Abstract
Epidural steroid injections are an important therapeutic modality employed by spinal surgeons in the treatment of patients with chronic low back pain with or without lumbar radiculopathy. The caudal epidural is a commonly used and well-established technique; however, little is known about the segmental level of pathology that may be addressed by this intervention. This prospective study of over 50 patients aimed to examine the spreading pattern of this technique using epidurography. The effect of variation in Trendelenburg tilt and the eradication of lumbar lordosis on the cephalic distribution of the injectate were investigated. 52 patients with low back pain and radiculopathy underwent caudal epidural. All had 20 ml volume injected, comprised of 5 ml contrast (Ultravist™ Schering) 2 ml Triamcinolone (Adcortyl™ Squibb) and 13 ml local anaesthetic (1% lignocaine). Patients were randomised to either 0° or 30° of Trendelenburg tilt, as referenced from the lumbar spine. Patients were further randomised to presence or absence of lumbar lordosis, which was eradicated using a flexion device placed beneath the prone patient. A lateral image of each sacrum was obtained, to identify variations in sacral geometry particularly resistant to cephalic spread of injectate. The highest segment reached on fluoroscopy was recorded post injection. Fifty-two patients with a mean age of 50 years underwent caudal epidural. Thirty-one were in 0° head tilt, with 21 in 30° of head tilt. In each of these groups, 50% had their lumbar lordosis flattened prior to caudal injection. The median segmental level reached was L3, with a range from T9 to L5. Eradication of lumbar lordosis did not significantly alter cephalic spread of injectate. There was a trend for 30° tilt to extend the upper level reached by caudal injection (p = 0.08). There were no adverse events in this series. Caudal epidural is a reliable and relatively safe procedure for the treatment of low back pain. Pathology at L3/4 and L4/5 and L5/S1 can be approached by this technique. Although in selected cases thoracic and high lumbar levels can be reached, this is variable. If pathology at levels above L3 needs to be addressed, we propose a 30° head tilt may improve cephalic drug delivery. The caudal route is best reserved for pathology below L3.
Keywords: Caudal epidural, Lumbar spine
Introduction
The caudal epidural steroid injection is well established in the setting of chronic low back pain in the presence or absence of lumbar radiculopathy. This is a relatively safe procedure, particularly with the use of fluoroscopy [1]. The ability of this technique to reach higher lumbar levels, and under what conditions can cephalic delivery be optimised, have not been examined extensively.
Evans, in 1930, publicised intrasacral epidural injection in the treatment of sciatica. He demonstrated that injection of 100 ml of fluid into the epidural space at the base of the sacrum caused diffusion of the fluid throughout the spinal canal. He did not demonstrate a difference in the effects obtained with local anaesthetic or saline [2]. Efforts to control the inflammatory aspect of nerve root compression led to the use of antiflammatory agents such as corticosteroids, where initial studies reported a beneficial effect [3]. A subsequent meta-analysis of 12 published randomised controlled trials concluded that epidural steroids were effective [4]. The beneficial effect appears to last from the short to medium term (1 week–3 months) [5].
Caudal epidural effectiveness has been examined by clinical response by Cyriax et al. [6] who report improved outcome with larger volumes. Volumetric caudal injections have been examined by epidurography by Kim et al. [7] who found no advantage in terms of cephalic migration of injectate, despite using incremental volumes up to 50 ml. They suggest that improved clinical outcome may be a result of mechanical forces generated intradurally and epidurally by the larger volumes. They confirmed radiographically that mid to lower lumbar vertebrae were reached. However, using serial injections of 10 ml up to 50 ml, no further spread was elicited but a ‘repainting’ of the path of previous injections was noted.
Apart from variations in caudal volumes, no work has focused on other potential strategies to improve cephalic drug delivery, or focused on local anatomical factors that render certain patients resistant to injectate migration.
This study aimed to investigate if variations in head tilt and eradication of the lumbar lordosis had a beneficial effect on the vertebral level reached on epidurography post caudal epidural. Variations in individual sacral geometry were also recorded to identify any particular pattern associated with unfavourable epidurography.
Methods
Study period
This prospective study was performed over a 6-month period. Patients fulfilling the inclusion criteria and sparing reasons for exclusion were enrolled into the study once informed consent was obtained.
Inclusion criteria
Patients with low back pain with or without lumbar radiculopathy were included in the study.
