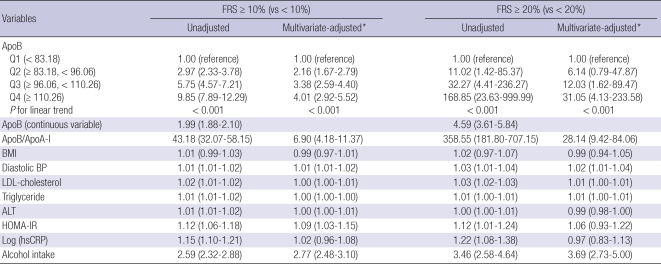
The relevant clinical characteristics of the 13,523 male subjects are shown in Table 1. Overall, the mean ± standard deviation of age and FRS were 41.7 ± 7.0 yr and 5.4 ± 5.3, respectively. The mean apoB, apoA-I and apoB/apoA-I were 97.4 ± 20.6 mg/dL, 135.1 ± 17.9 mg/dL and 0.7 ± 0.2, respectively (mean ± standard deviation). The prevalence of current smoker was 25.7%. 37.8% of the study subjects had an alcohol intake ≥ 20 g/day. The relevant clinical characteristics in relation to the quartiles (Q) of apoB level are shown in Table 2. In the categorical analyses, the FRS increased with the quartiles of apoB level (P for trend < 0.001). The relevant clinical characteristics in relation to the 10 yr-predicted-risk groups of FRS are shown in Table 3. These data showed that there was a significant relationship between all the clinical variables and three groups of the 10 yr-predicted-risk of FRS except for BMI. Table 4 presents the OR and 95% CI of the risk of CHD with respect to the continuous variable of apoB and the quartiles of apoB level. The unadjusted OR and 95% CI of the risk of CHD with respect to the continuous variable of apoB was 1.99 (1.88-2.10) in more-than-a-moderate risk (FRS ≥ 10%) and 4.59 (3.61-5.84) in high risk (FRS ≥ 20%), respectively. When Q1 set as a reference, in unadjusted analyses, the Q2, Q3, Q4 of apoB level had increased OR for the risk of CHD in both more-than-a-moderate risk and high risk group (P for trend < 0.001). After adjusting for apoB/apoA-I, BMI, diastolic BP, LDL-cholesterol, triglyceride, ALT, HOMA-IR, log (hsCRP) and alcohol intake, multivariable-adjusted logistic regression analyses showed a strong relationship between the quartiles of apoB level and more-than-a-moderate risk and high risk group, these associations were attenuated, but still remained statistically significant.
Table 1.
Characteristics of the study subjects (n = 13,523)
All values are the mean ± SD, median (interquartile range) or the number of subjects (percent of the total). SD, standard deviation; BMI, body mass index; BP, blood pressure; AST, aspartate aminotransferase; ALT, alanine aminotransferase; HOMA-IR, Homeostasis Model Assessment of insulin resistance; hsCRP, high-sensitivity C-reactive protein; FRS, Framingham risk score.
Table 2.
Comparison of baseline characteristics among quartile groups of ApoB level (n = 13,523)
Categorical data presented as No. (%); continuous data presented as mean (SD). *P value by ANOVA for continuous variables and chi square test for categorical variables.
Table 3.
Characteristics of the study subjects stratified for 10-yr predicted risk groups (n = 13,523)
Categorical data presented as No. (%); continuous data presented as mean (SD). *P value by ANOVA for continuous variables and chi square test for categorical variables.
Table 4.
Odds ratio (OR) and 95% confidence intervals (CI) assessing the independent influence of ApoB on more-than-a-moderate risk (FRS ≥ 10%) and high risk (FRS ≥ 20%) of CHD
*Multivariate-adjusted for apoB/apoA-I, BMI, diastolic BP, LDL-cholesterol, triglyceride, ALT, HOMA-IR, log (hsCRP) and alcohol intake.
The total of study subjects is 21,766; 13,523 included in analysis and 8,243 excluded from analysis. There are no major inconsistencies between the exclusion and inclusion of individuals except for age, fasting serum glucose and alcohol intake. Therefore, exclusion of these individuals would be unlikely to cause bias (data not shown).
