Abstract
BACKGROUND:
Patients with carpal tunnel syndrome (CTS) often complain of prominent pain in shoulder and arm, also there are patients that have pain in their shoulder and arm which is due to myofascial trigger point (MTP) located in their upper trapezius muscle. Despite the frequency of this observation, few studies have previously sought to establish possible relationship between the CTS and MTP in shoulder area.
METHODS:
Samples were 160 patients (221 hands) consist of 130 females and 30 males, with suspected diagnosis of CTS, from March 2008 to October 2008. In this study after performing electrodiagnosis searches, another evaluation was performed to find out if there was any sign of myofascial trigger point. The correlation between these two was sought.
RESULTS:
It was found that all of 36 hands with normal electrodiagnostic findings had myofascial trigger points in their upper trapezius muscle. Out of 185 hands, 130 hands (70%) with electrophysiological evidences of CTS showed myofascial trigger points in their trapezius muscles. Statistical analysis revealed significant (p < 0.001) reverse correlation between the severity of CTS and the presence of MTP.
CONCLUSIONS:
The findings of this study imply the significant correlation between occurrence of CTS and MTP. It is suggested that clinicians consider the probability of existence of MTP in patients referred for diagnosis of CTS.
Keywords: Carpal Tunnel Syndromes, Myofascial Trigger Point, Electrodiagnoses
Carpal tunnel syndrome (CTS), the most common focal peripheral neuropathy, results from compression of the median nerve at the wrist.1–7
Many patients referred to an electrodiagnostic laboratory for evaluation of possible CTS might have other complaints, most commonly musculoskeletal disorders.8–10
The spots are tender in palpation and can produce referred pain, and tenderness, motor dysfunction and autonomic phenomena.11–15
Active and latent are two subdivisions of MTP.16,17
Acute trauma or repetitive microtrauma may lead to the development of a MTP.12,18
Some studies have mentioned the abnormal electrodiagnosis findings and presence of MTP in different muscles.19–21
Other studies have reported the presence of active and latent MTP in trapezius muscles and the effect of injection in these points.22,23 This study was conducted to determine the proportions of negative and positive electrodiagnostic findings in patients referred to electrodiagnostic center for evaluation of clinically suspected CTS. Also it was meant to determine the incidence of MTP in CTS and any correlation between the severities of CTS based on clinical and electrophysiological criterion and presence of MTP.
Methods
After institutional approval and receiving patients’ written consent, 160 adult patients were selected for study. They referred to electrodiagnostic center for evaluation of possible CTS, from March 2008 to October 2008. These patients were referred from orthopedic surgeons, neurologist, neurosurgeons and rheumatologist. Patients’ signs and symptoms and occupation were collected from the referrals and from the patients’ reports at the time of study. Information about paresthesia and pain and presence of hypoesthesia in hands and shoulder were obtained during the examination. Those patients who had pain due to fibromyalgia, tendinitis around shoulder girdle, herniated disc as well as degenerative joint disease at cervical spine, rheumatoid arthritis or pancoast syndrome were excluded. The study was approved by Ethics Committee of Isfahan University of Medical Sciences.
Neurophysiological evaluations were performed by the same investigator using an Easoate Biomedics 4 channels electromyograph (Phaysis II Myoto, Italia 1997). NCS were done by surface electrodes and included (a) antidromic sensory studies (conduction velocity and amplitude) of median and ulnar nerve from wrist to respective fingers and (b) motor studies (distal latency, amplitude and conduction velocity) of median nerve from the wrist to abductor pollicis brevis muscles and of ulnar nerve from the wrist and the forearm to abductor digiti minimi muscle. All standard tests for CTS were performed according to American Association of Electrodiagnostic Medicine (AAEM) guidelines.24 To exclude proximal lesions of the median nerve, thoracic outlet syndrome, radiculopathy and polyneuropathy, nerve conduction studies of the ulnar and radial nerves and EMG of forearm and paraspinal muscles was also conducted.
All hands tested were divided into six classes of severity based on the neurophysiological abnormalities:
0- “Negative” (NEG): normal findings in all tests including comparison to the ulnar nerve and short segmental tests.
