Abstract
This study investigated the preoperative morphology and postoperative fusion of the atlanto-axial joint (AAJ) in patients with atlanto-axial subluxation (AAS) due to rheumatoid arthritis (RA) using computed tomography (CT). Furthermore, we examined the relationship between the preoperative morphology of AAJ and other radiographic results. Thirty patients with AAS due to RA treated by C1–2 transarticular screw fixation (TSF) were reviewed. The morphology of the AAJ was evaluated using sagittal reconstruction views on CT before and 1 year after surgery. Thereafter, the atlanto-dental interval (ADI) value at the neutral and maximal flexion position and atlanto-axial angle (AAA) at the neutral position was assessed in preoperative lateral cervical radiographs. The preoperative morphology of the AAJ on CT reconstruction views was graded as follows: Grade 1 showed maintenance of the joint space, Grade 2 showed the joint space narrowing and Grade 3 showed the destructive abnormality of subchondral bone. After surgery, the ADI value at the neutral position was assessed in lateral cervical radiographs. Furthermore, the fusion in the AAJ was investigated using CT sagittal reconstruction views taken 1 year after surgery. The preoperative CT image of the AAJ demonstrated Grade 1 in 12 cases (Group A), Grade 2 in 9 cases (Group B) and Grade 3 in 9 cases (Group C). There was no significant difference in age, gender and duration of RA among the three groups. The average ADI value at the flexion position was 11.0 mm in Group A, 12.3 mm in Group B and 12.7 mm in Group C (p > 0.313). The average ADI value at the neutral position before surgery was 4.5 mm in Group A, 7.3 mm in Group B and 11.4 mm in Group C (p < 0.003). The mean AAA value was 20.8° in Group A, 21.8° in Group B and 8.4° in Group C (p < 0.033). The average ADI value after TSF was 1.7 mm in Group A, 2.1 mm in Group B and 3.0 mm in Group C (p > 0.144). Fusion in the AAJ 1 year after surgery was demonstrated in 14 cases (46.7%; Group A, 0 case; Group B, 5 cases; Group C, 9 cases). According to the preoperative grading of the AAJ, the postoperative fusion in the AAJ was demonstrated in 0 of 32 joints (0%) in Grade 1, 7 of 18 joints (38.9%) in Grade 2 and all of 10 joints (100%) in Grade 3. In conclusion, this study showed that a destructive abnormality of subchondral bone in the AAJ induced an enlargement of the ADI and anterior inclination of the atlas in patients with AAS due to RA. The current study also showed that fusion in the AAJ was demonstrated in 14 of 30 patients after C1/2 TSF. This was easy to recognize in AAS patients whose joint destruction extended to the subchondral bone.
Keywords: Atlanto-axial subluxation, Atlanto-axial joint, Rheumatoid arthritis
Introduction
Atlanto-axial subluxation (AAS) occurs with marked frequency in patients with disorders of the upper cervical spine due to rheumatoid arthritis (RA). Matsunaga et al. [7] noted that 21 patients who had myelopathy caused by irreducible atlanto-axial instability and were treated by conservatively, all became bedridden within 3 years after the onset of myelopathy, and the survival rate was 0% in the first 8 years. Atlanto-axial transarticular screw fixation (TSF) is the common treatment for such instability [2, 6]. The fusion mass between the C1 posterior arch and C2 lamina must be examined to determine whether fusion has been achieved after atlanto-axial arthrodesis [9]. However, Ito et al. [5] reported that in patients with AAS due to RA, atlanto-axial transarticular screws achieved fusion in the atlanto-axial joint (AAJ) and yielding a stable C1–2 even with posterior graft failure. In fact, they noted facet fusion and a stable C1/2 in 5 out of 7 patients that showed posterior graft failure. Iizuka et al. [4] investigated the morphology of the atlanto-occipital joint in AAS patients due to RA using computed tomography; however, no study has so far evaluated the AAJ before atlanto-axial arthrodesis. Therefore, this study investigated the preoperative morphology and postoperative fusion of the AAJ in patients with AAS due to RA using computed tomography (CT). Furthermore, we examined the relationship between the preoperative morphology of AAJ and other radiographic results.
