Abstract
In debates over access to essential medical care, comparatively little attention has been paid to the provision of outpatient physiotherapy services. We examined physiotherapy utilization for musculoskeletal disorders (MSDs) among approximately 2,000 employees of a large, unionized, Ontario workplace. We obtained MSD-related physiotherapy claims and service data from the public Workplace Safety and Insurance Board, two private medical insurance carriers, a workplace special fund starting in 1995 and a workplace-contracted, on-site physiotherapy clinic starting in 1999. We observed substantial increases in overall physiotherapy utilization for MSDs: a median of 234 services per quarter for 1992–1994 to 1,281 for 1999–2002. With inclusive workplace provision policies, most physiotherapy utilization occurred on-site by 1999–2002 (70%). With a user-pay orientation to outpatient physiotherapy services increasing among working-age adults in Ontario, there is substantial potential for unequal access among those not privately insured or in workplaces with direct service provision.
Abstract
Dans les débats sur l'accès aux soins de santé essentiels, on porte comparativement peu d'attention à la prestation de services de physiothérapie pour les patients externes. Nous avons étudié l'utilisation de services de physiothérapie pour les troubles musculosquelettiques (TMS) chez environ 2,000 employés d'un grand milieu de travail syndiqué, en Ontario. Nous avons consulté les données sur les services et les réclamations relatives aux soins de physiothérapie provenant d'un organisme public – la Commission de la sécurité professionnelle et de l'assurance contre les accidents du travail – et de deux sociétés privées d'assurance médicale, soit un fonds spécial en milieu de travail qui existe depuis 1995 et une clinique de physiothérapie sur les lieux de travail qui existe depuis 1999. Nous avons observé une augmentation substantielle de l'utilisation générale des services de physiothérapie pour les TMS : une médiane de 234 services par trimestre pour la période 1992–1994 et de 1,281 services pour la période 1999–2002. Avec des politiques éclairées de prestation de services en milieu de travail, la majeure partie de l'utilisation des services de physiothérapie a eu lieu sur place pour la période 1999–2002 (70 %). Avec l'accroissement des politiques d'utilisateur-payeur pour les services externes de physiothérapie chez les adultes ontariens en âge de travailler, il existe un véritable potentiel d'inégalité d'accès chez ceux qui n'ont pas d'assurance privée ou qui ne bénéficient pas de prestation de services directs en milieu de travail.
Issues associated with parallel systems of public healthcare financing (e.g., workers' compensation board benefits and provincial health insurance plans) have recently received considerable attention (Leatt 2008). Private insurance has received less (Bogyo 2008), although it is an important source of payment for such services as chiropractic care and physiotherapy. Almost 9% of Canadians visited a physiotherapist in 2000 (CCHS n.d.), up from 7% in 1994 (NPHS n.d.). Physiotherapy is identified most explicitly in relation to hospital-associated care in the Canada Health Act.
The practice of physiotherapy in Ontario is defined as “the assessment of physical function and the treatment, rehabilitation and prevention of physical dysfunction, injury or pain, to develop, maintain, rehabilitate or augment function or to relieve pain” (Physiotherapy Act, SO 1991, c.37). A proposal to broaden the scope to include diagnosis is being considered (Physiotherapy Scope of Practice Review 2008).
In Ontario, the Regulated Health Professions Act, 1991 regulates physiotherapists' practice. Since January 1994, physiotherapists have been considered primary care practitioners. Physician referral is required only if a patient is seeing a physiotherapist in a public hospital or is billing the Ontario Health Insurance Plan (OHIP) for treatments. The public–private mix for physiotherapy has been changing over the last decade (Landry et al. 2007). In Ontario, approximately 39% of physiotherapists practise in hospitals, 35% are in private practice, 8% in home care, 5% in designated physiotherapy clinics and the remainder are found in a range of different sites (College of Physiotherapists of Ontario 2009). Less than 1% work directly in industry. OHIP currently covers physiotherapy services for (a) residents aged over 65 or under 20 years, (b) those who qualified for social support, (c) residents of long-term care facilities and (c) those who are returned to the community following hospital discharge (Ontario Ministry of Health and Long-Term Care 2005). The importance of physiotherapy in home care varies by province and location (Beland and Bergman 2000). “Most provincial health plans provide little or no coverage … for physiotherapy [among other services] … . How do we decide what is publicly covered and what is not?” (Stuart and Adams 2007). This question is an important one to Canadians, who take pride in medicare-ensured access to necessary healthcare.
Based on publicly available sources, the breakdown of provider mix and source of financing for rehabilitative care can only be estimated. Colombo and Tapay (2004) report that 65% of Canadians have private health insurance, mainly offered via employers, which provides benefits for healthcare services not typically covered by public schemes (e.g., dentistry, prescription drugs and rehabilitative care). Private health insurance accounts for only 11.4% of total healthcare expenditures in Canada. However, it pays for more than 90% of the approximately 11% of total healthcare expenditures that go towards other professionals (dentists, optometrists, chiropractors and physiotherapists, among others) (CIHI 2009).
The considerable changes in financing and provision of healthcare in general over the past decades (DiMatteo 2000) have affected rehabilitative care in Ontario in particular (Gildiner 2001). In a national key informant survey, McKillop (2005) found that 44% of providers likely had some private financing of physiotherapy delivery, with 43% structurally regarded as private in delivery. He argued that “[m]echanisms should be developed, in consultation with private sector providers, to ensure that private sector delivery activities are fully represented in Canada's national health databases.”
