Abstract

Following scoliosis surgery, lumbar motion segment degeneration below the level of fusion is not uncommon. Especially long fusions extending to the mid and lower lumbar spine increase the likelihood of degeneration of the remaining motion segments. The management for these patients is controversial and depends on the clinical presentation and level of degeneration. The increasing confidence in motion-preserving technology leads to a dilemma on whether to fuse the remaining lumbar levels or risk utilising disc arthroplasty to preserve the remaining motion segments and facilitate coronal balance in patients with previous long fusion for scoliosis. We present an interesting case of a 44-year-old lady, who underwent two-stage corrective surgery for progressive idiopathic scoliosis at the age of 22 years. In the first stage, she had T11–L3 anterior fusion, whilst in the second stage posterior fusion was done from T5 to L3. At 22 years after the initial surgery, she presented with worsening low back pain and bilateral L4 radicular symptoms. MRI scan confirmed severe disc degeneration at L3–4 and L5–S1 levels with preserved L4–5 disc. She initially underwent L3–L4 decompression and posterolateral fusion at that level, which relieved her radicular symptoms. However, she had persistent pain at the lumbosacral junction with Modic I changes. The options of an anterior L5–S1 fusion or disc replacement were considered and discussed with the patient. The disc replacement option was decided upon with the patient, as anterior fusion was judged to increase the risk of coronal imbalance. At the 1-year follow-up, she reported significant improvement in the back pain. The radiographs at 1 year showed satisfactory position and function of the artificial disc replacement. The disc was flexed laterally, accommodating the coronal balance of the spine. We conclude that L5–S1 motion segment can be preserved with artificial disc replacement in patients with previous long fusion for scoliosis surgery. The real difficulty arises when choosing between disc replacement and extension of fusion. In our patient, the disc replacement has worked well so far. However, the disc is clearly at a mechanical disadvantage, and loss of function in the mid- or long term would not be surprising.
Keywords: Scoliosis, Lumbar fusion, Lumbar disc arthroplasty, Lumbar disc degeneration
Case presentation
We present the case of a 44-year-old lady who had artificial disc replacement at the L5–S1 level with two previous fusion surgeries for scoliosis.
The first presentation was at the age of 22 years with obvious deformity, worsening back pain and costopelvic impingement. She underwent planned two-stage surgery for correction of scoliosis. In the first stage, she had T11 to L3 anterior fusion and in the second stage a posterior fusion was performed from T5 to L3 using the Harrington instrumentation. At 22 years after the initial surgery, she presented with low back pain and bilateral L4 radicular symptoms. MRI scan showed degenerative disc disease at L3–4 and L5–S1 with relatively preserved L4–5 disc. This was confirmed with lumbar discography, which showed concordant pain at L3–4 and L5–S1 and was negative at L4–5. In view of her bilateral radicular symptoms, she initially underwent L3–4 decompression and instrumented posterolateral fusion, which relieved her radicular symptoms. However, she had persistent pain at the lumbosacral junction with Modic I changes at the L5–S1 level. The surgical options of anterior fusion and disc replacement were considered and discussed in detail with the patient. The disc replacement option was chosen as the anterior fusion was judged to increase the risk of coronal imbalance. L5–S1 disc replacement resulted in immediate improvement in her back pain.
At the 1-year follow-up, she reported significant improvement in her back pain and reduction in the requirement of analgesic medicines. Radiographs showed satisfactory position of artificial disc replacement.
Diagnostic imaging section
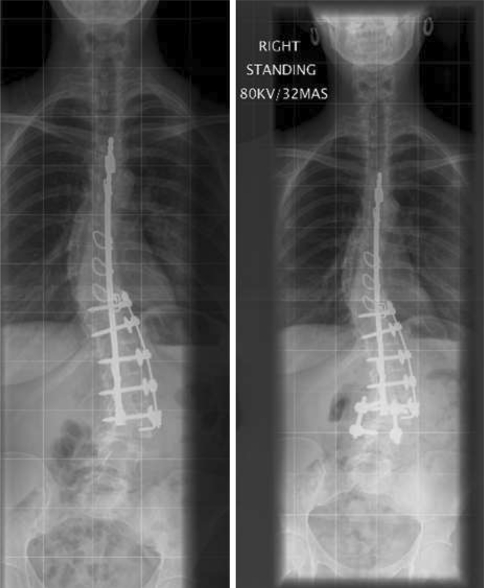
Figure 1 shows the AP X-rays before and after L3–4 fusion, but before disc replacement at the L5–S1 level.
Figure 2 shows lateral X-rays before and after L3–4 fusion, but before disc replacement at the L5–S1 level.