Materials and methods
Thirty-four patients with AAS due to RA treated by C1–2 TSF between September 2001 and May 2008 were reviewed. Two patients of the 34 patients died from causes unrelated to the procedure. Finally, 31 of remaining 32 patients had sufficient clinical and radiographic follow-up for analysis: the follow-up rate was 91.2%. The subjects included 19 females and 12 males. The average patient age at the time of surgery was 58.4 years (34–75). The preoperative duration of RA ranged from 3 to 35 years, and the mean was 14.2 years. AAS is defined as an atlanto-dental interval (ADI, distance between odontoid process and the posterior border of the anterior arch of the atlas) of greater than 3 mm as measured on plain radiography. In patients with cervical myelopathy with atlanto-axial instability, surgery was usually indicated. Surgery was also used when the patients complained of only neck pain, after unsuccessful conservative treatment.
All patients had reducible subluxation, therefore, they underwent selective C1–2 TSF using a cannulated cancellous screw (diameter 4.0 mm) with modified McGraw [8] techniques using ultra-high-molecular weight polyethylene cables, and the iliac bone was grafted on the inter-laminar region, but it was not grafted directly into the AAJ. Patients were mostly instructed to wear a cervical collar for 8 weeks after the surgery.
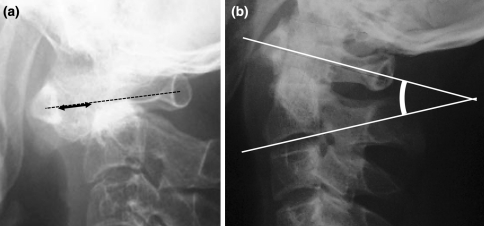
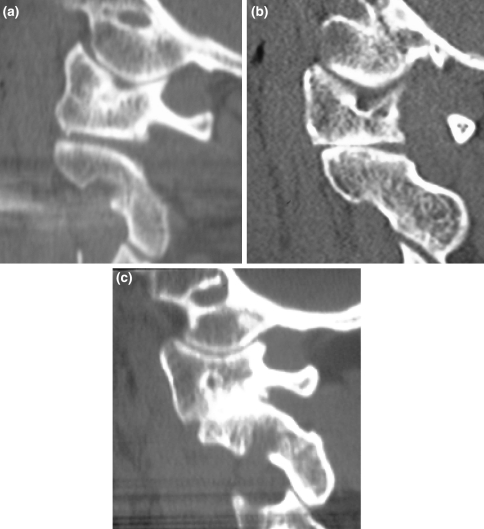
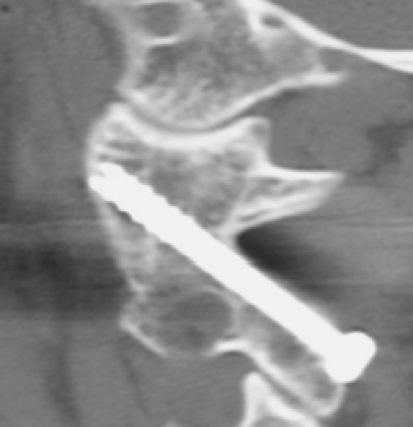
The morphology of the AAJ was evaluated using sagittal reconstruction views (slice thickness 2 mm) on computed tomography (CT: Light Speed Qx-I, GE, slice thickness 0.5–1.25 mm) before and 1 year after surgery. Thereafter, the ADI value at the neutral and maximal flexion position and atlanto-axial angle (AAA) at the neutral position was assessed in preoperative lateral cervical radiographs (Fig. 1). The preoperative morphology of the AAJ on CT reconstruction views was graded as follows: Grade 1 showed maintenance of the joint space (Fig. 2a), Grade 2 showed the joint space narrowing (Fig. 2b) and Grade 3 showed the destructive abnormality of subchondral bone (Fig. 2c). After surgery, the ADI value at the neutral position was assessed in lateral cervical radiographs. Furthermore, the fusion in the AAJ was investigated using CT sagittal reconstruction views taken 1 year after surgery. The fusion in the AAJ was defined as the bony continuity in at least two slices on each CT sagittal reconstruction view (Fig. 3). The morphological evaluation of the AAJ before and after surgery was conducted by the first author (Y.S.) who did not perform these operations. The ADI and AAA values were analyzed using ANOVA and Fisher’s PLSD test for an analysis of variance and the post hoc test.
