Abstract
When is it permissible to allow a newborn infant to die on the basis of their future quality of life? The prevailing official view is that treatment may be withdrawn only if the burdens in an infant's future life outweigh the benefits. In this paper I outline and defend an alternative view. On the Threshold View, treatment may be withdrawn from infants if their future well-being is below a threshold that is close to, but above the zero-point of well-being. I present four arguments in favor of the Threshold View, and identify and respond to several counterarguments. I conclude that it is justifiable in some circumstances for parents and doctors to decide to allow an infant to die even though the infant's life would be worth living. The Threshold View provides a justification for treatment decisions that is more consistent, more robust, and potentially more practical than the standard view.
Keywords: newborn infant, withholding treatment, medical ethics, quality of life, neonatal intensive care, disabled children
Withdrawal of life support is a frequent occurrence in newborn intensive care. In many units the majority of deaths follow decisions to withhold or withdraw treatment (Roy et al. 2004; Singh et al. 2004; Verhagen et al. 2009a; Wilkinson et al. 2006). There are two different contexts for decisions. Sometimes life support is withdrawn from infants who are dying, or who have such overwhelming illness that survival is unlikely. These decisions are largely uncontroversial. At other times life support is withdrawn from infants who might survive if all treatment were provided, for example, newborns with severe birth asphyxia (Case 1), premature infants with large brain hemorrhages, or infants with serious congenital abnormalities (e.g., severe spina bifida, trisomy 18 or 13). In such cases, treatment withdrawal is based upon predicted quality of life and is far more contentious (Verhagen et al. 2009a; Wilkinson 2009).
HENRY was born at 42 weeks gestation. When his mother arrived at the hospital in labor, the fetal heartbeat was found to be worryingly slow, and an emergency cesarean section was performed. Henry was born in poor condition and required extensive resuscitation. He was put on a mechanical ventilator and transferred to intensive care. He was floppy, comatose, and had abnormal electrical patterns on electroencephalogram. At 72 hours of age Henry remained dependent on the breathing machine, but his condition had stabilized. It appeared likely that he would survive if intensive care were continued. Magnetic resonance imaging of his brain at that time revealed abnormal signal in the basal ganglia, and absence of the normal signal in the internal capsule. His parents were told that based on his clinical condition and brain scan appearances Henry had a very high likelihood of developing severe spastic quadriplegic cerebral palsy with at least moderate cognitive impairment.1
Case 1: an infant with predicted severe impairment. Is it permissible to withdraw life support?
When is it permissible to withdraw life support from a newborn infant like Henry who would otherwise survive? One frequently encountered answer, at least as found in official guidelines, is that life support may be withdrawn only where the newborn's future is sufficiently dire that the burdens of treatment and of illness outweigh the benefits (American Academy of Pediatrics 1994; British Medical Association. 2007, 3; General Medical Council 2006; Tibballs 2007). It would be better for the infant if he were to die rather than to have life support continued.
But there are at least two problems for this view. The first is that it is not clear that all, or even the majority, of infants allowed to die in intensive care would have had lives so bad that they would have been better to have died in infancy. For example, some infants like Henry survive, albeit with severe impairments in physical and cognitive abilities. But it is not clear that their lives are so dreadful that it would be better for them to die than to continue to live (Case 2). The parents of such children often do not believe this is the case.2
MICHAEL is aged 7. He has severe spastic quadriplegic cerebral palsy, microcephaly, and epilepsy. He is cortically blind, and has severe intellectual disability. Michael appears to recognize the voices of his parents and teachers and responds with a smile. He also smiles and sometimes laughs in response to familiar music. Most of the time he does not appear to be in pain or discomfort. But he is not able to communicate verbally, nor with the aid of communication tools. He has a specially fitted wheelchair, but has no control over it. He is fed via a gastrostomy. Michael was in the newborn intensive care unit for a month after birth with severe birth asphyxia, and has had several hospital admissions since that time with prolonged seizures or chest infections. Michael's capacity for interaction is unlikely to change over time but his life expectancy is hard to predict. It is possible that he will survive into adult life, perhaps for several decades.3
Case 2: a child with severe impairment. Would it have been better for him if he had died in infancy?
The second problem is that faced with a prognosis like Henry's some parents request that life-support be continued, and doctors often support their request (McHaffie and Fowlie 1996, 205–215; Nuffield Council on Bioethics 2006, 101; Rennie and Leigh 2008; van der Heide et al. 1998; Whitelaw 1986). But if the burdens of treatment outweigh the benefits, it seems highly problematic to allow it to continue. Treatment withdrawal should be obligatory rather than optional.
There are different ways to respond to these challenges. We might question whether withdrawal of life support should be permitted from infants with severe impairment like Henry. Perhaps we are wrong to let them die? Alternatively, we may revise our judgment about the quality of life of surviving children like Michael with severe impairment. They would have been better to die in infancy. Perhaps we are wrong to continue life support? But there is another possible response. Where a critically ill newborn infant is predicted to have severe and irremediable impairment, such that they will not be able to take part in and realize many of the good features of life, it is permissible for parents and doctors either to allow them to die or to continue treatment. This may be the case even if it is likely that the child would have some overall benefit from life.
In this paper I set out and defend such a view. I focus on the practical policy question: In what circumstances should we permit parents and doctors to allow an impaired newborn infant to die?4 I start by relating the concept of a life worth living to future well-being, and point out an analogy with debates about “wrongful life” in conception decisions. I define two opposing views of the permissibility of treatment withdrawal: the Zero Line View, and the Threshold View. I outline four arguments in favor of the Threshold View and explore several challenges, including the relationship between those arguments and moral status.
My aim here is to argue in favor of a revised conceptual framework for decisions, not to set out in detail when treatment withdrawal should be permitted. However, I will end by setting out how the Threshold View might work in practice in newborn intensive care. The Threshold View would not necessarily lead to major changes in end-of-life care for newborns. But it would provide a better rationale for decision making in a number of important ways.
WELL-BEING AND A LIFE WORTH LIVING
Decisions about life support in newborn infants are based, inextricably, on predictions of future well-being, i.e., how well that individual's life is likely to go. There are various theories of well-being (Parfit 1984, 493–502; DeGrazia 1995; Griffin 1986, 7–74), but broadly there are three possibilities for a newborn:
A life worth living (LWL): A life in which future benefits for the individual outweigh burdens. There is positive net future well-being (Buchanan et al. 2000, 224; Garrard and Wilkinson 2006, 485).
A life not worth living (LNWL): A life in which future burdens for the individual outweigh benefits. There is negative net future well-being.
The zero point: A life in which future benefits for the individual are equal to burdens.5
The concept of a life worth living is controversial and sometimes confusing (Garrard and Wilkinson 2006, 485), and there are several competing meanings. There is an internal sense to a life worth living: Life is of sufficient value for the individual concerned to be worthwhile. This should not be confused with an external sense of the worth of a life, and its value to others (Buchanan and Brock 1986, 74). A second distinction is between the level of a life worth starting (for an individual who does not yet exist) and the level of a life worth continuing (for an existing individual) (Benatar 2006, 22–23). It is also possible to distinguish two ways of determining whether a life is above or below the zero point. There is an objective sense wherein we impartially balance the intrinsically good states against the bad in an individual's life. And there is the subjective judgment of the individual that life's positives outweigh the negatives and that it is worthwhile continuing to live (McMahan 1998, 226–228).
I use LWL to refer exclusively to the internal sense of a life worth continuing. The arguments that follow apply equally to subjective or objective senses of a LWL.
TWO VIEWS ABOUT THE PERMISSIBILITY OF CONCEPTION
The concept of an LWL has been central to some debates about artificial reproduction and conception decisions. Is it permissible for parents to deliberately implant an embryo that will have significant impairment or illness (e.g., deafness)? One view, as expressed by John Harris, is that it would be permissible as long as the child's future well-being were predicted to be above the zero point (Harris 2000). The child has not been harmed since he or she has an LWL and since the child would not otherwise exist. This has been referred to as a “zero line view.”6
But this view conflicts with commonsense morality as expressed by Bonnie Steinbock:
It's … a question of whether to create a child who is likely to have a life marked by pain and severe limitations…. What reason could be offered in justification of an affirmative answer? That the child's life, while miserable, is not so awful that he or she will long for death? That is not the kind of answer a loving parent could give. (Steinbock and McClamrock 1994, 18)
Steinbock and several other philosophers have rejected a zero line view for conception decisions (Archard 2004; Kavka 1982; Steinbock and McClamrock 1994). They have argued that instead of the zero point of net well-being, a higher standard should be applied. It is not permissible to undertake artificial reproduction unless the child will have at least a minimum level of well-being—the child's life will be above a certain threshold.