As part of a collaborative research arrangement with a metropolitan newspaper of approximately 2,000 employees, we negotiated anonymous access to multiple sources of information about physiotherapy utilization. These services were both directly employer provided and financed by third-party payers (i.e., “organizations such as workers' compensation boards, private health insurance companies, and employer-based healthcare plans that pay for insured health services for their clients and employees” [Health Canada 2007]). We were particularly interested in physiotherapy for musculoskeletal disorders (MSDs), which constitute a substantial disease burden among Ontario's general (Badley et al. 1994) and working (Choi et al. 1996) populations. Physiotherapy visits were common among those with back problems, and were reported by 15% of those with back pain in the 2000 Canadian Community Health Survey (CCHS) (Jacobs et al. 2004) and 11% of CCHS respondents with repetitive strain MSDs (CCHS n.d.).
Physiotherapy is important for people experiencing MSDs, both those with occupational upper extremity disorders in the US federal workforce (Feuerstein et al. 1998) and among employees at the newspaper in our study (Swift et al. 2001). Further, improved access to physiotherapy was part of a multifaceted program to reduce the burden of MSDs at the newspaper (Polanyi et al. 2005). We sought to describe the mix of providers and financing among the employee population over the period that the workplace parties recognized and responded to MSD injuries (1992–2002).
Methods
We sought data access with full knowledge of, and approval by, the RSI Committee, a joint labour–management committee that oversaw the RSI program at the workplace (Polanyi et al. 2005). [“RSI” refers to repetitive strain injury, and is the workplace term for MSD injuries. We use the abbreviation here only in reference to the RSI Committee and program.] All data sharing was governed by ethics approval from McMaster University's Health Research Ethics Board.
Data sources and preparation procedures
We obtained access to individual-level billing data from three different payers: the Ontario Workplace Safety and Insurance Board (WSIB), private health insurance companies and the workplace itself. An overarching research data-sharing agreement between the Institute for Work and Health and the WSIB enabled the research team to obtain WSIB data. The workplace provided entrée to the private health insurance companies, supported researchers to obtain contracted private clinic data and directly shared its own provision data.
A union representative on the RSI Committee suggested that we seek consent for individual-level data linkage and access to Ontario Health Insurance Plan (OHIP) data. Unfortunately, only about 13% of employees felt comfortable providing such consent, so we could not obtain OHIP data. Nor could we conduct linkages across data sources with traceable individual identifiers.
WSIB Data
The Ontario WSIB provides no-fault insurance coverage for workplace injuries and diseases to most Ontario workers and workplaces. Employers must submit claims within three days if a worker gets healthcare treatment (e.g., doctor's visit, physiotherapy care) for a workplace injury or illness. We were able to identify active claims for the workplace (using the firm identification number), determined by either the date of “accident,” a healthcare benefit or wage benefit provided during the time period of interest. Beyond the claim number for linking across files, we did not use any personal identifying information. We identified claims for MSDs using a series of available codes on part of body and nature of injury, as per earlier work (Brooker et al. 2001).
The WSIB healthcare benefit file contained information about healthcare services provided by a variety of healthcare providers except physicians. We excluded administrative costs and services incurred to obtain healthcare services (e.g., transportation, hotel), focusing only on delivered physiotherapy services.
Healthcare Insurer Data
Many Ontario workplaces offer enhanced medical coverage through a private insurance company for services not covered by OHIP. At the newspaper, two different insurance carriers provided negotiated benefit coverage during the study time period: carrier 1, from prior to the start of observation in 1992 until August 1996; and carrier 2, from August 1996 until the end of the observation period in 2002. All billings for the employees only (i.e., excluding spouses and dependents) were provided by both insurance carriers, stripped of actual identifying information but with pseudo-identification numbers permitting linkage for an individual within each distinct data source, but not across these two data sources (with consequences for Q3 1996, as highlighted in the results).
We used data about licensed physiotherapist billings for persons under the age of 65. Available variables included the pseudo-identifier, age of claimant, service date and amount paid. Unfortunately, diagnostic codes that might designate MSDs or any information to clarify whether the benefit was related to the workplace were not included.
Data about Workplace Directly Funded Activities
Through union–management negotiations, employees obtained reimbursement up to approximately CAD$1,500 per year for treatment of MSDs, starting in 1995. This special fund was explicitly for treatments not covered by OHIP or private health insurance carriers. The 1998 collective agreement made provision for on-site physiotherapy at the workplace. The human resources department supported research team efforts to obtain quarterly aggregated data, without personal identifiers, about physiotherapy use for both these sources.
Although data about the specific types of physiotherapy care provided were not available for the treatments we studied, we could ascertain the nature of on-site clinic services. Clinicians engaged in stretching, massage, instruction about exercises, adaptation of workstations and guidance about improved self-management (Pam Honeywell, physiotherapist, personal communication) for soft-tissue conditions such as neck and shoulder pain, arm pain and back pain (Cole et al. 2003).
Measured Outcomes
We set out trends in physiotherapy utilization by quarter for the number of unique claimants/clients, the number of bills/services and the total costs. For WSIB data, we also calculated physiotherapy as a proportion of total healthcare costs. The workplace human resources department provided information about the number of employees by year of observation, allowing calculation of rates per capita and per quarter. We calculated summary statistics to contrast utilization more explicitly across three time periods: 1st quarter (Q1) 1992 to 4th quarter (Q4) 1994, for WSIB and health insurance carriers; 1995 Q1 to 1999 Q1, for the special fund; and 1999 Q2 to 2002 Q4, for the on-site physiotherapy provision.
