Abstract
Objective
The study tested whether adding up to 18 months of telephone continuing care, either as monitoring and feedback (TM) or longer contacts that included counseling (TMC), to intensive outpatient programs (IOP) improved outcomes for alcohol dependent patients.
Methods
Participants (N=252) who completed 3 weeks of IOP continued to receive IOP (M=36 sessions over 6 months) and were randomized to up to 36 sessions of TM (M=11.5 sessions of M=8.2 minutes), TMC (M=9.1 sessions of M=16.8 minutes), or IOP only (TAU). Quarterly assessment of alcohol use with the Time-Line Follow-Back (79.9% assessed at 18 months) was corroborated with available collateral reports (N=63 at 12 months). Participants with lifetime cocaine dependence (N=199) also provided urine samples.
Results
Main effects favored TMC over TAU on any alcohol use (OR=1.88, CI=1.13,3.14) and any heavy alcohol use (OR=1.74, CI=1.03,2.94). TMC produced significantly fewer days of alcohol use during months 10–18 and heavy alcohol use during months 13–18 than TAU (ds of .46 to .65). TM produced significantly better alcohol use outcomes than TAU only on percent days alcohol use, only during months 10–12 and 13–15 (ds of .41 and .39). TMC produced significantly fewer days of any alcohol use and heavy alcohol use than TM only during months 4–6 (ds= .39 and .43). Among participants with cocaine dependence, there were no treatment main effects on rates of cocaine positive urines.
Conclusion
Adding telephone continuing care to IOP significantly improved alcohol use outcomes relative to IOP alone. Conversely, shorter telephone calls that provided monitoring and feedback but no counseling generally did not improve outcomes over IOP.
Keywords: comparative effectiveness study, alcohol dependence, continuing care, telephone counseling, monitoring and feedback
There is now general acceptance among treatment providers that substance use disorders often have a chronic course, with afflicted individuals cycling through periods of abstinence, sporadic use, and heavy use (Hser, Longshore, & Anglin, 2007; McKay, 2009a; McLellan, Lewis, O’Brien, & Kleber, 2000). Consequently, there is considerable interest in developing new approaches to treatment that better address the cyclical and relapsing nature of these disorders (Dennis & Scott, 2007; Humphreys & Tucker, 2002; McKay, 2009a; Miller & Weisner, 2002). One such approach has been to extend the duration of treatment by adding lower intensity continuing care interventions to the back end of more intensive, stabilization-oriented treatments such as residential care and intensive outpatient treatment (Humphreys & Tucker, 2002; McKay, 2005). The main goals of these continuing care interventions are to provide ongoing support and counseling to help patients cope with stressors experienced after the initial phase of care has ended and to prevent any brief episodes of use (i.e., “slips”) from escalating into more serious relapses that could jeopardize remission status (Dennis & Scott, 2007; McKay, 2005).
Although there is mounting evidence of the effectiveness of continuing care interventions (Dennis & Scott, 2007; McKay, 2005, 2009a), low retention rates in outpatient treatment remains a significant issue. For example, only 36% of admissions for substance use disorders complete intensive or standard outpatient treatment, and median lengths of stay are under 90 days (SAMHSA, 2008). Patient dropout appears to be related to a number of issues, including reduced motivation for treatment, relapse, and competing work and family responsibilities (McKay, 2009a). Unfortunately, even patients who stop attending treatment because they are doing well and feel that they do not need it anymore are still at risk for relapse and will remain so for an extended period (Anglin, Hser, & Grella, 1997; Dennis & Scott, 2007; Hser et al., 2007; Moos, Finney, & Chronkite, 1990).
A recent review of the substance use disorder continuing care literature concluded that two features that were associated with effective interventions were a longer planned duration of care (i.e., at least 12 months) and more active efforts to deliver the intervention to the patient (McKay, 2009b). Some of the approaches taken included involving a spouse or partner (O’Farrell, Choqueette, & Cutter, 1998), visiting the home (Patterson, MacPherson, & Brady, 1997), using the telephone to deliver the intervention (Foote & Erfurt, 1992; McKay, Lynch, Shepard, & Pettinati, 2005), aggressively looking for patients and getting them back into treatment when necessary (Dennis, Scott, & Funk, 2003), and actively linking patients to continuing care services through case management and outreach (Coviello, Zanis, Wesnoski, & Alterman, 2006; Godley, Godley, Dennis, Funk, & Passetti, 2006).