TWO VIEWS ABOUT TREATMENT WITHDRAWAL AND NEWBORN INFANTS
The setting for treatment withdrawal decisions is different—the judgment is inverted, but a view that parallels the Harris's view of permissible conception is:
The Zero Line View: Life support may be withdrawn from a newborn infant if and only if future burdens for the individual outweigh benefits, i.e., they are predicted to have a life not worth living.
The Zero Line View overlaps with another common way of expressing the permissibility of treatment withdrawal in newborns. This is the view that treatment may be withdrawn only if it would be in the best interests of the infant to die. Many writers when referring to best interests appear to be using a version of the Zero Line View (Arras 1984; Hope 2004, 50; Nuffield Council on Bioethics 2006, xxiii, 12; President's Commission 1983, 218; Sayeed 2006; Tibballs 2007).7
There is a second view about treatment withdrawal that is analogous to the Steinbock view about conception:
The Threshold View: Life support may be withdrawn from a newborn infant if and only if their net future well-being falls below a certain minimum threshold. This threshold is above the zero point of a life worth living.
These two views are summarized in Figure 1, which uses the following additional concepts.
Figure 1.
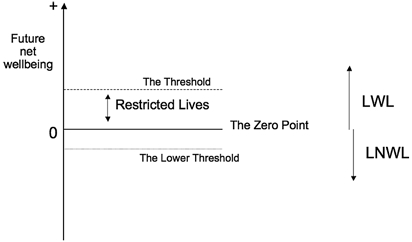
The permissibility of treatment withdrawal from newborn infants based upon predicted future well-being.
Restricted life: A life in which net well-being is above the zero point but below the threshold (Kavka 1982, 103).
The threshold: A positive (supra-zero) level of net well-being defining the upper border of permissibility of treatment withdrawal. It is obligatory to continue life support for newborns with predicted well-being above this level.
The lower threshold: A negative (below zero) level of net well-being defining the lower border of permissibility of treatment continuation. It is obligatory to withdraw life support for newborns with predicted well-being below this level.
There are three key features of the Threshold View. First, it explicitly permits allowing newborn infants to die who are predicted to have lives worth living. Second, below the threshold, treatment may be permissibly withdrawn or may be continued. Finally, in Figure 1, a lower threshold marks the point at which treatment may not be continued even if parents request it. I focus mostly on the (upper) threshold. The arguments that follow provide reasons why the threshold should be above the zero point. However, they also provide reasons why the lower threshold should be below the zero point.
The preceding view has some similarities to a classification of treatment for extremely premature infants elaborated by Tyson and colleagues and by John Paris (Tyson et al. 1996; Paris et al. 2007). The upper threshold would correspond to the point at which treatment becomes “mandatory,” the lower threshold corresponds to the point of “unreasonable” treatment. Between the two thresholds treatment is “optional.” The Threshold View can be seen as an attempt to relate these categories to the concept of an LWL, as well as to provide a robust defense of such a categorization. It extends such a categorization to infants with predicted impairment.8
I return later to where the threshold might be drawn. It may help for what follows, however, to give some idea of the conditions that would potentially fall below the threshold but above the zero point (i.e., restricted lives). I described earlier Michael (Case 2). His cognitive, physical, and sensory impairments fundamentally diminish his ability to communicate, interact, and develop goals. His well-being is restricted by his impairments in ways that cannot be overcome no matter how much support his parents or society provide to him. Other conditions in this category might include spinal muscular atrophy (type 1) or trisomy 18. For infants with these conditions, treatment may be continued or may be withdrawn.
ARGUMENTS IN FAVOR OF THE THRESHOLD VIEW
The Argument From Uncertainty
Uncertainty is common in newborn intensive care. Prognostic uncertainty arises from a number of factors including plasticity of the developing brain, individual resilience, the influence of the environment and treatment, and limitations in clinical assessment and prognostic tests (Shevell et al. 1999). There is further uncertainty about future experiences, particularly of individuals with significant cognitive impairment. For example, even if we knew the exact degree of future impairment we would remain unsure of how much pain or pleasure the child would experience. This experiential uncertainty makes it difficult to know whether life would be above or below the zero point.
There are two ways in which uncertainty may justify the threshold.
Uncertainty and Asymmetry of Harms
In a state of uncertainty, if we choose the zero line as the cutoff point for treatment withdrawal, it is inevitable that some infants who survive will actually have lives not worth living. Imagine, for example, an infant predicted to have future net well-being of zero.9 We make this prediction based upon median well-being in a group of past infants with relevantly similar prognostic features. On the Zero Line View this is the upper limit of permissible withdrawal. However, given our uncertainty, this infant has a 50% chance of actually experiencing well-being above the zero point, and a 50% chance of well-being below this point. Should we weigh these possibilities equally? One reason to reject this idea and adopt a higher threshold is an asymmetry between harms. It may be a worse mistake to allow a newborn to live with an LNWL than to allow a newborn to die who would have had an LWL—where the infant would have had a restricted life.
A newborn who survives in a state of such severe impairment and suffering that the child's life is not worth living has been harmed by a decision to prolong his or her life (Feinberg 1986; Benatar 2006, 20–22; McMahan 1998). On the other hand, a newborn who dies but who would have had an LWL has also been harmed. But these two harms differ in nature and magnitude. The harm of death for the second infant lies in being deprived of future well-being (Marquis 1989). Yet the degree of this harm depends on how good that life would have been. If, for example, the child would have lived a restricted life, the amount of net positive well-being that the child has lost is potentially small. What is more, the child was not and is not conscious of this loss. The child will never be in a position to regret the decision that led to his or her death. On the other hand, the harm of life for the child with an LNWL is experienced and may be regretted. Indeed, many would consider this one of the most serious harms imaginable.
Asymmetrical harms in conception decisions have been discussed previously (McMahan 2009). Although it is generally accepted that an individual can be harmed by coming into existence, there is no individual who is harmed if an individual (who would have had an LWL) is not conceived. This asymmetry is related to that problem, but it is different in one important way. There is an individual existing (the newborn) to whom harm could be attributed if the newborn dies. However, the nature of that harm is attenuated because of this newborn's limited awareness.
There are different possible versions of the asymmetry argument. I do not claim that there is no harm to an infant who is allowed to die (but would have had an LWL). Nor do I claim that any risk of an LNWL outweighs the risk of allowing an infant to die with an LWL. That would potentially warrant treatment limitation in any situation where there is the possibility of survival in a harmed state. There is, however, widespread intuitive support for at least some degree of asymmetry between harms and benefits (Alm 2009; Benatar 2006, 30–36; Kamm 2007, 17). Most parents and doctors, I suspect, have greater concern for the potential future harms to infants than for their future benefits. Such concern is sometimes expressed in the principle of non-maleficence (Beauchamp and Childress 1999, 120–193). To support the Threshold View I need only make the more moderate claim: It may be worse to allow an infant to live with an LNWL, than to allow a newborn to die who would have had a restricted life.10
Uncertainty and Liberalism
Some may reject the asymmetry argument. They may believe, contrary to the preceding claims, that death for an infant who would have had an LWL is one of the worst possible harms (Kon 2008, 28) and that the threshold should perhaps be below the zero point. But uncertainty provides a second argument in favor of the Threshold View. Prognostic uncertainty and experiential uncertainty make it difficult to know whether or not an infant will have well-being above the zero point. There is also significant moral uncertainty about how to evaluate future benefits and burdens. It is unclear which theory of well-being we should apply, and how we should weigh different harms. There is likely to be disagreement about the probability of an LNWL that would be sufficient to justify allowing a newborn to die.
The problem of moral uncertainty is complicated (Lockhart 2000) and beyond the scope of this paper. But one plausible approach to policy in the face of different normative beliefs is to give individuals the freedom to decide for themselves which values to apply to their own lives. This principle is extended to include decisions by parents on behalf of their children. The state will only interfere with parental choices where there is a significant risk of substantial harm to the child (Diekema 2004). One response to decision making for newborn infants would be to give parents the discretion to decide whether or not to continue life support when there is genuine uncertainty about whether a child will have a life above or below the zero point. The two thresholds would mark the boundaries of parental decision making.
