Abstract
AIM: To investigate the technical success and clinical complication rate of a cannulated pancreatic duct with guidewire for biliary access.
METHODS: During a five-year study period, a total of 2843 patients were included in this retrospective analysis. Initial biliary cannulation method consisted of single-guidewire technique (SGT) for up to 5 attempts, followed by double-guidewire technique (DGT) when repeated unintentional pancreatic duct cannulation had taken place. Pre-cut papillotomy technique was reserved for when DGT had failed or no pancreatic duct cannulation had been previously achieved. Main outcome measurements were defined as biliary cannulation success and post-endoscopic retrograde cholangiopancreatography (ERCP) complication rate.
RESULTS: SGT (92.3% success rate) was characterized by statistically significant enhanced patient outcome compared to either the DGT (43.8%, P < 0.001), pre-cut failed DGT (73%, P < 0.001) or pre-cut as first step method (80.6%, P = 0.002). Pre-cut as first step method offered a statistically significantly more favorable outcome compared to the DGT (P < 0.001). The incidence of post-ERCP pancreatitis did not differ in a statistically significant manner between either method (SGT: 5.3%, DGT: 6.1%, Pre-cut failed DGT: 7.9%, Pre-cut as first step: 7.5%) or with patients’ gender.
CONCLUSION: Although DGT success rate proved not to be superior to SGT or pre-cut papillotomy, it is considered highly satisfactory in terms of safety in order to avoid the risk of a pre-cut when biliary therapy is necessary in difficult-to-cannulate cases.
Keywords: Endoscopic retrograde cholangiopancreatography, Post-endoscopic retrograde cholangiopancreatography pancreatitis, Pre-cut papillotomy, Pancreatic duct
INTRODUCTION
Endoscopic retrograde cholangiopancreatography (ERCP) is widely considered as the most demanding endoscopic interventional procedure offering the least invasive way for biliary manipulations. In terms of procedure-related safety, atraumatic biliary cannulation is the fundamental prerequisite to secure a successful therapeutic-intended ERCP[1]. Nowadays, non-invasive imaging modalities [such as magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS)] have superseded diagnostic ERCP, reducing the potential complication rate and giving better selection criteria for patients who would benefit from therapeutic biliary manipulations[2].
Long discussions and reports from ERCP experts have proposed a plethora of different ways to provide an uncomplicated biliary cannulation[1]. Several factors during ERCP may lead an endoscopist to use the appropriate technique according to his experience and training. Many reports have shown that selective cannulation of the common bile duct (CBD) by insertion of a hydrophilic guidewire through a papillotome may minimize procedure-related complications (particularly post-ERCP pancreatitis-PEP), as opposed to standard CBD access method with direct injection of contrast media[3-7].
In difficult-to-cannulate cases, pre-cut papillotomy has been established as the alternative method to gain CBD access when biliary therapy is strongly indicated[8,9]. However, pre-cut technique predisposes to a higher rate of post-ERCP complications including hemorrhage, pancreatitis and perforation, even in the most experienced hands[10-14].
Furthermore, several studies have documented that a pancreatic duct (PD) previously cannulated with a guidewire may facilitate selective CBD cannulation with a second wire preloaded into a papillotome (double guidewire technique - DGT)[15-19]. Placement of such a guidewire into the pancreatic duct may act as an endoscopic road map for the CBD, open a stenotic papillary orifice, stabilize the papilla or straighten the common channel when dealing with a tortuous intraduodenal segment[1].
In view of the above, we retrospectively analyzed our data concerning the use of this method (DGT) in terms of procedure-related efficacy, safety and complication rate.
MATERIALS AND METHODS
Patients
During a 5-year period (from June 2003 through July 2008), 2843 therapeutic ERCPs were performed in our hospital. A retrospective database review was conducted in order to identify all cases involving the use of DGT. Inclusion criteria were the existence of an intact papilla (no prior ERCP attempts) in patients with clinical, laboratory and radiological (transabdominal US, abdominal CT scans, MRCP) findings of pancreatobiliary pathology. Patients with previous gastrointestinal surgical operation, use of needle-knife fistulotomy for papilla impacted stones and suspected sphincter of oddi dysfunction (SOD) were excluded from our study. Endoscopic sphincterotomy (EST) was performed in all patients.
