Abstract
This is the first reported detection of serum IgE antibody to piperacillin-human serum albumin (HSA) conjugate in a patient presenting with anaphylaxis that developed after occupational exposure. A 24-yr-old nurse, who had worked at a University Hospital for 2 yr, experienced chest tightness, dizziness, generalized urticaria, abdominal pain, and diarrhea 10 min after administering a piperacillin injection. She had previously suffered from atopic dermatitis. A skin prick test for common inhalant allergens was entirely negative; in contrast, her serum total IgE was elevated (283 IU/mL). A high level of piperacillin-specific serum IgE was detected by ELISA using piperacillin-HSA conjugate. Significant inhibition upon addition of both free piperacillin and piperacillin-HSA conjugate was detected by inhibition ELISA. These data suggest that piperacillin exposure in the workplace can induce occupational anaphylaxis and urticaria mediated by an interaction of IgE with the hapten of piperacillin.
Keywords: Anaphylaxis, Piperacillin, Occupational Diseases, IgE
INTRODUCTION
Piperacillin is an extended-spectrum beta-lactam antibiotic of the ureidopenicillin family. Piperacillin is widely used in conjunction with tazobactam, a beta-lactamase inhibitor. Some penicillins have been reported to cause occupational diseases, including bronchial asthma (1, 2), anaphylaxis (3), contact urticaria (4), contact dermatitis (5), and hypersensitivity pneumonitis (6), in pharmaceutical workers and health care professionals. Most of these penicillins belong to the benzylpenicillin or aminopenicillin family. Occupational contact urticaria and anaphylaxis induced by cephalosporins have often been reported (7). With regard to piperacillin, there is only one published report of occupational asthma, rhinitis, and urticaria in a pharmaceutical worker (1). However, to our knowledge, there has been no report of occupational anaphylaxis induced by piperacillin. Furthermore, no evidence of a serum IgE antibody response to piperacillin has been published. This is thus the first report of occupational anaphylaxis due to piperacillin and detection of a serum IgE response to a piperacillin-HSA conjugate.
CASE DESCRIPTION
The subject was a 24-yr-old female nurse who worked in the intensive care unit at a University Hospital. She had handled piperacillin/tazobactam without gloves or a mask since March 2003. Eighteen months later (October 2004), she experienced generalized urticaria with onset immediately and repeatedly after she had administered piperacillin. Nevertheless, she continued to work and finally experienced chest tightness, dizziness, sweating, generalized urticaria, abdominal pain, and diarrhea 10 min after giving a piperacillin injection in April 2005. Her blood pressure was 80/50 mmHg with a pulse rate of 104 beats/min. Her breath sounds were clear. The symptoms resolved completely after treatment with epinephrine, diphenhydramine, and methylprednisolone. She had a previous history of atopic dermatitis, and her hand eczema had become exacerbated after she had begun to work at the hospital.
Skin prick tests and measurement of serum total IgE
Skin prick tests using 80 common inhalant and food allergens (Bencard, Brentford, UK) were all negative. We did not perform a skin prick test with piperacillin/tazobactam because of the risk of anaphylaxis (8). Serum total IgE, measured using an immuno-CAP® system (Phadia, Uppsala, Sweden), was 283 IU/mL.