Fig. 1.
Method of radiological measurement. a Atlanto-dental interval (ADI). b Atlanto-axial angle (AAA)
Fig. 2.
Classification of morphology of the atlanto-axial joint on CT sagittal reconstruction view before surgery. a Grade 1, b Grade 2, c Grade 3
Fig. 3.
Fusion of the atlanto-axial joint on CT after surgery
Results
One patient developed pseudoarthrosis and required more extensive surgery, such as occipito-cervical fusion within 1 year after surgery; therefore, the remaining 30 cases were thus evaluated. Regarding fusion mass in inter-laminar region, we found two patients that demonstrated pseudoarthrosis, but did not perform any additional surgery. The preoperative CT sagittal reconstruction image of the AAJ demonstrated Grade 1 bilaterally in 12 cases (Group A), Grade 2 on at least one side of the AAJ in 9 cases (Group B: one side, 5 cases; both sides, 4 cases) and Grade 3 on at least one side of the AAJ in 9 cases (Group C: one side, 8 cases; both sides, 1 cases). The average age at surgery in Group A, Group B and Group C was 61.0, 54.7 and 58.7 years, respectively. The mean preoperative duration of RA in each group was 14.3, 12.9 and 15.3 years, respectively. There was no significant difference in those values among the three groups. These findings are summarized Table 1.
Table 1.
Summary of the background data
| Group A (n = 12) | Group B (n = 9) | Group C (n = 9) | |
|---|---|---|---|
| Gender (female/male) | 7/5 | 6/3 | 6/3 |
| Age | 61.0 ± 10.3 | 54.7 ± 10.9 | 58.7 ± 10.7 |
| Duration of RA (year) | 14.3 ± 9.1 | 12.9 ± 4.9 | 15.3 ± 10.1 |
The average ADI value at the flexion position was 11.0 mm in Group A, 12.3 mm in Group B and 12.7 mm in Group C. There was no significant difference among those groups (p > 0.313). The average ADI value at the neutral position before surgery was 4.5 mm in Group A, 7.3 mm in Group B and 11.4 mm in Group C (Table 2). There was a significant difference among these groups (p < 0.003). There was no significant difference between Groups A and B (p > 0.118), however, there was a significant difference between Groups A and C (p < 0.001), and Groups B and C (p < 0.038). The mean AAA value was 20.8° in Group A, 21.8° in Group B and 8.4° in Group C (Table 2). There was a significant difference among those groups (p < 0.033). There was no significant difference between Groups A and B (p > 0.853), however, there was a significant difference between Groups A and C (p < 0.022), and Groups B and C (p < 0.021). The average ADI value after TSF was 1.7 mm in Group A, 2.1 mm in Group B and 3.0 mm in Group C. There was no significant difference among these groups (p > 0.144).
Table 2.
Summary of the radiological data
| Group A (n = 12) | Group B (n = 9) | Group C (n = 9) | |
|---|---|---|---|
| ADI (pre-op) flexion (mm) | 11.0 ± 2.3 | 12.3 ± 1.9 | 12.7 ± 3.5 |
| ADI (pre-op) neutral (mm) | 4.5 ± 3.5 | 7.3 ± 4.5 | 11.4 ± 4.1 |
| AAA (pre-op) | 20.8° ± 10.4° | 21.8° ± 12.1° | 8.4° ± 12.3° |
| ADI (post-op) | 1.7 ± 1.4 | 2.1 ± 1.5 | 3.0 ± 1.2 |
Fusion in the AAJ 1 year after surgery was demonstrated in 14 cases (46.7%; Group A, 0 case; Group B, 5 cases; Group C, 9 cases). According to the preoperative grading of the AAJ, the postoperative fusion in the AAJ was demonstrated in 0 of 32 joints (0%) in Grade 1, 7 of 18 joints (38.9%) in Grade 2 and all of 10 joints (100%) in Grade 3 (Table 3).