Results
Table 1 sets out the number of employees and the number of unique claimants/clients found in each data source on a yearly basis. We extracted a total of 1,890 WSIB claims, defined as “active” claims for workers aged 65 and under during the period under investigation. Of these, 1,131 (60%) were for MSDs, and 132 claimants (7%) made physiotherapy claims. Because of the overlap in private health insurance carriers in 1996, the estimated number of claimants appears larger than the size of the workforce. Further, the number of unique claimants identified from the second carrier's data was also bigger than the number of employees for years 1997 and 1998, though this carrier indicated that the data contained claims for employees only (no other family members) aged less than 65.
TABLE 1.
Employee population and claimant/service rates (%) per 1,000 employees, by year
| Year | Employees (#) | Ontario WSIB (Workplace Safety & Insurance Board) Claims | Health Insurance Carriers1 | Special Physiotherapy Reimbursement Fund Claimants (#, rate) | Workplace On-Site Physiotherapy Clinic Clients (#, rate) | |||
|---|---|---|---|---|---|---|---|---|
| All Claimants (#, rate) |
MSD Claimants (#, rate) |
Physiotherapy Claimants (#, rate) |
All Claimants (#, rate) |
Physiotherapy Claimants (#, rate) |
||||
| 1992 | 2,160 | 180 (83) | 113 (52) | 30 (14) | 1,935 (895) | 16 (7) | Not Applicable (NA) | |
| 1993 | 2,021 | 179 (89) | 105 (52) | 16 (8) | 1,855 (918) | 42 (21) | ||
| 1994 | 1,769 | 151 (85) | 103 (58) | 21 (12) | 1,703 (963) | 40 (23) | ||
| 1995 | 1,800 | 203 (113) | 138 (77) | 20 (11) | 1,701 (945) | 46 (26) | 22 (12) | NA |
| 1996 | 1,792 | 165 (92) | 116 (65) | 6 (3) | 3,360 (1,875) | 28 (16) | 45 (25) | NA |
| 1997 | 1,807 | 135 (75) | 73 (40) | <5 (-) | 2,026 (1,121) | 38 (21) | 175 (97) | NA |
| 1998 | 1,884 | 150 (80) | 93 (49) | 8 (4) | 2,534 (1,345) | 34 (18) | 183 (97) | NA |
| 1999 | 1,879 | 169 (90) | 95 (51) | 5 (3) | 1,559 (830) | 27 (14) | 377 (201) | 273 (145) |
| 2000 | 1,914 | 178 (93) | 99 (52) | <5 (-) | 1,744 (911) | 41 (21) | 93 (49) | 350 (183) |
| 2001 | 1,901 | 219 (115) | 125 (66) | 15 (8) | 1,658 (872) | 43 (23) | 542 (28) | 324 (170) |
| 2002 | 1,818 | 161 (89) | 71 (39) | 6 (3) | 1,584 (871) | 37 (20) | -2 | 324 (178) |
| Total claims/clients | 1,557 | 896 (58%) | 105 (6.7%) | 6,587 | 312 (4.7%) | -3 | -3 | |
aIn 1996, the newspaper changed insurance companies from Liberty to Sun Life, and the study was not allowed to identify persons in insurer data sets, so a person might be double-counted.
bData are available up to Q2, 2001 and not thereafter.
cData are not available.
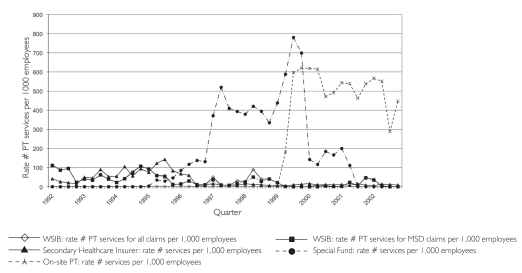
The shifts in numbers of clients from WSIB and private carriers to the special fund are notable in 1995, and from all three sources to the on-site clinic by 2000. Figure 1 demonstrates these patterns graphically for service rates.
FIGURE 1.
Physiotherapy service rates by different providers and payers (1992–2002)
Aggregated into the periods of interest, the addition of the special fund in Q1 of 1995 resulted in an approximately threefold increase (depending on the measure) in physiotherapy services used per quarter. The presence of an on-site service increased utilization by another three times (again, depending upon the measure) (see left-hand columns in Table 2). The shift in financing from WSIB and health insurance carriers is also apparent, first to the special fund, and then to employer-provided on-site services.
TABLE 2.