Methods and definitions
Our department protocol for biliary cannulation consists of a 3-step procedure undertaken in a single session. In the first step, attempts to cannulate the CBD consist of the use of a sphincterotome preloaded with a hydrophilic guidewire (single guidewire technique-SGT). Initial cannulation using SGT is both time- and cost-efficient when sphincterotomy is anticipated. The use of a guidewire seems to reduce the possibility of chemical-and pressure-related pancreatic injury by avoiding unintentional injection of contrast medium into the main PD or the papilla itself (submucosal injection). Up to 5 attempts within a 15-min period are considered adequate to provide safe cannulation without significant injury of the papillary area (i.e. trauma, edema, bleeding). If these attempts fail and repeated deep PD insertion has resulted, then the guidewire is left distally in the main PD and DGT technique is performed up to 3 times. The tip of the papillotome is positioned against the first wire placed in the PD (Figure 1) and its curve is altered in the anticipated CBD axis. The guidewire into the PD acts as a radiological marker for the PD and facilitates endoscopic location of the biliary orifice (Figure 2). Pre-cut technique with needle-knife is reserved as the 3rd step in cases when DGT has failed or no PD cannulation has been achieved in the first place.
Figure 1.
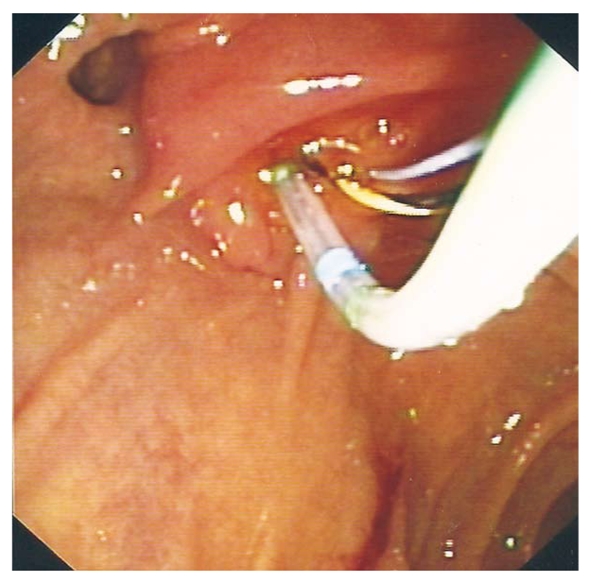
Endoscopic view of the papilla with a hydrophilic wire advanced into the pancreatic duct. A sphincterotome is advanced alongside the pancreatic wire with its tip oriented in the anticipated bile duct position.
Figure 2.
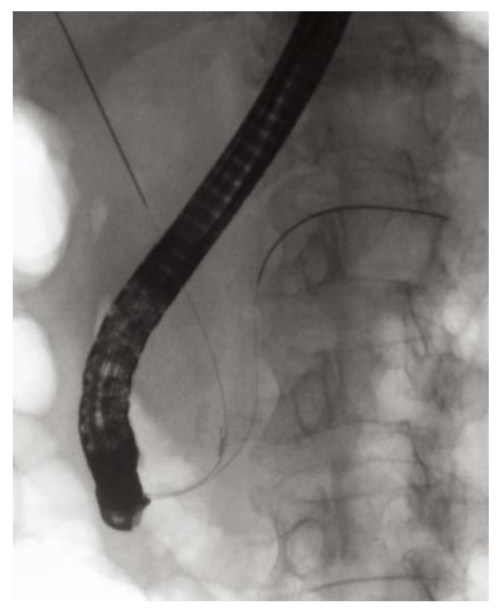
Biliary cannulation with the use of double-guidewire technique. One guidewire has been inserted into the distal part of the pancreatic duct and another is being moved in the direction of common bile duct through the sphincterotome inserted into the ampulla.
Procedural success was defined as the insertion of the guidewire into the CBD. To determine safety and complication rate, all patients underwent measurement of serum amylase before and 24 h after ERCP. Asymptomatic hyperamylasemia was defined as a threefold rise in serum amylase without epigastric pain at 24 h after ERCP. Definition of PEP was the incidence of epigastric pain associated with serum amylase elevation to greater than 3 times normal values at 24 h after the procedure. Bleeding, perforation and other post-ERCP-related adverse events were recorded in detail.
Statistical analysis
Due to the fact that the distribution of the variables under study was not Gaussian, analysis of differences between these parameters, in each patient group, was performed with the non-parametric Mann-Whitney, χ2, or Fischer’s exact statistical tests, where applicable. The correlation between the employment of different cannulation methods and either final patient outcome, or presence of asymptomatic hyperamylasemia or clinical pancreatitis, was studied using univariate logistic regression analysis.