Others have made this claim about uncertainty and parental freedom.11 It has some similarities with the idea of a “gray zone” for neonatal treatment decisions (American Academy of Pediatrics Committee on Fetus and Newborn 2007; Harrison 2008). However, the Threshold View differs from conventional accounts of the gray zone in several ways. First, I have argued that this zone will extend above and below the zero point. The Threshold View explicitly acknowledges that it may be permissible to withdraw life support from infants who will probably have lives above the zero point, whereas some descriptions of the gray zone seem to extend only below the zero point. Second, the threshold is based upon both prognostic and moral uncertainty. And third, there may be reasons to support a supra-zero threshold even where there is certainty about outcome.
What if we were certain that an infant would have an LWL? Imagine an infant with a genetic disorder uniformly associated with profound cognitive impairment (he will have the cognitive capacities of a 3-month-old infant). Children with this condition usually have good physical health, and do not suffer from illness or require painful medical interventions. (Call this the Harmless Case.)12 If there is no chance of this infant having an LNWL, is it still permissible to withdraw life-sustaining treatment?13
The Argument From Other Interests
One reason why we may be permitted to withdraw life support in the hypothetical Harmless Case is because of the burden of care. Individuals with severe impairment often need substantial support throughout their lives. Their care usually falls upon immediate family, often involving physical, financial and emotional burdens. There are well-documented potential costs for families in psychological and physical illness as well as marital discord and breakup (Barlow and Ellard 2006; Harrison 2008; Murphy et al. 2007; Raina et al. 2005; Reichman et al. 2008; Macks and Reeve 2007; Williams 1997). The care of individuals with severe impairments also imposes significant costs on society. Their education and health needs are substantially greater than for children and adults without such impairments.
On the Zero Line View there is no scope for taking such factors into account except insofar as they determine whether or not the child will have an LWL. But in practice there is a recognition that the interests of parents and of siblings should be given some weight (McHaffie and Fowlie 1996, 67, 73, 87; Nuffield Council on Bioethics 2006, xvii, 17). Most pediatric and neonatal intensivists appear to incorporate family interests into decision making (Hardart and Truog 2003). Yet if parental or family interests are to have any role in decisions about withdrawal of treatment, this would necessarily support the Threshold View. After all, if these interests could only be taken into account when the child's life was below the zero point, they would actually be playing no role at all in determining the permissibility of withdrawal of treatment.
When would the interests of others justify allowing an infant to die? One way of answering this question is by determining when society is prepared to take over the care of a child. If the future burden of care is sufficiently great that parents are not able or willing to look after the child, the alternative to allowing the infant to die would be for her or him to be adopted or put into foster care. In the hypothetical Harmless Case, the infant will certainly have a life worth living. But supporting the infant involves considerable cost, while providing only a small benefit to the child. When resources are limited, the provision of lifesaving treatment to an infant with a restricted life may mean that other children or adults are denied surgery or medical treatment, or other children with impairment are denied educational and supportive care. The level of impairment that a society is able to support will depend upon the resources available. In societies that are very impoverished, the threshold would potentially be higher than in societies that have ample resources.
What if there were no costs and no harm? If we imagine a version of the Harmless Case such that the care of the child will not cause a burden on parents and will not divert needed health and educational resources away from others, there would no longer be a positive reason to allow the child to die. Correspondingly, we should not permit life support to be withdrawn in a Harmless Costless Case. But in practice such cases will rarely, if ever, occur. Infants who are predicted to have very severe impairment have a real risk that their future well-being will fall below the zero point, and their care substantially affects the interests of others. These reasons converge to support the Threshold View.
Deontological Arguments for the Threshold
Arguments in favor of a threshold view for conception decisions are based on parental duties or rights. Steinbock refers to a “principle of parental responsibility” (Steinbock and McClamrock 1994). David Archard argues that a “minimally decent life” provides a constraint on parental reproductive rights (Archard 2004). Both accounts seek to explain why it would be wrong to deliberately conceive a child with a restricted life. But these arguments do not necessarily extend to treatment withdrawal decisions.
Nevertheless, the threshold could be seen as providing a constraint to a different duty. Parents and doctors have a strong prima facie duty to do what they can to preserve the life of a newborn infant. In the previous section I discussed the possibility that this duty may be outweighed. But there may also be limits to it. We are not obliged to keep a child alive who is dependent on life support and in a permanent vegetative state. A life of permanent unconsciousness offers no benefit to the child, and dissolves the normal duty to preserve life.14 But where a child's future life is predicted to contain a very low amount of positive net well-being, the duty to preserve life may also be significantly attenuated or absent.15 On this basis it would be permissible for parents and doctors to elect not to preserve the life of a newborn predicted to have a restricted life.
A complementary way of justifying the Threshold View would be in terms of the right of parents to make decisions about their children. For most decisions there is a rebuttable presumption that parents have such a right (Dare 2009). This might be justified by parents’ right to autonomy, but also by the value of preserving intimate family relationships, and in the avoidance of undue state interference in family life (Downie and Randall 1997; Schoeman 1985). Again, if such a right has any relevance for decisions about life-sustaining treatment, it would necessarily support the Threshold View.
The preceding arguments about the duties or rights of parents capture an intuitive sense that there is more to such decisions than the Zero Line View would imply. For parents and doctors to be obliged to preserve the life of the infant, or for society to overrule parents’ right to decide, the infant's life must be more than one barely worth living; it must be above the threshold; it should be a life worth giving.
COUNTERARGUMENTS TO THE THRESHOLD VIEW
The Threshold View will be controversial for some. What arguments might be presented against it?
The Scope of the Threshold and the Moral Status of Newborn Infants
I have referred exclusively to newborn treatment decisions. But there might be a concern that the Threshold View would justify the withdrawal of life-sustaining treatment from older children or adults with LWL. Alternatively, it could be argued that the Threshold View should be resisted since it permits different standards for treatment decisions, and by inference, different moral status for newborn infants (Janvier et al. 2007).
A full discussion of the moral status of newborn infants is beyond the scope of this paper. But if the threshold is to apply to newborn infants and not to older patients it must imply that they warrant different moral consideration.16 There are several reasons that would support such a view. First, a newborn's interest in her or his future well-being may be diminished by her or his reduced awareness of her-or himself, and of that future (McMahan 2002, 170). This affects how that interest should be weighed against other interests and other considerations and gives rise to the asymmetry in harms noted earlier. Second, there is greater uncertainty for newborn treatment decisions than for older children and adults.17 This arises from the greater degree of plasticity and thus variability in response to injury (Stiles 2000) and from their greater developmental immaturity, making clinical assessment difficult (Shevell et al. 1999). It gives more weight to the arguments from uncertainty.18 Third, there is often a long period of time before the extent of an infant's impairment is known. By the time that it is clear that he or she is destined for an LNWL, an infant may no longer be dependent upon life-sustaining treatment. Prolonged survival in a harmed state is possible. These three reasons would not usually apply, or would apply less forcefully, for older children or adults.19 It would be appropriate to use the zero line for determining the permissibility of withdrawal of treatment outside the newborn period.
What is the relationship between well-being and moral status? It is not that future low levels of well-being make an individual less worthy of moral consideration. Rather, the moral status of an individual determines how we should take into account the well-being in that person's future and whether it is obligatory to preserve their life. The moral status of an adult would remain unchanged following a prediction that the adult's future contains only a very slight positive balance of well-being or even net negative well-being (though this would potentially have major implications for their treatment). Similarly, a newborn's moral status is not altered by predicted future impairment. However, in newborn infants it is legitimate to use a different well-being threshold for deciding whether or not to continue to keep them alive.
The other question about the scope of the Threshold View is about the period during which it should be applied. One approach might be to limit it to the first month of life (or to 1 month corrected age for infants born prematurely). Such a time limit would be in one sense arbitrary, but also defensible. I return in the following to the question of arbitrariness and the Threshold View.
The Threshold and Discrimination
It may be objected that the Threshold View represents a form of discrimination against disabled infants.