DISCUSSION
This study demonstrated that apoB showed significant relationship with three groups of the 10 yr-predicted-risk of FRS. In unadjusted and multivariable-adjusted logistic regression analyses, apoB was found to be independently related to the risk of CHD using FRS in healthy Korean men, and the link between apoB and the risk of CHD was found to be dose-response related. In addition, apoB with a high risk showed a tendency to increase the risk of developing CHD. These findings provided an important point of view understanding the incidence of CHD, and furthermore, supported the notion that apoB should be considered as an additional atherogenic parameter in relation to CHD. As far as we know, few epidemiologic studies have explored the link between apoB and the risk of CHD using FRS, especially healthy men. Our findings are so valuable for the basis of the public health because these are based on a large sample of the general population of Korean men, where the incidence of CHD is common.
In the western countries, high apoB and low apoA-I have been shown to be an independent predictor of CHD (13-18); however, there have been no evidence to date that apos have a predictive value for CHD in Korea, even in Asian countries. In this regard, the present findings suggest the possibility that apoB rather than other atherogenic parameter, such as LDL-cholesterol, triglyceride and alcohol intake might be able to predict the future development of CHD in Korean population.
The mechanisms and the reasons that the apoB is highly associated with the CHD are not fully understood. However, Sniderman et al. (19) emphasized the importance of apoB in the development of cardiovascular disease, suggesting that the risk of cardiovascular disease is maximized if hypertriglyceridemia was associated with the high level of apoB, as an increased number of LDL particles and density.
Several recent reports have presented the possibility that the apos have been proposed as a better index for predicting the risk of cardiovascular disease than the traditional lipid parameters, based on the premise that apoB levels fully reflect the number of atherogenic lipoprotein particles, such as VLDL, intermediate-density lipoproteins, and LDL (13, 14, 18, 20-23). In the present study, the odds ratio of apoB was bigger than that of other lipid parameters.
The findings of the present study have clinically important implications. ApoB measurements may be more convenient, because they do not require blood sampling at fasting status (24). The costs for apoB measurement are lower than those of total cholesterol and HDL-cholesterol (25). The present diagnostic guideline of dyslipidemia did not include the apoB level in clinical settings, and the proper guideline for diagnose, treatment and medication should also be established, sooner or later.
This study has several potential limitations. First, this study is just confined to relatively racially homogeneous male of individuals of Korean ancestry who were recruited at a single urban hospital, so we cannot extrapolate our results to another race. Second, we used the FRS scales which were applied for the western people, so the FRS in this study may not reflect the typical characteristics of Korean people completely. In the future, FRS scales for Korean people should be prepared for next analysis. Despite these limitations, strengths of the present study include the large number of healthy male participants with comprehensive measurement of a panel of lipids and apos, including the direct measurement of lipids. Additionally, detailed information on cardiovascular risk factors was available. The participants not only had no past histories of a malignancy but also did not take medication for diabetes and hypertension at their initial examinations. So, this study was considered to provide strong evidence for association between FRS and the other various lipid parameters, such as apoB, apoA-I and so on.
In conclusion, our results strongly suggest that apoB is independently related to the risk of CHD using FRS in healthy Korean men, and the link between apoB and the risk of CHD is found to be dose-dependent.
ACKNOWLEDGMENTS
We thank members of the health screening center at Kangbuk Samsung Hospital, Seoul, Korea for their efforts.
AUTHOR SUMMARY
Apolipoprotein B is Highly Associated with the Risk of Coronary Heart Disease as Estimated by the Framingham Risk Score in Healthy Korean Men
Jae-Hong Ryoo, Eun- Hee Ha, Soo-Geun Kim, Seungho Ryu, and Da-Woon Lee
Apolipoproteins (Apos) are the protein components of plasma lipoproteins. In the western countries, high apoB has been shown to be an independent predictor of coronary heart disease (CHD); however, there is no evidence to date that apoB has a predictive value for CHD in Korea. Here we investigated whether the plasma concentrations of apoB have an elevated 10-yr risk of developing CHD using Framingham risk score (FRS) in healthy Korean men. Multivariable-adjusted logistic regression analyses showed a strong relationship between the quartile groups of apoB and high CHD risk group. ApoB measurement is more convenient, because it does not require fasting status. Therefore, our data suggest that apoB could be considered as an additional predictive parameter in relation to the CHD.