Physiotherapy utilization and associated costs, by period
| Services Total # in the corresponding entire period (mean; SD by quarter) [median by quarter] | Costs Total $ in the corresponding entire period (mean; SD by quarter) [median by quarter] | |||||
|---|---|---|---|---|---|---|
| 1992Q1–1994Q4 | 1995Q1–1999Q1 | 1999Q2–2002Q4 | 1992Q1–1994Q4 | 1995Q1–1999Q1 | 1999Q2–2002Q4 | |
| Ontario WSIB claim | 1,466 (122.2; 67.6) [103] |
935 (55; 41.5) [46] |
227 (15.1; 27.2) [2] |
42,266.00 (3,522.17; 2,974.14) [2,959.50] |
17,520.00 (1,030.59; 1,138.48) [756.00) |
4,266.00 (284.40; 501.79) [54.00] |
| Health insurance carriers | 1,249 (104.1; 50.5) [98] |
1,190 (70; 80.2) [23] |
295 (19.7; 6.4) [19] |
15,149.60 (1,262.47; 635.98) [1,195.60] |
30,679.00 (1,804.65; 809.85) [1,671.40] |
25,836.49 (1,722.43; 926.44) [1,496.20] |
| Special fund | NA | 7,813 (459.6; 331.2) [630] |
5,641 (626.8; 511.7) [353] |
NA | 418,483.48 (24,616.68; 19,164.42) [33,007.64] |
303,576.92 (33,730.77; 28,156.14) [17,242.91] |
| On-site | NA | NA | 14,153 (943.5; 237.3) [1,021.0] |
NA | NA | 576,607.85 (38,440.5; 8,132.83) [40,663.76] |
| Total | 2,715 (226.3; 81.5) [234.0] |
9,938 (584.6; 264.9) [718.0] |
20,316 (1,354.4; 552.7) [1,281.0] |
57,415.60 (4,784.63; 3,047.06) [4,740.30] |
466,682.48 (27,451.91; 18,643.55) [35,155.24] |
910,287.26 (60,685.82; 25,007.48) [52,133.98] |
Cost increases surpassed utilization increases. There were associated differential costs per service: an eightfold increase overall from 1992–94 (57K) to 1995–99 Q1 (467K). However, these increases took place over four years in the second period, compared to three years in the first. A further near-doubling of costs occurred in the 1999 Q2 to 2002 period (910K vs. 467K in 1995–99 Q1) (see right-hand columns of Table 2). In keeping with the shift away from WSIB financing, physiotherapy costs became a decreasing proportion of overall WSIB healthcare benefit costs: more than 30% from 1992 to 1995 versus less than 10% for 1999 on. This decline was due to a reduced number of claims, and a lower median and mean cost of services per claim (see Table 3).
TABLE 3.
Physiotherapy costs for MSD claimants paid directly by the Ontario WSIB, by year
| Year | Physiotherapy costs (CAD$) | All healthcare costs (CAD$) | ||||
|---|---|---|---|---|---|---|
| n | Median | Mean (SD) | Total (% of all healthcare costs) | Median | Total | |
| 1992 | 30 | 652 | 715 (618) | 21,452 (47%) | 84 | 46,054 |
| 1993 | 16 | 521 | 590 (521) | 9,440 (34%) | 89 | 27,884 |
| 1994 | 21 | 392 | 539 (504) | 11,325 (40%) | 89 | 28,648 |
| 1995 | 20 | 244 | 431 (474) | 8,622 (36%) | 52.5 | 24,033 |
| 1996 | 6 | 171 | 242 (232) | 1,451 (9%) | 44 | 16,117 |
| 1997 | <5 | 501 | 496 (31) | 1,489 (12%) | 46 | 12,850 |
| 1998 | 8 | 576 | 603 (279) | 4,822 (39%) | 46 | 12,245 |
| 1999 | 5 | 18 | 244 (328) | 1,221 (7%) | 63 | 17,130 |
| 2000 | <5 | 83 | 83 (61) | 166 (0.6%) | 63 | 27,616 |
| 2001 | 15 | 54 | 178 (246) | 2,677 (7%) | 85 | 37,630 |
| 2002 | 6 | 131 | 231 (272) | 1,387 (9%) | 71 | 16,285 |
Healthcare costs include those for actual healthcare services but exclude those for transportation, vocational rehabilitation, accommodations, etc.
Discussion
We documented dramatic increases in physiotherapy utilization over the 11 years, accompanied by substantial shifts among providers and payers. In the absence of reasonably valid data in the public domain about financing physiotherapy utilization across a range of sources, our efforts are an important benchmark for Canadian research. They respond to McKillop's (2005) call and provide a far clearer picture of physiotherapy utilization among a working population.
With the availability of the special fund, increases in physiotherapy use may have been due to reduced financial barriers and greater affordability, comparable to the removal of user fees for other medical services. The second rise may have been due to several factors. An active workplace campaign encouraged early reporting and treatment, likely prompting employees to come forward with MSDs that they had not dealt with previously (Polanyi et al. 2005) or to seek physiotherapy to reduce pain and improve function.
Greater geographical accessibility (on-site vs. off-site) was important for employees and their supervisors. The latter were more likely to support employee treatment when time away from work was minimized. On-site clinic data showed declines in presenting symptom duration over the years 1999 to 2002 (Cole et al. 2003), indicating that employees were seeking treatment earlier. As well, on-site providers had useful skills – the physiotherapists were more experienced with MSDs typical in office work settings – and took more time in treatment and education (Pam Honeywell, personal communication).
There are several limitations in the findings presented. Identifying individuals in the second insurance carrier's data led to overestimation of the number of claimants. However, given that we had an independent measure of workforce size directly from the company, this should not affect our per capita utilization rate estimates. Our inability to obtain OHIP data likely led to underestimation of total utilization and of publicly funded contributions. We also missed physiotherapy reimbursed under a plan held by a spouse or other family member and out-of-pocket payments to physiotherapists. We expect these last would be minimal in a unionized workforce with extended health benefits and other provisions, such as the special fund, in comparison to other populations without these resources (CIHI 2009). However, employees might have used each of these in the period from 1992 to 1996, and then transferred some of this unmeasured utilization to the special fund and worksite services from 1997 onwards. The extent of such a transfer is hard to estimate accurately. Given what we know from existing surveys on physiotherapy utilization and our own experience as worksite researchers and as clinicians serving working patients, we do not think such transfers would represent more than 20% of utilization increases.
If improved affordability and geographic accessibility promoted more timely physiotherapy utilization, we can ask, “What other criteria would contribute to describing such services as ‘medically necessary’”? Some payers, particularly insurers, might argue that without the imprimatur of a physician diagnosis and referral, not required for the on-site clinic nor for physiotherapy services more generally in Ontario, then the services could not be classified as medically necessary. However, physician control of access to other health professionals is increasingly being questioned by nurse practitioners, physiotherapists (Massey 2002) and, more recently, by governments moving towards coordinated, interprofessional care arrangements (Interprofessional Care Steering Committee 2007). Hence, the term “medical” has been expanded in meaning to include clinical care more broadly rather than physician-sanctioned or supplied.
Another common approach to assessing “necessary” services considers the effectiveness of the clinical services. A spate of relevant systematic reviews of effectiveness for the types of conditions seen and physiotherapy treatments applied in the on-site physiotherapy facility, at least, are available. Despite the caveats that systematic reviewers note around the uneven quality of clinical research available, evidence for effectiveness should at least meet requirements to substantiate medical necessity, as summarized in Table 4.
TABLE 4.
Evidence available from systematic reviews on physiotherapy treatment effectiveness
| Condition | Treatment | Effectiveness | 1st Author (year) |
|---|---|---|---|
| Mechanical neck disorders | Exercises | Limited evidence of benefit for strengthening, stretching and strengthening exercises for neck disorder with headache. | Kay et al. (2005) |
| Limited evidence of benefit for active range-of-motion exercises or a home exercise program for acute mechanical neck disorder. | |||
| Unclear evidence of benefit for a stretching and strengthening program in chronic mechanical neck disorder. | |||
| Non-specific neck pain | Massage | Uncertain | Ezzo et al. (2007) |
| Manual & supervised exercise interventions | For subacute or chronic non-specific neck pain, more effective than no treatment, sham or alternative interventions. | Hurwitz et al. (2008) | |
| Interventions focused on regaining function & return to work | For neck pain without radicular symptoms, relatively more effective than interventions that do not have such a focus. | ||
| Shoulder pain | Exercise | Effective in short-term recovery and longer-term benefit to function. | Green et al. (2003) |
| Work-related complaints of the neck, shoulder or arm | Exercises | Conflicting evidence concerning efficacy vs. no treatment. | Verhagen et al. (2006) |
| Lateral epicondylitis (elbow) | Exercise | Positive effects in the reduction of pain or improvement in function. | Trudel et al. (2004) |
| Low-back pain | Exercise | Slightly effective at decreasing pain and improving function in adults with chronic low-back pain. In subacute low-back pain, some evidence that a graded activity program improves absenteeism outcomes. | Hayden et al. (2005) |
| Massage | Might be beneficial for patients with subacute and chronic non-specific low-back pain, especially when combined with exercises and education. | Furlan (2002) |
Hence, we argue that such treatments should be accessible to those with MSD conditions in working-age populations. The newspaper took an inclusive approach, not differentiating between workplace “caused,” “aggravated” or “prevalent” MSDs and more concerned about improving function, both for employee well-being and productivity. Further, these newspaper workers were among the approximately 30% of Canadian workers who are unionized (Strategic Policy, Analysis and Workplace Information Directorate 2008). They were more likely to have benefits than the non-unionized majority of workers. The latter must rely on less common employer-based private insurance benefits, WSIB benefits for the small percentage with MSDs deemed “work-related,” or employment insurance healthcare benefits for those who lose their job because of their MSD. They may face issues of access to physiotherapy services (e.g., geographic, financial, time), as witnessed by the low rate of physiotherapy utilization observed in the early years of this study.
Publicly funded physiotherapy services are unlikely to fill the gap, as provincial health insurance programs among those aged 20 to 64 have become more restrictive, rather than less (Gildiner 2001; Landry et al. 2007). As the OHIP circular announcing policy changes noted under frequently asked questions: “Q: Will my employer or my insurance company now pay for the whole cost of these [physiotherapy] services? A: This depends on the employer's insurance policy. Individuals should speak with their employers about their plan” (Ontario Ministry of Health and Long-Term Care 2005). Recent studies show that access to physiotherapy is impeded in the current system for people with chronic conditions, those lacking private healthcare and those living in less urban regions (Cott et al. 2007). Documenting changes before and after the delisting of physiotherapy services in Ontario, Landry and colleagues (2006) showed that 18% of physiotherapy patients discontinued their physiotherapy after delisting because they could not pay for it. In an increasingly competitive global marketplace, the generosity observed at this newspaper is likely not common among employers, nor may it be sustainable.
The extent to which constraints on accessibility to effective treatments such as physiotherapy services are deemed to infringe upon the access provisions enshrined in medicare (Stradiotto 2007) remains an important issue for Canadian healthcare policy makers over the coming years. Landry and colleagues (2006) showed that patients who were able to maintain access to physiotherapy after delisting were 10 times as likely to report good or excellent self-rated health compared to the patients unable to continue with physiotherapy. However positive this finding may seem, selection effects are likely present (i.e., the most vulnerable and poorest may have been less likely to be able to maintain access, and they would have poorer health status to begin with). We argue that such vulnerable groups should be given first consideration in support for access to physiotherapy services, a principle recognized by some provincial medicare plans that retain coverage of services to those >65 and <20 years of age. Some provinces and communities have chosen another route, including physiotherapy in community health centre services, particularly for those CHCs serving large senior populations (e.g., in Ontario, community care access centres for senior citizens upon hospital discharge but with strict limitations on eligibility [Ontario Ministry of Health and Long-Term Care 2007; Ontario Physiotherapy Association 2009], community rehabilitation services for low-income persons in Alberta [Alberta Health Services 2010] and in Manitoba with Aboriginal health and the Geriatric Program Assessment Team [GPAT] of the Winnipeg Regional Health Authority [Fricke 2005]).
Conclusion
In light of shorter hospital stays and continued occurrences of injuries in communities and workplaces, and the ongoing burden of chronic MSDs, many patients in the community need rehabilitative services. Their growing dependence on private physiotherapy services, with resulting inequities in access, requires a review of services covered under the concept of “universal healthcare” in Canada. Cost-minimization analyses might support coverage of a broader range of patients by provincial plans (e.g., patients whose maintenance in the community with adequate outpatient physiotherapy would prevent re-hospitalization, and working-age adults whose treatment would let them return to productive employment, reducing other social welfare costs).
Just as Canadians uphold medicare to employers as a social benefit (deemed a “subsidy” by US free-trade advocates), we argue that ensuring public coverage of physiotherapy and other rehabilitative services would support small- and medium-sized employers and their employees, who together cannot finance adequate private benefit plans. Such options might confront both the “crisis in access” that physiotherapists' associations have highlighted (e.g., see http://www.opa.on.ca) and tackle the burden of MSDs. Sustaining healthy, productive small- and medium-sized workforces is in the interests of Canadian families and communities that depend upon them. We hope our findings inform a dialogue about such options.
Acknowledgements
The authors would like to acknowledge: members of the Worksite Upper Extremity Group at the Institute for Work & Health (Anne Moore, Michael Polanyi, Harry Shannon, Michael Swift, Dwayne van Eerd); labour and management members of the RSI (Repetitive Strain Injury) Committee at the workplace; and physiotherapy providers of the private clinic. This project was sponsored by the Institute for Work & Health. The Institute, an independent not-for-profit research organization, receives support from the Ontario Workplace Safety & Insurance Board. Funding was provided by the RSI Committee and the U.S. National Institute for Occupational Safety and Health/National Institutes of Health under Research Grant #5 R01 OH003708-03.
Contributor Information
Sheilah Hogg-Johnson, Senior Scientist, Institute for Work & Health, Dalla Lana School of Public Health, Toronto, ON.
Donald C. Cole, Institute for Work & Health, Associate Professor, Dalla Lana School of Public Health, University of Toronto, Toronto, ON.
Hyunmi Lee, Research Associate, Institute for Work & Health, Toronto, ON.
Dorcas E. Beaton, Director, Research Mobility Unit, Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Institute for Work & Health, Graduate Department of Rehabilitation Science, Faculty of Medicine, University of Toronto, Toronto, ON.
Carol Kennedy, Research Associate, Institute for Work & Health, Keenan Research Centre, Li Ka Shing Knowledge Institute, St. Michael's Hospital, Toronto, ON.
Peter Subrata, Institute for Work & Health, Toronto, ON.
References
- Alberta Health Services. Community Rehabilitation Services – Physiotherapy. 2010. Retrieved January 16, 2011. < http://www.albertahealthservices.ca/services.asp?pid=service&rid=1001414>.
- Badley E.M., Rasooly I., Webster G.K. Relative Importance of Musculoskeletal Disorders As a Cause of Chronic Health Problems, Disability and Health Care Utilization: Findings from the 1990 Ontario Health Survey. Journal of Rheumatology. 1994;21(3):505–14. [PubMed] [Google Scholar]
- Beland F., Bergman H. Home Care, Continuing Care and Medicare: A Canadian Model or Innovative Models for Canadians? Healthcare Papers. 2000;1(4):38–45. doi: 10.12927/hcpap..17349. [discussion, 109–12]. [DOI] [PubMed] [Google Scholar]
- Bogyo T. The Case for Excluding Workers' Compensation Insurance from Medicare. Healthcare Papers. 2008;8(3):21–29. doi: 10.12927/hcpap.2008.19794. [DOI] [PubMed] [Google Scholar]
- Brooker A.S., Cole D.C., Hogg-Johnson S., Smith J., Frank J.W. the Early Claimant Cohort Prognostic Modeling Group. Modified Work: Prevalence and Characteristics in a Sample of Workers with Soft-Tissue Injuries. Journal of Occupational & Environmental Medicine. 2001;43(3):276–84. doi: 10.1097/00043764-200103000-00017. [DOI] [PubMed] [Google Scholar]
- Canadian Community Health Survey (CCHS) special tabulation. Ottawa: Statistics Canada; n.d.. Retrieved January 14, 2011. < http://www.statcan.gc.ca/cgi-bin/imdb/p2SV.pl?Function=getSurvey&SDDS=3226&lang=en&db=imdb&adm=8&dis=2>. [Google Scholar]
- Canadian Institute for Health Information (CIHI) National Health Expenditure Trends, 1975 to 2009. Ottawa: Author; 2009. [Google Scholar]
- Choi B.C.K., Levitsky M., Lloyd R.D., Stones I.M. Patterns and Risk Factors for Sprains and Strains in Ontario, Canada 1990: An Analysis of the Workplace Health and Safety Agency Data Base. Journal of Occupational & Environmental Medicine. 1996;38:379–89. doi: 10.1097/00043764-199604000-00016. [DOI] [PubMed] [Google Scholar]
- Cole D.C., Ferrier S., Hogg-Johnson S., Kennedy C., Lee H., Van Eerd D., Mazumder A., Beaton D., Wells R., Ibrahim S., Subrata P., Shannon H., Manno M., Moore A., Resendes E. National Institute for Occupational Safety and Health. Toronto: Institute for Work & Health; 2003. WMSD: Evaluating Interventions among Office Workers. pp. 1–96. (NIOSH) research grant #5 R01 OH003708-03:. [Google Scholar]
- College of Physiotherapists of Ontario. Annual Report 08/09. Retrieved January 14, 2011. < http://www.collegept.org/Stakeholders/College%20Documents/CollegeDocuments>.
- Colombo F., Tapay N. Private Health Insurance in OECD Countries: The Benefits and Costs for Individuals and Health Systems. Paris: Organisation for Economic Co-operation and Development; 2004. OECD Health Working Papers No. 15. [Google Scholar]
- Cott C.A., Devitt R.M.A., Falter L.B., Soever L.J., Passalent L.A. Barriers to Rehabilitation in Primary Health Care in Ontario: Funding and Wait Times for Physical Therapy Services. Physiotherapy Canada. 2007;59:173–83. [Google Scholar]
- DiMatteo L. The Determinants of the Public–Private Mix in Canadian Health Care Expenditures: 1975–1996. Health Policy. 2000;52(2):87–112. doi: 10.1016/s0168-8510(00)00071-3. [DOI] [PubMed] [Google Scholar]
- Ezzo J., Haraldsson B.G., Gross A.R., Myers C.D., Morien A., Goldsmith C.H., Bronfort G., Peloso P.M. Massage for Mechanical Neck Disorders: A Systematic Review. Spine. 2007;32(3):353–62. doi: 10.1097/01.brs.0000254099.07294.21. [DOI] [PubMed] [Google Scholar]
- Feuerstein M., Miker V.L., Burrell L.M., Nerger R. Occupational Upper Extremity Disorders in the Federal Workforce: Prevalence, Health Care Expenditures and Patterns of Work Disability. Journal of Occupational & Environmental Medicine. 1998;40:547–55. doi: 10.1097/00043764-199806000-00007. [DOI] [PubMed] [Google Scholar]
- Fricke M. Physiotherapy and Primary Health Care: Evolving Opportunities. Winnipeg: Manitoba Branch of the Canadian Physiotherapy Association, College of Physiotherapists of Manitoba and Department of Physical Therapy, School of Medical Rehabilitation, University of Manitoba; 2005. Retrieved January 14, 2011. < http://www.manitobaphysio.com/pdf/FinalMBPHCReportJune_05_000.pdf>. [Google Scholar]
- Furlan A.D., Brosseau L., Imamura M., Irvin E. Massage for Low-Back Pain: A Systematic Review within the Framework of the Cochrane Collaboration Back Review Group. Spine. 2002;27(17):1896–910. doi: 10.1097/00007632-200209010-00017. [DOI] [PubMed] [Google Scholar]
- Gildiner A. What's Past Is Prologue: A Historical–Institutional Analysis of Public–Private Change in Ontario's Rehabilitation Health Sector, 1985–1999. Toronto, ON: University of Toronto; 2001. Doctoral thesis. [Google Scholar]
- Green S., Buchbinder R., Hetrick S. Physiotherapy Interventions for Shoulder Pain. Cochrane Database of Systematic Reviews. 2003;(Issue 2) doi: 10.1002/14651858.CD004258. Art. no. CD004258. doi:10.1002/14651858.CD004258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayden J.A., Van Tulder M.W., Malmivaara A.V., Koes B.W. Meta-Analysis: Exercise Therapy for Nonspecific Low Back Pain. Annals of Internal Medicine. 2005;142(9):765–75. doi: 10.7326/0003-4819-142-9-200505030-00013. [DOI] [PubMed] [Google Scholar]
- Health Canada. Canada Health Act, Annual Report 2006–2007. 2007. Annex D, Glossary. Retrieved January 14, 2011. < http://www.hc-sc.gc.ca/hcs-sss/pubs/cha-lcs/2006-cha-lcs-ar-ra/app-ann-d-eng.php>.
- Hurwitz E.L., Carragee E.J., van der Velde G., Carroll L.J., Nordin M., Guzman J., Peloso P.M., Holm L.W., Côte P., Hogg-Johnson S., Cassidy J.D., Haldeman S. Treatment of Neck Pain: Noninvasive Interventions: Results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4S):S123–S152. doi: 10.1097/BRS.0b013e3181644b1d. [DOI] [PubMed] [Google Scholar]
- Interprofessional Care Steering Committee. Ontario Ministry of Health and Long-Term Care. Health Human Resources Strategy Division. Interprofessional Care: A Blueprint for Action in Ontario. 2007. Jul, Retrieved January 14, 2011. < http://www.healthforceontario.ca/upload/en/whatishfo/ipc%20blueprint%20final.pdf>.
- Jacobs P., Schopflocher D., Klarenbach S., Golmohammadi K., Ohinmaa A. A Health Production Function for Persons with Back Problems: Results from the Canadian Community Health Survey of 2000. Spine. 2004;29:2304–8. doi: 10.1097/01.brs.0000142228.10239.f8. [DOI] [PubMed] [Google Scholar]
- Kay T.M., Gross A., Goldsmith C., Santaguida P.L., Hoving J., Bronfort G. Exercises for Mechanical Neck Disorders. Cochrane Database Systematic Review. 2005;(Issue 3) doi: 10.1002/14651858.CD004250.pub3. Art. no. CD004250. doi:10.1002/14651858.CD004250.pub3. [DOI] [PubMed] [Google Scholar]
- Landry M.D., Deber R.B., Jaglal S., Laporte A., Holyoke P., Devitt R., Cott C. Assessing the Consequences of Delisting Publicly Funded Community-Based Physical Therapy on Self-Reported Health in Ontario, Canada: A Prospective Cohort Study. Journal of Rehabilitation Research. 2006;29(4):303–7. doi: 10.1097/MRR.0b013e328010badc. [DOI] [PubMed] [Google Scholar]
- Landry M.D., Williams A.P., Verrier M.C., Zakus D., Deber R.B. Shifting the Public–Private Mix: A Policy Analysis of Physical Therapy Funding in Ontario. Physiotherapy Canada. 2007;59(4):255–65. [Google Scholar]
- Leatt P., editor. Healthcare Papers. 2008;8(3 “Unequal Access”):1–54. (Entire issue.) [PubMed] [Google Scholar]
- Massey B.F., Jr. What's All the Fuss about Direct Access? 2002 APTA Presidential Address. Physical Therapy. 2002;82(11):1120–3. [PubMed] [Google Scholar]
- McKillop I. Private Sector Delivery: Scope and Extent in Canada's Health Care System. 2005. Feb, Project number: 6795-15-2002/4570001. Health Policy Research Program Summary of Research Results. Health Canada. Retrieved January 14, 2011. < http://www.hc-sc.gc.ca/sr-sr/pubs/hpr-rpms/2005-pratique-priv-sector-eng.php>.
- National Population Health Survey (NPHS) (special tabulation) Ottawa: Statistics Canada; n.d.. Retrieved January 14, 2011. < http://www.statcan.gc.ca/concepts/nphs-ensp/index-eng.htm>. [Google Scholar]
- Ontario Ministry of Health and Long-Term Care. Changes in Coverage for Physiotherapy Services. 2005. Mar, Catalogue no. 7610-2142024. Retrieved January 14, 2011. < http://www.health.gov.on.ca/english/public/pub/ohip/physiotherapy.html>.
- Ontario Ministry of Health and Long-Term Care. Health Services in Your Community: Community Care Access Centre Locations. 2007. Retrieved January 14, 2011. < http://www.health.gov.on.ca/english/public/contact/ccac/ccacloc_mn.html>.
- Ontario Physiotherapy Association. Position Statement: Access to Publicly Funded Physiotherapy in Ontario. 2009. Retrieved January 14, 2011. < http://www.opa.on.ca/health_pos.shtml>.
- Physiotherapy Act, SO 1991, c.37.
- Physiotherapy Scope of Practice Review. 2008. Submission to the Health Professions Regulatory Advisory Council by the Ontario Physiotherapy Association and College of Physiotherapists of Ontario, June 30, 2008. Retrieved January 14, 2011. < http://www.collegept.org/AnnouncementRetrieve.aspx?ID=18976>.
- Polanyi M.F., Cole D.C., Ferrier S.E., Facey M. The Worksite Upper Extremity Research Group. Paddling Upstream: A Contextual Analysis of Implementation of a Workplace Ergonomic Policy at a Large Newspaper. Applied Ergonomics. 2005;36:231–39. doi: 10.1016/j.apergo.2004.10.011. [DOI] [PubMed] [Google Scholar]
- Stradiotto R.A. Access to Non-Funded Health Services (the Legal Implications). Healthcare Quarterly. 2007;10(3):46–56. doi: 10.12927/hcq..18924. [DOI] [PubMed] [Google Scholar]
- Strategic Policy, Analysis, and Workplace Information Directorate, Labour Program, Human Resources and Social Development Canada. Union Membership in Canada 2007. Ottawa: Human Resources and Skills Development Canada; 2008. Retrieved January 14, 2011. < http://www.hrsdc.gc.ca/eng/lp/wid/union_membership.shtml>. [Google Scholar]
- Stuart N., Adams J. The Sustainability of Canada's Healthcare System: A Framework for Advancing the Debate. Healthcare Quarterly. 2007;10(2):96–102. doi: 10.12927/hcq.2007.18839. [DOI] [PubMed] [Google Scholar]
- Swift M.B., Cole D.C., Beaton D.E., Manno M. Health Care Utilization and Workplace Interventions for Neck and Upper Limb Problems among Newspaper Workers. Journal of Occupational & Environmental Medicine. 2001;43(3):265–75. doi: 10.1097/00043764-200103000-00016. [DOI] [PubMed] [Google Scholar]
- Trudel D., Duley J., Zastrow I., Kerr E.W., Davidson R., MacDermid J.C. Rehabilitation for Patients with Lateral Epicondylitis: A Systematic Review. Journal of Hand Therapy. 2004;17(2):243–66. doi: 10.1197/j.jht.2004.02.011. [DOI] [PubMed] [Google Scholar]
- Verhagen A.P., Karels C., Bierma-Zeinstra S.M.A., Burdorf L., Feleus A., Dahaghin S., de Vet H.C.W., Koes B.W. Ergonomic and Physiotherapeutic Interventions for Treating Work-Related Complaints of the Arm, Neck or Shoulder in Adults. Cochrane Database of Systematic Reviews. 2006;(Issue 3) doi: 10.1002/14651858.CD003471.pub3. Art. no. CD003471. doi:10.1002/14651858.CD003471.pub 3. [DOI] [PubMed] [Google Scholar]