RESULTS
Of the 2843 ERCPs performed in the study period, 511 were excluded as patients had previously undergone endoscopic manipulations (EST, endoscopic papillary balloon dilation), or altered anatomy was observed due to gastrectomy, or SOD was suspected on the basis of clinical and ERCP findings. A total of 2332 patients met selection criteria. Indications for therapeutic ERCP varied, with suspected common bile duct stones and suspected malignant biliary strictures being the most common (Table 1).
Table 1.
Patient characteristics and indications n (%)
| Dermographics | |
| Patient number | 2332 |
| Age (year, mean) | 68.4 |
| Gender (male/female) | 1236/1096 |
| Indications | |
| Choledocholithiasis | 1732 (74.3) |
| Malignant stricture | 545 (23.4) |
| Bile leak after cholecystectomy | 42 (1.8) |
| Primary sclerosing cholangitis | 11 (0.5) |
Using SGT as the first step method, CBD cannulation was achieved in 2153 patients (92.3%). Unintentional PD guidewire insertion after 5 attempts was documented in 112 patients. In these cases, DGT was performed after the last effort and selective CBD access was successful in 49 out of 112 patients (43.8%). In the 63 failed DGT cases pre-cut papillotomy gained CBD access in 46 patients (73%). In 67 patients no CBD or PD cannulation was possible with the initial 5 attempts. Fifty-four of them underwent successful pre-cut papillotomy at the same session (80.6%).
SGT was characterized by statistically significant enhanced patient outcome compared to either the DGT (P < 0.001), pre-cut failed DGT (P < 0.001) or pre-cut as first step method (P = 0.002) (Tables 2 and 3). In addition, pre-cut as first step method offered a statistically significantly (P < 0.001) more favorable outcome compared to the DGT method. These observations were further confirmed using univariate logistic regression analysis (Table 4).
Table 2.
Comparison between single-guidewire technique/double-guidewire technique, single-guidewire technique/pre-cut failed double-guidewire technique and single-guidewire technique/pre-cut first step methods in terms of patient outcome, the development of asymptomatic hyperamylasemia or post-endoscopic retrograde cholangiopancreatography pancreatitis n (%)
| Variables | SGT | DGT | SGT | Pre-cut failed DGT | SGT | Pre-cut first step |
| Outcome (success) | 2153 (92.3) | 49 (43.8) | 2153 (92.3) | 46 (73.0) | 2153(92.3) | 54 (80.6) |
| P value1 | < 0.001a | < 0.001a | 0.002a | |||
| Asymptomatic hyperamylasemia | 258 (12.0) | 11 (22.4) | 258 (12.0) | 15 (23.8) | 258 (12.0) | 10 (14.9) |
| P value1 | 0.046a | 0.008a | 0.591 | |||
| PEP | 115 (5.3) | 3 (6.1) | 115 (5.3) | 5 (7.9) | 115 (5.3) | 5 (7.5) |
| P value1 | 0.935 | 0.538 | 0.629 | |||
P < 0.05.
Calculated by Fisher’s exact test; SGT: Single-guidewire technique; DGT: Double-guidewire technique; PEP: Post-endoscopic retrograde cholangiopancreatography pancreatitis.
Table 3.
Comparison between double-guidewire technique/pre-cut failed double-guidewire technique, pre-cut failed double-guidewire technique /pre-cut first step and double-guidewire technique/pre-cut first step methods in terms of patient outcome, the development of asymptomatic hyperamylasemia or post-endoscopic retrograde cholangiopancreatography pancreatitis n (%)
| Variables | DGT | Pre-cut failed DGT | Pre-cut failed DGT | Pre-cut first step | DGT | Pre-cut first step |
| Outcome (success) | 49 (43.8) | 46 (73.0) | 46 (73.0) | 54 (80.6) | 49 (43.8) | 54 (80.6) |
| P value1 | < 0.001a | 0.405 | < 0.001a | |||
| Asymptomatic hyperamylasemia | 11 (22.4) | 15 (23.8) | 15 (23.8) | 10 (14.9) | 11 (22.4) | 10 (14.9) |
| P value1 | 0.955 | 0.266 | 0.426 | |||
| PEP | 3 (6.1) | 5 (7.9) | 5 (7.9) | 5 (7.5) | 3 (6.1) | 5 (7.5) |
| P value1 | 0.999 | 0.588 | 0.928 | |||
P < 0.05.
Calculated by Fisher’s exact test. SGT: Single-guidewire technique; DGT: Double-guidewire technique; PEP: Post-endoscopic retrograde cholangiopancreatography pancreatitis.
Table 4.