In a prior study, we examined the effectiveness of a 12-week telephone-based continuing care intervention in 359 participants dependent on alcohol and/or cocaine who had completed 4-week intensive outpatient programs (IOPs) (McKay et al., 2004, 2005). In this protocol, participants received one 15–30 minute call per week, and were also provided with a weekly transition support group for the first four weeks. The content of the telephone calls consisted of several cognitive-behavioral therapy (CBT) components, including monitoring of substance use status and progress toward selected goals, identification of current and anticipated high-risk situations, and development and rehearsal of improved coping behaviors.
The telephone intervention was compared to continuing care “treatment as usual” (TAU) in these settings (two group counseling sessions per week for 12 weeks) and to a CBT relapse prevention intervention (one individual and one group session per week for 12 weeks). Self-report and biological (e.g., cocaine urine toxicology and liver function tests) data gathered over a 24 month follow-up indicated that the telephone intervention produced better substance use outcomes than TAU, as indicated by higher rates of self-reported abstinence in the full sample (McKay et al., 2005), and fewer heavy drinking days and lower GGT liver enzyme values in the alcohol dependent participants (McKay et al., 2004, 2005). Among the cocaine dependent participants, the telephone intervention also yielded lower rates of cocaine positive urine samples than CBT/RP (McKay et al., 2005). The positive effect of the telephone intervention, relative to standard care, was mediated by its effect on self-help attendance, self-efficacy, and commitment to abstinence (Mensinger, Lynch, TenHave, & McKay, 2007).
The current comparative effectiveness study evaluated a new version of the telephone continuing care protocol, which was modified in several ways to better address the chronic nature of alcohol use disorders and to be more compatible with publicly funded outpatient treatment. First, the protocol was lengthened to 18 months, to provide extended therapeutic contact for patients in community-based specialty care, many of whom continue to live in environments that are not supportive of recovery. The calls were initially placed at one week intervals, with the frequency reduced to bi-weekly calls after 8 weeks, and then to monthly calls after 12 months. Second, each call began with a brief structured assessment of current risk and protective factors, which was used to determine the focus of the remainder of the session. This modification was added to facilitate tracking of risk and protective factors over time and to make sure that the content of the sessions addressed the patient’s most pressing current issues. As in the first version of the protocol, the intervention included CBT techniques such as identification of high risk situations and rehearsal of improved coping behaviors.
Finally, many publicly funded programs in the Philadelphia area and elsewhere now have IOPs that provide up to 4 months of treatment, although some patients stop attending well before that point (SAMHSA, 2008). Providing continuing care only to those patients who complete these longer programs would sharply reduce the percentage of patients who would be eligible to receive that phase of care. Therefore, our modified protocol enrolled participants after they had achieved initial stabilization in IOP, at about the 3 week point, to engage them before possible dropout from IOP. While participants continued to come to IOP, the protocol included strategies to support continued attendance at IOP.
Recent research has indicated that for patients with alcohol use disorders, there is therapeutic value in brief assessments (Clifford, Maisto, & Davis, 2007). Therefore, there is some question as to whether longer telephone contacts that included an actual counseling component would confer more benefit than shorter calls that consisted of a brief assessment of current symptom severity and functioning plus feedback only, with no counseling. To determine if this were the case, we included a second extended telephone contact condition in the study, which provided calls on the same schedule as the telephone counseling condition. This intervention was shorter (e.g., 5–10 minutes vs. 15–30 minutes), and did not include any of the counseling components of the full telephone intervention. Both telephone interventions were compared to treatment as usual, which consisted of up to 4 months of IOP and any step down standard outpatient care that the participants received. We predicted that (a) the continuing care interventions would produce better substance use outcomes than treatment as usual, and (b) the telephone intervention with counseling would be superior to the intervention with only monitoring and feedback. This article presents substance use outcomes during the period in which the two telephone continuing care interventions were provided (i.e., months 1–18).