Assay of serum IgE and IgG levels
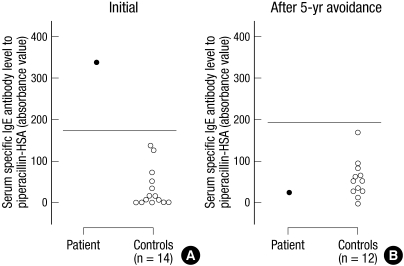
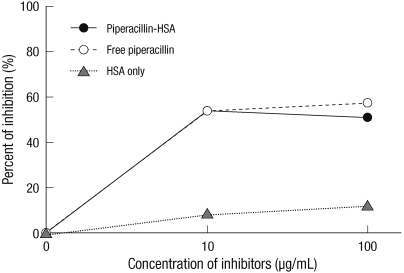
To assay piperacillin-specific serum IgE and IgG, we prepared piperacillin-human serum albumin (HSA) conjugates in our laboratory and performed an ELISA as described previously (11). Piperacillin-specific IgE and IgG levels in an initial serum sample and the IgE level in a serum sample obtained 5 yr later (May 2010) were measured. In brief, the wells of a 96-well ELISA microplate (Corning, New York, NY, USA) were coated by incubation with piperacillin-HSA conjugate at 10 µg/mL in phosphate-buffered saline (PBS) overnight at 4℃. After the wells were washed four times with 350 µL of PBS containing 0.05% Tween 20 (PBS-T; Sigma-Aldrich, St. Louis, MO, USA), nonspecific binding sites were blocked by incubation with 200 µL of 10% fetal bovine serum (FBS; GIBCO/Invitrogen, Carlsbad, CA, USA) in PBS at room temperature for 2 hr. After washing four times with 0.05% PBS-T, 50 µL of diluted serum (1:3) were added to each well, followed by incubation for 2 hr at 37℃. The plate was washed four times with 0.05% PBS-T, then 100 µL of goat anti-human IgE antibody (Kirkegaard & Perry Laboratories, Inc., Gaithersburg, MD, USA) diluted 1:1,000 with 10% FBS-PBS were added to each well, and the plate was incubated for 1 hr at room temperature. After washing four times with 0.05% PBS-T, 100 µL of alkaline phosphate-conjugated rabbit anti-goat IgG antibody (ReserveAPTM; Kirkegaard & Perry Laboratories) diluted 1:500 with 10% FBS-PBS were added to each well, and the plate was incubated for 1 hr at room temperature. PNPP (p-nitro-phenyl phosphate; Sigma-Aldrich) substrate was added, and the reaction was stopped by the addition of 1 N NaOH. The optical density of the solution in each well was measured at 405 nm using a microplate reader (Synergy HT; Bio-Tek, Winooski, VT, USA). The final absorbance value of piperacillin was determined by subtracting the absorbance value of a control crosslinker-HSA conjugate, which was obtained using a procedure identical to that described above, except that a crosslinker-HSA conjugate was used in place of piperacillin-HSA conjugate. The positive cutoff value was determined as the mean plus three standard deviations of the absorbance values in serum samples from 11 unexposed, non-atopic healthy controls. For the inhibition ELISA, increasing amounts (1-100 µg/mL) of free piperacillin, piperacillin-HSA conjugate, and HSA alone, dissolved in 10% FBS-PBS, were incubated with serum overnight, and an ELISA was performed as described above. The percentage inhibition was calculated as follows: % inhibition = (1 - absorbance with inhibitor/absorbance without inhibitor) × 100. For the ELISA of piperacillin-specific serum IgG levels, alkaline phosphate-conjugated rabbit anti-human IgG antibody (Kirkegaard & Perry Laboratories) was used instead of goat anti-human IgE antibody and alkaline phosphate-conjugated rabbit anti-goat IgG antibody. A high level of specific IgE antibody to piperacillin-HSA conjugate was detected in the initial serum sample from the subject; however, this had decreased markedly after 5 yr (Fig. 1). Significant inhibition by both free piperacillin and piperacillin-HSA conjugate occurred in a dose-dependent manner, with minimal inhibition by HSA alone (Fig. 2). High levels of piperacillin-HSA conjugate-specific IgG were also detected in the initial serum sample (data not shown).
Fig. 1.
Measurement of piperacillin specific IgE antibodies by inhibition ELISA. Levels of specific IgE to piperacillin-human serum albumin (HSA) conjugate in patient serum (•), collected at the initial visit (A) and after 5 yr' avoidance (B) and in sera from unexposed, non-atopic healthy control subjects (◦). Horizontal bars indicate the cut-off values (mean plus three standard deviations of the absorbance values of controls).
Fig. 2.
Effect of piperacillin-HSA conjugate (•), free piperacillin (◦), or HSA only (▴) in an inhibition ELISA. Both piperacillin-HSA conjugate and free piperacillin showed significant inhibition.
Based on these findings, the subject was diagnosed with occupational anaphylaxis and urticaria caused by piperacillin. The subject was transferred to a different department and has not again experienced anaphylaxis or urticaria.
DISCUSSION
Although we did not perform provocation and skin prick tests with piperacillin, we diagnosed this patient with occupational anaphylaxis because: 1) the temporal correlation between handling piperacillin and anaphylaxis; 2) a history of recurrent urticaria after handling piperacillin; and 3) detection of piperacillin-specific IgE in the serum. The complete disappearance of anaphylaxis and the reduction of serum IgE after avoidance of piperacillin further support this diagnosis. These findings suggest that occupational exposure to piperacillin induced IgE-mediated anaphylaxis in this subject.