1- “Minimal CTS” (MIN): abnormalities only when compared to the ulnar nerve or tested by short segmental studies
2- “Mild CTS” (MILD): slowing of sensory conduction across digit-wrist segment but normal distal motor latency (DML)
3- “Moderate CTS” (MOD): slowing of sensory conduction across digit-wrist segment and increased DML.
4- “Severe CTS” (SEV): absence of median SNAPs and increased DML.
5- “Extremely severe CTS” (EXT): absence of thenar motor and sensory response.
All patients with CTS underwent clinical assessment for MTP.
Patients were examined for MTP by a blinded examiner just after NCS was done.
According to Simons et al,11 the diagnostic criteria for the presence of myofascial trigger point were as follow: taut band, tender nodule on the taut band with increased pain on pressure, pain recognition, referred pain, and local twitch.
Statistics
Statistical analysis included independent t test and non parametric test such as Chi Square, Mann-Whitney and ANOVA tests were used for non-normal distributed data. P value < 0.05 was considered to be significant.
Results
A total of 221 hands (122 right and 99 left hands) from 160 patients, 130 females and 30 males, with mean age of 46 ± 13 years old (Range: 16-75) were included in the study. Of 221 hands with clinical diagnosis of CTS, 36 hands (16.3%) had no electrophysiological abnormality exhibited MTP in their Trapezius muscles. Of the remaining 185 hands with electrophysiological evidences of CTS, 130 showed MTP (70%) and 55 (30%) did not have MTP. In general, as the severity of CTS increased, the incidence of MTP decreased. Of 156 hands with minimal to moderate CTS, 121 (77.6%) presented MTP whereas out of 29 (69%) with severe and extreme CTS, only 9 (31%) showed evidence of MTP. Spearman test revealed significant (p < 0.001) reverse correlation between the severity of CTS and the presence of MTP (Table 1) (Figure 1).
Table 1.
MTP in different CTS Severity classes
| CTS severity | Presence of MTP | |||||
|---|---|---|---|---|---|---|
| Severity | Frequency | Percent | No MTP | With MTP | ||
| 0 | Normal | 36 | 16.3% | 0 (0%) | 36 (21.7%) | |
| 1 | Minimum | 64 | 29.0% | 12 (21.8%) | 52 (31.3%) | |
| 2 | Mild | 50 | 22.6% | 7 (12.7%) | 43 (25.9%) | |
| 3 | Moderate | 42 | 19.0% | 16 (29.1%) | 26 (15.7%) | |
| 4 | Severe | 26 | 11.8% | 19 (34.5%) | 7 (4.2%) | |
| 5 | Extreme severe | 3 | 1.4% | 1 (1.2%) | 2 (1.8%) | |
| Total | 221 | 100% | 55 (100.0%) | 166 (100.0%) | ||
Figure 1.
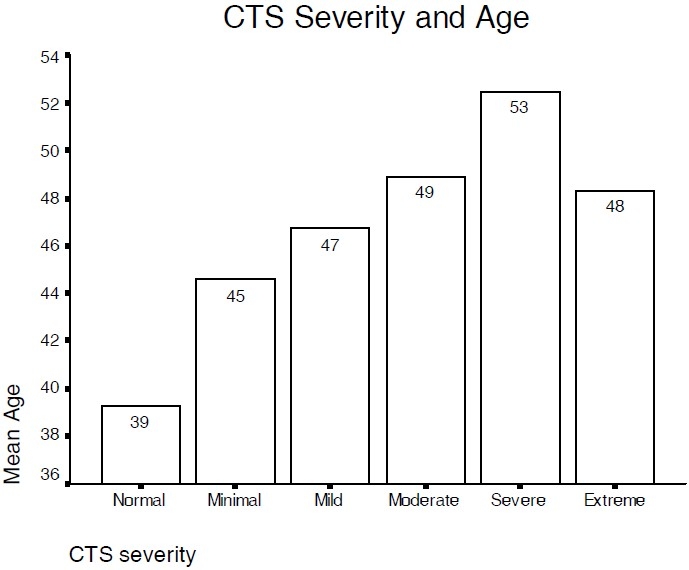
Mean ages in patients with different severity of CTS
Also a possible relationship between the severity of CTS and age was assessed. The mean age was significantly (p < 0.005) greater in more advanced CTS groups “Severe and Extremely severe” as compared to less advanced CTS cases (Moderate, Mild and Minimal groups)(Figure 2).