Method
Participants
The participants were 252 adults enrolled in two publicly funded IOPs in Philadelphia who met criteria for current DSM-IV alcohol dependence at the time of entrance to treatment (i.e., IOP or any other intervention that immediately preceded it). The other criteria for eligibility were a willingness to participate in research and be randomly assigned to one of the three continuing care conditions; completion of three weeks of IOP; no psychiatric or medical condition that precluded outpatient treatment (i.e., severe dementia, current audio or visual hallucinations); between the ages of 18 and 65; no IV heroin use within the past 12 months; ability to read at approximately the 4th grade level; and at least a minimum degree of stability in living situation (e.g., not living on the street). To facilitate follow-up, participants had to be able to provide the names, addresses, and telephone numbers of at least three contacts. Participants who were currently taking medication for psychiatric conditions were also required to have a follow-up appointment with a provider of psychiatric services to ensure continuity of medication.
The participants averaged 43.0 (sd=7.4) years of age and 11.8 (sd= 1.8) years of education, and the majority of participants were male (64.3%), African American (88.9%), and not currently married (91.3%). The participants averaged 20.9 (sd=9.3) years of regular alcohol use, 11.2 (sd=8.3) years of regular cocaine use, 3.4 (sd= 3.7) prior treatments for alcohol problems, and 3.1 (sd=3.8) treatments for drug problems. All participants had a current alcohol dependence diagnosis, based on alcohol use and consequences in the 30 days prior to entering IOP (79.7%) or in the 30 days prior to any controlled environment they were in immediately prior to IOP (20.3%). Seventy-nine percent of the sample carried a lifetime diagnosis of cocaine dependence, and 49.2% met criteria for current cocaine dependence at entrance to treatment.
Intensive Outpatient Treatment
Participants in the study were patients at one of two publicly funded community IOPs. Treatment in both sites was focused on overcoming denial, fostering participation in self-help groups, and providing information about the process of addiction and cues to relapse (McKay et al., 1994). These programs provided approximately 9 hours of group-based treatment per week, and patients could typically attend for up to 3–4 months. Patients who successfully completed the IOP phase of care at these programs were typically offered 3–4 months standard outpatient treatment (i.e., one group counseling session per week) for a total of up to 6–8 months of treatment.
Continuing Care Treatment Conditions
Telephone monitoring (TM)
Participants in this condition had one initial face-to-face session with their counselor in the first week of the protocol (i.e., week 3–4 of IOP) to orient them to the protocol and go over the assessment of risks and protective factors that they would be completing at each call. The patient and counselor decided who would initiate the calls; this decision was made on the basis of which approach was likely to yield the highest contact rate, and was subject to review and change at later points. A toll free number was provided to the participants, to reduce financial barriers to call completion.
Following this session, participants received brief telephone calls for up to 18 months. These 5–10 minute calls were offered weekly for the first 8 weeks, every other week for the next 44 weeks, and once per month for the final 6 months. Therefore, the total number of possible scheduled calls in the protocol was 36. Each call consisted of a structured 10 item assessment of current substance use status, other risk factors (e.g., craving, low self-efficacy, depression), and protective factors (e.g., attendance at self-help meetings, participation in other pro-recovery social activities), which was referred to as a progress assessment. A scoring algorithm produced a single summary score, with three levels of risk (e.g., low, medium, high), which was provided to the participant. A score of high risk could be generated by scores on two single items (e.g., any substance use in the past week, very low confidence in being able to abstain from use in the coming week), or a combination of high scores on other risk factors and low scores on protective factors. A score of low risk required some participation in pro-recovery behaviors, in addition to low scores on the risk items.
In the TM condition, the calls did not include any formal counseling. However, when participants were relapsing or experiencing other crises, the counselors did make recommendations to re-enter treatment or go to other facilities for help as part of the feedback they provided. In a few cases, counselors also suggested that a patient call back prior to his or her next scheduled contact. However, in general no stepped care was offered in this condition.
Telephone monitoring and counseling (TMC)
Participants in this condition also had one initial face-to-face session with their counselor in the first week to orient them to the protocol. In addition to what was discussed in the TM orientation, participants in the TMC orientation also selected goals to address in the upcoming sessions. The call schedule was the same as in the TM condition, and participants also completed the progress assessment and were given their overall risk score at the beginning of each call. For participants at low risk, current goals and the specific objectives that needed to be accomplished to reach each goal were reviewed. Any problems identified in the risk assessment were also addressed. In addition, reinforcement of positive behaviors and further encouragement for involvement in pro-recovery activities were provided. For participants at moderate or high risk, greater attention was devoted to identifying and rehearsing better coping responses to existing or anticipated risky situations.