However, the justification for treatment withdrawal on the Threshold View is based on future well-being, not on disability or impairment. If an infant were predicted to be impaired, but to have future well-being significantly above the zero point, it would not be permissible to allow them to die. The Threshold View would also, in theory, permit treatment withdrawal from an infant who did not have a physical or cognitive impairment, but who was predicted to have levels of well-being only just above the zero point.20
In practice, the majority of infants with restricted lives would be infants with predicted impairment. Yet it does not follow that this represents a form of wrongful discrimination (Arneson 2006). Treatment withdrawal on the Zero Line View is not thought to be discriminatory even though it largely affects impaired infants. Future impairments do not change the moral status of an individual. The question is whether they affect well-being. Some types of impairment, for example, severe cognitive impairment, necessarily reduce the amount of well-being in an infant's future life (Kahane and Savulescu 2009). Other impairments only contingently reduce well-being, depending upon the support provided to the impaired individual and the social context in which they live. Such impairments would not, in my view, justify withdrawal of life support.
Arbitrariness of the Threshold
One potential concern with the Threshold View is that there is no nonarbitrary way of arriving at a threshold.21
There are, however, different senses of arbitrariness. A cutoff point may be arbitrary in the sense that it could be defensibly drawn at a different level. Or it could be arbitrary in the sense that there is no reason to make the distinction. A law that allows people to apply for a driving license after the age of 18 years is arbitrary in the first sense. But there is good reason to draw a line somewhere, and a number of reasons why a point in the late teenage years is an appropriate place. It is not arbitrary in the second sense. Similarly, there are multiple plausible places to draw a threshold for treatment withdrawal, but a number of reasons (outlined earlier) why the threshold should be set above the zero point.
Second, a decision, on the basis of the Zero Line View, that a newborn should or should not be allowed to die may also be criticized on the grounds of arbitrariness. There is profound uncertainty about how to define the zero point and substantial prognostic uncertainty about whether or not an infant will fall above or below it. Furthermore, it is simply unclear, on the Zero Line View, what level of certainty (that an infant will live an LNWL) would justify treatment withdrawal.
Third, even if the threshold is arbitrary, there is a further question about whether this should lead us reject the Threshold View. Given the important practical need to determine whether or not treatment withdrawal is permissible, and the reasons that I have outlined in favor of a supra-zero threshold, it may be that the disadvantages of greater arbitrariness are outweighed by the other advantages of the Threshold View.
The Best Interests of the Infant
Another potential objection to the Threshold View is that it would be contrary to the best interests of the infant to permit withdrawal of treatment if the individual were predicted to have an LWL.
If the objection is that the Threshold View would be contrary to the legal best interests principle, it may have some traction. Previous legal judgments about withdrawal of life support (at least in the United Kingdom) have often used the concept of “intolerability,” which appears to be a stringent subjective version of the Zero Line View.22 But the arguments here are about what policy should be—not about what is currently permitted.
Alternatively, the objection might be that the Threshold View is inconsistent with the ethical principle of the best interests of the child. If the best interests principle is equivalent to the Zero Line View, the Threshold View will diverge from best interests. But if that is the case, the arguments given earlier provide reasons for either rejecting or modifying the best interests principle for newborn treatment decisions.
The Threshold View may also be consistent with the best interests principle. I discussed the asymmetry between harms. But we could also express this in terms of the balance between a newborn's interest in not living an LNWL and in realizing a future LWL. The arguments given earlier would give us reason to weigh the former interest as potentially stronger than the latter—particularly where the infant's future well-being is predicted to be low. Furthermore, at least some descriptions of the best interests standard allow a role for taking into account the interests of others (Kopelman 2007) in a way that supports a supra-zero threshold. It could be in an infant's best interests to be allowed to die, though the infant is predicted to have an LWL.
WELL-BEING AND WITHDRAWAL: IMPLICATIONS OF THE THRESHOLD FOR TREATMENT DECISIONS
The aim of this paper has been to defend an alternative framework for treatment withdrawal decisions, not to set out a particular cutoff point. But how could we arrive at a substantive definition of the threshold, and what would the implications be for treatment decisions? A full answer would need to draw on an account of well-being (Crisp 2006; Kraut 2007; Sumner 1996) and on empirical data on conditions and their effect on well-being, and ideally seek consensus about those conditions where parental discretion in treatment decisions is reasonable. Here I can only hope to make a preliminary suggestion.
The preceding arguments may prove useful in setting out the necessary and sufficient conditions (C) for the thresholds, as follows.
Normative Criteria for the Threshold
Treatment withdrawal is permissible for infants with conditions that:
C1. Reduce future well-being, either by reducing benefits or by imposing substantial burdens on the child (or both) AND
C2. Are close to the level of an LNWL, AND EITHER
C3. Involve a significant risk of an LNWL OR
C4. Impose a substantial burden of care on others.
Normative Criteria for the Lower Threshold
Treatment continuation is not permissible for infants with conditions that:
C1. Reduce future well-being, either by reducing benefits or by imposing substantial burdens on the child (or both) AND
C5. Render it highly likely that the infant will have an LNWL and be harmed by continuing treatment.
Practical Criteria
What is a “significant” risk, or a “substantial” burden of care? Which conditions are close to the level of an LNWL? If the Threshold View were adopted it would be important to provide clinicians and parents with some idea of the sorts of conditions that would fall into the different normative categories that I have described. Figure 2 represents an attempt to apply the Threshold View to prognostication in birth asphyxia, the condition that affected Henry and Michael.
Figure 2.
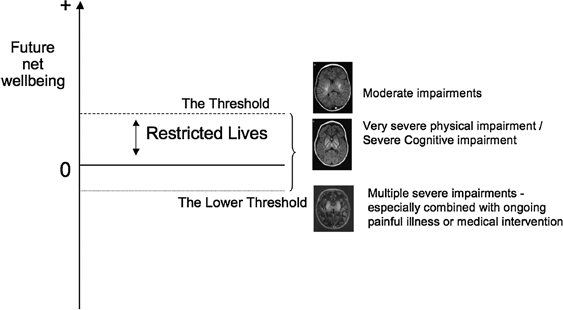
The Threshold View and predicted impairment in birth asphyxia.
In Figure 2 I have drawn the threshold at the level of severe cognitive impairment23 or very severe physical impairment.24 Why choose this level? Children with moderate physical impairment are usually able to walk with assistive mobility devices (Himmelmann et al. 2006), while individuals with moderate cognitive impairment (IQ 35–50) are usually socially interactive and able to communicate at least to the level of basic needs, and often can carry on simple conversations (Harris 2006, 54). Both types of impairment would be consistent with a broad range of goods on either subjective or objective theories of well-being. It is not usually thought that such individuals have an LNWL, nor that there is a significant risk of this befalling them.
In contrast, for individuals with very severe physical impairment or with severe cognitive impairment it is more questionable whether their lives fall above the zero point, and more reasonable to worry that they may have an LNWL. It is for infants with this level of impairment that there is most debate about whether or not treatment is in their best interests. Although Henry may be expected to have a life that is worth living, there is a risk that his impairments will be more severe than anticipated, or that other medical problems arise. It is also for such infants, particularly those with severe cognitive impairment, that the benefits of life appear clearly diminished (McMahan 2009; Wilkinson 2006).
I have not indicated a specific statistical threshold, but the arguments from uncertainty would suggest that it is reasonable to give weight to at least modest chances of significant harms. Is it possible to be more specific? One way of capturing this idea without using specific numerical thresholds would be by borrowing the language of the law. Civil cases are often settled on the basis of the balance of probabilities, while criminal conviction is usually required to establish guilt beyond reasonable doubt (Murphy 2007, 111). The latter is unsatisfactory for the threshold, since there is always some doubt about prognosis. Stipulating the former would permit treatment withdrawal in infants with a slightly less than 50% chance of survival without severe impairment, which may give too great a weight to survival with a restricted life. In the absence of a better standard, I suggest that it would be permissible to withdraw treatment if there is clear and convincing evidence that an infant will have severe impairments as described earlier.25 Similarly, if there is clear and convincing evidence that continuing treatment would harm an infant, it should not be provided even if parents request it.
The idea that life support may be permissibly withdrawn from newborn infants who are predicted to have lives worth living may seem striking, even shocking to some. But in fact this proposal is not a radical suggestion. The Threshold View as I have outlined it is broadly consistent with current practice in many neonatal units. On the basis of the guideline outlined earlier, it would be permissible to withdraw life support from newborn infants with predicted severe cognitive deficits, including infants like Henry who have had severe hypoxic ischemic brain injury, congenital brain malformations such as lissencephaly, or infants with trisomy 13 or 18. It would also potentially include infants with overwhelming physical impairments such as spastic quadriplegic cerebral palsy, severe spina bifida, or spinal muscular atrophy.26 It would not permit withdrawal of life support from infants with Down syndrome27 or milder forms of spina bifida.