Exclusion criteria
The following findings led to exclusion from the study: history or presence of alcohol or drug abuse, psychotic disorders, subjects unable to understand informed consent. Also, patients with a known allergy to contrast or other contra-indication to administered reagents, critical skin conditions at injection site, use of anticoagulants or previous lumbar surgery were excluded.
Caudal injections
Fifty-two patients with low back pain and radiculopathy underwent caudal epidural. All had 20 ml volume injected, comprised of 5 ml contrast (Ultravist™ Schering) 2 ml Triamcinolone (Adcortyl™ Squibb), 13 ml local anaesthetic (1% lignocaine) with correct placement of needle confirmed on fluoroscopy. Local anaesthetic was administered to the skin and subcutaneous tissues to periosteum prior to injection, and all injections were performed by the senior author.
Patients were randomised to either 0° or 30° of Trendelenburg tilt, as referenced from the lumbar spine. Patients were further randomised to presence or absence of lumbar lordosis, which was eradicated using a flexion device placed beneath the prone patient. A lateral image of each sacrum was obtained to identify variations in sacral geometry particularly resistant to cephalic spread of injectate. The highest segment reached on fluoroscopy was recorded post injection.
Statistical methods
Statistical analysis was performed using a Mann–Whitney U test. p Values of less than 0.05 were considered significant.
Results
Fifty-two patients with a mean age of 50 years underwent caudal epidural. Thirty-one were in 0° head tilt, with 21 in 30° of head tilt. In each of these groups, 50% had their lumbar lordosis flattened prior to caudal injection. The median segmental level reached was L3, with a range from T9 to L5. Eradication of lumbar lordosis did not significantly alter cephalic spread of injectate (Fig. 1). There was a trend for 30° head tilt to extend the upper level reached by caudal injection (p = 0.08). There was an insufficient variation in sacral geometry noted in this cohort to identify a particular pattern associated with unfavourable delivery of caudal injectate to the lumbar spine (Fig. 2). No adverse effects occurred in this series.
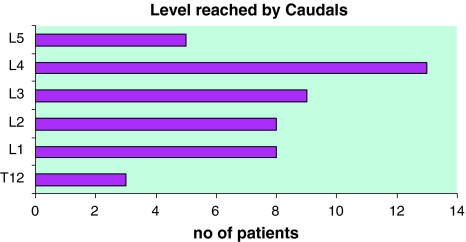
Fig. 1.
This graph illustrates the range of spreading levels reached by the injectate
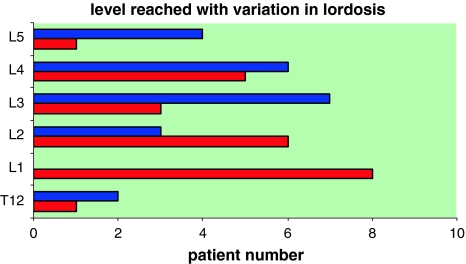
Fig. 2.
Spreading levels reached by the injectate with normal prone position and normal lumbar lordosis (blue) and level reached with lumbar lordosis eradicated (red). There was no statistically significant alteration in most cranial level reached
Discussion
Caudal epidural is an established technique in the setting of radicular low back pain. However, this technique is not without its limitations, owing to the variations in sacral hiatus anatomy. The sacral hiatus, the site of needle insertion is located at the base of the sacrum at the level of the spinous process of S4. The hiatus is typically bordered laterally by the two sacral cornua. Sekiguchi et al. [8] in their anatomic study of the sacral hiatus found that there was an absence of the hiatus in 4% of examined cases, an imperforate hiatus in 3% of cases and only 42% had both hiatus and cornu as typically described (Fig. 3).
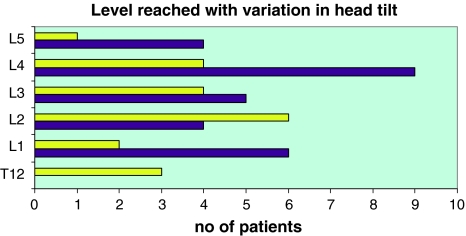
Fig. 3.
Spreading levels reached by the injectate with variation in head down tilt. There was no statistically significant difference in 30° head down tilt (yellow) versus 0 degree tilt (purple)
Although the sacral epidural space is largest it also has the greatest amount of leakage [9]. Kim et al. [7] showed that the mid to lower lumbar region of the spine could be consistently treated using caudal epidurals of up to 30 ml. There was no change in the levels attained by subsequent injections.