Logistic regression analysis for every possible comparison of the cannulation method used, for the prediction of outcome (failure)
| Method | HR1 | 95% CI | P value2 |
| SGT | 1 | ||
| Pre-cut first step | 1.43 | 1.16-1.76 | 0.001 |
| SGT | 1 | ||
| DGT | 3.93 | 3.21-4.81 | < 0.001 |
| Pre-cut first step | 1 | ||
| DGT | 1.23 | 1.13-1.35 | < 0.001 |
| Pre-cut first step | 1 | ||
| Pre-cut failed DGT | 1.063 | 0.95-1.20 | 0.307 |
Hazard ratio;
Test for trend. SGT: Single-guidewire technique; DGT: Double-guidewire technique.
Thirty patients in whom therapeutic ERCP failed were referred to surgical or interventional radiological treatment. The total success rate of CBD cannulation in the study population was 98.7% (2302/2332).
The development of asymptomatic hyperamylasemia was significantly more frequent in the DGT and precut-failed DGT group of patients, compared to the SGT patients (Table 2). Employing regression analysis, patients who underwent DGT were 2.15 times [HR] more likely (95% CI 1.39-4.60, P = 0.002) to develop asymptomatic hyperamylasemia than the SGT patients.
The rates of PEP did not differ in a statistically significant manner between groups of patients who underwent different types of cannulation (Tables 2 and 3). The presence of PEP in the DGT group of patients was statistically significantly (P = 0.010) more evident in younger individuals (Median = 42.00 years) than in older ones (63.00 years), without statistical correlation with the initial pathology (Table 4).
In the group of patients who underwent SGT, a statistically significant difference (P = 0.005) between age and outcome was observed, as younger patients (Median = 64.00 years) were more likely to be attributed with a successful outcome than older ones (Median = 67.00 years). However, PEP was more frequently present (P < 0.001) in younger (Median = 62.00 years) patients than older ones (Median = 67.00 years). Patients who suffered from choledocholithiasis were more likely to present PEP than patients who suffered from malignancy, without reaching statistically significant difference (Table 5).
Table 5.
Associations between the development of post-endoscopic retrograde cholangiopancreatography pancreatitis and the initial pathology within groups of patients who underwent each cannulation method n (%)
| Method | Choledocholithiasis | Malignancy |
| Pre-cut first step | ||
| PEP | 5 (19.2) | 0 (0.0) |
| P value1 | 0.007a | |
| DGT | ||
| PEP | 3 (8.3) | 0 (0.0) |
| P value1 | 0.556 | |
| Pre-cut failed DGT | ||
| PEP | 5 (16.1) | 0 (0.0) |
| P value1 | < 0.001a | |
| SGT | ||
| PEP | 97 (5.8) | 17 (3.9) |
| P value1 | 0.146 | |
P < 0.05.
Calculated by Fisher’s exact test. SGT: Single-guidewire technique; DGT: Double-guidewire technique; PEP: Post-endoscopic retrograde cholangiopancreatography pancreatitis.
In the pre-cut failed DGT group of patients, PEP was more frequently present (P = 0.021) in younger (Median = 45.00 years) patients than older ones (Median = 63.50 years). As far as the pre-cut as first step method is concerned, the presence of PEP was found more frequently (P = 0.017) in younger patients (Median = 52.00 years) than older patients (Median = 68.00 years). The presence of PEP was statistically more evident in patients with choledocholithiasis compared to patients with malignancy in both groups of patients in which pre-cut technique was performed (Table 5).
Patients’ gender did not seem to relate in any statistically significant way with the presence of asymptomatic hyperamylasemia and PEP within patients who underwent pre-cut first step, DGT or pre-cut failed DGT method. On the contrary, female patients who underwent SGT showed a statistically significant elevated presence of asymptomatic hyperamylasemia (14.0%) compared to male patients (Table 6).
Table 6.
Associations between patient gender and the presence of PEP and asymptomatic hyperamylasemia, within groups of patients who underwent each cannulation method n (%)
| Method | PEP | Asymptomatic hyperamylasemia |
| Pre-cut first step | ||
| Male | 2 (5.1) | 3 (7.7) |
| Female | 3 (10.7) | 7 (25.0) |
| P value1 | 0.642 | 0.081 |
| DGT | ||
| Male | 1 (3) | 6 (18.2) |
| Female | 2 (12.5) | 5 (31.3) |
| P value1 | 0.086 | 0.467 |
| Pre-cut failed DGT | ||
| Male | 1 (2.9) | 9 (26.5) |
| Female | 4 (13.8) | 6 (20.7) |
| P value1 | 0.171 | 0.768 |
| SGT | ||
| Male | 62 (5.5) | 115 (10.2) |
| Female | 53 (5.2) | 143 (14.0) |
| P value1 | 0.77 | 0.008a |
P < 0.05.