However, one advantage of the Threshold View is that it does not commit us to saying that the lives of children with the severe impairments outlined earlier (e.g., Michael) are not worth living. Unlike the Zero Line View, it does not commit us to the judgment that if parents refuse to allow withdrawal of life support from the infant, they, and by extension any doctors who go along with their request, are harming the infants. It is consistent with the approach adopted currently in many neonatal units. In cases like those described here, doctors do not force parents to agree to withdrawal of life support. In my experience they often do not even try to persuade parents that treatment should be withdrawn. On the contrary, withdrawal of life support is offered to parents as an alternative that they may choose to embrace (Wilkinson 2010b). With rare exceptions, doctors usually comply with parental requests to continue life support.28
There are two other advantages of the Threshold View over the Zero Line View. The Threshold View potentially provides more practical assistance with decision making than the Zero Line View. The problems with determining exactly where the zero point lies raise serious challenges about how to apply the Zero Line View in practice. How severe does impairment have to be to make an LNWL? What probability of severe impairment would warrant a judgment, based on the zero line, that treatment should be withdrawn? On the other hand, if we adopted the Threshold View it might be possible to generate far more specific and detailed guidelines about the types of conditions where parental discretion would be permitted, and those where it would not. Figure 2 represents an attempt to do this for birth asphyxia. If such guidelines could be generated, the Threshold View would have the potential to lead to more consistent decision making between doctors and between hospitals.
CONCLUSION
A decision to allow a newborn to die is one that no doctor or parent takes lightly. But such decisions are a regular part of work in newborn intensive care. The prevailing view of the permissibility of withdrawal of life support (at least as expressed in written guidelines for decisions) is one that I have here labeled the Zero Line View—treatment may be withdrawn only where an infant is predicted to have a life not worth living. I have outlined and defended an alternative to that view. On the Threshold View it is not obligatory to continue life support for infants who will have very low levels of well-being. Recall the infant Henry described at the start of this paper. It is simply unclear whether or not his future life will be so bad that it would be better for him to die than to live. I have not argued that treatment should be withdrawn in such cases. Henry may turn out to have a life worth living. We should permit Henry's parents to decide to continue treatment. If they do choose continued treatment, we should support them as much as possible to maximize the well-being for their child. But we can be reasonably certain that if Henry survives, his capacity to experience the goods of life will be severely constrained. To keep Henry alive risks a very serious harm—that of being harmed by life. Treatment will impose serious burdens on Henry's family while yielding relatively little benefit to Henry. His parents have a right to decide about treatment given reasonable disagreement about how to weigh the risk of an LNWL and because they will ultimately bear the costs of that choice.
The Threshold View, as I have outlined it, would not necessarily lead to a radical change in practice in newborn intensive care. It would not lead to withdrawal of life support from infants with a reasonable chance of a good life. It accords with a sense (that I suspect many parents and neonatologists share) that for us to be obligated to save a life it must not only be a life worth living, it must also be a life worth giving. There is further work to be done in order for such a view to be translated into practical guidelines. But I have argued here that such a view is superior to the standard way of thinking about these decisions in a number of important ways. The Threshold View provides a more consistent, more robust, and potentially more practical basis for the withdrawal of life support from newborn infants.
Footnotes
Acknowledgments: I am extremely grateful for the support of Tony Hope and Julian Savulescu in the preparation of this paper, who read and commented on several previous drafts of this article. I have also benefited substantially from discussions and comments with Derek Parfit, Jeff McMahan, Tom Douglas and Toby Ord, and from the comments of three anonymous reviewers. Dominic Wilkinson was supported by an Oxford Nuffield Medical Fellowship, Eric Burnard Fellowship, and Royal Australasian College of Physicians Astra-Zeneca Medical Fellowship during the preparation of this article. This work was supported in part by a grant from the Wellcome Trust [086041/Z/08/Z]. The funders had no involvement in this work.
1. Rennie, Hagmann, and Robertson (2007) and Wilkinson (2010a). This case is fictitious but representative of a fairly common situation in newborn intensive care. It is not unusual for lifesaving treatment to be withdrawn in situations such as this.
2. There are, to my knowledge, no surveys of such parents, but the narrative accounts of parents with severely impaired children confirm this impression (see for example “The Ashley Treatment” 2007; Cogan and Whardall 2008; Nugent et al. 2008; Sheffield 2007; Wyn 2007; Yorgason 2003). Although it is possible that caregivers are biased in their assessment, and systematically overemphasize the positives while underestimating the negatives for the child, there is an argument that bioethicists should not discount the views of disabled people (and by extension their caregivers) (Goering 2008). In my experience at least, if such children require short-term treatment for life-threatening illnesses, it is usually provided.
3. This case, too, is completely fictional. But it describes the condition of many children whom I have cared for. As will become clear, I do not claim that Michael should now be allowed to die. In fact, I believe that we should provide him with lifesaving medical treatments as long as they do not cause him prolonged suffering. But the key question is whether it would have been permissible for Michael to be allowed to die in infancy.
4. I restrict discussion to the issue of withdrawal of or withholding treatment in newborns. These arguments should not be taken to have direct implications for debates about whether or when it is permissible to actively end the life of a newborn, for example, as allowed in the Netherlands under the Groningen protocol (Verhagen and Sauer 2005). If it is ever permissible to euthanize a newborn infant, the threshold for permissibility might be significantly different from that articulated here.
5. The zero point is a philosopher's abstraction (Glover 2006, 57). But it represents a useful way of conceptualizing decisions about life and death. Some people reject the idea of a zero point because they deny that the negatives of life can ever outweigh the positives (Garrard and Wilkinson 2006, 486; Wyatt 2005). Others may reject it on the grounds of incommensurability. I assume in what follows that there is a zero point of well-being even if it is hard to identify.
6. Glover (2006, 53). A zero line view is one that draws a normative distinction at the zero point.
7. Whether a best interests judgment necessarily means adopting this view is a further question that I return to later.
8. Other writers discussing treatment withdrawal for newborn infants have also articulated views with some similarity to the Threshold View. They have argued that it may be permissible to allow newborns to die who lack certain key capacities (for example, the capacity to develop relationships, or to engage in minimal social interaction), or whose lives are not going to be meaningful (Arras 1984; Doyal and Durbin 1998; Engelhardt 1978; Kohl 1978; McCormick 1974). These authors do not talk explicitly about well-being and whether such lives would be worth living. They are also somewhat unclear about whether it would be permissible to continue life support for an infant lacking those key capacities. For similarities between the Threshold view and the “gray zone” for treatment decisions see later discussion in this article.
9. Set aside for the moment the doubts that we may have about quantifying well-being or about determining the zero point.
10. Although not expressing it in terms of asymmetrical harms, Kenneth Kipnis (2007) has also argued that the risk of an LNWL would justify allowing an infant to die.
11. See for example Boyle and colleagues (2004), Diekema (2004), and Jonas (2007). The 1983 U.S. President's Commission report also included a category of “ambiguous or uncertain” treatment warranting parental discretion in treatment decisions (President's Commission 1983, 218–223).
12. The harm here refers to the individual. As is next discussed, other harms may still be possible.
13. Some may still be tempted in such a case to think that the zero point is above this level and that perhaps it would be better for the infant to die in such a case. But there are at least two problems with such a view. First, we do not generally think that the lives of 3-month-old infants are bad lives. (We may be glad that they subsequently develop, especially if we are their sleep-deprived parents, but that is a separate issue.) Second, such a view would appear to imply that the lives of many nonhuman animals (with cognitive capacities no greater than a 3-month-old human infant) are bad, and that it would be better for them to die. This seems highly implausible.
14. The majority of pediatric intensivists surveyed would limit treatment in the setting of predicted vegetative state (Devictor et al. 2008). Surveys of patient preferences also suggest that the vast majority of adults would not want life-sustaining treatment provided if they were in a vegetative state (Emanuel et al. 1991). While the 2004 statement by Pope John Paul II maintained that patients in a vegetative state retain a right to certain basic treatments, including artificial nutrition and hydration (Pope John 2004), the Catholic church has long held that the duty to preserve life is relative rather than absolute (Clark 2006). For patients in a vegetative state, mechanical ventilation and intensive care would usually be regarded as extraordinary means and therefore not obligatory (Clark 2006).