Epidural injections may be introduced through caudal, interlaminar and transforaminal (lumbar) routes. The choice of technique is based on several different factors. Primarily, one approach is chosen over another because of the anatomic location of the suspected pain generator. However, previous surgery, such as spinal fusion, may block the lumbar approaches. Another advantage of caudal injection is the ease of performance, although larger volumes of fluid are thought to be required. The relatively low charge for a caudal epidural compared with that of multiple selective injections is another important consideration. These routes of administration are often grouped together; however, these approaches have different efficacy and safety profiles [11, 13]. It should be noted that conventional techniques do not guarantee that injectates reach the desired target nerve nor does the recorded spread of contrast necessarily reflect later distribution [10]. A study to compare the impact of method of injection on outcome revealed no difference attributable to method of administration [11].
In this study, the effect of caudal epidural on outcome was not examined, as previous studies have already supported their use in the setting of low back pain, predominantly secondary to disc herniation [12–14]. However, a recent systematic review looking at caudal epidural also suggested evidence for relief of chronic pain in discogenic pain without disc herniation or radiculitis [15].
The focus of this study was to identify anatomical lumbar segments reached by the caudal route in our cohort and to identify potential strategies to improve cephalic drug delivery. Although not a validated method, a flexion device placed beneath the prone patient flattened the lumbar lordosis, as confirmed objectively by on-table fluoroscopy (Figs. 4, 5). This, intuitively, would be expected to improve the cephalic migration of caudal injectate. However, a beneficial effect on spreading levels achieved was not demonstrated by altering lumbar lordosis.
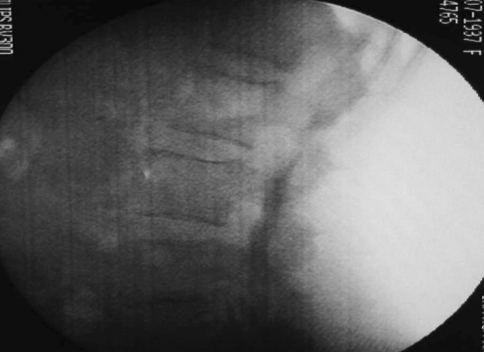
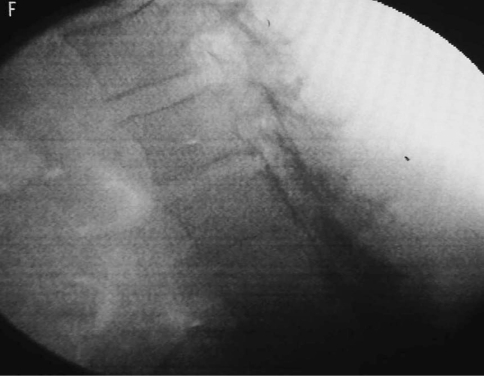
Fig. 4.
Fluroscopy image of lateral lumbar spine in a subject in control prone position. Injectate can be seen at upper border of L3
Fig. 5.
Fluroscopy image of lateral lumbar spine with injectate reaching L3 in a subject with eradication of lumbar lordosis
They was a trend for 30° tilt to extend the upper level reached by caudal injection (p = 0.08). As this did not reach statistical significance, we are unable to confirm that Trendelenburg tilt improved cephalic drug delivery; however, our study may be underpowered in this regard.
Conclusion
In the literature, caudal epidural is a useful and relatively safe procedure for the treatment of radicular low back pain [16–19], as well as a potential treatment in the setting of non radicular low back pain [13, 14]. Pathology at L3/4 and L4/5 and L5/S1 can be approached by this technique. Although in selected cases thoracic and high lumbar levels can be reached, this is variable. If pathology at levels above L3 needs to be addressed, we propose a 30° head tilt may improve cephalic drug delivery. Delivery by caudal epidural should be reserved to address pathology at L3 and below. Larger prospective studies may elucidate this further.
Conflict of interest
None.
References
- 1.White AH. Injection techniques for the diagnosis and treatment of low back pain. Orthop Clin North Am. 1983;14:553–567. [PubMed] [Google Scholar]
- 2.Evans W. Intrasacral epidural injection in the treatment of sciatica. Lancet. 1930;2:1225–1229. doi: 10.1016/S0140-6736(00)86498-3. [DOI] [Google Scholar]
- 3.Dilke TF, Burry HC, Grahame R. Extradural corticosteroid injection in the management of lumbar nerve root compression. BMJ. 1973;2:635–637. doi: 10.1136/bmj.2.5867.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watts RW, Silagy CA. A meta-analysis of the efficacy of epidural corticosteroids in the treatment of sciatica. Anaesth Intensive Care. 1995;23:564–569. doi: 10.1177/0310057X9502300506. [DOI] [PubMed] [Google Scholar]
- 5.Bowman SJ, Wedderburn L, Whaley A, Grahame R, Newman S. Outcome assessment after epidural corticosteroid injection for low back pain and sciatica. Spine. 1993;18(10):1345–1350. doi: 10.1097/00007632-199308000-00014. [DOI] [PubMed] [Google Scholar]
- 6.Cyriax J (1982) Epidural local anaesthesia. In: Textbook of orthopaedic medicine, vol 1, 8th edn. Harcourt publishers, New York, pp 310–327
- 7.Kim KM, Kim HS, Chow KH, Ahn WS. Cephalic spreading levels after volumetric caudal epidural injections in chronic low back pain. J Korean Med Sci. 2001;16:193–197. doi: 10.3346/jkms.2001.16.2.193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sekiguchi M, Yabuki S, Satoh K, Kikuchi S. An anatomic study of the sacral hiatus: a basis for successful caudal epidural block. Clin J Pain. 2004;20(1):51–54. doi: 10.1097/00002508-200401000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Bryce-Smith R. The spread of solutions in the extradural space. Anaesthesia. 1954;9:201–205. doi: 10.1111/j.1365-2044.1954.tb01563.x. [DOI] [PubMed] [Google Scholar]
- 10.Bogduk N. Spine update: epidural steroids. Spine. 1995;20:845–848. doi: 10.1097/00007632-199504000-00021. [DOI] [PubMed] [Google Scholar]
- 11.McGregor AH, Anjarwalla NK, Stambach T. Does the method of injection alter the outcome of epidural injections? J Spinal Disorders. 2001;14(6):507–510. doi: 10.1097/00002517-200112000-00008. [DOI] [PubMed] [Google Scholar]
- 12.Breivik H, Hesla PE, Molnar I, Lind B. Treatment of chronic low back pain and sciatica. Comparison of caudal epidural injections of bupivacaine and methylprednisolone with bupivacaine followed by saline. In: Bonica JJ, Albe-Fessard D, editors. Advances in pain research and therapy. New York: Raven Press; 1976. pp. 927–932. [Google Scholar]
- 13.Bush K, Hillier S. A controlled study of caudal epidural injections of triamcinolone plus procaine for the management of intractable sciatica. Spine. 1991;16:572–575. doi: 10.1097/00007632-199105000-00015. [DOI] [PubMed] [Google Scholar]
- 14.Sayegh FE, Kenanidis EL, Papavasiliou KA, Potoupnis ME, Kirkos JM, Kepetanos GA. Efficacy of steroid and nonsteroid caudal epidural injections for low back pain and sciatica: a prospective, randomized, double-blind clinical trial. Spine 15. 2009;34(14):1441–1447. doi: 10.1097/BRS.0b013e3181a4804a. [DOI] [PubMed] [Google Scholar]
- 15.Conn A, Buenaventura RM, Datta S, Abdi S, Diwan S. Systematic review of caudal epidural injections in the management of chronic low back pain. Pain Physician. 2009;12(1):109–135. [PubMed] [Google Scholar]
- 16.Cuckler JM, Bernini PA, Wiesel SW, Booth RE, Rothman RH, Pickens GT. The use of epidural steroids in the treatment of radicular pain. J Bone Joint Surg (Am) 1985;67:63–66. [PubMed] [Google Scholar]
- 17.Young IA, Hyman GS, Packia-Raj LN, Cole AJ. The use of lumbar epidural/transforaminal steroids for managing spinal disease. J Am Acad Orthop Surg. 2007;15(4):228–238. doi: 10.5435/00124635-200704000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Grundy EM, Rammurthy S, Patel KP, Mani M, Winnie AP. Extradural analgesia revisited. A statistical study. Br J Anaesth. 1978;50:805–809. doi: 10.1093/bja/50.8.805. [DOI] [PubMed] [Google Scholar]
- 19.Carette S, et al. Epidural corticosteroid injections for sciatica due to herniated nucleus pulposus. N Engl J Med 5. 1997;336(23):1634–1640. doi: 10.1056/NEJM199706053362303. [DOI] [PubMed] [Google Scholar]