References
- 1.Olofsson SO, Wiklund O, Borén J. Apolipoproteins A-I and B: biosynthesis, role in the development of atherosclerosis and targets for intervention against cardiovascular disease. Vasc Health Risk Manag. 2007;3:491–502. [PMC free article] [PubMed] [Google Scholar]
- 2.Wilson PW, D'Agostino RB, Levy D, Belanger AM, Silbershatz H, Kannel WB. Prediction of coronary heart disease using risk factor categories. Circulation. 1998;97:1837–1847. doi: 10.1161/01.cir.97.18.1837. [DOI] [PubMed] [Google Scholar]
- 3.Kim DS, Kang SK. Work-related cerebro-cardiovascular diseases in Korea. J Korean Med Sci. 2010;25(Suppl):S105–S111. doi: 10.3346/jkms.2010.25.S.S105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Poirier P. Healthy lifestyle: even if you are doing everything right, extra weight carries an excess risk of acute coronary events. Circulation. 2008;117:3057–3059. doi: 10.1161/CIRCULATIONAHA.108.784389. [DOI] [PubMed] [Google Scholar]
- 5.Wood D, De Backer G, Faergeman O, Graham I, Mancia G, Pyörälä K. Prevention of coronary heart disease in clinical practice: recommendations of the Second Joint Task Force of European and other Societies on Coronary Prevention. Atherosclerosis. 1998;140:199–270. doi: 10.1016/s0021-9150(98)90209-x. [DOI] [PubMed] [Google Scholar]
- 6.Kannel WB, Feinleib M, McNamara PM, Garrison RJ, Castelli WP. An investigation of coronary heart disease in families. The Framingham offspring study. Am J Epidemiol. 1979;110:281–290. doi: 10.1093/oxfordjournals.aje.a112813. [DOI] [PubMed] [Google Scholar]
- 7.National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) Third report of the National Cholesterol Education Program (NCEP) expert panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel III) final report. Circulation. 2002;106:3143–3421. [PubMed] [Google Scholar]
- 8.Otsuka T, Kawada T, Katsumata M, Ibuki C, Kusama Y. High-sensitivity C-reactive protein is associated with the risk of coronary heart disease as estimated by the Framingham Risk Score in middle-aged Japanese men. Int J Cardiol. 2008;129:245–250. doi: 10.1016/j.ijcard.2007.07.099. [DOI] [PubMed] [Google Scholar]
- 9.Jeong JC, Ro H, Hwang YH, Lee HK, Ha J, Ahn C, Yang J. Cardiovascular diseases after kidney transplantation in Korea. J Korean Med Sci. 2010;25:1589–1594. doi: 10.3346/jkms.2010.25.11.1589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wannamethee SG, Lennon L, Shaper AG. The value of gamma-glutamyltransferase in cardiovascular risk prediction in men without diagnosed cardiovascular disease or diabetes. Atherosclerosis. 2008;201:168–175. doi: 10.1016/j.atherosclerosis.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 11.WHO Western Pacific Region; IASO; IOTF. The Asia-Pacific perspective: redefining obesity and its treatment. Sydney: Health Communications Australia Pty; 2000. [Google Scholar]
- 12.Anderson KM, Wilson PW, Odell PM, Kannel WB. An updated coronary risk profile. A statement for health professionals. Circulation. 1991;83:356–362. doi: 10.1161/01.cir.83.1.356. [DOI] [PubMed] [Google Scholar]
- 13.Lamarche B, Moorjani S, Lupien PJ, Cantin B, Bernard PM, Dagenais GR, Després JP. Apolipoprotein A-I and B levels and the risk of ischemic heart disease during a five-year follow-up of men in the Québec cardiovascular study. Circulation. 1996;94:273–278. doi: 10.1161/01.cir.94.3.273. [DOI] [PubMed] [Google Scholar]