15. A version of this argument is expressed by John Arras: “In the absence of certain distinctly human capacities … the duty to sustain life loses its hold on caregivers” (Arras 1984, 32).
16. Moral status is sometimes discussed as if it were an all-or-none phenomenon, as evidenced by the question “does X have moral status?” But it arguably makes more sense for moral consideration to admit of degree, and for the appropriate question to be “what moral status does X have?” (DeGrazia 2008).
17. It is difficultto quantify uncertainty, and there are (to my knowledge) no studies that have compared prognostication between newborns and older patients. However, for the reasons given earlier, this appears likely to be the case.
18. Some may reject the arguments from uncertainty. They may believe, for example, that treatment withdrawal is only permissible where there is a very high degree of certainty about prognosis. If this were the case, greater uncertainty about outcome for newborn infants would potentially warrant less parental discretion. (I am grateful to an anonymous reviewer for this point.)
19. I set aside here the question of whether a supra-zero threshold should be applied to decisions about life support for older individuals whose awareness of themselves and of their future is no greater than newborns.
20. For example, imagine an infant with a very limited life expectancy (for example, a matter of days), but who appears to be suffering little, if at all. Their brief future life may well contain a positive balance of well-being. If so, the Zero Line View would appear to mandate that treatment continue. On the Threshold View, however, it would not be obligatory to continue life support.
21. A similar objection has been raised against threshold views for conception decisions (Garrard and Wilkinson 2006).
22. See for example Re J ([1991], 55F).
23. A standard definition of severe cognitive impairment includes an intelligence quotient (IQ) of 20–35. Individuals with this level of impairment usually also have impairment of motor skills, difficulty in ambulation, and limited communication ability. Most require close supervision and care throughout life (Harris 2006; King et al. 2000).
24. I use very severe physical impairment to refer to severe quadriplegia with a Gross Motor Functional Classification System level 5 or equivalent (self-mobility is severely limited even with assistive devices) (Wake et al. 2003; Palisano et al. 1997).
25. The clear and convincing evidence standard is used in some American legal cases, and indicates a high degree of probability—more than 50%, but less stringent than beyond reasonable doubt (Murphy 2007, 111).
26. Although I have focussed on infants with predicted impairments, the Threshold View might also include infants born at the borderline of viability (for example, the Messenger case, or the case of Miller v. HCA), where a significant risk of dying, or of survival with severe impairment is often taken to permit parental discretion about resuscitation (American Academy of Pediatrics Committee on Fetus and Newborn 2007).
27. For example, the U.S. Bloomington Baby Doe case, or the UK case of “B” (Paris 2007; Ahluwahlia et al. 2007).
28. There is little data on conflicts in end-of-life decision making in newborn infants, but this may vary between cultures. In one recent study from the Netherlands, doctors agreed to continue treatment in all cases where parents opposed treatment withdrawal (Verhagen et al. 2009b). From an earlier survey of neonatologists it was estimated that in 20–25 infants per year in the Netherlands treatment was not withdrawn because parents refused consent for this (van der Heide et al. 1998). In a comparative qualitative study in U.S. neonatal units treatment was continued in all cases where parents declined treatment withdrawal (Orfali 2004). However, in French neonatal units decisions about treatment were made by medical staff and conveyed to parents (Orfali 2004).
References
- Ahluwalia J., Lees C., Paris J. J. Decisions for life made in the perinatal period: Who decides and on which standards? Archives of Disease in Childhood—Fetal and Neonatal Edition. 2008;93((5)):F332–F335. doi: 10.1136/adc.2006.113373. [DOI] [PubMed] [Google Scholar]
- The “Ashley treatment”: Towards a better quality of life for “pillow angels.” 2007. Available at: http://ashleytreatment.spaces.live.com/blog/cns!E25811FD0AF7C45C!1837.entry (accessed February 2, 2010)
- Alm D. Deontological restrictions and the good/bad asymmetry. Journal of Moral Philosophy. 2009;6((4)):464–481. [Google Scholar]
- American Academy of Pediatrics. American Academy of Pediatrics Committee on Bioethics: Guidelines on foregoing life-sustaining medical treatment. Pediatrics. 1994;93((3)):532–536. [PubMed] [Google Scholar]
- American Academy of Pediatrics Committee on Fetus and Newborn. Noninitiation or withdrawal of intensive care for highrisk newborns. Pediatrics. 2007;119((2)):401–403. doi: 10.1542/peds.2006-3180. [DOI] [PubMed] [Google Scholar]
- Archard D. Wrongful life. Philosophy. 2004;79:403–420. doi: 10.1017/s0031819104000348. [DOI] [PubMed] [Google Scholar]
- Arneson R. J. What is wrongful discrimination? San Diego Law Review. 2006;43:775–807. [Google Scholar]
- Arras J. D. Toward an ethic of ambiguity. Hastings Center Report. 1984;14((2)):25–33. [PubMed] [Google Scholar]
- Barlow J. H., Ellard D. R. The psychosocial well-being of children with chronic disease, their parents and siblings: An overview of the research evidence base. Child: Care, Health and Development. 2006;32((1)):19–31. doi: 10.1111/j.1365-2214.2006.00591.x. [DOI] [PubMed] [Google Scholar]
- Beauchamp T. L., Childress J. F. Principles of biomedical ethics. Oxford:: Oxford University Press; 1999. [Google Scholar]
- Benatar D. Better never to have been: The harm of coming into existence. Oxford:: Clarendon; 2006. [Google Scholar]
- Boyle R., Salter R., Arnander M. W. Ethics of refusing parental requests to withhold or withdraw treatment from their premature baby. Journal of Medical Ethics. 2004;30((4)):402–405. doi: 10.1136/jme.2002.000745. discussion 406–409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- British Medical Association. Withholding and withdrawing lifeprolonging medical treatment: Guidance for decision making. Malden, MA:: Blackwell; 2007. [Google Scholar]
- Buchanan A., Brock D. W. Deciding for others. Milbank Quarterly. 1986;64((suppl. 2)):17–94. [PubMed] [Google Scholar]
- Buchanan A. E., Brock D. W., Daniels N., Wikler D., Sober E. From chance to choice: Genetics and justice. Cambridge:: Cambridge University Press; 2000. [Google Scholar]
- Clark P. Tube feedings and persistent vegetative state patients: Ordinary or extraordinary means? Christian Bioethics. 2006;12((1)):43–64. doi: 10.1080/13803600600629934. [DOI] [PubMed] [Google Scholar]
- Cogan W., Whardall D. A life worth living—Living in the community with a tracheostomy. 2008. CP Australia Available at: http://www.cpaustralia.com.au/news/whardallcogan.pdf (accessed September 4, 2009)
- Crisp R. Reasons and the good. New York:: Clarendon Press; 2006. [Google Scholar]
- Dare T. Parental rights and medical decisions. Paediatric Anaesthesia. 2009;19((10)):947–952. doi: 10.1111/j.1460-9592.2009.03094.x. [DOI] [PubMed] [Google Scholar]
- DeGrazia D. Value theory and the best interests standard. Bioethics. 1995;9((1)):50–61. doi: 10.1111/j.1467-8519.1995.tb00300.x. [DOI] [PubMed] [Google Scholar]
- DeGrazia D. Moral status as a matter of degree? Southern Journal of Philosophy. 2008;46((2)):181–198. [Google Scholar]
- Devictor D. J., Tissieres P., Gillis J., Truog R. Intercontinental differences in end-of-life attitudes in the pediatric intensive care unit: Results of a worldwide survey. Pediatric Critical Care Medicine. 2008;9((6)):560–566. doi: 10.1097/PCC.0b013e31818d3581. [DOI] [PubMed] [Google Scholar]
- Diekema D. S. Parental refusals of medical treatment: The harm principle as threshold for state intervention. Theoretical Medicine and Bioethics. 2004;25((4)):243–264. doi: 10.1007/s11017-004-3146-6. [DOI] [PubMed] [Google Scholar]
- Downie R. S., Randall F. Parenting and the best interests of minors. J Med Philos. 1997;22((3)):219–31. doi: 10.1093/jmp/22.3.219. [DOI] [PubMed] [Google Scholar]
- Doyal L., Durbin G. When life may become too precious: the severely damaged neonate. Seminars in Neonatology. 1998;3:275–284. [Google Scholar]
- Emanuel L. L., Barry M. J., Stoeckle J. D., Ettelson L. M., Emanuel E. J. Advance directives for medical care—A case for greater use. New England Journal of Medicine. 1991;324((13)):889–895. doi: 10.1056/NEJM199103283241305. [DOI] [PubMed] [Google Scholar]
- Engelhardt H. Medicine and the concept of a person. In: Beauchamp T. L., Perlin S., editors. Ethical issues in death and dying. Englewood Cliffs, NJ:: Prentice-Hall; 1978. pp. 271–284. [Google Scholar]
- Feinberg J. Wrongful life and the counterfactual element in harming. Social Philosophy and Policy. 1986;4((1)):145–178. doi: 10.1017/s0265052500000467. [DOI] [PubMed] [Google Scholar]
- Garrard E., Wilkinson S. Selecting disability and the welfare of the child. Monist. 2006;89((4)):482–504. [Google Scholar]
- General Medical Council. Withholding and withdrawing life-prolonging treatments: Good practice in decision-making. London: GMC; 2006. [Google Scholar]
- Glover J. Choosing children: Genes, disability, and design. Oxford:: Clarendon Press; 2006. [Google Scholar]
- Goering S. ‘You say you're happy, but…’: Contested quality of life judgments in bioethics and disability studies. Bioethical Inquiry. 2008;5((2–3)):125–135. [Google Scholar]
- Griffin J. Well-being: Its meaning, measurement and moral importance. Oxford:: Clarendon; 1986. [Google Scholar]
- Hardart G. E., Truog R. D. Attitudes and preferences of intensivists regarding the role of family interests in medical decision making for incompetent patients. Critical Care Medicine. 2003;31((7)):1895–1900. doi: 10.1097/01.ccm.0000084805.15352.01. [DOI] [PubMed] [Google Scholar]
- Harris J. The welfare of the child. Health Care Analysis: HCA: Journal of Health Philosophy and Policy. 2000;8((1)):27–34. doi: 10.1023/A:1009430326447. [DOI] [PubMed] [Google Scholar]
- Harris J. C. Intellectual disability: Understanding its development, causes, classification, evaluation, and treatment. Oxford:: Oxford University Press; 2006. [Google Scholar]
- Harrison H. The offer they can't refuse: parents and perinatal treatment decisions. Seminars in Fetal & Neonatal Medicine. 2008;13((5)):329–334. doi: 10.1016/j.siny.2008.03.004. [DOI] [PubMed] [Google Scholar]
- Himmelmann K., Beckung E., Hagberg G., Uvebrant P. Gross and fine motor function and accompanying impairments in cerebral palsy. Developmental Medicine & Child Neurology. 2006;48((6)):417–423. doi: 10.1017/S0012162206000922. [DOI] [PubMed] [Google Scholar]
- Hope R. A. Medical ethics: A very short introduction. Oxford:: Oxford University Press; 2004. [Google Scholar]
- Janvier A., Bauer K. L., Lantos J. D. Are newborns morally different from older children? Theoretical Medicine and Bioethics. 2007;28((5)):413–425. doi: 10.1007/s11017-007-9052-y. [DOI] [PubMed] [Google Scholar]
- Jonas M. The baby MB case: Medical decision making in the context of uncertain infant suffering. Journal of Medical Ethics. 2007;33((9)):541–544. doi: 10.1136/jme.2006.017335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahane G., Savulescu J. The welfarist account of disability. In: Cureton A., Brownlee K., editors. Disability and disadvantage. Oxford:: Oxford University Press; 2009. pp. 14–53. [Google Scholar]
- Kamm F. M. Intricate ethics: Rights, responsibilities, and permissible harm. Oxford:: Oxford University Press; 2007. [Google Scholar]
- Kavka G. S. The paradox of future individuals. Philosophy and Public Affairs. 1982;11((2)):93–112. [Google Scholar]
- King B., Hodapp R., Dykens E. Mental Retardation. In: Sadock B., Sadock V., editors. Kaplan & Sadock's comprehensive textbook of psychiatry. Philadelphia:: Lippincott, Williams and Wilkins; 2000. pp. 2587–2613. [Google Scholar]
- Kipnis K. Harm and uncertainty in newborn intensive care. Theoretical Medicine and Bioethics. 2007;28((5)):393–412. doi: 10.1007/s11017-007-9051-z. [DOI] [PubMed] [Google Scholar]
- Kohl M. Voluntary death and meaningless existence. In: Kohl M., editor. Infanticide and the value of life. New York:: Prometheus Books; 1978. p. 210. [Google Scholar]
- Kon A. A. We cannot accurately predict the extent of an infant's future suffering: The Groningen Protocol is too dangerous to support. American Journal of Bioethics. 2008;8((11)):27–29. doi: 10.1080/15265160802513150. [DOI] [PubMed] [Google Scholar]
- Kopelman L. M. The best interests standard for incompetent or incapacitated persons of all ages. Journal of Law, Medicine & Ethics. 2007;35((1)):187–196. doi: 10.1111/j.1748-720X.2007.00123.x. [DOI] [PubMed] [Google Scholar]
- Kraut R. What is good and why: The ethics of well-being. Cambridge, MA:: Harvard University Press; 2007. [Google Scholar]
- Lockhart T. Moral uncertainty and its consequences. New York:: Oxford University Press; 2000. [Google Scholar]
- Macks R. J., Reeve R. E. The adjustment of non-disabled siblings of children with autism. Journal of Autism and Developmental Disorders. 2007;37((6)):1060–1067. doi: 10.1007/s10803-006-0249-0. [DOI] [PubMed] [Google Scholar]
- Marquis D. Why abortion is immoral. Journal of Philosophy. 1989;86:183–202. [PubMed] [Google Scholar]
- McCormick R. A. To save or let die. The dilemma of modern medicine. Journal of the American Medical Association. 1974;229((2)):172–176. [PubMed] [Google Scholar]
- McHaffie H. E., Fowlie P. W. Life, death and decisions: Doctors and nurses reflect on neonatal practice. Hale:: Hochland and Hochland; 1996. [Google Scholar]
- McMahan J. Wrongful life: Paradoxes in the morality of causing people to exist. In: Coleman J., Morris C., editors. Rational commitment and social justice: Essays for Gregory Kavka. Cambridge:: Cambridge University Press; 1998. pp. 208–247. [Google Scholar]
- McMahan J. The ethics of killing: Problems at the margins of life. New York:: Oxford University Press; 2002. [Google Scholar]
- McMahan J. Asymmetries in the morality of causing people to exist. In: Roberts M., Wasserman D., editors. Harming future persons: Ethics, genetics and the nonidentity problem. New York:: Springer; 2009. pp. 49–70. [Google Scholar]
- McMahan J. Radical cognitive limitation. In: Brownlee K., Cureton A., editors. Disability and disadvantage. Oxford:: Oxford University Press; 2009. pp. 240–259. [Google Scholar]
- Miller v. HCA, Inc., 118 S.W. 3rd 758 (Tex., 2003)
- Murphy N. A., Christian B., Caplin D. A., Young P. C. The health of caregivers for children with disabilities: Caregiver perspectives. Child: Care, Health and Development. 2007;33((2)):180–187. doi: 10.1111/j.1365-2214.2006.00644.x. [DOI] [PubMed] [Google Scholar]
- Murphy P. Murphy on evidence. Oxford:: Oxford University Press; 2007. [Google Scholar]
- Nuffield Council on Bioethics. Critical care decisions in fetal and neonatal medicine: Ethical issues. London:: Nuffield Council on Bioethics; 2006. [Google Scholar]
- Nugent M., Snow K., Lowney M. My child, my gift: A positive response to serious prenatal diagnosis. New York:: New City Press; 2008. [Google Scholar]
- Orfali K. Parental role in medical decision-making: fact or fiction? A comparative study of ethical dilemmas in French and American neonatal intensive care units. Social Science & Medicine. 2004;58((10)):2009–2022. doi: 10.1016/S0277-9536(03)00406-4. [DOI] [PubMed] [Google Scholar]
- Palisano R., Rosenbaum P., Walter S., Russell D., Wood E., Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Developmental Medicine & Child Neurology. 1997;39((4)):214–223. doi: 10.1111/j.1469-8749.1997.tb07414.x. [DOI] [PubMed] [Google Scholar]
- Parfit D. Reasons and persons. Oxford:: Oxford University Press; 1984. [Google Scholar]
- Paris J.J. Manslaughter or a Legitimate Parental Decision? The Messenger Case. Journal of Perinatology. 1996;16:60–64. [PubMed] [Google Scholar]
- Paris J. J., Schreiber M. D., Moreland M. P. Parental refusal of medical treatment for a newborn. Theoretical Medicine and Bioethics. 2007;28((5)):427–441. doi: 10.1007/s11017-007-9046-9. [DOI] [PubMed] [Google Scholar]
- Pope John Paul II. Address of Pope John Paul II to the participants in the International Congress on “Life-sustaining treatments and vegetative state: scientific advances and ethical dilemmas,” Saturday, 20 March 2004. NeuroRehabilitation. 2004;19((4)):273–275. [PubMed] [Google Scholar]
- President's Commission. Deciding to forego life-sustaining treatment: A report on the ethical, medical and legal issues in treatment decisions. President's Commission for the Study of Ethical Problems in Medicine and Biomedical and Behavioral Research. Washington, DC:: The Commission; 1983. [PubMed] [Google Scholar]
- Raina P., O'Donnell M., Rosenbaum P., et al. The health and well-being of caregivers of children with cerebral palsy. Pediatrics. 2005;115((6)):e626–e636. doi: 10.1542/peds.2004-1689. [DOI] [PubMed] [Google Scholar]
- Re J (a minor) (wardship: medical treatment) [1991]. Fam 33.
- Reichman N. E., Corman H., Noonan K. Impact of child disability on the family. Maternal and Child Health Journal. 2008;12((6)):679–683. doi: 10.1007/s10995-007-0307-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rennie J., Leigh B. The legal framework for end-of-life decisions in the UK. Seminars in Fetal and Neonatal Medicine. 2008;13((5)):296–300. doi: 10.1016/j.siny.2008.03.007. [DOI] [PubMed] [Google Scholar]
- Rennie J. M., Hagmann C. F., Robertson N. J. Outcome after intrapartum hypoxic ischaemia at term. Seminars in Fetal & Neonatal Medicine. 2007;12((5)):398–407. doi: 10.1016/j.siny.2007.07.006. [DOI] [PubMed] [Google Scholar]
- Roy R., Aladangady N., Costeloe K., Larcher V. Decision making and modes of death in a tertiary neonatal unit. Archives of Disease in Childhood Fetal and Neonatal Edition. 2004;89((6)):F527–F530. doi: 10.1136/adc.2003.032912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayeed S. A. The marginally viable newborn: Legal challenges, conceptual inadequacies, and reasonableness. Journal of Law, Medicine & Ethics. 2006;34((3)):600–610. 481. doi: 10.1111/j.1748-720x.2006.00074.x. [DOI] [PubMed] [Google Scholar]
- Schoeman F. Parental discretion and children's rights: Background and implications for medical decision-making. Journal of Medicine and Philosophy. 1985;10((1)):45–61. doi: 10.1093/jmp/10.1.45. [DOI] [PubMed] [Google Scholar]
- Sheffield K. “Not compatible with life,” a diary of keeping Daniel. 2007. Available at: http://www.trisomyoz.bounce.com.au/#/danielsbook/4528173715 (accessed March 8, 2009)
- Shevell M. I., Majnemer A., Miller S. P. Neonatal neurologic prognostication: The asphyxiated term newborn. Pediatric Neurology. 1999;21((5)):776–784. doi: 10.1016/s0887-8994(99)00102-2. [DOI] [PubMed] [Google Scholar]
- Singh J., Lantos J., Meadow W. End-of-life after birth: Death and dying in a neonatal intensive care unit. Pediatrics. 2004;114((6)):1620–1626. doi: 10.1542/peds.2004-0447. [DOI] [PubMed] [Google Scholar]
- Steinbock B., McClamrock R. When is birth unfair to the child? Hastings Center Report. 1994;24((6)):15–21. [PubMed] [Google Scholar]
- Stiles J. Neural plasticity and cognitive development. Developmental Neuropsychology. 2000;18((2)):237–272. doi: 10.1207/S15326942DN1802_5. [DOI] [PubMed] [Google Scholar]
- Sumner L. W. Welfare, happiness, and ethics. Oxford:: Clarendon Press; 1996. [Google Scholar]
- Tibballs J. Legal basis for ethical withholding and withdrawing life-sustaining medical treatment from infants and children. Journal of Paediatrics and Child Health. 2007;43((4)):230–236. doi: 10.1111/j.1440-1754.2007.01028.x. [DOI] [PubMed] [Google Scholar]
- Tyson J. E., Younes N., Verter J., Wright L. L. Viability, morbidity, and resource use among newborns of 501- to 800-g birth weight. National Institute of Child Health and Human Development Neonatal Research Network. Journal of the American Medical Association. 1996;276((20)):1645–1651. [PubMed] [Google Scholar]
- Van Der Heide A., van der Maas P. J., van der Wal G., Kollée L. A., de Leeuw R., Holl R. A. The role of parents in end-of-life decisions in neonatology: physicians’ views and practices. Pediatrics. 1998;101((3 part 1)):413–418. doi: 10.1542/peds.101.3.413. [DOI] [PubMed] [Google Scholar]
- Verhagen A., Dorscheidt J., Engels B., Hubben J., Sauer P. End-of-life decisions in Dutch neonatal intensive care units. Archives of Pediatrics & Adolescent Medicine. 2009a;163((10)):895–901. doi: 10.1001/archpediatrics.2009.166. [DOI] [PubMed] [Google Scholar]
- Verhagen A. A., de Vos M., Dorscheidt J. H., Engels B., Hubben J. H., Sauer P.J. Conflicts about end-of-life decisions in NICUs in the Netherlands. Pediatrics. 2009b;124((1)):e112–e119. doi: 10.1542/peds.2008-1839. [DOI] [PubMed] [Google Scholar]
- Verhagen E., Sauer P. J. The Groningen protocol— euthanasia in severely ill newborns. New England Journal of Medicine. 2005;352((10)):959–962. doi: 10.1056/NEJMp058026. [DOI] [PubMed] [Google Scholar]
- Wake M., Salmon L., Reddihough D. Health status of Australian children with mild to severe cerebral palsy: Crosssectional survey using the Child Health Questionnaire. Developmental Medicine & Child Neurology. 2003;45((3)):194–199. doi: 10.1017/s0012162203000379. [DOI] [PubMed] [Google Scholar]
- Whitelaw A. Death as an option in neonatal intensive care. Lancet. 1986;2((8502)):328–331. doi: 10.1016/s0140-6736(86)90014-0. [DOI] [PubMed] [Google Scholar]
- Wilkinson D. Is it in the best interests of an intellectually disabled infant to die? Journal of Medical Ethics. 2006;32((8)):454–459. doi: 10.1136/jme.2005.013508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkinson D. Death in the Netherlands: Evidence and argument. Archives of Pediatrics & Adolescent Medicine. 2009;163((10)):958–959. doi: 10.1001/archpediatrics.2009.197. [DOI] [PubMed] [Google Scholar]
- Wilkinson D. Magnetic resonance imaging and withdrawal of life support from newborn infants with hypoxic-ischemic ecnephalopathy. Pediatrics. 2010a;126((2)):e451–e458. doi: 10.1542/peds.2009-3067. [DOI] [PubMed] [Google Scholar]
- Wilkinson D. We don't have a crystal ball’: Neonatologists views on prognosis and decision-making in newborn infants with birth asphyxia. Monash Bioethics Review. 2010b;29((1)):5.1–5.19. [PubMed] [Google Scholar]
- Wilkinson D. J., Fitzsimons J. J., Dargaville P. A., et al. Death in the neonatal intensive care unit: changing patterns of end of life care over two decades. Archives of Disease in Childhood Fetal and Neonatal Edition. 2006;91((4)):F268–F271. doi: 10.1136/adc.2005.074971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams P. D. Siblings and pediatric chronic illness: A review of the literature. International Journal of Nursing Studies. 1997;34((4)):312–323. doi: 10.1016/s0020-7489(97)00019-9. [DOI] [PubMed] [Google Scholar]
- Wyatt J. Quality of life. 2005. Available at: http://www.cmf.org.uk/literature/content.asp?context=article&id=1702 (accessed May 25, 2009)
- Wyn N. Blue sky July. Bridgend:: Seren; 2007. [Google Scholar]
- Yorgason B. One tattered angel: A touching true story of the power of love. Salt Lake City, UT:: Shadow Mountain; 2003. [Google Scholar]