Piperacillin can induce allergic reactions such as bronchial asthma, rhinitis (1), urticaria, anaphylaxis (9, 12), immune hemolytic anemia (10), maculopapular exanthem (13, 14), acute generalized exanthematous pulstulosis (15), and drug hypersensitivity syndrome (16). Several reports used skin prick, provocation, and serologic tests to demonstrate that piperacillin induced these reactions (1, 9, 10). A previous study reported that two of 311 tertiary hospital nurses showed a positive skin prick test to piperacillin (0.6%) (17). Two studies attempted to measure piperacillin-specific IgE levels in serum (1, 9). One involved a case of anaphylaxis, urticarial, and angioedema after intravenous piperacillin injection in an acute bronchitis patient, and the other was a case of occupational asthma, rhinitis, and urticaria induced by piperacillin powder exposure in a pharmaceutical worker. In those reports, a radioisotope test was used to detect IgE levels, but the assay failed. In the present study, we successfully detected piperacillin-HSA conjugate-specific serum IgE by ELISA in a patient with suspected piperacillin-induced occupational anaphylaxis. Furthermore, the binding specificity of the IgE was confirmed by inhibition ELISA. As significant inhibition by both free piperacillin and piperacillin-HSA conjugate was detected, it is likely that the hapten component of piperacillin is the antigenic determinant. High serum piperacillin-HSA conjugate-specific IgG levels were also detected in this patient, while levels in controls were minimal (data not shown). Although one study has sought to evaluate penicillin-specific IgG levels in the sera of patients with penicillin allergies, the significance of IgG levels remains unclear (18). Further studies are needed to investigate the role of specific IgG or its subclasses in occupational allergic diseases induced by piperacillin.
Nontherapeutic exposure to antibiotics, including penicillins, can occur by various routes (3). Contact with spilled drugs and inhalation of powder or foam are the most common routes. Exposure by the contact route usually induces contact urticaria (4), anaphylaxis (19), or dermatitis (5), whereas the inhalation route induces most commonly asthma or rhinitis (2, 20). Inhalation can also induce urticaria (1). Piperacillin, an intravenous antibiotic, is provided as a powder in a bottle and should be dissolved prior to administration. When dissolved, piperacillin develops little foam, but emits a more obvious odor than other intravenous antibiotics. The subject in the present report sometimes suffered from urticaria without direct contact with the solution, suggesting that inhalation of evaporated piperacillin may be the major route of sensitization. However, considering the reported exacerbation of hand eczema that occurred prior to the anaphylaxis, we speculate that exposure by direct contact with piperacillin solution may also have been a factor.
In conclusion, we report a case of a nurse with anaphylaxis and generalized urticaria caused by piperacillin and mediated by an interaction of IgE with the hapten of piperacillin. Sensitization was suspected to have occurred through inhalation of piperacillin vapor. Given that an ELISA was capable of detecting piperacillin-specific serum IgE, this system could be used for detecting piperacillin-HSA conjugate-specific IgE in the serum of occupational anaphylaxis or asymptomatic sensitized patients.
Footnotes
This study was supported by a grant of the Korea Science and Engineering Foundation (KOSEF) grant funded by the Korea government (MEST, 2009-0078646).
References
- 1.Moscato G, Galdi E, Scibilia J, Dellabianca A, Omodeo P, Vittadini G, Biscaldi GP. Occupational asthma, rhinitis and urticaria due to piperacillin sodium in a pharmaceutical worker. Eur Respir J. 1995;8:467–469. doi: 10.1183/09031936.95.08030467. [DOI] [PubMed] [Google Scholar]
- 2.Jiménez I, Antón E, Picáns I, Sánchez I, Quiñones MD, Jerez J. Occupational asthma specific to amoxicillin. Allergy. 1998;53:104–105. doi: 10.1111/j.1398-9995.1998.tb03784.x. [DOI] [PubMed] [Google Scholar]