The TMC condition also included a stepped care component, which was triggered when participants were categorized at high risk. The algorithm consisted first of more frequent telephone calls, which were provided over several weeks. If level of risk did not drop, face-to-face MI-based evaluation sessions followed by CBT sessions were offered via face-to-face sessions at the clinic. Participants in both conditions were told that they should contact their telephone counselor between regularly scheduled sessions if they felt that they were suddenly at heightened risk for relapse, or had used drugs or alcohol.
Therapists
The two telephone continuing care interventions were provided by seven therapists (four women and three men), each of whom delivered both interventions. All therapists had prior experience with providing outpatient treatment for substance use disorders, ranging from 1 to 20 years. Five of the therapists had MA-level degrees in psychology or social work, one had a BA, and one had a Ph.D. in clinical psychology. None had provided telephone-based counseling prior to this study.
Adherence to treatment protocols
The TM and TMC continuing care sessions were audio-taped to facilitate supervision and monitor adherence to the protocol as described in the manuals. Supervision was provided weekly by the study clinical coordinator, and one group supervision session was also held per week in which therapeutic issues were discussed with the senior clinical research staff on the project. Any deviations from the treatment protocol that were identified by the clinical coordinator were immediately addressed in the weekly supervision meetings. Analyses of adherence to the treatment manuals are presented in the Results section.
Procedures
Recruitment
Potential participants were screened at some point during their first three weeks of treatment in the two IOPs by the study research technicians. Those who appeared eligible based on the screening were informed that they would be given a full screening if they completed three weeks of the IOP and wanted to participate in the research study. Completion of 3 weeks of IOP was not contingent on achieving confirmed or self-reported abstinence during that period. Informed consent procedures were completed for those who appeared eligible after completing three weeks of IOP. A final determination of eligibility for the study was made after the baseline assessments were completed. The size of the study sample was selected to provide power to find a moderate size effect in the main effect analyses. The study was conducted in compliance with the policies of the Institutional Review Board of the University of Pennsylvania. Participants were recruited between May 17, 2004 and August 7, 2007.
Representativeness of the study sample
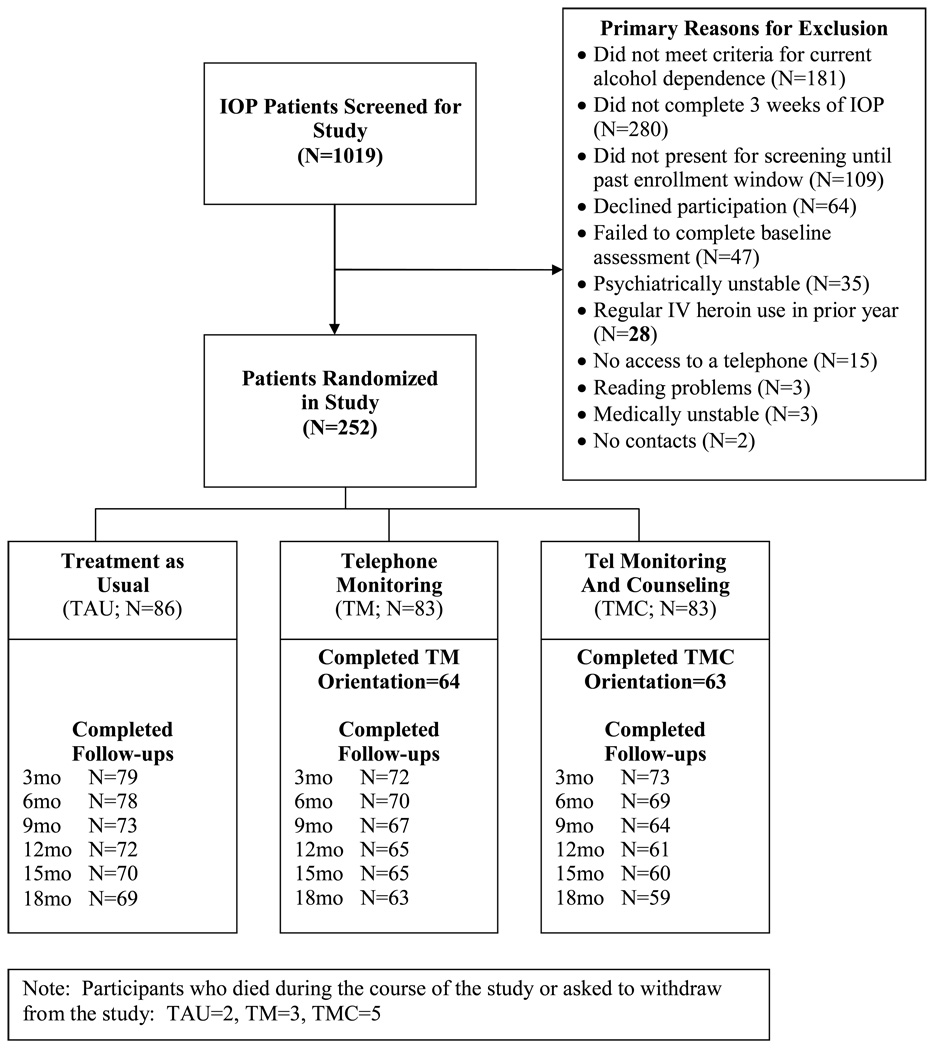