- 14.Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB. Non-high-density lipoprotein cholesterol and apolipoprotein b in the prediction of coronary heart disease in men. Circulation. 2005;112:3375–3383. doi: 10.1161/CIRCULATIONAHA.104.532499. [DOI] [PubMed] [Google Scholar]
- 15.Ridker PM, Rifai N, Cook NR, Bradwin G, Buring JE. Non-HDL cholesterol, apolipoproteins A-I and b100, standard lipid measures, lipid ratios, and CRP as risk factors for cardiovascular disease in Women. JAMA. 2005;294:326–333. doi: 10.1001/jama.294.3.326. [DOI] [PubMed] [Google Scholar]
- 16.Shai I, Rimm EB, Hankinson SE, Curhan G, Manson JE, Rifai N, Stampfer MJ, Ma J. Multivariate assessment of lipid parameters as predictors of coronary heart disease among postmenopausal women: potential implications for clinical guidelines. Circulation. 2004;110:2824–2830. doi: 10.1161/01.CIR.0000146339.57154.9B. [DOI] [PubMed] [Google Scholar]
- 17.Sharrett AR, Ballantyne CM, Coady SA, Heiss G, Sorlie PD, Catellier D, Patsch W Atherosclerosis Risk in Communities Study Group. Coronary heart disease prediction from lipoprotein cholesterol levels, triglycerides, lipoprotein(a), apolipoproteins A-I and B, and HDL density subfractions: the Atherosclerosis Risk in Communities (ARIC) study. Circulation. 2001;104:1108–1113. doi: 10.1161/hc3501.095214. [DOI] [PubMed] [Google Scholar]
- 18.Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E. High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS study): a prospective study. Lancet. 2001;358:2026–2033. doi: 10.1016/S0140-6736(01)07098-2. [DOI] [PubMed] [Google Scholar]
- 19.Sniderman AD, Scantlebury T, Cianflone K. Hypertriglyceridemic hyperapob: the unappreciated atherogenic dyslipoproteinemia in type 2 diabetes mellitus. Ann Intern Med. 2001;135:447–459. doi: 10.7326/0003-4819-135-6-200109180-00014. [DOI] [PubMed] [Google Scholar]
- 20.Walldius G, Jungner I. Apolipoprotein B and apolipoprotein A-I: risk indicators of coronary heart disease and targets for lipid-modifying therapy. J Intern Med. 2004;255:188–205. doi: 10.1046/j.1365-2796.2003.01276.x. [DOI] [PubMed] [Google Scholar]
- 21.Lamarche B, Tchernof A, Moorjani S, Cantin B, Dagenais GR, Lupien PJ, Després JP. Small, dense low-density lipoprotein particles as a predictor of the risk of ischemic heart disease in men. Prospective results from the Québec Cardiovascular Study. Circulation. 1997;95:69–75. doi: 10.1161/01.cir.95.1.69. [DOI] [PubMed] [Google Scholar]
- 22.St-Pierre AC, Ruel IL, Cantin B, Dagenais GR, Bernard PM, Després JP, Lamarche B. Comparison of various electrophoretic characteristics of LDL particles and their relationship to the risk of ischemic heart disease. Circulation. 2001;104:2295–2299. doi: 10.1161/hc4401.098490. [DOI] [PubMed] [Google Scholar]
- 23.Lemieux I, Lamarche B, Couillard C, Pascot A, Cantin B, Bergeron J, Dagenais GR, Després JP. Total cholesterol/HDL cholesterol ratio vs LDL cholesterol/HDL cholesterol ratio as indices of ischemic heart disease risk in men: the Quebec Cardiovascular Study. Arch Intern Med. 2001;161:2685–2692. doi: 10.1001/archinte.161.22.2685. [DOI] [PubMed] [Google Scholar]
- 24.Marcovina SM, Albers JJ, Kennedy H, Mei JV, Henderson LO, Hannon WH. International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. IV. Comparability of apolipoprotein B values by use of International Reference Material. Clin Chem. 1994;40:586–592. [PubMed] [Google Scholar]
- 25.Miremadi S, Sniderman A, Frohlich J. Can measurement of serum apolipoprotein B replace the lipid profile monitoring of patients with lipoprotein disorders? Clin Chem. 2002;48:484–488. [PubMed] [Google Scholar]