Figure 2.
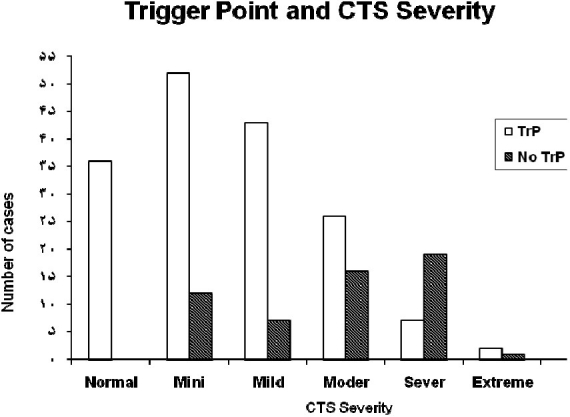
MTP in different severity of CTS are present
As the patients became older, the presence of MTP was less and conversely younger patients showed a higher prevalence of MTP (p < 0.001). There were 55 limbs (24.9%) without MTP, and 166 limbs (75.1%) with MTP in the area of the shoulder. From all upper limbs with MTP, 31 (22.8%) had active and 135 (77.2%) had latent MTP (Figure 3).
Figure 3.
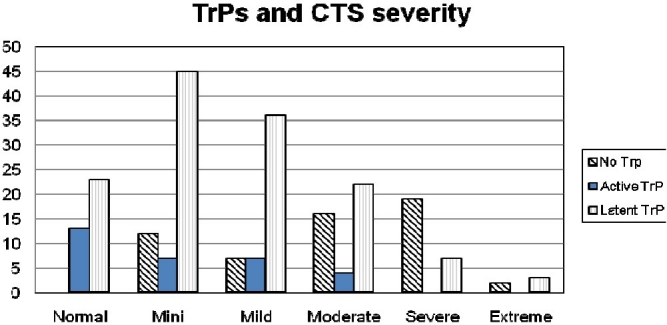
Number of patients who had MTP with different severity of CTS
Statistical analyses showed a reverse correlation between presence of MTP and patients’ ages. Presence of MTP was 50% in males and was %79.1 in females (Figure 4).
Figure 4.
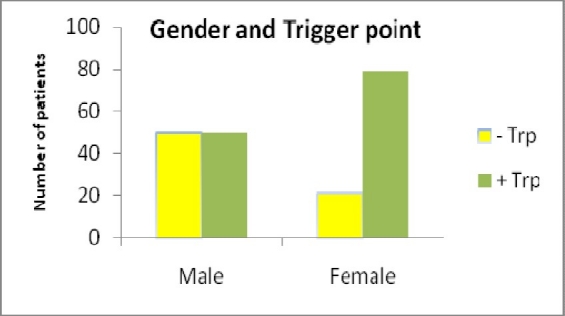
The incidence of MTP in both genders
Discussion
This single-blinded study searched the occurrence of myofascial trigger point in the upper trapezius muscle in a patients population (166 patients with 221 hand involved) referred for CTS. Thirty six hands (21.7%) showed normal electrophysiological findings but all had MTP in the upper trapezius muscle associated with paresthesia and pain referred to the arm and fingers. In these cases MTP possibly would explain their symptoms. This study is in line with Lo et al study20 as well as Qerama et al.21 The current study confirm the results of Padua et al study,25,26 who emphasized the importance of differentiating CTS from musculoskeletal disorders by performing a comprehensive musculoskeletal history and physical examinations. The results of the present study suggest that a patient with CTS may also have MTP as Qerama noticed it too.21 Also the present results are in favor of Davies findings19 but in this study the trapezius muscles showed the place where MTP are located and not scalenous or Infraspinatus muscles.21 All of the present patients with normal NCV (36 cases) showed MTP, which is twice the percentage that Qerama noted.21 They did not mention that they have included latent MTPs or just active ones. Infraspinatus muscle is a layer beneath the trapezius and latissimus dorsi muscles, so finding the exact location of MTP might be confusing which is in favor of literature review that Lucas et al performed.27 Presence of MTP in patients with different intensity of CTS was found here, which is not consistent with the results of Lo et al20 ; they postulated that patient who do not have CTS, might have musculoskeletal involvement, and they did not search the presence of MTP in their CTS subjects. MTPs in CTS patients should be considered as a secondary phenomenon and not a different pathology associated with it.