Calculated by Fisher’s exact test. SGT: Single-guidewire technique; DGT: Double-guidewire technique.
One case of retroperitoneal perforation was recorded using SGT, and 2 patients developed massive bleeding using pre-cut as first step and sphincterotomy after successful SGT, respectively. These patients underwent immediate surgical treatment without further complications.
DISCUSSION
In the era of modern non-invasive imaging modalities, the role of ERCP has been focused in the therapeutic management of pancreatobiliary diseases. Several techniques and accessories have been used in order to achieve selective CBD cannulation and to decrease the rate of post-ERCP complications.
In the present study, SGT proved to be an effective and safe CBD cannulation approach. The ability to manually control the angle of orientation of the sphincterotome has been shown to be advantageous when dealing with unusually oriented or distorted papillas caused by either diverticula or surgically altered anatomy[20]. Moreover, the use of hydrophilic coated-tip guidewires seems to offer a direct way of CBD cannulation under fluoroscopy with less papillary trauma compared to the rather blind method of contrast media injection[4].
Three large prospective randomized studies comparing post-ERCP complications between the use of a papillotome with a guidewire (SGT) and papillotome with contrast media injection as cannulation methods, demonstrated significantly lower incidence of PEP in the SGT group (0%-8.6% vs 4.1%-16.6%)[4-6]. In addition, PEP rate was lower if unintentional guidewire cannulation of the PD occurred compared to that of unintentional PD opacification by contrast injection (0%-5.1% vs 4.4%-19%). In a SGT group, Lee et al[6] reported a total of 3 cases of PEP, two in patients with SOD diagnosis, a well-known risk factor for PEP. In these studies, the authors concluded that the reduction in PEP in SGT groups of patients was mainly the result of avoiding elevation of hydrostatic pressure into the PD, partly attributed to the contrast media injection.
Dumonceau et al[21] first described the successful use of PD guidewire placement as an adjunct to cannulate CBD in a case of Billroth I gastrectomy with a distorted prepapillary segment of CBD. Later on, Gyökeres et al[15] reported successful use of DGT in 24 difficult CBD cannulation cases with no significant difference in PEP rate when compared to conventional cannulation. Maeda et al[16], in a prospective study, documented a superior CBD cannulation rate (93%) with a modified technique, using a PD wire placement and a cannula instead of a papillotome, as opposed to the conventional method with cannula and contrast media (58% success rate). No episodes of pancreatitis with either method were noted, but a significantly higher incidence of hyperamylasemia occurred in the PD wire group. It should be mentioned, however, that patients of the latter group were submitted to pancreatography prior to PD wire insertion, thus increasing the risk of overinjection into the PD with possible acinarization.
In our study, using DGT, selective CBD cannulation was achieved in 43.8% of patients (49/112) with previously failed SGT. Three patients of this group developed pancreatitis (6.1%) and 11 patients asymptomatic amylasemia (22.4%), showing an acceptable safety profile comparable to SGT (5.3% and 12%, respectively). Recently published data from a prospective randomized study assessing clinical efficacy and safety of DGT versus conventional cannulation method reported almost equivalent CBD cannulation success in difficult cases (47.3% vs 54%). The DGT group showed an increased incidence of clinical pancreatitis compared to the SGT group, without, however, reaching a statistically significant difference (17% vs 8%)[22].
According to our results, PD reaction (i.e. PEP) seems to be affected by both iatrogenic and patient-related characteristics. Young patients suffering from choledocholithiasis proved to be statistically more prone to develop pancreatitis when pre-cut access papillotomy as first step was used, or after a failed DGT technique was performed. On the other hand, elderly patients, despite repeated PD wire insertion and use of pre-cut, demonstrated hyperamylasemia as part of a benign post-ERCP clinical course. In addition, 12.5% and 13.8% of female patients who underwent a successful DGT and pre-cut failed DGT developed PEP, respectively. Although these observations were not found to be statistically significant, patients’ gender seems to carry an independent risk factor concerning pancreatic injury following PD manipulations.
Age, sex, prior PEP or recurrent history of acute pancreatitis and SOD are well known risk factors for PEP[23,24] and many experts have already proposed the use of a temporary prophylactic pancreatic stent in these situations[1,25]. Several uncertainties remain regarding patients’ selection criteria for pancreatic stent use and the appropriate diameter. These may be attributed to the lack of long-term data on changes in PD anatomy and stent-induced complications in failed stent placement cases[26]. Goldberg et al[27] documented the aid of a 5F pancreatic stent placement for CBD cannulation in 39 patients with 97.4% success rate. To achieve biliary cannulation, 59% of patients underwent pre-cut sphincterotomy over the pancreatic stent with only 5% PEP rate. The authors, however, do not mention the existence of SOD indication, nor do they report in how many cases pancreatic sphincterotomy was performed to facilitate stent insertion.
No pancreatic stent insertion was performed in our series, as our initial aim was to investigate the contribution of a simple and non-time-consuming technique involving the use rather than abuse of PD. In addition, patients with suspected SOD were excluded due to the lack of manometry which would imply a clear therapeutic indication and the need for a pancreatic stent use. What seems technically more important in DGT technique, regarding success and complication rate, is the gentle straight deep passage of the wire into the PD. Insertion of the wire in angulated mode into a normal PD may potentially increase side-branch acinarization associated with the occurrence of PEP.
It should always be kept in mind that basic CBD cannulation techniques cannot be substituted by any available trick and only proper expertise in ERCP secures periprocedural efficacy. Based on this knowledge, the wire into the PD seems to be helpful for cases of difficult cannulation, particularly when the papilla is mobile with small orifice or disoriented due to a diverticulum or malignancy. In these cases, the anatomical axis of the common channel is stabilized by the inserted wire into the PD, offering the possibility of a new, less traumatic, wire cannulation attempt than pre-cut access papillotomy may cause.
The special incisional technique of pre-cut has been estimated to enable biliary access in about 5% to 10% of hard-to-cannulate cases, according to several reports[28]. However, pre-cut has been described to be an independent risk factor for post-ERCP complications (variation between 8% and 35.3%) and only recommended as an expert’s alternative method[14]. In full agreement with these reports, 5.6% of patients in the period of our study underwent pre-cut papillotomy (77% overall success rate) and 10 patients experienced PEP (7.7%). Data analysis showed no statistically increased possibility of PEP in patients with previously failed DGT followed by pre-cut (7.9% of cases), compared to patients who underwent pre-cut as initial cannulation technique (7.5% of cases).
The decision as to the appropriate CBD cannulation method in specialized situations should to be dependent on a patient’s individual clinical and anatomical basis as well as on an endoscopist’s experience in the available techniques. In the present study, while proposing the SGT as the standard technique for achieving CBD cannulation, DGT offered a remarkable alternative in difficult cases before proceeding to pre-cut papillotomy. DGT success and low complication rate is considered highly satisfactory in order to avoid the risk of a pre-cut when biliary therapy is necessary. Further randomized prospective trials comparing various pre-cut techniques and pancreatic duct cannulation approaches, as rescue methods to facilitate biliary access, will eventually offer an evidence-based approach.
COMMENTS
Background
Biliary cannulation is the fundamental prerequisite to secure a successful therapeutic-intended magnetic resonance cholangiopancreatography (MRCP). Selective biliary cannulation by insertion of a hydrophilic guidewire tends to be the standard method of choice in terms of efficacy and safety [single guidewire technique (SGT)]. In difficult-to-cannulate cases, pre-cut papillotomy has been established as the alternative method to gain biliary access. However, pre-cut technique predisposes to a higher rate of post-ERCP complications, even in the most experienced hands.
Research frontiers
Several studies have documented that a pancreatic duct previously cannulated with a guidewire may facilitate selective biliary cannulation with a second wire (double guidewire technique-DGT).
Innovations and breakthroughs
In a single-center, retrospective study using DGT, selective biliary cannulation was achieved in 43.8% of patients with previously failed SGT. Pre-cut papillotomy gained biliary access in 73% of failed DGT cases and 80.6% of cases as first step method, respectively. Univariate analyses revealed no statistically significant difference in terms of complication rate between patients with different types of cannulation.
Applications
Although the DGT success rate proved not to be superior to that of SGT or pre-cut papillotomy, it is considered a highly satisfactory technique in terms of safety in order to avoid the risk of a pre-cut when biliary therapy is necessary.
Peer review
In this study, the authors conclude that the DGT may be safely performed before proceeding to pre-cut if repeated pancreatic duct cannulation occurs.
Acknowledgments
We particularly wish to thank El Papakonstantinou for her valuable aid with fluoroscopic procedures. There are no potential conflicts of interest for any of the authors.
Footnotes
Peer reviewer: Dr. Jörg C Hoffmann, MA, Priv, Doz, MD, Chief of the Medizinischen Klinik I, mit Schwerpunkt Gastroenterologie, Diabetologie, Rheumatologie und Onkologie, St. Marien- und St. Annastiftskrankenhaus, Salzburger Straße 15, D67067 Ludwigshafen, Germany
S- Editor Sun H L- Editor Logan S E- Editor Ma WH
References
- 1.Freeman ML, Guda NM. ERCP cannulation: a review of reported techniques. Gastrointest Endosc. 2005;61:112–125. doi: 10.1016/s0016-5107(04)02463-0. [DOI] [PubMed] [Google Scholar]
- 2.NIH state-of-the-science statement on endoscopic retrograde cholangiopancreatography (ERCP) for diagnosis and therapy. NIH Consens State Sci Statements. 2002;19:1–26. [PubMed] [Google Scholar]
- 3.Cortas GA, Mehta SN, Abraham NS, Barkun AN. Selective cannulation of the common bile duct: a prospective randomized trial comparing standard catheters with sphincterotomes. Gastrointest Endosc. 1999;50:775–779. doi: 10.1016/s0016-5107(99)70157-4. [DOI] [PubMed] [Google Scholar]
- 4.Lella F, Bagnolo F, Colombo E, Bonassi U. A simple way of avoiding post- ERCP pancreatitis. Gastrointest Endosc. 2004;59:830–834. doi: 10.1016/s0016-5107(04)00363-3. [DOI] [PubMed] [Google Scholar]
- 5.Artifon EL, Sakai P, Cunha JE, Halwan B, Ishioka S, Kumar A. Guidewire cannulation reduces risk of post-ERCP pancreatitis and facilitates bile duct cannulation. Am J Gastroenterol. 2007;102:2147–2153. doi: 10.1111/j.1572-0241.2007.01378.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee TH, Park DH, Park JY, Kim EO, Lee YS, Park JH, Lee SH, Chung IK, Kim HS, Park SH, et al. Can wire-guided cannulation prevent post-ERCP pancreatitis? A prospective randomized trial. Gastrointest Endosc. 2009;69:444–449. doi: 10.1016/j.gie.2008.04.064. [DOI] [PubMed] [Google Scholar]
- 7.Cheon YK, Cho KB, Watkins JL, McHenry L, Fogel EL, Sherman S, Lehman GA. Frequency and severity of post-ERCP pancreatitis correlated with extent of pancreatic ductal opacification. Gastrointest Endosc. 2007;65:385–393. doi: 10.1016/j.gie.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 8.Vandervoort J, Carr-Locke DL. Needle-knife access papillotomy: an unfairly maligned technique? Endoscopy. 1996;28:365–366. doi: 10.1055/s-2007-1005482. [DOI] [PubMed] [Google Scholar]
- 9.Rollhauser C, Johnson M, Al-Kawas FH. Needle-knife papillotomy: a helpful and safe adjunct to endoscopic retrograde cholangio-pancreatography in a selected population. Endoscopy. 1998;30:691–696. doi: 10.1055/s-2007-1001390. [DOI] [PubMed] [Google Scholar]
- 10.Vandervoort J, Soetikno RM, Tham TC, Wong RC, Ferrari AP Jr, Montes H, Roston AD, Slivka A, Lichtenstein DR, Ruymann FW, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652–656. doi: 10.1067/mge.2002.129086. [DOI] [PubMed] [Google Scholar]
- 11.Foutch PG. A prospective assessment of results of needle-knife papillotomy and standard endoscopic sphincterotomy. Gastrointest Endosc. 1995;41:25–32. doi: 10.1016/s0016-5107(95)70272-5. [DOI] [PubMed] [Google Scholar]
- 12.Bruins Slot W, Schoeman MN, Disario JA, Wolters F, Tytgat GN, Huibregtse K. Needle-knife sphincterotomy as a pre-cut procedure: a retrospective evaluation of efficacy and complications. Endoscopy. 1996;28:334–339. doi: 10.1055/s-2007-1005476. [DOI] [PubMed] [Google Scholar]
- 13.Rabenstein T, Ruppert T, Schneider HT, Hahn EG, Ell C. Benefits and risks of needle-knife papilotomy. Gastrointest Endosc. 1997;46:207–211. doi: 10.1016/s0016-5107(97)70087-7. [DOI] [PubMed] [Google Scholar]
- 14.Cotton PB. Pre-cut sphincterotomy: a risky technique for experts only. Gastrointest Endosc. 1989;35:578–579. doi: 10.1016/s0016-5107(89)72921-7. [DOI] [PubMed] [Google Scholar]
- 15.Gyökeres T, Duhl J, Varsányi M, Schwab R, Burai M, Pap A. Double guide wire placement for endoscopic pancreatobiliary procedures. Endoscopy. 2003;35:95–96. doi: 10.1055/s-2003-36403. [DOI] [PubMed] [Google Scholar]
- 16.Maeda S, Hayashi H, Hosokawa O, Dohden K, Hattori M, Morita M, Kidani E, Ibe N, Tatsumi S. Prospective randomised pilot trial of selective biliary cannulation using pancreatic guide-wire placement. Endoscopy. 2003;35:721–724. doi: 10.1055/s-2003-41576. [DOI] [PubMed] [Google Scholar]
- 17.Iqbal S, Sharma P, Shah S, Dhar V, Stavropoulos SN, Stevens PD. Role of Double Guide wire cannulation during ERCP. Gastrointest Endosc. 2008;67 Suppl 5:S1528. [Google Scholar]
- 18.Ito K, Fujita N, Noda Y, Kobayashi G, Horaguchi J, Takasawa O, Obana T. The usefulness and safety of pancreatic guidewire placement for achieving deep cannulation of the bile duct. Gastrointest Endosc. 2008;67 Suppl 5:S554. [Google Scholar]
- 19.Cotton PB, Lehman G, Vennes J, Geenen JE, Russell RC, Meyers WC, Liguory C, Nickl N. Endoscopic sphincterotomy complications and their management: an attempt at consensus. Gastrointest Endosc. 1991;37:383–393. doi: 10.1016/s0016-5107(91)70740-2. [DOI] [PubMed] [Google Scholar]
- 20.Schwacha H, Allgaier HP, Deipert P, Olschewski M, Allgaier U, Blum HE. A sphincterotome-based technique for selective transpapillary common bile duct cannulation. Gastrointest Endosc. 2000;52:387–391. doi: 10.1067/mge.2000.107909. [DOI] [PubMed] [Google Scholar]
- 21.Dumonceau JM, Devière J, Cremer M. A new method of achieving deep cannulation of the common bile duct during endoscopic retrograde cholangiopancreatography. Endoscopy. 1998;30:S80. doi: 10.1055/s-2007-1001379. [DOI] [PubMed] [Google Scholar]
- 22.Herreros de Tejada A, Calleja JL, Díaz G, Pertejo V, Esoinel J, Gacho G, Jimenez J, Millan I, Gasrcia F, Abreu L. Double-guidewire technique for difficult bile duct cannulation: a multicenter randomized, controlled trial. Gastrointest Endosc. 2009;70:700–709. doi: 10.1016/j.gie.2009.03.031. [DOI] [PubMed] [Google Scholar]
- 23.Freeman ML. Cannulation techniques for ERCP: one size does not fit all. Gastrointest Endosc. 2007;65:132–133. doi: 10.1016/j.gie.2006.07.038. [DOI] [PubMed] [Google Scholar]
- 24.Freeman ML. Adverse outcomes of endoscopic retrograde cholangiopancreatography: avoidance and management. Gastrointest Endosc Clin North Am. 2003;13:775–798. doi: 10.1016/s1052-5157(03)00107-7. [DOI] [PubMed] [Google Scholar]
- 25.Singh P, Das A, Isenberg G, Wong RC, Sivak MV, Agrawal D, Chak A. Does prophylactic pancreatic stent placement reduce the risk of post-ERCP acute pancreatitis? A meta-analysis of controlled trials. Gastrointest Endosc. 2004;60:544–550. doi: 10.1016/s0016-5107(04)02013-9. [DOI] [PubMed] [Google Scholar]
- 26.Elta GH. Temporary prophylactic pancreatic stents: which patients need them? Gastrointest Endosc. 2008;67:262–263. doi: 10.1016/j.gie.2007.07.037. [DOI] [PubMed] [Google Scholar]
- 27.Goldberg E, Titus M, Haluszka O, Darwin P. Pancreatic-duct stent placement facilitates difficult common bile duct cannulation. Gastrointest Endosc. 2005;62:592–596. doi: 10.1016/j.gie.2005.04.046. [DOI] [PubMed] [Google Scholar]
- 28.Misra SP. Pre-cut sphincterotomy: does the timing matter? Gastrointest Endosc. 2009;69:480–483. doi: 10.1016/j.gie.2008.11.030. [DOI] [PubMed] [Google Scholar]