- 3.Blanca M, Garcia J, Vega JM, Miranda A, Carmona MJ, Mayorga C, Moreno F, Juarez C. Anaphylaxis to penicillins after non-therapeutic exposure: an immunological investigation. Clin Exp Allergy. 1996;26:335–340. [PubMed] [Google Scholar]
- 4.Condé-Salazar L, Guimaraens D, González MA, Mancebo E. Occupational allergic contact urticaria from amoxicillin. Contact Dermatitis. 2001;45:109. doi: 10.1034/j.1600-0536.2001.045002109.x. [DOI] [PubMed] [Google Scholar]
- 5.Pecegueiro M. Occupational contact dermatitis from penicillin. Contact Dermatitis. 1990;23:190–191. doi: 10.1111/j.1600-0536.1990.tb04785.x. [DOI] [PubMed] [Google Scholar]
- 6.de Hoyos A, Holness DL, Tarlo SM. Hypersensitivity pneumonitis and airways hyperreactivity induced by occupational exposure to penicillin. Chest. 1993;103:303–304. doi: 10.1378/chest.103.1.303. [DOI] [PubMed] [Google Scholar]
- 7.Lee KH, Choi IS, Lee WJ, Kang SJ, Jeong HK. A case of cefotiam-contact anaphylaxis. Korean J Med. 2009;76(Suppl 1):S238–S242. [Google Scholar]
- 8.Weber-Mani U, Pichler WJ. Anaphylactic shock after intradermal testing with betalactam antibiotics. Allergy. 2008;63:785. doi: 10.1111/j.1398-9995.2008.01682.x. [DOI] [PubMed] [Google Scholar]
- 9.Romano A, Di Fonso M, Viola M, Adesi FB, Venuti A. Selective hypersensitivity to piperacillin. Allergy. 2000;55:787. doi: 10.1034/j.1398-9995.2000.00725.x. [DOI] [PubMed] [Google Scholar]
- 10.Leger RM, Arndt PA, Garratty G. Serological studies of piperacillin antibodies. Transfusion. 2008;48:2429–2434. doi: 10.1111/j.1537-2995.2008.01852.x. [DOI] [PubMed] [Google Scholar]
- 11.Suh YJ, Lee YM, Choi JH, Suh CH, Nahm DH, Park HS. Heterogeneity of IgE response to cefteram pivoxil was noted in 2 patients with cefteram-induced occupational asthma. J Allergy Clin Immunol. 2003;112:209–210. doi: 10.1067/mai.2003.1525. [DOI] [PubMed] [Google Scholar]
- 12.Rank MA, Park MA. Anaphylaxis to piperacillin-tazobactam despite a negative penicillin skin test. Allergy. 2007;62:964–965. doi: 10.1111/j.1398-9995.2007.01418.x. [DOI] [PubMed] [Google Scholar]
- 13.Romano A, Di Fonso M, Artesani MC, Viola M, Andriolo M, Pettinato R. Delayed hypersensitivity to piperacillin. Allergy. 2002;57:459. doi: 10.1034/j.1398-9995.2002.23612.x. [DOI] [PubMed] [Google Scholar]
- 14.Gaeta F, Alonzi C, Valluzzi RL, Viola M, Romano A. Delayed hypersensitivity to acylureidopenicillins: a case report. Allergy. 2008;63:787–789. doi: 10.1111/j.1398-9995.2008.01691.x. [DOI] [PubMed] [Google Scholar]
- 15.Grieco T, Cantisani C, Innocenzi D, Bottoni U, Calvieri S. Acute generalized exanthematous pustulosis caused by piperacillin/tazobactam. J Am Acad Dermatol. 2005;52:732–733. doi: 10.1016/j.jaad.2004.08.030. [DOI] [PubMed] [Google Scholar]
- 16.Fahim S, Jain V, Victor G, Pierscianowski T. Piperacillin-tazobactam-induced drug hypersensitivity syndrome. Cutis. 2006;77:353–357. [PubMed] [Google Scholar]
- 17.Choi IS, Han ER, Lim SW, Lim SR, Kim JN, Park SY, Chae SK, Lim HH, Seol YA, Bae YI, Won YH. Beta-lactam antibiotic sensitization and its relationship to allergic diseases in tertiary hospital nurses. Allergy Asthma Immunol Res. 2010;2:114–122. doi: 10.4168/aair.2010.2.2.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Torres MJ, Mayorga C, Pamies R, Rodriquez JL, Juarez C, Romano A, Blanca M. Immunologic response to different determinants of benzylpenicillin, amoxicillin, and ampicillin. Comparison between urticaria and anaphylactic shock. Allergy. 1999;54:936–943. doi: 10.1034/j.1398-9995.1999.00175.x. [DOI] [PubMed] [Google Scholar]
- 19.Kim JE, Kim SH, Choi GS, Ye YM, Park HS. Detection of specific IgE antibodies to cefotiam-HSA conjugate by ELISA in a nurse with occupational anaphylaxis. Allergy. 2010;65:791–792. doi: 10.1111/j.1398-9995.2009.02229.x. [DOI] [PubMed] [Google Scholar]
- 20.Pala G, Pignatti P, Perfetti L, Cosentino R, Moscato G. Occupational asthma and rhinitis induced by a cephalosporin intermediate product: description of a case. Allergy. 2009;64:1390–1391. doi: 10.1111/j.1398-9995.2009.02062.x. [DOI] [PubMed] [Google Scholar]