Abstract
Background
The safety and efficacy of thoracoscopy for thoracic lesions and conditions in children is evolving. Our experience with thoracoscopy has expanded in recent years. Therefore, we reviewed our most recent 7-year experience to examine the current applications for thoracoscopy in children.
Methods
A retrospective review of all patients undergoing a thoracoscopic operation at Children’s Mercy Hospital (Kansas City, MO) between January 1, 2000, and June 18, 2007, was performed. Data points reviewed included patient demographics, type of operation, final diagnosis, complications, and recovery.
Results
During the study period, 230 children underwent 231 thoracoscopic procedures. The mean age was 9.6 ± 6.1 years with a mean weight of 36.6 ± 24.1 kg. Fifty percent of the patients were male. The thoracoscopic approach was used for decortication and debridement for empyema in 79 patients, wedge resection for lung lesions in 37, exposure for correction of scoliosis in 26, excision or biopsy of an extrapulmonary mass in 26, operation for spontaneous pneumothorax in 25, lung biopsy for a diffuse parenchymal process in 15, lobectomy in 9, repair of esophageal atresia with a tracheoesophageal fistula (EA-TEF) in 8, clearance of the pleural space for hemothorax or effusion in 3, diagnosis for trauma in 1, and repair of bronchopleural fistula in 1. Conversion was required in 3 patients, all of whom were undergoing a lobectomy. Two of these were right upper lobectomies and the other was a left lower lobectomy with severe infection and inflammation.
The mean time of chest tube drainage (excluding scoliosis and EA-TEF patients) was 2.9 ± 2.0 days. There were no major intraoperative thoracoscopic complications. A correct diagnosis was rendered in all patients undergoing a biopsy. One patient required a second thoracoscopic biopsy to better define a mediastinal mass. Two patients developed postoperative atelectasis after scoliosis procedures. One patient had a small persistent pneumothorax after a bleb resection for a spontaneous pneumothorax. This subsequently resolved.
Conclusions
In pediatric patients with thoracic pathology, thoracoscopy is highly effective for attaining the goal of the operation, with a low rate of conversion and complications.
INTRODUCTION
The application of thoracoscopy in the pediatric patient has advanced and expanded in the last two decades. The first significant utilization of this approach was reported in the late 1970s, limited to the pleural debridement for empyema and biopsy of intrathoracic lesions.1 Despite the initial success and early recognition of the benefits of minimal access thoracic surgery in children, its wide acceptance and use among pediatric surgeons did not emerge until the 1990s. Such advancement was based on the evolution of the instrumentation and optics as well as an understanding of the safety and management of pediatric anesthesia during thoracoscopy.2,3
Currently, with advances in the endosurgical technology, a variety of indications are recognized for thoracoscopic operations in children.4 Although the majority of procedures still include decortication for empyema and biopsy of intrathoracic lesions, its application has expanded to advanced procedures, such as the repair of esophageal atresia and the resection of mediastinal masses. Despite a plethora of literature regarding the use of thoracoscopy for specific indications, there appears to be a lack of an entire institutional review of thoracoscopic procedures in the pediatric population. Therefore, we reviewed our most recent 7-year thoracoscopic experience involving 230 patients.
METHODS
After obtaining approval from our institutional review board, a retrospective review of the medical records was performed. The study included all patients that underwent a thoracoscopic operation at Children’s Mercy Hospital (Kansas City, MO) between January 1, 2000, and June 18, 2007. Patient demographics included age and weight at the time of surgery, as well as gender. Additional patient data points included the type of thoracoscopic operation, indications for operations, final diagnosis, presence and length of the postoperative chest tube or drain, intra- and postoperative complications, and length of recovery.
RESULTS
During the study period, 230 children were identified who underwent 231 thoracoscopic operations. The average age at the time of the operation was 9.6 ± 6.1 years, while the average weight was 36.6 ± 24.1 kg. The gender distribution was exactly equal (115 boys and 115 girls).