A total of 1019 patients were screened at the two IOPs, and of these, 252 were eligible and willing to participate and were enrolled in the study (see Figure 1). The reasons for failure to enter the study were as follows: did not have current alcohol dependence (N=181), stopped coming to IOP during the first three weeks of treatment (280), did not present for the screening until past the window for study enrollment (109), declined participation (64), did not complete the baseline assessment (47), was psychiatrically unstable (35), was a regular IV heroin use in the prior year (28), had no access to a telephone (15), low reading ability (3), medical problems (3), and no contacts (2).
Figure 1.
Consort Diagram
Randomization procedures
Separate randomized allocation schemes were used within each site. In each scheme, a blocked randomization scheme, using blocks of size 30, was used to yield a balanced allocation of participants to the three treatment groups. The study statistician, Kevin G. Lynch, generated the sequences. The assignments were placed in envelopes, and the sequence was concealed until the point of randomization. The project coordinators, Kathleen Ward and Donna Coviello, conveyed the results of the randomization to the participants.
Baseline and follow-up assessments
Baseline assessments were administered in 1 or 2 sessions that were started in weeks 3 or 4 of IOP. The follow-up assessments were conducted at 3, 6, 9, 12, 15, and 18 months post baseline. In most cases, these assessments were done in person, at the research offices. A minority of follow-ups were conducted at other sites (i.e., prison), or over the telephone. Participants received $50 for completing the baseline research sessions, and $35 per visit for completing each the six follow-up sessions. All study interviews were conducted by research personnel who had received extensive training in the use of the assessment instruments and were closely monitored during the course of the study. These interviewers were blind to the study hypotheses but not to treatment condition. The nature of material gathered at follow-up interviews, informal comments made by participants, and the length of the follow-up period precluded maintaining a cadre of interviewers who were unaware of treatment group assignment.
Follow-up rates
The follow-up rates for self-report data on alcohol use were as follows: 3 months, 89.6%; 6 months, 86.8%; 9 months, 81.9%; 12 months, 81.1%; 15 months, 80.6%; and 18 months, 78.9%. Follow-up rates for urine samples among participants with lifetime cocaine dependence were lower, ranging from a low of 60.2% at 9 months to a high of 69.8% at 18 months. The three treatment conditions did not differ significantly on follow-up rates at any point.
Measures
Psychiatric diagnoses
The Structured Clinical Interview for DSM-IV (SCID) (First et al., 1996) was administered at baseline to assess DSM-IV Axis I disorders. It was used to confirm alcohol dependence diagnosis and rule out any psychiatric disorders that would preclude study participation. In the most rigorous evaluation to date of the reliability of the SCID, which was done with the DSM-III-R version of the instrument, kappas of .61 for current diagnoses and .68 for lifetime diagnoses were obtained when participants were interviewed on two separate occasions by different interviewers (Williams et al., 1992).