Table 3.
Fusion rate in the atlanto-axial joint after surgery
| Grade 1 (n = 32) | Grade 2 (n = 18) | Grade 3 (n = 10) | |
|---|---|---|---|
| Fusion in the AAJ | 0 | 7 | 10 |
| % | 0 | 38.9 | 100 |
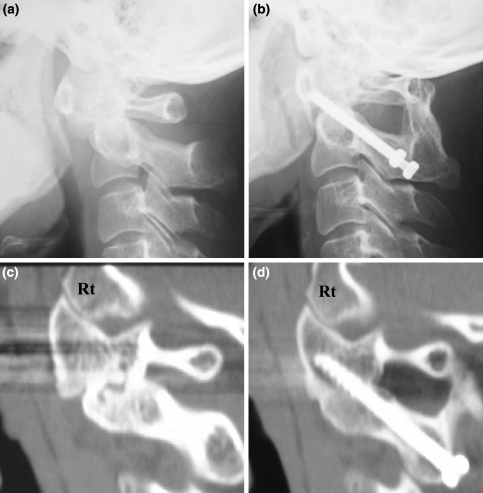
Case report
A 37-year-old female showed AAS involvement in the neutral position and was treated by C1–2 transarticular screw fixation (Fig. 4a, b). Destructive change was observed on the right side of the AAJ (Fig. 4c). Fusion in the right AAJ was clearly demonstrated after surgery (Fig. 4d).
Fig. 4.
Case 14: a 37-year-old female was treated by C1–2 transarticular screw fixation. CT reconstruction view before surgery showing Grade 3 joint destruction of the AAJ on right side. The fusion in the right AAJ was demonstrated 1 year after surgery. a Preop, b 1 year post-op, c pre-op sagittal reconstruction view of AAJ on right side, d 1 year post-op reconstruction view of AAJ on right side
Discussion
Regarding the results after C1/2 arthrodesis in AAS patients due to RA, Grob et al. [3] noted that once atlanto-axial arthrodesis was achieved in AAS patients, the resolution of the inflammatory process with destruction of the lateral masses of the atlas prevented further deterioration with vertical cranial migration. Recent reports have evaluated the morphology of the upper cervical spine in RA patients using CT. Iizuka et al. [4] evaluated the AOJ of AAS patients using a sagittal reconstruction view on CT and noted ankylosis of the AOJ in 5 of 26 surgical cases, and induced severe displacement between C1 and C2 in the neutral position, despite the fact that normal findings of AOJ showed a slight displacement before surgery. Ito et al. [5] evaluated the AAJ after TSF in patients with AAS due to RA using CT reconstruction, and noted facet fusion and a stable C1/2 in 5 out of 7 patients showing posterior graft failure.
In the current study, the average ADI value at the neutral position in Group C showing a destructive abnormality of subchondral bone in the AAJ at least on one side was significantly larger than the value of Group A showing maintenance of the joint space in the AAJ bilaterally, although no difference was observed in those values at the flexion position among those groups. Furthermore, the mean AAA values in Group C was significantly lower than in Groups A and B. The findings of this study therefore suggest that the destructive abnormality of the subchondral bone in the AAJ at least on one side induced an enlargement of the ADI and anterior inclination of the atlas at the neutral position and, consequently, a severe displacement between C1 and C2 at the neutral position was demonstrated in Group C.
Fusion in the AAJ was demonstrated in 14 patients (46.7%) using CT reconstruction views at 1 year after C1–2 TSF. According to the preoperative grading of AAJ on the CT views, the postoperative fusion in the AAJ was demonstrated in 0 of 32 joints (0%) in Grade 1, 7 of 18 joints (38.9%) in Grade 2 and all of 10 joints (100%) in Grade 3. Therefore, the findings of this study suggest that fusion in the AAJ after TSF tended to occur in the AAS patients showing severe destructive changes in the AAJ before surgery. This also suggests that when the AAS patients showed severe displacement between C1 and C2 before surgery, it thus appears easy to acquire fusion after C1/2 arthrodesis, even if a reduction position can be achieved. Furthermore, AAS patients demonstrating the severe destruction of AAJ may not require either posterior supplementation or grafting.