There was a wide range of diagnostic and therapeutic applications of thoracoscopy to the study population (Table 1). Diagnostic thoracoscopic operations included wedge biopsies of solitary lung lesions in 37 patients, excision and/or biopsy of extrapulmonary masses, including chest wall and mediastinal lesions, in 26 patients, wedge biopsies of diffuse lung parenchymal disease in 15 patients, and exploration for trauma in 1 patient. Thoracoscopy for therapeutic indications included decortication for empyema in 79 patients, exposure for release, diskectomy, and fusion in 26 patients with scoliosis, operations for spontaneous pneumothorax in 25, lobectomy in 9 patients, repair of esophageal atresia and fistula (EA-TEF) in 8 patients, evacuation of the pleural space for hemothorax or simple effusions in 3, and repair of a bronchopleural fistula in 1 patient.
Table 1.
Thoracoscopic Operations at Children’s Mercy Hospital (2000–2007)
| Diagnostic | No. of patients |
|---|---|
| Wedge biopsy of solitary lung lesions | 37 |
| Biopsy and excision of mediastinal masses | 26 |
| Wedge biopsy of diffuse parenchymal disease | 15 |
| Evaluation of penetrating thoracic trauma | 1 |
| Total | 79 |
| Therapeutic | |
| Pleural decortication for empyema | 79 |
| Exposure for scoliosis | 26 |
| Bullae resection for pneumothorax | 25 |
| Lobectomy | 9 |
| Repair of esophageal atresia and fistula | 8 |
| Evacuation of hemothorax and pleural effusion | 3 |
| Repair of bronchopleural fistula | 1 |
| Total | 151 |
A wide spectrum of malignancies was diagnosed via thoracoscopy. These included alveolar soft-part sarcoma, Ewing’s sarcoma, ganglioneuroma, lymphoma, neuroblastoma, rhabdomyosarcoma, Schwannoma, Wilms’ tumor, and yolk sac tumor (Table 2).
Table 2.
Diagnosis of Malignancies in Patients Undergoing Thoracoscopy at Children’s Mercy Hospital (2000–2007)
|
Conversion to an open thoracotomy was limited to 3 patients (1.3%). All 3 were lobectomies: 2 right upper lobectomies and 1 left lower lobectomy due to severe infection and inflammation.
Postoperatively, the overall length of postoperative hospitalization was 3.8 ± 4.0 days, excluding patients who had undergone repairs of scoliosis and EA-TEF. Chest tubes were utilized in 211 patients (91%). Various types of chest tubes were inserted, including traditional, wall-suction thoracostomy tubes as well as self-containing, closed-suction bulb drainage systems (i.e., Jackson-Pratt drains), based on surgeon preference. The mean duration of postoperative tube drainage was 2.9 ± 2.0 days. These averages also excluded procedures for scoliosis exposure and repair of EA-TEF. Scoliosis patients were excluded due to the co-management relationship with the orthopedic surgeons. In addition, EA-TEF repairs were excluded due to the variable nature of esophageal atresia repairs. Of the 20 patients who did not require a postoperative chest tube or drain, these included 4 patients who underwent scoliosis exposure, while the rest were biopsies of mediastinal or parenchymal lesions.
There were no intraoperative complications. Besides the 3 conversions, 1 patient underwent a second thoracoscopic procedure to better define the mediastinal mass. Two scoliosis patients developed postoperative atelectasis. Both had postoperative chest tubes. Finally, 1 patient had a persistent small pneumothorax after a bleb resection for a spontaneous pneumothorax, which was conservatively managed and did not require any further intervention.
DISCUSSION
Minimally invasive thoracic surgery remains a staple within our institution. With advances in pediatric anesthesia and endosurgical equipment, thoracoscopy has become the primary approach for most thoracic conditions at Children’s Mercy Hospital. In addition, we have been able to expand the spectrum of disease that we approach thoracoscopically. As with most institutions, the frequency of thoracoscopy that is performed at our institution is a result of accumulated experience among surgeons and anesthesiologists. Thus, thoracoscopy is often our first choice for any thoracic operation.
Preoperative considerations
Pediatric anesthesia remains a vital component to the general success of any thoracoscopic operation.5 Whereas single-lung ventilation is a relatively easy and, often, a critical technique in adults, this maneuver may not be possible in all children. Utilization of a double-lumen endotracheal tube in children is often limited by tube and patient size. Subsequently, a variety of alternative techniques have been employed. These include the utilization of bronchial blockers, main-stem intubation, and intrathoracic insufflation. The utilization of low-flow (1–2 L/minute), low-pressure (4–6 mm Hg CO2) insufflation is often used as an adjunct to alternative endotracheal techniques to achieve ipsilateral lung collapse. In small children or neonates, intrathoracic insufflation alone may provide enough lung deflation to provide an adequate working space. This technique is utilized in the repair of esophageal atresia and fistula.