Conclusions
In conclusion, electrodiagnostic evaluations play an important role in the assessment of CTS. Patients with CTS undocumented by neurophysiologic studies are often prone to further diagnostic tests such as cervical spine CT and/or MRI. Before ordering the expensive studies, it is best to search for MTP, which may respond to appropriate therapy. Therefore, further studies are suggested to explore the possible relationship between CTS and MTP, reverse correlation between CTS severity and MTP and the affect of patients’ ages with these two disorders.
Acknowledgments
Author thank the support and fund provided by research affair of the faculty of Rehabilitation Sciences, Isfahan University of Medical Sciences, Iran, (Grant no. 286030) and Masoud Mazaheri, PhD, for manuscript revision and Akbar Hassanzadeh for statistical analysis.
Footnotes
Conflict of Interest:Authors have no conflict of interests
Authors’ Contributions
HA carried out the design and coordinated the study, participated in most of the experiments and prepared the manuscript. MD provided assistance in the design of the study, coordinated and referred patients for evaluation and participated in manuscript correction. AZ provided assistance for all manuscript preparation and referring patients. All authors have read and approved the content of the manuscript.
References
- 1.Turgut F, Cetinsahinahin M, Turgut M, Bolukbasi O. The management of carpal tunnel syndrome in pregnancy. J Clin Neurosci. 2001;8(4):332–4. doi: 10.1054/jocn.2000.0761. [DOI] [PubMed] [Google Scholar]
- 2.Sternbach G. The carpal tunnel syndrome. J Emerg Med. 1999;17(3):519–23. doi: 10.1016/s0736-4679(99)00030-x. [DOI] [PubMed] [Google Scholar]
- 3.Katz JN, Losina E, Amick BC 3rd, Fossel AH, Bessette L, Keller RB. Predictors of outcomes of carpal tunnel release. Arthritis Rheum. 2001;44(5):1184–93. doi: 10.1002/1529-0131(200105)44:5<1184::AID-ANR202>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- 4.Gerritsen AA, de Krom MC, Struijs MA, Scholten RJ, de Vet HC, Bouter LM. Conservative treatment options for carpal tunnel syndrome: a systematic review of randomised controlled trials. J Neurol. 2002;249(3):272–80. doi: 10.1007/s004150200004. [DOI] [PubMed] [Google Scholar]
- 5.Stevens JC, Witt JC, Smith BE, Weaver AL. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology. 2001;56(11):1568–70. doi: 10.1212/wnl.56.11.1568. [DOI] [PubMed] [Google Scholar]
- 6.Ingram-Rice B. Carpal tunnel syndrome: more than a wrist problem. J Bodyw Mov Ther. 1997;1(3):155–62. [Google Scholar]
- 7.Von Schroeder HP, Botte MJ. Carpal tunnel syndrome. Hand Clin. 1996;12(4):643–55. [PubMed] [Google Scholar]
- 8.Atroshi I, Gummesson C, Johnsson R, Ornstein E, Ranstam J, Rosen I. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282(2):153–8. doi: 10.1001/jama.282.2.153. [DOI] [PubMed] [Google Scholar]
- 9.Kummel BM, Zazanis GA. Shoulder pain as the presenting complaint in carpal tunnel syndrome. Clin Orthop Relat Res. 1973;(92):227–30. doi: 10.1097/00003086-197305000-00019. [DOI] [PubMed] [Google Scholar]
- 10.Kruse RA, Jr, Christiansen JA. Thermographic imaging of myofascial trigger points: a follow-up study. Arch Phys Med Rehabil. 1992;73(9):819–23. [PubMed] [Google Scholar]
- 11.Simons DG, Travel JG, Simons LS, Cummings BD. Myofascial pain and dysfunction: the trigger point manual. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 1998. [Google Scholar]
- 12.Han SC, Harrison P. Myofascial pain syndrome and trigger-point management. Reg Anesth. 1997;22(1):89–101. doi: 10.1016/s1098-7339(06)80062-3. [DOI] [PubMed] [Google Scholar]