Problem severity
The Addiction Severity Index (ASI; McLellan, Luborsky, Woody, & O'Brien, 1980) was used to gather information on problem severity levels in seven areas of functioning: medical, employment, drug use, alcohol use, legal, family/social, and psychiatric. Composite scores provide an indication of overall problem severity in each area during the prior 30 days (range of 0.00 – 1.00, with higher scores indicating greater problem severity). The ASI has demonstrated adequate to good internal consistency, test-retest, and interrater reliabilities in different groups of substance abusers (McLellan et al., 1985).
Self-reported substance use
Time-line follow-back (TLFB) (Sobell, Maisto, Sobell, & Cooper, 1979) calendar assessment techniques were used to gather self-reports of alcohol use during the 6 months preceding entrance into continuing care and the 18 month follow-up period. Studies with alcoholics (Sobell, Sobell, Leo, & Cancilla, 1988) and drug users (Ehrman & Robbins, 1994) have consistently demonstrated test-retest reliability of .80 or greater. In validity studies, TLFB reports of percent days abstinent have generally correlated .80 or better with collateral reports (Maisto, Sobell, & Sobell, 1979; Stout, Beattie, Longabaugh, & Noel, 1989). Self-reports of alcohol use in the context of a research study generally have been found to have high validity (Babor, Steinberg, Anton, & Del Boca, 2000).
The primary self-report outcome measures that were derived from the time-line data were percent days of alcohol use, percent days heavy alcohol use (i.e., 5 or more drinks/day for men, 4 or more drinks/day for women), and dichotomous measures of any alcohol use vs. no use and any heavy use vs. no heavy use. All measures derived from the TLFB were computed for each 3-month segment of the follow-up. For the “percent days” measures, the scores represented the percentage of days not in a controlled environment on which the participant used alcohol. Prior to analysis, a log transformation was used with these variables to reduce skewness.
The two abstinence-oriented measures (e.g., % days of alcohol use, any alcohol use) were selected because all participants were recruited from IOPs which stressed the importance of total abstinence. The two measures of heavy alcohol use (e.g., % days heavy alcohol use, any heavy alcohol use) were included because of the public health implications of heavy drinking. Both continuous and dichotomous versions of these measures were included to capture reductions in the frequency of drinking in addition to the achievement of abstinence or elimination of heavy drinking. The continuous measures were also important because despite the IOP’s stated goal of complete abstinence, some participants wanted to reduce the frequency of alcohol use rather than stop altogether. All four of these measures are widely used in alcohol treatment research, which facilitates comparisons with other studies.
Collateral reports
We attempted to obtain collateral reports on the participants’ alcohol and drug use at the 12 month follow-up. Collaterals were defined as an individual who knew the participant and would have regular enough contact to provide a reasonably accurate report of the participant’s drinking and drug use behavior. Of the 198 participants who provided data at the 12 month follow-up, collateral reports were available in 63 cases (32%). The low rate of collateral information collection was due to the social instability of our participants and difficulty in identifying individuals able and willing to serve as collaterals.
In these 63 cases, 68.3% of the participants and 50.8% of their collaterals reported at least some alcohol or drug use by the participant over months 1–12 [2 collaterals (3.2%) reported that they were unsure about whether any use had occurred]. In the 61 cases where collaterals provided data on use or abstinence, participants and collaterals agreed on use/no use in 50.8% of cases. In 32.8% of the cases, the participant reported alcohol or drug use and the collateral reported no use. In 16.4% of the reports, the patient reported abstinence but the collateral reported at least some alcohol or drug use. Because of the relatively low rate of apparent under-reporting by participants relative to collaterals, and the small percentage of participants for whom collateral data were available, participant self-reports were used in the analyses of alcohol use.
To determine how representative the 63 participants were of all 198 participants who provided 12 month data, we compared those with and without collaterals on 16 baseline and three outcome measures. The groups did not differ significantly on gender, age, psychiatric diagnoses, number of prior treatments for alcohol or drug use disorders, negative consequences from substance use, or on six of seven ASI baseline composite scores. Those without collaterals did have higher ASI medical composite scores (p= .04). With regard to alcohol use outcomes, those without collaterals reported higher percent days alcohol use in months 4–6 (p= .03), 7–9 (p= .04), and 10–12 (p= .05), and higher percent days heavy drinking at months 4–6 (p= .03) than those with collaterals. The groups did not differ at any follow-up on percentage with cocaine positive urines results. These results indicate that participants without collaterals generally did not differ from those with collaterals on baseline data and they also did not appear to underreport alcohol or drug use during follow-up relative to those with collaterals.