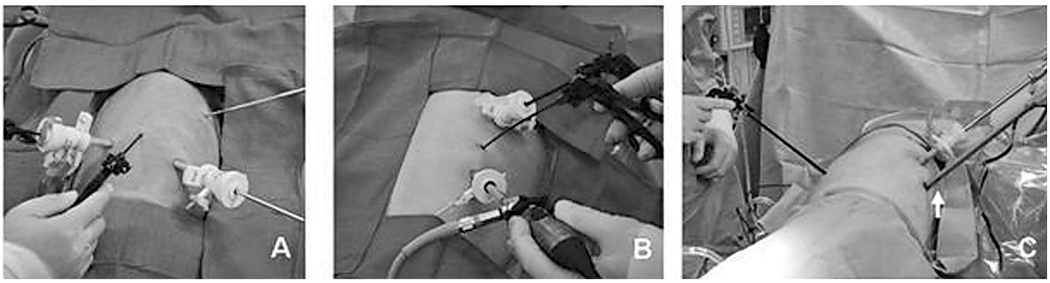
In our institution, 5- and 3-mm instruments are adequate for most thoracoscopic procedures. Valved cannulas are used sparingly and only reserved for the introduction of telescopes and various cautery and stapling devices. Instead, after the initial valved port is introduced for insufflation and the telescope, we usually utilize the stab-incision technique with the insertion of 3- and 5-mm instruments directly through the skin and chest wall6 (Fig. 1). Therefore, the utilization of cannulas is limited regardless of the patient’s age and size.
FIG. 1.
Over the past 6 years, we have begun to utilize the “stab incision” technique with the direct insertion of instruments through the skin and chest wall rather than utilizing cannulas at all working sites. On the left (A), this patient is undergoing an excision of a thoracic duplication cyst. In the center (B), the patient is undergoing a biopsy of a mediastinal mass. On the right (C), the patient is undergoing a wedge biopsy by using an endoscopic stapler (arrow), which has been directly introduced through the chest wall.
Diagnostic thoracoscopy
Thoracoscopy remains an invaluable approach for the diagnosis of intrathoracic pathology. In our study, 79 patients (34.2%) underwent a thoracoscopic procedure for diagnostic purposes. Lung biopsy was the most commonly performed procedure (52 cases). This included 37 biopsies for solitary lung lesions and 15 biopsies for diffuse parenchymal disease. In all cases, thoracoscopic biopsies were successful in achieving adequate pathologic diagnosis. There were no intra- or postoperative complications.
In addition to lung lesions, thoracoscopy was widely used for the diagnosis of mediastinal masses (26 patients). Accuracy of diagnosis was achieved in all cases. However, 1 patient underwent a second thoracoscopic mediastinal biopsy to provide additional tissue for further delineation of disease. Again, all biopsies were achieved without complications.
Thoracoscopy for malignancies within lung and mediastinal lesions remains highly accurate. We recently reported on a series of 58 patients who underwent thoracoscopy for the diagnosis of cancer.7 In all cases, the diagnosis was accurately established. This included a variety of pathologic entities (Table 2). None of the patients required conversion to open thoracotomy. Further, thoracoscopy was able to exclude two thirds of the potential malignant lesions that would otherwise require thoracotomy.
Finally, thoracoscopy was utilized in 1 patient in the setting of penetrating chest trauma. In this case, a 15-year-old patient underwent a combination of diagnostic laparoscopy and thoracoscopy after sustaining a gun shot wound to the chest. A chest tube was utilized for 1 day. The minimally invasive approach in dealing with stable pediatric trauma patients has been sparsely reported. We recently reported on the utilization of laparoscopy for a thoraco-abdominal penetrating injury in a child.8 Such minimally invasive techniques could be utilized more often in patients who are stable and have thoracic injuries. However, the efficacy and safety of this approach for this indication need further investigation.
Therapeutic thoracoscopy
As our experience with thoracoscopy has increased, we have been able to expand the realm of therapeutic interventions using the minimally invasive approach. In this study, 152 operations (65.8%) were performed for therapeutic indications. Consistent with most reports, the predominant procedure was thoracoscopic decortication or debridement for empyema (79 cases). There were no intraoperative complications. Chest tubes were placed in all cases. However, the management of postoperative tube thoracostomy has evolved during the 7-year study period. Whereas patients received traditional wall suction tubes in the early years, we have migrated to the utilization of self-containing, bulb suction devices in some of our more recent patients.9 The duration of postoperative drainage remains variable and often is based on surgeon preference. Despite our success with thoracoscopic decortication for empyema, the overall efficacy, compared to fibrinolysis, remains unclear. Although there are several small series suggesting an advantage to thoracoscopic pleural debridement, there remain no published reports directly comparing fibrinolysis and thoracoscopy.10–12 Thus, the efficacy of thoracoscopic decortication versus fibrinolysis remains to be studied.
Thoracoscopic exposure for anterior spinal release, diskectomy and fusion for the treatment of severe scoliosis was a large subgroup of patients undergoing therapeutic interventions (26 patients). However, due to the co-management system of this condition within our institution, the duration of chest tube drainage and the postoperative course were too variable to include in the overall analysis. Nonetheless, thoracoscopy was able to provide excellent exposure without any of the intra- or postoperative complications associated with procedures for scoliosis.
Resection of bullae for spontaneous pneumothorax can be easily achieved using the thoracoscopic approach (25 patients). The identification of the inciting bleb can usually be identified and, subsequently, resected using endosurgical staplers. The addition of pleurodesis was utilized in 13 patients (5 chemical, 6 mechanical, and 2 both). In all cases, the bullae were identified and resected and a chest tube was introduced. There were no intraoperative complications, although 1 patient had a persistent, stable pneumothorax after chest tube removal, which resolved with observation.
Lobectomies can be successfully achieved via thoracoscopy. In our series, 9 patients underwent formal lobectomies for intralobar sequestrations, bronchiectasis, emphysema, congenital cystic adenomatoid malformations, and chronic lung abscess. Three patients required conversion to open thoracotomy. This included 2 right upper lobectomies for emphysema and 1 left lower lobectomy for chronic abscess. Right upper lobectomies remain the most technically challenging procedures due to the close proximity of the main pulmonary arterial trunk. Conversions were due to suboptimal visualization and not due any intraoperative complications. The left lower thoracoscopic lobectomy was abandoned due to poor visualization and the inability to delineate anatomical planes. Despite these conversions, thoracoscopy still remains our initial preferred approach.
The thoracoscopic approach to the repair of esophageal atresia has been previously described.13 Our series included 8 esophageal atresia repairs with a distal tracheoesophageal fistula. All repairs were transpleural and successfully completed, although an extrapleural approach has been described.14 During the last 2 years (4 patients in this series), we have inserted a biosynthetic mesh between the esophageal anastamosis and tracheal closure.15 Currently, we have not experienced an anastamotic leak or recurrent TEF using this technique. The main operative advantage of thoracoscopy remains the excellent visualization of the posterior mediastinal structures when the ports and instruments are placed correctly. The thoracoscopic repair of EA-TEF remains a technically challenging, but achievable, operation.
Postoperative considerations
The utilization and management of chest tubes within our institution has evolved during the study period. The average duration of postoperative tube thoracostomy was 2.9 ± 2.0 days (excluding patients undergoing thoracoscopic exposure for scoliosis and esophageal atresia repair). As our experience has evolved, a large portion (20%) of the mediastinal and parenchymal wedge biopsies have been managed without a chest tube. In all these cases, the air was evacuated prior to closure of port sites. There were no symptomatic residual pneumothoraces that required subsequent chest tubes.
Postoperative management for patients undergoing thoracoscopic biopsies or limited lung resection is uncomplicated. Chest tubes, if utilized, are usually removed on the first or second postoperative day. The overall length of hospitalization (excluding scoliosis and EA-TEF patients) was 3.8 ± 4.0 days. The immediate benefits of minimal access thoracic surgery are evident, as most patients quickly transition to oral pain medications.
CONCLUSIONS
Minimally invasive surgery in the management of pediatric thoracic pathology continues to evolve with advances in instrumentation and a better understanding of pediatric anesthesia. As the spectrum of thoracoscopic operations continues to develop, the indications for these procedures have also expanded. Thus, thoracoscopy remains a highly effective application in the pediatric population with an extremely low conversion rate and minimal complications.
REFERENCES
- 1.Rodgers BM, Moazam F, Talbert JL. Thoracoscopy in children. Ann Surg. 1979;189:176–180. doi: 10.1097/00000658-197902000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rothenberg SS, Wagner JS, Chang JH, et al. The safety and efficacy of thoracoscopic lung biopsy for diagnosis and treatment in infants and children. J Pediatr Surg. 1996;31:100–103. doi: 10.1016/s0022-3468(96)90328-0. [DOI] [PubMed] [Google Scholar]
- 3.Rodgers BM. Pediatric thoracoscopy: Where have we come and what have we learned? Ann Thorac Surg. 1993;56:704–707. doi: 10.1016/0003-4975(93)90958-k. [DOI] [PubMed] [Google Scholar]
- 4.Engum SA. Minimal access thoracic surgery in the pediatric population. Semin Pediatr Surg. 2007;16:14–26. doi: 10.1053/j.sempedsurg.2006.10.003. [DOI] [PubMed] [Google Scholar]
- 5.Tobias JD. Anaesthesia for neonatal thoracic surgery. Best Pract Res Clin Anaesthesiol. 2004;18:303–320. doi: 10.1016/j.bpa.2003.11.005. [DOI] [PubMed] [Google Scholar]
- 6.Ostlie DJ, Holcomb GW. The use of stab incisions for instrument access in laparoscopic operations. J Pediatr Surg. 2003;38:1837–1840. doi: 10.1016/j.jpedsurg.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 7.Nair A, St. Peter SD, Tsao K, et al. Thoracoscopy for malignancy in children. Surg Endosc. 2007;21:S476. [Google Scholar]
- 8.Garg NT, St. Peter SD, Tsao K, et al. Minimally invasive management of penetrating throracoabdominal trauma in a child. J Trauma. 2006;61:211–212. doi: 10.1097/01.ta.0000202468.51113.15. [DOI] [PubMed] [Google Scholar]
- 9.Valusek PA, Tsao K, St. Peter SD, et al. A comparison of chest tubes versus bulb suction drains in pediatric thoracic surgery. J Pediatr Surg. 2007;42:812–814. doi: 10.1016/j.jpedsurg.2006.12.061. [DOI] [PubMed] [Google Scholar]
- 10.Padman R, King KA, Iqbal S, et al. Parapneumonic effusion and empyema in children: Retrospective review of the duPont experience. Clin Pediatr. 2007;46:518–522. doi: 10.1177/0009922806299096. [DOI] [PubMed] [Google Scholar]
- 11.Dzielicki J, Korlacki W. The role of thoracoscopy in the treatment of pleural empyema in children. Surg Endosc. 2006;20:1402–1405. doi: 10.1007/s00464-005-0750-0. [DOI] [PubMed] [Google Scholar]
- 12.Avansino JR, Goldman B, Sawin RS, et al. Primary operative versus nonoperative therapy for pediatric empyema: A meta-analysis. Pediatrics. 2005;115:1652–1659. doi: 10.1542/peds.2004-1405. [DOI] [PubMed] [Google Scholar]
- 13.Holcomb GW, Rothenberg SS, Bax KM, et al. Thoracoscopic repair of esophageal atresia and tracheoesophageal fistula: A multi-institutional analysis. Ann Surg. 2005;242:422–428. doi: 10.1097/01.sla.0000179649.15576.db. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tsao K, Lee H. Extrapleural thoracoscopic repair of esophageal atresia with tracheo-esophageal fistula. Pediatr Surg Intl. 2005;21:308–310. doi: 10.1007/s00383-005-1366-0. [DOI] [PubMed] [Google Scholar]
- 15.St. Peter SD, Calkins CM, Holcomb GW. The use of biosynthetic mesh to separate the anastomoses during the thoracoscopic repair of esophageal atresia and tracheoesophageal fistula. J Laparoendosc Adv Surg Tech A. 2007;17:380–382. doi: 10.1089/lap.2006.0138. [DOI] [PubMed] [Google Scholar]