Abstract
Objective
Given the perceived technical demands of laparoscopic appendectomy and the expected postoperative morbidity in patients with a well-defined abscess, initial percutaneous drainage has become an attractive option in this patient population. This strategy allows for a laparoscopic appendectomy to be performed in an elective manner at the convenience of the surgeon. However, the medical burden on the patient and on the quality of patient outcomes has not been described in the literature. Therefore, we audited our experience with initial percutaneous drainage followed by laparoscopic interval appendectomy to evaluate the need for a prospective trial.
Methods
After institutional review board approval, a retrospective chart review was performed on all children who presented with perforated appendicitis and a well-defined abscess and were treated by initial percutaneous aspiration/drainage followed by interval appendectomy between January 2000 and September 2006. Continuous variables are listed with standard deviation.
Results
There were 52 patients with a mean age of 9.0 ± 3.9 years and weight of 34.4 ± 18.8 kg. The mean duration of symptoms at presentation was 8.4 ± 7.6 days. Percutaneous aspiration only was performed in 2 patients. The mean volume of fluid on initial aspiration/drain placement was 76.3 ± 81.1 mL. The mean time to appendectomy was 61.9 ± 25.2 days. The laparoscopic approach was used in 49 patients (94.2%), of which one was converted to an open operation. The mean length of hospitalization after interval appendectomy was 1.4 ± 1.4 days. A recurrent abscess developed in 17.3% of the patients. Six patients (11.5%) required another drainage procedure. The mean total charge to the patients was $40,414.02. There were 4 significant drain complications (ileal perforation, colon perforation, bladder perforation, and buttock/thigh necrotizing abscess).The child with the ileal perforation after drain placement is the only patient who failed initial nonoperative therapy.
Conclusions
The use of initial percutaneous aspiration/drainage of periappendiceal abscess followed by interval appendectomy is an effective approach. However, this management poses complication risks and uses considerable resources. Therefore, this strategy should be compared with early operation in a prospective trial.
Keywords: Appendicitis, Abscess, Drainage, Interval appendectomy
Appendicitis is the most common disease requiring surgical intervention in children. Delayed presentation with perforation is a common scenario that may be complicated by a well-formed abscess. When children present with perforated appendicitis and a well-defined abscess seen on computed tomography (CT), percutaneous drainage followed by interval appendectomy usually allows for an uneventful subsequent appendectomy. The theoretical advantages of this approach to the patient include a decrease in the risk of intraoperative complications and morbidity of the postoperative course. The major advantage for the surgeon is a less arduous operation at the time of appendectomy. Although these advantages have led to widespread application of drainage/interval appendectomy, there are little data published describing how these patients fare during the interval between abscess drainage and operation. Furthermore, the utilization of resources for the management of perforated appendicitis and intraabdominal abscess with subsequent interval appendectomy has not been addressed. Therefore, we reviewed our experience with initial percutaneous drainage followed by interval appendectomy for patients who presented with a well-defined abscess.
1. Methods
After institutional review board approval (06 11-166X), a retrospective chart review of all patients treated with percutaneous drainage/aspiration followed by interval appendectomy was performed. The period of data collection was from January 2000 to September 2006. Collected data points included the patient’s age, weight, duration of symptoms, drainage procedure, initial length of hospitalization, and time to interval appendectomy. Outcomes included the total number of CT scans, total length of hospitalization, total charges, recurrent abscess rates, further drainage procedures, and drain complications. Descriptive statistics are listed as mean ± standard deviation for continuous variables.
2. Results
There were 52 patients treated with interval appendectomy during the study period. The mean age of this population was 9.0 ± 3.9 years, with a mean weight of 34.4 ± 18.8 kg. Sex distribution included 29 (56%) male and 23 female patients. The mean duration of symptoms per parental history was 8.4 ± 7.6 days. The images of all 52 patients were reviewed by an interventional radiologist. A percutaneous drain was placed in 37 (71%) patients, whereas 2 patients underwent percutaneous aspiration only. No drainage was attempted in 13 patients because of concern about injuring other structures, especially small bowel. The mean volume of fluid recovered at the time of initial drainage was 76.3 ± 81.1 mL, and the mean number of days with a drain was 6.4 ± 7.0. Mean hospital stay after presentation was 5.4 ± 3.7 days. Outcomes from admission to conclusion of care are depicted in Table 1. During the interval period, we observed a mean of 7.6 ± 2.8 health care visits per patient including hospital admissions, of which 16 patients underwent at least one evaluation for continued abdominal pain and/or fever in the emergency department.
Table 1.
Overall outcomes from interval appendectomy
| Parameter (per patient) | Mean ± SD |
|---|---|
| No. of CT scans | 3.5 ± 2.0 |
| Total hospital days | 7.0 ± 3.9 |
| Total days of drainage | 6.4 ± 7.0 |
| No. of health care visits | 7.6 ± 2.8 |
| Recurrent abscess | 17.3% |
| Repeated drainage | 11.5% |
Interval appendectomy was performed at a mean of 61.9 ± 25.2 days after initial presentation (Fig. 1). The mean hospitalization after interval appendectomy was 1.4 ± 1.4 days. The mean total charge to the patient was $40,414.02 (Table 2). There were 4 major complications from percutaneous drainage: one ileal perforation, one colonic perforation, one bladder perforation, and one buttock/thigh necrotizing abscess. The only patient requiring early operation was the child who developed the ileal perforation after percutaneous drain insertion.
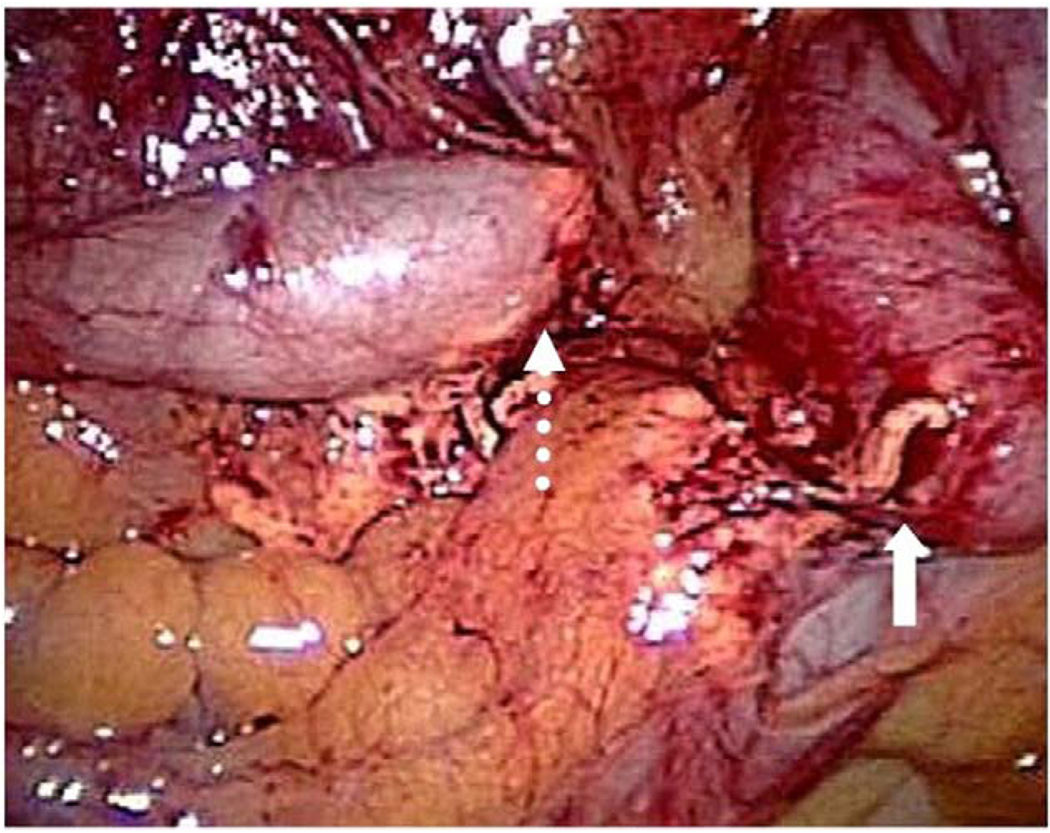
Fig. 1.
This operative photograph, taken at the time of laparoscopic interval appendectomy, shows that the appendix (dotted arrow) is completely disconnected from the cecum (solid arrow). Such a finding emphasizes the need for interval appendectomy in patients initially treated nonoperatively.
Table 2.
Mean charges to patient
| Narcotics | Medication charges | Antibiotic charges | Radiology charges | Hospital charges | Total charges | |
|---|---|---|---|---|---|---|
| Mean | $500.0 | $5050.20 | $1946.04 | $17,146.62 | $18,217.21 | $40,414.02 |
| SD | $363.6 | $4393.99 | $2203.17 | $9169.25 | $9842.07 | $20,046.68 |
Only one complication developed after interval appendectomy. A 9-year–old boy who had previously undergone liver transplantation developed a pelvic phlegmon that responded to intravenous antibiotics. Neither drainage nor exploration was needed.
3. Discussion
Perforated appendicitis remains a common surgical problem in children, although the optimum treatment remains unclear. Nonoperative management for perforated appendicitis with abscess followed by interval appendectomy was described more than 25 years ago [1], and it is practiced by many pediatric surgeons [2]. In a patient with an abscess on presentation, percutaneous drainage is an additional modality to nonoperative management [3]. The safety and efficacy of interval appendectomy have been described in a few studies [4,5]. However, there is no concurrent comparative data available describing how the patients with percutaneous drainage fare in comparison with a cohort undergoing early operation. In our series, 52 patients were initially managed with initial nonoperative therapy, with most patients having percutaneous drainage. However, 13 patients were treated with intravenous antibiotics without drainage. This management strategy is similar to a previous survey of pediatric surgeons [6]. Mean length of hospitalization after initial presentation was around 5 days, which in our practice is the time at which they are tolerating regular diet. Because patients are discharged with intravenous access to continue antibiotics at home, they do not need to defervesce before discharge. In our experience, the mean 5-day stay suggests that recovery after drainage is similar to recovery after appendectomy for perforated appendicitis. There were only 2 patients during this time frame who presented with abscess and were treated with appendectomy on presentation; thus, we cannot bring forth meaningful comparative data in this population but simply offer critical review of the interval approach.
During the interval between initial presentation and interval appendectomy, 9 recurrent abscesses developed (17.3%). In most of these (6), repeated percutaneous drainage and antibiotics were used for therapy. Two patients had small collections that could not be drained and were treated with antibiotics only. One abscess was identified at interval appendectomy. This recurrent abscess rate is very similar to the rate of postoperative abscess formation after laparoscopic appendectomy for perforated appendicitis without abscess during our recently completed prospective trial [7].
Percutaneous drainage of a well-defined abscess is an invasive procedure with inherent risks of complications. At least one percutaneous pass of a needle was performed in 39 patients, and 4 complications were noted (10%). The patient with ileal perforation has been mentioned. One patient was found on repeated CT to have the drain traversing the sigmoid colon. With no evidence of peritonitis, the patient was discharged after 1 week and readmitted 1 month later for slow removal of the drain over 4 days that allowed resolution of the fistula. The bladder perforation was managed with urinary catheter drainage for 5 days after the drain was removed. The most morbid complication resulted from a transgluteal drain for a pelvic abscess in a morbidly obese patient that led to an extremely large buttock/thigh abscess. This complicated abscess required operative drainage and debridement and resulted in a large wound that was managed with vacuum therapy. She required 3 weeks of wound care before being discharged to home with a regimen of dressing changes. The interval appendectomy was performed uneventfully in these latter 3 patients.
Computed tomographic imaging is clearly becoming more prevalent in the management of appendicitis. Recent reports in the literature concerning an increased cancer risk in children undergoing CT scans recommend radiation dose reduction for children [8,9]. Approximately one half of pediatric surgeons who completed an anonymous survey recognized this increased cancer risk [10]. In our series, the mean number of CT scans was 3.5 ± 2.0. One patient had 10 CT scans, whereas 3 patients had 7 scans. Most of these scans were ordered by our radiologists. Multiple CT scans not only increase the risk of cancer, but are a significant burden for families, especially in the outpatient setting, with missed days of work and school as well as travel expenses. Logistical considerations aside, the financial burden of these examinations quickly totals to a formidable sum. Mean radiology charges were $17,146. In the current cost-conscious era for medical care, this excessive number of CT scans is an imprudent use of imaging. The multiple health care visits (mean, 7.6 ± 2.8 per patient) seen in this population also paint an unflattering picture of how patients fare during the interval between presentation and appendectomy.
There remains a lack of consensus on the appendectomy approach for perforated appendicitis. Laparoscopic appendectomy has been reported to have advantages when compared with the open approach, including faster recovery time, less scarring, shorter postoperative hospitalization, and a decreased incidence of small bowel obstruction [11–13]. Others have found no benefit for the laparoscopic approach [14]. In our institution, laparoscopy is the current approach for all cases regardless of perforation or abscess. In our series, 3 patients early in our experience underwent an open operation, one of whom was the patient with the ileal perforation from the percutaneous drain. Another one was converted to open operation because of poor visualization of the appendiceal stump.
The time from initial presentation to interval appendectomy was previously reported at a mean of 93 days [4], which is a month longer than our series. The mean 1.4 hospital days after interval appendectomy in our series was consistent with prior published data [4].
Our experience indicates that initial nonoperative management with antibiotics with/without percutaneous drainage allows for a successful and straightforward interval laparoscopic appendectomy. However, drainage complications, persistent symptoms, recurrent abscesses, multiple CT scans, home health care visits, and an excessive financial burden are apparent detriments to this management strategy. Furthermore, a significant disruption to daily life and the mental state of patients and families can only be assumed but deserves illumination. As experience grows with laparoscopic appendectomy, it appears that the role for early operation in patients presenting with an abscess deserves to be reconsidered. Therefore, we have instituted a prospective, randomized pilot study with quality of life assessments comparing initial nonoperative management followed by interval appendectomy to early laparoscopic exploration and appendectomy in patients with perforated appendicitis and abscess.
Appendix
Discussion
Panayides, MD (Des Moines, Iowa): I was wondering did you standardize which patients received drains and which didn’t? Did you look at the size of the abscess or presence of fecoliths or factors such as that? Or is that going to be something you’re going to look at in your prospective trial?
Scott Keckler, MD (response): No, we did not look at any of those variables. I think one thing to point out is that when we did this study, we didn’t have any sort of a protocol for patients with well-defined abscess.
Thomas Inge, MD (Cincinnati, Ohio): In your justification for the RCT, do you have any sort of comparison of cost data for treatment of these complicated patients with an additional operation just to compare to that 40 number for us?
Scott Keckler, MD (response): No, we don’t have any—
Douglas Barnhart, MD (Birmingham, Alabama): I had a question, about your office visits. Having taken care of a number of patients this way, I think at least in our experience, it would be atypical to have a patient in the office seven times between the time of discharge on home IV antibiotics until their interval appendectomy is done. Can you tell us what exactly counted as an office visit and why there were so many?
Scott Keckler, MD (response): If I said office visits, I misspoke. When we say physician visits, we include office visits, trips to the emergency room as well as trips to interventional radiology for drain removal or re-CT.
Footnotes
Presented at the 59th Annual Meeting of the Section on Surgery, American Academy of Pediatrics, San Francisco, CA, October 25–27, 2007.
References
- 1.Janik JS, Ein SH, Shandling B, et al. Nonsurgical management of appendiceal mass in late presenting children. J Pediatr Surg. 1980;15:574–576. doi: 10.1016/s0022-3468(80)80776-7. [DOI] [PubMed] [Google Scholar]
- 2.Chen C, Botello C, Cooper A, et al. Current practice patterns in the treatment of perforated appendicitis in children. J Am Coll Surg. 2003;196:212–221. doi: 10.1016/S1072-7515(02)01666-6. [DOI] [PubMed] [Google Scholar]
- 3.Morrow SE, Newman KD. Current management of appendicitis. Semin Pediatr Surg. 2007;16:34–40. doi: 10.1053/j.sempedsurg.2006.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Owen A, Moore O, Marven S, et al. Interval laparoscopic appendectomy in children. J Laparoendosc Adv Surg Tech. 2006;16:308–311. doi: 10.1089/lap.2006.16.308. [DOI] [PubMed] [Google Scholar]
- 5.Weiner DZ, Katz A, Hirschl RB, et al. Interval appendectomy in perforated appendicitis. Pediatr Surg Int. 1995;10:82–85. [Google Scholar]
- 6.Muehlstedt SG, Pham TQ, Schmeling DJ. The management of pediatric appendicitis: a survey of North American Pediatric Surgeons. J Pediatr Surg. 2004;39:875–879. doi: 10.1016/j.jpedsurg.2004.02.035. [DOI] [PubMed] [Google Scholar]
- 7.St. Peter SD, Tsao K, Spilde TL, et al. Single daily dosing ceftriaxone and metronidazole versus standard triple antibiotic regimen for perforated appendicitis in children: a prospective randomized trial. J Pediatr Surg. doi: 10.1016/j.jpedsurg.2008.02.018. [Submitted] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brenner D, Elliston C, Hall E, et al. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol. 2001;176:289–296. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 9.Donnelly LF, Emery KH, Brody AS, et al. Minimizing radiation dose for pediatric body applications of single-detector helical CT. AJR Am J Roentgenol. 2001;176:303–306. doi: 10.2214/ajr.176.2.1760303. [DOI] [PubMed] [Google Scholar]
- 10.Rice HE, Frush DP, Harker MJ, et al. Peer assessment of pediatric surgeons for potential risks of radiation exposure from computed tomography scans. J Pediatr Surg. 2007;42:1157–1164. doi: 10.1016/j.jpedsurg.2007.02.007. [DOI] [PubMed] [Google Scholar]
- 11.el Ghoneimi A, Valla JS, Limonne B, et al. Laparoscopic appendectomy in children: report of 1,379 cases. J Pediatr Surg. 1994;29:786–789. doi: 10.1016/0022-3468(94)90371-9. [DOI] [PubMed] [Google Scholar]
- 12.Meguerditchian AN, Prasil P, Cloutier R, et al. Laparoscopic appendectomy in children: a favorable alternative in simple and complicated appendicitis. J Pediatr Surg. 2002;37:695–698. doi: 10.1053/jpsu.2002.32255. [DOI] [PubMed] [Google Scholar]
- 13.Tsao K, St Peter SD, Valusek PA, et al. Adhesive small bowel obstruction after appendectomy in children: comparison between the laparoscopic and open approach. J Pediatr Surg. 2007;42:939–942. doi: 10.1016/j.jpedsurg.2007.01.025. [DOI] [PubMed] [Google Scholar]
- 14.Little DC, Custer MD, May BH, et al. Laparoscopic appendectomy: an unnecessary and expensive procedure in children? J Pediatr Surg. 2002;37:310–317. doi: 10.1053/jpsu.2002.30841. [DOI] [PubMed] [Google Scholar]