Grob et al. [3] noted that atlanto-axial arthrodesis achieved by TSF can prevent a further deterioration of the vertical cranial migration due to the destruction of the lateral masses of the atlas in RA AAS patients. However, Fujiya et al. [1] noted in 57 patients showing either isolated atlanto-axial instability or in combination with mild vertical subluxation treated by atlanto-axial arthrodesis (Brooks method), that superior migration of the odontoid process occurred in 4 patients (7%), while 2 patients required occipital–cervical fusion as a second procedure. We therefore speculated that this difference was due to the fusion in the AAJ induced by TSF.
In conclusion, this study showed that a destructive abnormality of subchondral bone in the AAJ, at least on one side, induced an enlargement of the ADI and anterior inclination of the atlas in patients with AAS due to RA. The current study also showed that fusion in the AAJ was demonstrated in 14 of 30 patients after C1/2 TSF. This was easy to recognize in AAS patients whose joint destruction extended to the subchondral bone. Therefore, this morphology of the AAJ improves the fusion rate after C1–2 TSF.
Conflict of interest
No benefits in any form have been received or will be received from a commercial party related either directly or indirectly to the subject of this article.
References
- 1.Fujiya M, Oguma T, Hasegawa K, Oda I, Minami M, Matsuno S. Long-term outcome of the operated cervical spine in rheumatoid arthritis: comparative study of cases with and without vertical subluxation (in Japanese) Rinsho Seikei Geka. 2003;38:427–435. [Google Scholar]
- 2.Grob D, Jeanneret B, Aebi M, Markwalder TM. Atlanto-axial fusion with transarticular screw fixation. J Bone Jt Surg Br. 1991;73:972–976. doi: 10.1302/0301-620X.73B6.1955447. [DOI] [PubMed] [Google Scholar]
- 3.Grob D. Atlantoaxial immobilization in rheumatoid arthritis: a prophylactic procedure? Eur Spine J. 2000;9:404–409. doi: 10.1007/s005860000174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Iizuka H, Sorimachi Y, Ara T, et al. Relationship between the morphology of the atlanto-occipital joint and the radiographic results in patients with atlanto-axial subluxation due to rheumatoid arthritis. Eur Spine J. 2008;17:826–830. doi: 10.1007/s00586-008-0659-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ito H, Neo M, Fujibayashi S, Miyata M, Yoshitomi H, Nakamura T. Atlantoaxial transarticular screw fixation with posterior wiring using polyethylene cable: facet fusion despite posterior graft resorption in rheumatoid patients. Spine. 2008;33:1655–1661. doi: 10.1097/BRS.0b013e31817b5c07. [DOI] [PubMed] [Google Scholar]
- 6.Magerl F, Seemann PS. Stable posterior fusion of the atlas and axis by transarticular screw fixation. In: Kehr P, Weidner A, editors. Cervical spine I. Wien: Springer; 1987. pp. 322–327. [Google Scholar]
- 7.Matsunaga S, Sakou T, Onishi T, et al. Prognosis of patients with upper cervical lesions caused by rheumatoid arthritis, comparison of occipitocervical fusion between C1 laminectomy and nonsurgical management. Spine. 2003;28:1581–1587. [PubMed] [Google Scholar]
- 8.McGraw RW, Rusch RM. Atlanto-axial arthrodesis. J Bone Jt Surg Br. 1973;55:482–489. [PubMed] [Google Scholar]
- 9.Wang C, Yan M, Zhou H, Wang S, Dang G. Atlantoaxial transarticular screw fixation with morselized autograft and without additional internal fixation: technical description and report of 57 cases. Spine. 2007;32:643–646. doi: 10.1097/01.brs.0000257539.75693.cc. [DOI] [PubMed] [Google Scholar]