Cocaine Urine Toxicology
Urine samples were obtained at baseline and at each follow-up point to serve as the measure of cocaine use in analyses with participants who had lifetime cocaine dependence. The urine samples were tested for the cocaine metabolite benzoylecgonine using either the Emit assay system or FPIA analysis (with quantitative output converted to a dichotomous variable).
Continuing care participation
Attendance data were obtained directly from the study therapists, using a web-based form that included dates of scheduled telephone sessions, attendance status, and scores from each item in the progress assessment. The therapists also recorded information on the duration of the session and time spent in trying to contact the patient if the patient was not reached at the specified session time.
Participation in standard care and self-help programs
The TLFB was also used to gather data on days of outpatient substance abuse treatment received by participants in the study. As was the case with the TLFB alcohol use data, these services data were aggregated for each three month period of the follow-up. Degree of participation in self-help program activities in the 30 days prior to each assessment was also obtained (McKay et al., 1994).
Data Analyses
Differences between the three conditions at baseline were evaluated with one-way nonparametric ANOVAs (continuous measures) and chi-square tests (categorical measures). Treatment differences in number of days on which intensive outpatient treatment sessions were received were also evaluated with one-way ANOVAs.
Generalized estimating equations (GEE; SAS PROC GENMOD) were used to compare the continuing care groups on the continuous and binary TLFB and urine toxicology outcome measures. The TLFB data were collapsed into a pre-continuing care baseline period (6 months prior to baseline, including IOP) and six follow-up periods (months 1–3, 4–6, 7–9, 10–12, 13–15, and 16–18). A compound symmetry / exchangeable covariance structure was used for these models. Time was modeled as a categorical factor with six levels.
The primary analyses, conducted with the full sample (i.e., intent to treat), compared the three conditions on percent days of alcohol use, percent days of heavy alcohol use, percentage with any alcohol use, and percentage with any heavy alcohol use within each 3-month segment of the follow-up. Cocaine urine toxicology results at each assessment point were also examined with participants who had lifetime cocaine dependence (N=199). The independent variables that were included in these models were treatment condition, site, and time, and the baseline value of the outcome measure was included as a covariates. The analyses examined treatment condition main effects, and treatment condition × time interactions. Post hoc contrasts were used to probe significant treatment condition × time effects to determine the nature of the interactions.
Finally, pattern mixture analyses (Hedeker & Gibbons, 1997) were conducted to evaluate the potential effects of non-ignorably missing TLFB and urine toxicology data.
Results
Comparison of Treatment Conditions at Baseline
Participants in the three treatment conditions were compared on 21 demographic, diagnostic, treatment, and problem severity level variables assessed at baseline. These data are presented in Table 1. There were no significant differences between the treatment conditions. All p values were .14 or greater, except for gender (p= .10).
Table 1.
Characteristics of Sample at Baseline
| TAU | TM | TMC | F or | P | |
|---|---|---|---|---|---|
| N=86 | N=83 | N=83 | Chi-square | Value | |
| Demographics | |||||
| Race - % (N) | 2.18 | .34 | |||
| African American | 84.9 (73) | 90.4 (75) | 91.6 (76) | ||
| Other | 15.1 (13) | 9.6 (8) | 8.4 (7) | ||
| Marital Status - % married (N) | 8.1 (7) | 6.0 (5) | 12.1 (10) | 1.94 | .37 |
| Gender - % male (N) | 60.5 (52) | 59.0 (49) | 73.5 (61) | 4.61 | .10 |
| Age – mean (SD) | 42.75 (7.72) | 43.79 (7.35) | 42.36 (7.16) | 1.97 | .37 |
| Education – mean (SD) | 11.86 (1.85) | 11.55 (1.95) | 12.01 (1.52) | 2.85 | .24 |
| Substance Use – mean (SD) | |||||