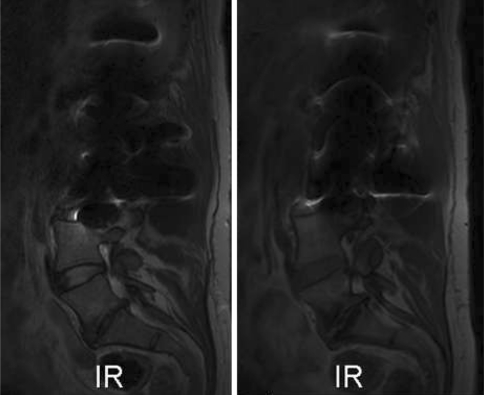
Figure 3 shows T1 and T2-weighted MR images of the lumbar spine. The L3–4 level is obscured due to the old steel implants.
Fig. 1.
AP X-rays before (left) and after (right) L3–4 fusion
Fig. 2.
Lateral images before (left) and after (right) L3–4 fusion
Fig. 3.
Pre-operative MRI scan showing severe disc degeneration at the L5–S1 level. T2-weighted image on the left and T1 image on the right
Historical review the condition, epidemiology, diagnosis, pathology and differential diagnosis
Scoliosis was described for the first time by Hippocrates in the fifth century BC, but the first surgical attempts to treat scoliosis started in the mid and late nineteenth century [15]. The Harrington distraction system, developed in 1955, clearly had the advantage of achieving and maintaining maximal correction of deformity. The comparison between Harrington instrumentation and Risser localiser cast was carried out by Moe and Valuska in 1966, who found that the instrumented group showed better outcome in terms of curve correction and ambulation [14]. However, the distractive kyphotic effect of Harrington instrumentation can lead to a flat lumbar spine. These patients in the long run can develop secondary degeneration below the level of fusion [1]. Some studies have shown that incidence of adjacent segment disease ranges from 5.2% with few fused levels to 18.5% in longer constructions [16]. In a retrospective study of 31 patients, Kuhns et al. [9] reported that 69% of patients developed severe degenerative disc disease of L5–S1 after long fusions to L5. Initially, the intervertebral disc below a long fusion for scoliosis reacts to biomechanical stimuli by increase in size [17]. The disc height then decreases with time eventually leading to degenerative disease of the disc [13]. These patients usually present with low back pain with or without leg pain [2], and the intervertebral disc or facet joints can be the source of pain [3]. The evaluation of the source of pain in the degenerative spine is crucial as this can affect the management plan [1]. MR imaging can show the degenerative disc, especially Modic changes can help in the diagnosis of discogenic low back pain [18]. However, sometimes diagnostic disc injections and facet blocks are necessary to evaluate the source of pain [1].
Rational for treatment and evidence-based literature
In this case, the choice was between two logical options: to extend the fusion to L5–S1 or replace the L5–S1 disc. There is evidence in literature that long primary fusions or extension of fusion to more distal lumbar levels can increase the likelihood of complications [4, 5, 8]. Amongst these complications, pseudarthrosis is the most prevalent and this is commonly seen in patients who undergo extensions of fusion [16]. Extending a lumbar fusion to the sacrum can also adversely change the load on both hips and sacroiliac joints [1].
Artificial disc replacement below a long fusion has its own advantages and disadvantages. At the L5–S1 level, it can preserve the last motion segment. This is important because in case of L5–S1 fusion, non-union can result due to undesirable mechanical conditions between the two major lever arms of the rigid pelvis and fused spine [1]. Ronald et al. [10] reported good clinical outcome after artificial disc replacement with a 2-year follow-up at L5–S1 below a long thoracolumbar fusion for scoliosis surgery. Lenke et al. [11] in a biomechanical study of human spines, attempted to demonstrate that addition of one artificial disc below a long fusion provided biomechanical stability and motion properties similar to that of an intact intervertebral disc. In addition, a single level disc replacement has been reported to have significantly less operative time, less blood loss and less hospital stay and it is more cost-effective compared to the 1-level circumferential fusion [7, 19]. However, the unconstrained total disc replacement systems cannot restore rotational stability in the lumbar spine and potentially can increase the deforming loads at the adjacent disc [12]. Additionally, if revision becomes inevitable after disc arthroplasty, it is not only technically challenging but also increases the risk of vascular injury [6].
In our case, the options of fusion and disc replacement were discussed in detail with the patient. Fusion was thought to increase the risk of coronal imbalance and further surgery. In the light of the available evidence and patient’s wishes, the disc replacement choice was considered to be more feasible. With previous scoliosis, a semiconstrained disc (Prodisc) was thought to be better than an unconstrained disc (Charite), because we wanted to restrict any rotational or translatory motion at this level. However, if we had considered fusion, we would have performed anterior fusion only at the L5–S1 level as the discogram was negative at the L4–5 level.
Procedure
A right paramedian incision was made as the patient previously had left anterior surgery for lumbar scoliosis correction. The L5–S1 disc area was exposed via a retroperitoneal approach. Anterior discectomy with release followed by insertion of a Prodisc artificial disc was carried out at that level. Severe disc degeneration was noted. There were no intra-operative or post-operative complications.
Procedure imaging section
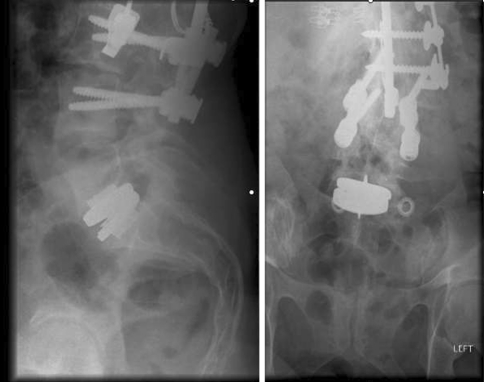
Figure 4 shows AP and lateral views of the lumbar spine at 3 months after surgery.
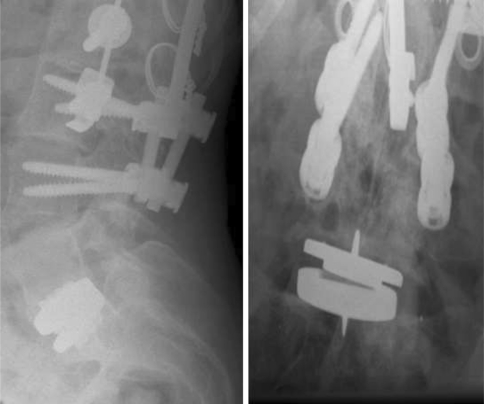
Figure 5 shows the targeted lumbosacral AP and lateral views at the 1-year follow-up with some lateral flexion of the disc.
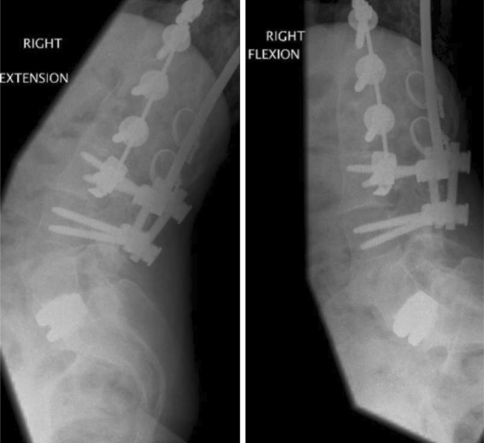
Figure 6 illustrates the flexion and extension views of the lower lumbar spine with artificial disc in situ at the 1-year follow-up.
Fig. 4.
Post-operative radiographs 3 months after disc replacement
Fig. 5.
Radiographs 1 year after disc replacement. Targeted lumbosacral AP radiograph on the right shows some lateral flexion of disc to accommodate coronal balance
Fig. 6.
Flexion and extension radiographs at the 1-year follow-up
Outcome and follow up
At the 1-year follow-up, the patient reported marked improvement in back pain. The analgesic requirement for back pain was also reduced to a minimum level. The artificial disc exhibits flexion to the left (Fig. 5) in accordance with the clinically maintained coronal balance of the patient.
References
- 1.Aebi M. The adult scoliosis. Eur Spine J. 2005;14:925–948. doi: 10.1007/s00586-005-1053-9. [DOI] [PubMed] [Google Scholar]
- 2.Berg S, Tullberg T, Branth B, Olerud C, Tropp H. Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J. 2009;18:1512–1519. doi: 10.1007/s00586-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kleuver M, Oner FC, Jacobs WC. Total disc replacement for chronic low back pain: background and a systematic review of the literature. Eur Spine J. 2003;12:108–116. doi: 10.1007/s00586-002-0500-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Eck KR, Bridwell KH, Ungacta FF, Riew KD, Lapp MA, Lenke LG, Baldus C, Blanke K. Complications and results of long adult deformity fusions down to L4, L5, and the sacrum. Spine. 2001;26:E182–E192. doi: 10.1097/00007632-200105010-00012. [DOI] [PubMed] [Google Scholar]
- 5.Emami A, Deviren V, Berven S, Smith JA, Hu SS, Bradford DS. Outcome and complications of long fusions to the sacrum in adult spine deformity: Luque–Galveston, combined iliac and sacral screws, and sacral fixation. Spine. 2002;27:776–786. doi: 10.1097/00007632-200204010-00017. [DOI] [PubMed] [Google Scholar]
- 6.Freeman BJ, Davenport J. Total disc replacement in the lumbar spine: a systematic review of the literature. Eur Spine J. 2006;15:S439–S447. doi: 10.1007/s00586-006-0186-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Guyer RD, Tromanhauser SG, Regan JJ. An economic model of one-level lumbar arthroplasty versus fusion. Spine J. 2007;7:558–562. doi: 10.1016/j.spinee.2006.09.006. [DOI] [PubMed] [Google Scholar]
- 8.Kostuik JP, Hall BB. Spinal fusions to the sacrum in adults with scoliosis. Spine. 1983;8:489–500. doi: 10.1097/00007632-198307000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Kuhns CA, Bridwell KH, Lenke LG, Amor C, Lehman RA, Buchowski JM, Edwards C, II, Christine B. Thoracolumbar deformity arthrodesis stopping at L5: fate of the L5–S1 disc, minimum 5-year follow-up. Spine. 2007;32:2771–2776. doi: 10.1097/BRS.0b013e31815a7ece. [DOI] [PubMed] [Google Scholar]
- 10.Lehman RA, Jr, Lenke LG. Long-segment fusion of the thoracolumbar spine in conjunction with a motion-preserving artificial disc replacement: case report and review of the literature. Spine. 2007;32:E240–E245. doi: 10.1097/01.brs.0000259211.22036.2a. [DOI] [PubMed] [Google Scholar]
- 11.Lenke LG, Eiserman L, Bilancini ME et al (2004) Biomechanics of disc arthroplasty below a simulated long spinal fusion construct: is it stable and feasible? In: Paper presented at 68th international meeting on advanced spine techniques (IMAST) 11th Annual Meeting, July 1–3, South Hampton, Bermuda
- 12.McAfee PC, Cunningham BW, Hayes V, Sidiqi F, Dabbah M, Sefter JC, Hu N, Beatson H. Biomechanical analysis of rotational motions after disc arthroplasty: implications for patients with adult deformities. Spine. 2006;31:S152–S160. doi: 10.1097/01.brs.0000234782.89031.03. [DOI] [PubMed] [Google Scholar]
- 13.Miyakoshi N, Abe E, Shimada Y, Okuyama K, Suzuki T, Sato K. Outcome of one-level posterior lumbar interbody fusion for spondylolisthesis and postoperative intervertebral disc degeneration adjacent to the fusion. Spine. 2000;25:1837–1842. doi: 10.1097/00007632-200007150-00016. [DOI] [PubMed] [Google Scholar]
- 14.Moe JH, Valuska JW. Evaluation of treatment of scoliosis by Harrington instrumentation. J Bone Joint Surg. 1966;48:1656–1657. [Google Scholar]
- 15.Moen KY, Nachemson AL. Treatment of scoliosis a historical perspective. Spine. 1999;24(24):2570–2575. doi: 10.1097/00007632-199912150-00003. [DOI] [PubMed] [Google Scholar]
- 16.Quirno M, Kamerlink JR, Valdevit A, Kang M, Yaszay B, Duncan N, Boachie-Adjei O, Lonner BS, Errico TJ. Biomechanical analysis of a disc prosthesis distal to a scoliosis model. Spine. 2009;34:1470–1475. doi: 10.1097/BRS.0b013e3181a8e418. [DOI] [PubMed] [Google Scholar]
- 17.Violas P, Estivalezes E, Briot J, Sales de Gauzy J, Swider P. Quantification of intervertebral disc volume properties below spine fusion, using magnetic resonance imaging, in adolescent idiopathic scoliosis surgery. Spine. 2007;32:E405–E412. doi: 10.1097/BRS.0b013e318074d69f. [DOI] [PubMed] [Google Scholar]
- 18.Zhang YH, Zhao CQ, Jiang LS, Chen XD, Dai LY. Modic changes: a systematic review of the literature. Eur Spine J. 2008;17:1289–1299. doi: 10.1007/s00586-008-0758-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zigler J, Delamarter R, Spivak et al (2007) Results of the prospective, randomized, multicenter Food and Drug Administration investigational device exemption study of the ProDisc-L total disc replacement versus circumferential fusion for the treatment of 1-level degenerative disc disease. Spine 32:1155–1162 (discussion 1163) [DOI] [PubMed]