- 13.Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. Am Fam Physician. 2002;65(4):653–60. [PubMed] [Google Scholar]
- 14.Brezinschek HP. Mechanisms of muscle pain: significance of trigger points and tender points. Z Rheumatol. 2008;67(8):653-4–656-7. doi: 10.1007/s00393-008-0353-y. [DOI] [PubMed] [Google Scholar]
- 15.Mense S, Schmit RF. Muscle pain: which receptors are responsible for the transmission of noxious stimuli? In: Rose FC, editor. Physiological aspects of clinical neurology. Oxford: Blackwell Scientific Publications; 1977. p. 265-78. [Google Scholar]
- 16.Ling FW, Slocumb JC. Use of trigger point injections in chronic pelvic pain. Obstet Gynecol Clin North Am. 1993;20(4):809–15. [PubMed] [Google Scholar]
- 17.Fricton JR, Kroening R, Haley D, Siegert R. Myofascial pain syndrome of the head and neck: a review of clinical characteristics of 164 patients. Oral Surg Oral Med Oral Pathol. 1985;60(6):615–23. doi: 10.1016/0030-4220(85)90364-0. [DOI] [PubMed] [Google Scholar]
- 18.Fischer AA. Injection techniques in the management of local pain. J Back Musculoskeletal Rehabil. 1996;7(2):107–17. doi: 10.3233/BMR-1996-7205. [DOI] [PubMed] [Google Scholar]
- 19.Davies C. Trigger point therapy for carpal tunnel syndrome: self-applied message of the forearms and scalenes. J Am Chiropr Assoc. 2002;39(8):18–23. [Google Scholar]
- 20.Lo JK, Finestone HM, Gilbert K, Woodbury MG. Community-based referrals for electrodiagnostic studies in patients with possible carpal tunnel syndrome: what is the diagnosis? Arch Phys Med Rehabil. 2002;83(5):598–603. doi: 10.1053/apmr.2002.32476. [DOI] [PubMed] [Google Scholar]
- 21.Qerama E, Kasch H, Fuglsang-Frederiksen A. Occurrence of myofascial pain in patients with possible carpal tunnel syndrome-a single-blinded study. Eur J Pain. 2009;13(6):588–91. doi: 10.1016/j.ejpain.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 22.Hong CZ, Hsueh TC. Difference in pain relief after trigger point injections in myofascial pain patients with and without fibromyalgia. Arch Phys Med Rehabil. 1996;77(11):1161–6. doi: 10.1016/s0003-9993(96)90141-0. [DOI] [PubMed] [Google Scholar]
- 23.Ge HY, Nie H, Madeleine P, Danneskiold-Samsøe B, Graven-Nielsen T, Arendt-Nielsen L. Contribution of the local and referred pain from active myofascial trigger points in fibromyalgia syndrome. Pain. 2009;147(1-3):233–40. doi: 10.1016/j.pain.2009.09.019. [DOI] [PubMed] [Google Scholar]
- 24.Jablecki CK, Andary MT, So YT, Wilkins DE, Williams FH. Literature review of the usefulness of nerve conduction studies and electromyography for the evaluation of patients with carpal tunnel syndrome. AAEM Quality Assurance Committee. Muscle Nerve. 1993;16(12):1392–414. doi: 10.1002/mus.880161220. [DOI] [PubMed] [Google Scholar]
- 25.Padua L, Lo Monaco M, Valente EM, Tonali PA. A useful electrophysiologic parameter for diagnosis of carpal tunnel syndrome. Muscle Nerve. 1996;19(1):48–53. doi: 10.1002/(SICI)1097-4598(199601)19:1<48::AID-MUS6>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 26.Padua L, Lo Monaco M, Gregori B, Valente EM, Padua R, Tonali P. Neurophysiological classification and sensitivity in 500 carpal tunnel syndrome hands. Acta Neurol Scand. 1997;96(4):211–7. doi: 10.1111/j.1600-0404.1997.tb00271.x. [DOI] [PubMed] [Google Scholar]
- 27.Lucas N, Macaskill P, Irwig L, Moran R, Bogduk N. Reliability of physical examination for diagnosis of myofascial trigger points: a systematic review of the literature. Clin J Pain. 2009;25(1)(1):80–9. doi: 10.1097/AJP.0b013e31817e13b6. [DOI] [PubMed] [Google Scholar]