| ASI alcohol composite | .30 (.20) | .30 (.20) | .26 (.18) | 1.98 | .37 |
| ASI drug composite | .09 (.08) | .11 (.09) | .09 (.08) | 2.25 | .32 |
| Alcohol – years regular use | 20.94 (9.48) | 21.73 (9.32) | 20.08 (8.98) | 1.65 | .49 |
| Cocaine – years regular use | 10.69 (8.08) | 11.19 (8.01) | 11.75 (8.88) | .72 | .70 |
| Prior treatments for alcohol abuse | 3.35 (3.94) | 3.29 (3.70) | 3.42 (3.47) | .52 | .77 |
| Prior treatments for drug abuse | 2.98 (3.87) | 3.14 (4.22) | 3.05 (3.22) | .87 | .65 |
| Other Axis I Diagnoses-- % yes (N) | |||||
| Cocaine dependence | |||||
| Current | 51.2 (44) | 44.6 (37) | 51.8 (43) | 1.07 | .59 |
| Lifetime | 76.7 (66) | 79.5 (66) | 80.7 (67) | .43 | .81 |
| Major Depression (Current) | 12.8 (11) | 15.7 (13) | 8.4 (7) | 2.04 | .36 |
| Co-occurring Problem – mean (SD) | |||||
| ASI medical composite | .44 (.36) | .37 (.36) | .40 (.36) | 1.75 | .42 |
| ASI employment composite | .84 (.20) | .86 (.20) | .80 (.24) | 2.12 | .35 |
| ASI legal composite | .09 (.15) | .05 (.11) | .07 (.13) | 3.97 | .14 |
| ASI family/social composite | .21 (.22) | .16 (.20) | .17 (.19) | 3.05 | .22 |
| ASI psychiatric composite | .27 (.23) | .25 (.24) | .24 (.24) | 1.35 | .51 |
Participation in Outpatient Treatment
Over the first six months of the follow-up, participants averaged 36 days on which they received IOP or OP treatment sessions (range 0 to 98, sd=22.58). There were no differences between the three treatment condition on days attended of IOP or OP [F(2,223)= .17, p= .84].
Participation in Continuing Care
Of the 83 participants randomized to TM, 64 (77.1%) completed the orientation session and were eligible to receive continuing care sessions in the protocol. In the TMC condition, 63 of 84 (75.9%) participants completed orientation. The total number of continuing care sessions received by participants who completed their orientation to the protocol was 11.5 (SD= 9.7) in TM and 9.1 (SD=9.6) in TMC. Although 86.7% of the sessions were completed in the first year of the protocol, 39% of TM and 37% of TMC participants had at least one session between months 12 and 18. The mean duration of sessions was 8.2 minutes (SD=4.4) in the TM condition and 16.8 minutes (SD=10.9) in the TMC condition.
Adherence to Treatment Manuals
All sessions were recorded and approximately 1 in 6 sessions (208 of 1307, or 16% of sessions) were rated for adherence to the manuals. Most ratings were performed by the clinical supervisor and therapists trained in the protocol who had not provided clinical services in the study. The rating scale included 4 items reflecting session components to be included in all calls regardless of treatment condition; 5 items reflecting session components to be included in all TMC calls; and 1 item reflecting adaptive care components to be included as needed in TMC calls.
Overall, the treatments were provided in a manner consistent with the protocol and distinct from each other (see Table 2). Each of the 4 components intended to be included in all calls was present in at least 88% of the sessions reviewed in each condition (e.g., greets client, progress assessment, feedback, schedules next session). Each of the six components intended to be included in TMC calls were much more likely to be included in TMC than in TM calls (e.g., review of progress, identify high risk situations, select topic, CBT work, set goal for week, recommended stepped care). The relatively low endorsement rate for the “select topic” item in the TMC condition was primarily due to the fact that in many calls, the most concerning issue was clear from the material presented by the patient and a formal process of selection was not necessary. The conditions did not differ on number of call attempts (p= .20) or the percentage of calls initiated by the therapists (p= .31).
Table 2.
Adherence to Clinical Protocols
| Treatment Component | TM | TMC |
|---|---|---|
| Greets and orients client | 97.9 | 100.0 |
| Risk Assessment | 100.0 | 97.7 |
| Feedback | 99.2 | 88.4 |
| Schedules Next Session | 98.3 | 96.4 |
| Review of Progress | 23.5 | 90.7 |
| ID High Risk Situations | 9.5 | 57.1 |
| Select Topic | 5.0 | 25.3 |
| RP/CBT Work | 18.8 | 73.8 |
| