Abstract
The mechanisms underlying the relationship between health literacy, numeracy, and glycemic control are unclear. We explored the role of self-efficacy in the predicted pathway linking health literacy and numeracy to glycemic control (A1C). Adults with type 1 or type 2 diabetes mellitus (N=383) were enrolled in a cross-sectional study at primary care and diabetes clinics at three medical centers. Data collected included demographic information, health literacy, general numeracy, and A1C. Path analytic models estimated relations among health literacy, numeracy, and self-efficacy as predictors of A1C. Health literacy (r=0.14, p<0.01) and numeracy skills (r=0.17, p<0.001) were each associated with greater self-efficacy; and greater diabetes self-efficacy was associated with lower A1C levels (r=−0.25, p<001). When considered in combination, numeracy was related to self-efficacy (r=0.13, p<0.05) and the effect of health literacy on self-efficacy was reduced to non-significance (r=0.06, p=0.30). Health literacy and numeracy are each associated with greater diabetes self-efficacy; and greater diabetes self-efficacy is associated with lower A1C levels. Diabetes self-efficacy may be an important target of interventions to improve diabetes control and promote health equity related to health literacy and general numeracy skills needed for diabetes management.
Keywords: Health Literacy, Numeracy, Self-efficacy, Diabetes, Glycemic Control
Limited health literacy and numeracy skills are common in patients with diabetes and have been associated with less diabetes knowledge and worse glycemic control (Cavanaugh et al., 2008; DeWalt, Berkman, Sheridan, Lohr, & Pignone, 2004). Health literacy and numeracy skills are important in successfully executing the complex recommendations related to diabetes self-care, including glucose monitoring, dietary intake modification, and medication administration. However, there is limited understanding regarding the pathways, or possible mechanisms, through which health literacy and numeracy influence diabetes outcomes.
Self-efficacy, a person’s confidence in their ability to perform a goal-directed behavior (Bandura, 1977; Wallston, 1989), has been associated with self-care behaviors and glycemic control in patients with diabetes (Wallston, Rothman, & Cherrington, 2007). Health literacy has predicted self-efficacy in other chronic conditions, such as HIV, hormone therapy, and asthma (Mancuso & Rincon, 2006; Torres & Marks, 2009; Wolf et al., 2007). Numeracy level has been shown to predict self-efficacy in asthma (Apter et al., 2009). While both self-efficacy to manage one’s diabetes and health literacy or numeracy skill have been related to glycemic control (Cavanaugh et al., 2008; Sarkar & Schillinger, 2008), the pathways through which these factors relate to each other and, in turn, impact glycemic control remains unknown.
The objectives of this study are to describe the association between health literacy, numeracy, and diabetes self-efficacy (i.e., one’s perceived ability to self-manage diabetes) in patients with type 1 and type 2 diabetes. We also examine the predicted pathway linking health literacy, numeracy, and diabetes self-efficacy to glycemic control.
Method
Setting and study participants
From March 2004 until November 2005, study participants were enrolled in a cross-sectional study from two primary care clinics and two diabetes specialty clinics located at three medical centers in Chapel Hill, North Carolina and Nashville, Tennessee. These clinics serve patients from urban, rural, and suburban areas that are heterogeneous with respect to age, race/ethnicity, education, and income. Inclusion criteria were a diagnosis of type 1 or type 2 diabetes mellitus, age 18 to 85 years, and English-speaking. Exclusion criteria were a previous diagnosis of dementia, psychosis or blindness. In addition, patients with a corrected visual acuity of 20/50 or worse using a Rosenbaum Screener (Prestige Medical, Northridge, CA) were excluded. Participants received $20 for participation. The Veterans Affairs Tennessee Valley Healthcare System Research & Development Committee and Institutional Review Boards at Vanderbilt University Medical Center and the University of North Carolina at Chapel Hill approved this study. Written consent was obtained from all participants.
Data and procedure
Trained research assistants collected data from participating patients and from the patient’s medical record. Information gathered included patient demographics, health literacy, numeracy, and perceived diabetes self-efficacy. Clinical information included the use of insulin, diabetes type, years of diagnosed diabetes, and glycemic control.
Measures
Health literacy and numeracy
Health literacy was assessed using the Rapid Estimate of Adult Literacy in Medicine (REALM), a valid and widely used measure of health literacy (Davis et al., 1991; Davis et al., 1993). If a patient scored less than a 6th grade reading level by the REALM, then the remainder of the instruments were administered orally to ensure that the content of the survey questions were understood by the patient. Numeracy was measured with the math section of the Wide Range Achievement Test, 3rd Edition (WRAT-3R), a valid measure of calculation skills (Wilkinson, 1993). The WRAT-3R is a valid and widely used measure of general numeracy and was selected because a valid measure of general health numeracy was unavailable when this study was designed. We also measured diabetes-specific numeracy in this study, and have reported elsewhere its association with self-efficacy and A1C (Cavanaugh et al., 2008).
Diabetes self-efficacy
Diabetes self-efficacy was assessed using the 8-item Perceived Diabetes Self-Management Scale (PDSMS) (Wallston et al., 2007). Response options are in Likert format ranging from 1=“Strongly Disagree” to 5=“Strongly Agree.” Items are summed to produce a score ranging from 8 to 40, with higher scores indicating more confidence in diabetes self-care. Cronbach’s alpha for the PDSMS was 0.83.
Glycemic control
Glycemic control was assessed by the most recent hemoglobin A1C (A1C) value in the patient’s medical record; 96% were obtained within 6-months of the subject evaluation and the median time between A1C and evaluation was 15-days (range: 0 to 323 days).
Statistical analyses
A series of path analytic models were performed using AMOS, version 17; a structural equation modeling program. Path analysis allows the simultaneous modeling of related regression relationships. It also allows a variable to be a dependent variable in one relationship and an independent variable in another. Structural equation model (SEM) packages are commonly used in lieu of stand-alone path analysis programs because SEM software provides generality and flexibility of model specification, the ability to assess model fit of the hypothesized model to the observed data. We relied on the comparative fit index (CFI) and root mean error of approximation (RMSEA) to assess model fit. CFI values that exceed 0.90 and RMSEA values below 0.08 indicate acceptable model fit; and RMSEA values close to 0.06 have been designated as indicative of “good fit” (Kline, 2004).
Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients. A path coefficient is a standardized regression coefficient (beta) showing the direct effect of one variable on another variable. When there are two or more variables, the path coefficient reflects the effect of one variable controlling for all other variables. Path coefficients may be decomposed into direct and indirect effects, corresponding to direct and indirect arrows in a path model. In this study, a direct effect occurs when variable B (self-efficacy) is significantly related to variable C (A1C), whereas an indirect effect occurs when variable A (health literacy or numeracy) is also related to variable B (self-efficacy) and a part of this relationship is transmitted to variable C (A1C) (i.e., a part of A’s “direct effect” on variable C is due to relations between A and B).
The path models were estimated with a correlation matrix generated by 383 cases; a sample size considered to provide adequate power to detect large effects (Kline, 2004; MacCallum, Browne, & Sugawara, 1996). Model 1 tested whether health literacy had a direct effect on A1C after controlling for age, gender, race, years of education, annual income, insulin use, diabetes type, and years of diagnosed diabetes. Next, to test for an indirect effect of health literacy on A1C, significant predictors of A1C in model 1 were retained, and diabetes self-efficacy was introduced into the pathway between health literacy and A1C. Model 2 tested whether numeracy had a direct effect on A1C after controlling for age, gender, race, years of education, annual income, insulin use, diabetes type, and years of diagnosed diabetes. To test for an indirect effect of numeracy on A1C, significant predictors of A1C in model 2 were retained, and the model was re-run with diabetes self-efficacy introduced into the pathway between numeracy and A1C. Model 3 included both health literacy and numeracy in the same model, and diabetes self-efficacy was introduced into the predicted pathway linking both health literacy and numeracy with A1C.
Results
Participant characteristics
A total of 615 patients were referred for possible enrollment. Of these, 191 refused participation and 18 were excluded due to: poor vision (n=7), age (n=4), non-English speaking (n=2), or other exclusion criteria (n=5). Of 406 patients who consented, 398 (98%) completed the study. Patients self-reporting White or African American race (n=383) were included in our analyses. Characteristics of these patients are presented in Table 1. The mean age (SD) was 54 (13) years; 50% were female, and 65% were White. Eight percent of the patients reported having less than a 9th grade education level, 56% had greater than a high school level education, 31% had less than 9th grade level health literacy skills, and 69% had less than 9th grade level numeracy skills. The majority of the patients (62%) were on insulin, and the mean (SD) A1C was 7.6% (1.7%).
Table 1.
Characteristics of study population by health literacy and numeracy grade level
| Characteristics | M ± SD or n (%) |
Health Literacy (REALM) | Numeracy (WRAT-3R) | ||||
|---|---|---|---|---|---|---|---|
| ≤9th grade | ≥9th grade | p-value† | ≤9th grade | ≥9th grade | p-value† | ||
| N | 383 | 120 | 263 | 266 | 117 | ||
| Age (years) | 54.4 ± 13.0 | 55.6 ± 10.7 | 53.8 ± 13.9 | 0.15 | 55.2 ± 12.9 | 52.5 ± 13.1 | 0.07 |
| Female | 193 (50) | 56 (47) | 137 (52) | 0.38 | 139 (52) | 54 (46) | 0.16 |
| Race | |||||||
| White | 249 (65) | 45 (37) | 204 (78) | p<0.0001 | 147 (55) | 102 (87) | p<0.0001 |
| Nonwhite | 134 (35) | 75 (63) | 59 (22) | 119 (45) | 15 (13) | ||
| Income | |||||||
| <$20,000 | 166 (44) | 84 (73) | 82 (31) | p<0.0001 | 142 (55) | 24 (21) | p<0.0001 |
| ≥$20,000 | 209 (56) | 31 (27) | 178 (69) | 117 (45) | 92 (79) | ||
| Education | |||||||
| ≤9th grade | 32 (8) | 23 (19) | 9 (3) | p<0.0001 | 31 (12) | 1 (1) | p<0.0001 |
| 10th grade - High School/GED | 135 (35) | 65 (54) | 70 (27) | 120 (45) | 15 (13%) | ||
| >High School/GED | 216 (57) | 32 (27) | 184 (70) | 115 (43) | 101 (86) | ||
| Private Insurance (% yes) | 185 (48) | 36 (30) | 149 (57) | p<0.0001 | 108 (41) | 77 (66) | p<0.0001 |
| Diabetes: Type 2 (% yes) | 327 (85) | 111 (93) | 216 (82) | p<0.01 | 242 (91) | 85 (73) | p<0.0001 |
| Years of diabetes | 11.3 ± 9.5 | 11.1 ± 9.4 | 11.4 ± 9.6 | 0.79 | 11.1 ± 9.2 | 12.0 ± 10.3 | 0.40 |
| Insulin use (% yes) | 236 (62) | 151 (71) | 57 (57) | p<0.01 | 166 (62) | 70 (60) | 0.36 |
| BMI (kg/m2) | 33.6 ± 8.1 | 34.1 ± 8.0 | 33.4 ± 8.2 | 0.45 | 33.7 ± 8.1 | 33.4 ± 8.4 | 0.76 |
| Hemoglobin A1c (%) | 7.6 ± 1.7 | 7.7 ± 1.6 | 7.5 ± 1.7 | 0.36 | 7.7 ± 1.7 | 7.5 ± 1.6 | 0.28 |
Note: Chi-square and independent samples t-tests comparing across health literacy and numeracy grade level. REALM=Rapid Estimate of Adult Literacy in Medicine Health literacy); WRAT-3R=Wide Range Achievement Test-3rd edition (General numeracy); BMI=Body Mass Index.
Test of path analytic models
Model 1 included nine predictor variables: age, gender, race (White or African American), years of education, annual income, insulin use (no or yes), diabetes type (1 or 2), years of diagnosed diabetes, health literacy, and one outcome variable: A1C. Examination of the path coefficients in this model suggested that younger age (r=−0.21, p<0.001), using insulin (r=0.26, p<0.001), having been diagnosed with diabetes for more years (r=0.16, p<0.01), and African American race (r=0.12, p<0.01) had a direct effect on higher A1C levels, accounting for 17% of the variability in A1C. Health literacy did not have a direct effect on A1C levels (r=−0.02, ns).
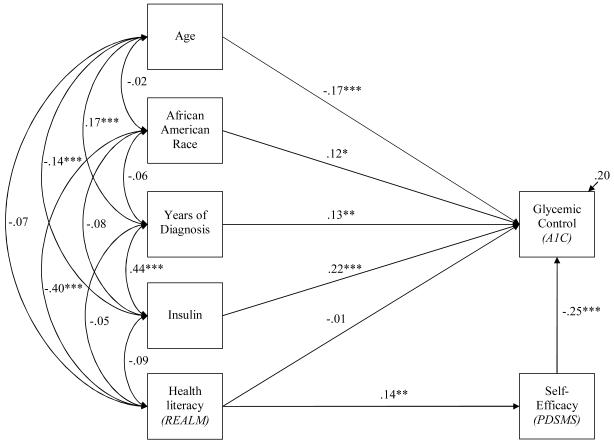
A refined version of model 1 (See Figure 1) was evaluated that included all significant predictors of A1C from the original model 1, the non-significant pathway from health literacy to A1C, and introduced self-efficacy into the predicted pathway between health literacy and A1C. Examination of the path coefficients suggested that the direct effects of younger age (r=−0.17, p<0.001), using insulin (r=0.22, p<0.001), having been diagnosed with diabetes for more years (r=0.13, p<0.01), and African American race (r=0.12, p<0.05) on higher A1C levels remained. Health literacy had a direct effect on diabetes self-efficacy (r=0.14, p<0.01), and greater diabetes self-efficacy had a direct effect on lower A1C levels (r=−0.25, p<001). Although health literacy did not have a direct effect on A1C, it had an indirect effect on A1C through its relationship with diabetes self-efficacy (indirect effect on A1C, r=−0.04). The estimated model accounted for 20% of variability in A1C. As indicated in Figure 1, this model showed excellent data fit, χ2 (4, N=383)=6.88, p=0.14, CFI=0.99, RMSEA=0.04 (90% CI: 0.00 – 0.10).
Figure 1.
Health literacy is directly associated with self-efficacy, and indirectly associated with glycemic control.
Note: REALM=Rapid Estimate of Adult Literacy in Medicine; PDSMS=Perceived Diabetes Self-Management Scale. Overall model fit, χ2 (4, N=383)=6.88, p=0.14, CFI=0.99, RMSEA=0.04 (90% CI: 0.00 - 0.10). Coefficients are standardized path coefficients, *p<.05, **p<.01, and ***p<.001. The squared multiple correlation coefficient is presented for A1C.
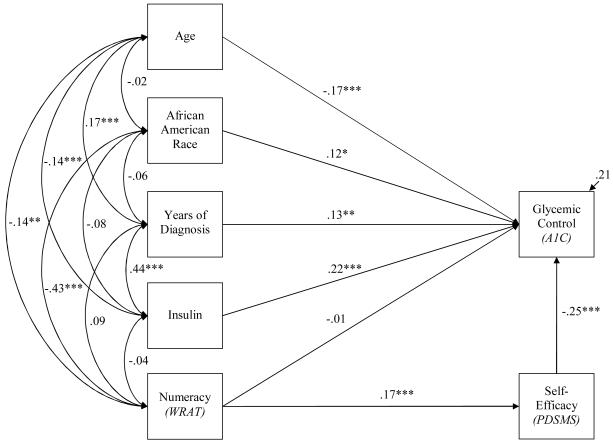
Model 2 included the same nine predictor variables as model 1, except numeracy was substituted for health literacy, and one outcome variable: A1C. Examination of the path coefficients similarly suggested that younger age, using insulin, having been diagnosed with diabetes for more years, and African American race had a direct effect on higher A1C levels, accounting for 17% of the variability in A1C. Numeracy did not have a direct effect on A1C levels (r=−0.01, ns).
A refined version of model 2 (Figure 2) that included all significant predictors of A1C in the initial model 2, the non-significant pathway from numeracy to A1C, and introduced self-efficacy into the predicted pathway between health literacy and A1C was then evaluated. Examination of the path coefficients suggested that the direct effects of younger age (r=−0.17, p<0.001), using insulin (r=0.22, p<0.001), having been diagnosed with diabetes for more years (r=0.13, p<0.01), and African American race (r=0.12, p<0.05) on higher A1C levels remained. Numeracy had a direct effect on greater diabetes self-efficacy (r=0.17, p<0.001), and greater diabetes self-efficacy had a direct effect on lower A1C levels (r=−0.25, p<001). Thus, as with health literacy, numeracy had an indirect effect on A1C through its relationship with diabetes self-efficacy (indirect effect on A1C, r=−0.04). The estimated model accounted for 21% of variability in A1C. As indicated in Figure 2, this model showed excellent data fit, χ2 (4, N=383)=6.75, p=0.15, CFI=0.99, RMSEA=0.04 (90% CI: 0.00 - 0.10).
Figure 2.
Numeracy is directly associated with self-efficacy, and indirectly associated with glycemic control.
Note: WRAT=Wide Range Achievement Test; PDSMS=Perceived Diabetes Self-Management Scale. Overall model fit, χ2 (4, N=383)=6.75, p=0.15, CFI=0.99, RMSEA=0.04 (90% CI: 0.00 - 0.10). Coefficients are standardized path coefficients, *p<.05, **p<.01, and ***p<.001. The squared multiple correlation coefficient is presented for A1C.
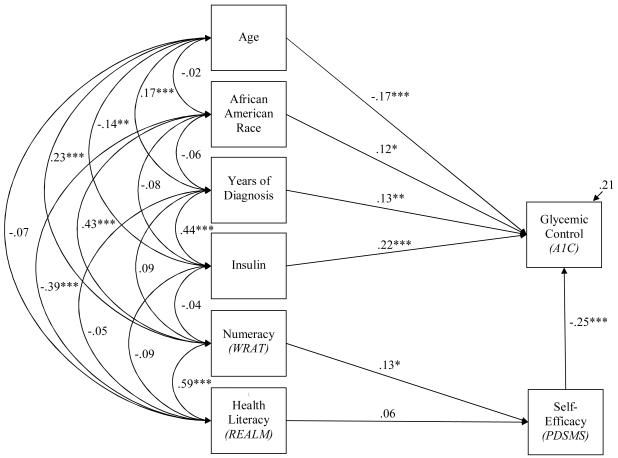
Model 3 (Figure 3) included all significant predictors of A1C from prior models (i.e., age, insulin, years of diagnosed diabetes, and race), health literacy and numeracy as predictors of diabetes self-efficacy, and diabetes self-efficacy as an additional predictor of A1C. Examination of the path coefficients in this model suggested that younger age (r=−0.17, p<0.001), using insulin (r=0.22, p<0.001), having been diagnosed with diabetes for more years (r=0.16, p<0.01), and African American race (r=0.12, p<0.01) each had a direct effect on higher A1C levels. When numeracy and health literacy were included in the same model, health literacy no longer had a direct effect on diabetes self-efficacy (r=0.06, p=0.30). Rather, numeracy maintained the direct effect on diabetes self-efficacy (r=0.13, p<0.05); and, consistent with the previous models, greater diabetes self-efficacy had a direct effect on lower A1C levels (r=−0.25, p<0.001). The estimated model accounted for 21% of variability in A1C. As indicated in Figure 3, this model showed excellent data fit, χ2 (4, N=383) = 6.17, p=0.41, CFI =1.00, RMSEA=0.01 (90% CI: 0.00 - 0.07).
Figure 3.
Numeracy, but not health literacy, is directly associated with self-efficacy, and indirectly associated with glycemic control.
Note: REALM=Rapid Estimate of Adult Literacy in Medicine; WRAT=Wide Range Achievement Test; PDSMS=Perceived Diabetes Self-Management Scale. Overall model fit, χ2 (4, N=383)=6.17, p =0 .41, CFI=1.00, RMSEA=0.01 (90% CI: 0.00 - 0.07). Coefficients are standardized path coefficients, *p<.05, **p<.01, and ***p<.001. The squared multiple correlation coefficient is presented for A1C.
Discussion
Our study shows that, when considered in isolation, health literacy and numeracy skills are each associated with greater diabetes self-efficacy, and greater diabetes self-efficacy is associated with lower A1C levels. When considered in combination, numeracy is more strongly associated with diabetes self-efficacy than health literacy. Although neither health literacy nor numeracy were directly related to glycemic control after adjustment for potential confounding variables, our analyses support the presence of an indirect effect for each objective skill assessment on glycemic control through an association with diabetes self-efficacy. This finding suggests that self-efficacy may be an appropriate target of directed diabetes educational interventions, especially for patients with low health literacy or numeracy skills.
According to Baron and Kenny (1986), three assumptions must be met for mediation: (1) there is a relationship between predictor and criterion, (2) a relationship between mediator and criterion, and (3) a relationship between predictor and mediator (Baron & Kenny, 1986). Our results support assumptions 2 and 3, but not 1. The predictors (health literacy and numeracy) were not associated with criterion (A1C). Mediation occurs when the mediator (self-efficacy) accounts for the relationship between two variables (i.e., health literacy and A1C or numeracy and A1C) by reducing their relationship to non significance. Because there was no relationship between predictor and criterion to begin with, our findings do not suggest self-efficacy mediates the association between health literacy and A1C or numeracy and A1C. Rather, our findings suggest that when considered in isolation, both health literacy and numeracy have an indirect effect on A1C through an association with self-efficacy and when considered in combination, only numeracy has an indirect effect on A1C.
There have been several studies exploring the relationship between health literacy and diabetes self-efficacy, and glycemic control and they have demonstrated mixed results (DeWalt, Boone, & Pignone, 2007; Gerber et al., 2005; Ishikawa, Takeuchi, & Yano, 2008; Sarkar, Fisher, & Schillinger, 2006). Health literacy has not been shown to have an association with diabetes self-efficacy except in one study which used a non-traditional measure of health literacy (Ishikawa et al., 2008). In earlier work, we reported a relationship between diabetes-related numeracy and diabetes self-efficacy (Cavanaugh et al., 2008). In the current analysis, we report a significant relationship between health literacy and self-efficacy, and between general numeracy and self-efficacy. Interestingly, it is numeracy that is more closely related to diabetes self-efficacy than health literacy. This may be due to the high burden of quantitative tasks that are often required by patients with diabetes to execute daily self-care. If health literacy is a precursor to knowledge and numeracy reflects applied knowledge, then it is not surprising that numeracy skills may be more strongly associated with one’s confidence in managing their diabetes.
The variability in the findings for the association between health literacy and diabetes self-efficacy between previous studies and ours may be because self-efficacy was measured differently in each study. The PDSMS measure employed in our study represents an overall assessment of self-efficacy of diabetes self-care that is not driven by specific self-care behaviors. This may allow for a patient to express a global view of their self-efficacy related to diabetes self-care, rather than a summation of separate efficacy judgments for carrying out different individual tasks such as glucose monitoring, dietary adherence, foot care, and medication adherence.
To date, self-efficacy has not been examined in the predicted pathway linking health literacy and general numeracy to patient outcomes. Only one previous study described the role of self-efficacy as a partial mediator in the relationship between numeracy and asthma quality of life (Apter et al., 2009). Thus, to our knowledge, this is the first study to show that health literacy and numeracy are indirectly related to glycemic control through diabetes self-efficacy. Self-efficacy includes the application of diabetes-care knowledge, and may be more proximal to patient behavior. Health literacy and numeracy have both been associated with diabetes knowledge, although knowledge itself is often not associated with glycemic control (Cavanaugh et al., 2008; Rothman et al., 2005); thus, because self-efficacy may be considered more closely related to actual execution of diabetes self-management behaviors, it is not surprising that it may be more strongly predictive of glycemic control than either health literacy or numeracy.
Although health literacy has been reported to be significantly associated with glycemic control (Schillinger et al., 2002), there have been several studies that have not demonstrated a direct relationship (Cavanaugh et al., 2008; Morris, MacLean, & Littenberg, 2006; Ross, Frier, Kelnar, & Deary, 2001; Rothman, DeWalt et al., 2004; Rothman, Malone et al., 2004; Williams, Baker, Parker, & Nurss, 1998). In a small underpowered study, Williams et al. found that A1C levels were somewhat higher among those with lower health literacy than those with higher health literacy, but the difference was not statistically significant, and they did not perform adjusted analyses (Williams et al., 1998). Morris et al. adjusted for sociodemographic characteristics, duration of diabetes, diabetes education, depression, alcohol use, and medications use, and did not find a significant association between health literacy and glycemic control (Morris et al., 2006). In our earlier analyses, health literacy and general numeracy were not significantly associated with glycemic control, but diabetes-specific numeracy did have a significant relationship (Cavanaugh et al., 2008). We theorize that diabetes-related numeracy skills are more specific to diabetes self-management activities, and therefore are more strongly associated with glycemic control than are health literacy or even general numeracy skills. Upon further examination in the current path analysis, we demonstrated that diabetes self-efficacy forms an indirect pathway between health literacy, general numeracy and glycemic control; when considered in combination, numeracy has the sole indirect effect and actually mediates the relationship between health literacy and self-efficacy.
Several study limitations should be acknowledged. First, the cross-sectional design only describes associations; therefore, no conclusions regarding causation can be made. Longitudinal cohort studies to determine the role of health literacy, numeracy, and self-efficacy in diabetes care are needed. Secondly, although our path analytic models adjusted for many potential confounding variables, there remains the possibility of residual confounding. Thirdly, it is also possible that the REALM, while well validated and considered one of the primary evaluations in health literacy research, lacks the precision at higher levels of literacy needed for a detailed analysis of the literacy-glycemic control relationship. Finally, this study did not include non-English speaking participants who may be at high risk for low health literacy, low numeracy, low diabetes self-efficacy, and poor glycemic control.
Conclusion
Diabetes self-efficacy is important in promoting effective diabetes self-management behaviors and ultimately to optimize diabetes care. For patients with diabetes who have low health literacy and/or numeracy skills, consideration of efforts to improve self-efficacy and patient empowerment should be included in the delivery of clinical recommendations as well as diabetes patient education. Additional research is needed to develop and determine successful strategies to promote health equity related to health literacy and numeracy in patients with diabetes.
Our initial finding of a significant association between health literacy, self-efficacy and glycemic control in diabetes is important as it suggests that diabetes self-efficacy should be considered in diabetes management programs – especially those for patients with limited health literacy or numeracy skills. Previously described intervention strategies have focused on other potential pathways between health literacy and health outcomes, such as simplifying health education materials to improve patients’ knowledge of their illness, or providing general care management support (Clement, Ibrahim, Crichton, Wolf, & Rowlands, 2009). Along with enhanced knowledge and motivation, patients with diabetes need behavioral skills, and the confidence that accompanies such skills, to overcome the barriers imposed by low levels of health literacy and, likely, numeracy (Osborn, 2006). In addition to materials designed with clear communication principles, programs including materials and training to encourage skill-building and mastery, such as diabetes self-management literacy and numeracy sensitive worksheets to practice reading a food label, designing a meal plan or reinforcing medication recommendations, may address these barriers and result in improved diabetes self-care self-efficacy (Wolff et al., 2009). Given the consistent association between self-efficacy and glycemic control, this comprehensive and interactive approach may be utilized throughout the course of diabetes care as a strategy to improve diabetes self-efficacy, behaviors, and outcomes for all patients.
Acknowledgements
This research was funded with support from the American Diabetes Association (Novo Nordisk Clinical Research Award), the Pfizer Clear Health Communication Initiative, and the Vanderbilt Diabetes Research and Training Center (NIDDK P60 DK020593). Dr. Osborn is supported by an NIH Diversity Supplement Award (NIDDK P60 DK020593-30S2). Dr. Cavanaugh is supported by a National Kidney Foundation Young Investigator Grant and also by NIH NIDDK K23 DK080951. Dr. Rothman is also currently supported by an NIDDK Career Development Award (NIDDK K23 DK065294).
References
- Apter AJ, Wang X, Bogen D, Bennett IM, Jennings RM, Garcia L, et al. Linking numeracy and asthma-related quality of life. Patient Education and Counseling. 2009 doi: 10.1016/j.pec.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychological Review. 1977;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Cavanaugh K, Huizinga MM, Wallston KA, Gebretsadik T, Shintani A, Davis D, et al. Association of numeracy and diabetes control. Annals of Internal Medicine. 2008;148(10):737–746. doi: 10.7326/0003-4819-148-10-200805200-00006. [DOI] [PubMed] [Google Scholar]
- Clement S, Ibrahim S, Crichton N, Wolf M, Rowlands G. Complex interventions to improve the health of people with limited literacy: A systematic review. Patient Education and Counseling. 2009;75(3):340–351. doi: 10.1016/j.pec.2009.01.008. [DOI] [PubMed] [Google Scholar]
- Davis TC, Crouch MA, Long SW, Jackson RH, Bates P, George RB, et al. Rapid assessment of literacy levels of adult primary care patients. Family Medicine. 1991;23(6):433–435. [PubMed] [Google Scholar]
- Davis TC, Long SW, Jackson RH, Mayeaux EJ, George RB, Murphy PW, et al. Rapid estimate of adult literacy in medicine: a shortened screening instrument. Family Medicine. 1993;25(6):391–395. [PubMed] [Google Scholar]
- DeWalt DA, Berkman ND, Sheridan S, Lohr KN, Pignone MP. Literacy and health outcomes: a systematic review of the literature. Journal of General Internal Medicine. 2004;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. American Journal of Health Behavior. 2007;31(Suppl 1):S27–35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- Gerber BS, Brodsky IG, Lawless KA, Smolin LI, Arozullah AM, Smith EV, et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care. 2005;28(7):1574–1580. doi: 10.2337/diacare.28.7.1574. [DOI] [PubMed] [Google Scholar]
- Ishikawa H, Takeuchi T, Yano E. Measuring functional, communicative, and critical health literacy among diabetic patients. Diabetes Care. 2008;31(5):874–879. doi: 10.2337/dc07-1932. [DOI] [PubMed] [Google Scholar]
- Mancuso CA, Rincon M. Impact of health literacy on longitudinal asthma outcomes. Journal of General Internal Medicine. 2006;21(8):813–817. doi: 10.1111/j.1525-1497.2006.00528.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morris NS, MacLean CD, Littenberg B. Literacy and health outcomes: a cross-sectional study in 1002 adults with diabetes. BMC Family Practice. 2006;7:49. doi: 10.1186/1471-2296-7-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY. Using the IMB model of health behavior change to promote self-management behaviors in Puerto Ricans with diabetes. Dissertation Abstracts International Section A: Humanities and Social Sciences. 2006;67(6-A):2064. [Google Scholar]
- Ross LA, Frier BM, Kelnar CJ, Deary IJ. Child and parental mental ability and glycaemic control in children with Type 1 diabetes. Diabetic Medicine. 2001;18(5):364–369. doi: 10.1046/j.1464-5491.2001.00468.x. [DOI] [PubMed] [Google Scholar]
- Rothman RL, DeWalt DA, Malone R, Bryant B, Shintani A, Crigler B, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. Journal of the American Medical Association. 2004;292(14):1711–1716. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- Rothman RL, Malone R, Bryant B, Horlen C, DeWalt D, Pignone M. The relationship between literacy and glycemic control in a diabetes disease-management program. Diabetes Educator. 2004;30(2):263–273. doi: 10.1177/014572170403000219. [DOI] [PubMed] [Google Scholar]
- Rothman RL, Malone R, Bryant B, Wolfe C, Padgett P, DeWalt DA, et al. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. Diabetes Educator. 2005;31(2):215–224. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- Sarkar U, Fisher L, Schillinger D. Is self-efficacy associated with diabetes self-management across race/ethnicity and health literacy? Diabetes Care. 2006;29(4):823–829. doi: 10.2337/diacare.29.04.06.dc05-1615. [DOI] [PubMed] [Google Scholar]
- Sarkar U, Schillinger D. Does lower diabetes-related numeracy lead to increased risk for hypoglycemic events? Annals of Internal Medicine. 2008;149(8):594. doi: 10.7326/0003-4819-149-8-200810210-00018. author reply 594. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, Wang F, Osmond D, Daher C, et al. Association of health literacy with diabetes outcomes. Journal of the American Medical Association. 2002;288(4):475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Torres RY, Marks R. Relationships among health literacy, knowledge about hormone therapy, self-efficacy, and decision-making among postmenopausal health. Journal of Health Communication. 2009;14(1):43–55. doi: 10.1080/10810730802592247. [DOI] [PubMed] [Google Scholar]
- Wallston KA. Assessment of control in health-care settings. Wiley; Chichester, England: 1989. [Google Scholar]
- Wallston KA, Rothman RL, Cherrington A. Psychometric properties of the Perceived Diabetes Self-Management Scale (PDSMS) Journal of Behavioral Medicine. 2007;30(5):395–401. doi: 10.1007/s10865-007-9110-y. [DOI] [PubMed] [Google Scholar]
- Wilkinson GS. WRAT3: Wide Range Achievement Test Administration Manual. Wide Range, Inc.; Wilmington, DE: 1993. [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients’ knowledge of their chronic disease. A study of patients with hypertension and diabetes. Archives of Internal Medicine. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Davis TC, Osborn CY, Skripkauskas S, Bennett CL, Makoul G. Literacy, self-efficacy, and HIV medication adherence. Patient Education and Counseling. 2007;65(2):253–260. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- Wolff K, Cavanaugh K, Malone R, Hawk V, Gregory BP, Davis D, et al. The Diabetes Literacy and Numeracy Education Toolkit (DLNET): materials to facilitate diabetes education and management in patients with low literacy and numeracy skills. Diabetes Educator. 2009;35(2):233–236. 238–241, 244–235. doi: 10.1177/0145721709331945. [DOI] [PMC free article] [PubMed] [Google Scholar]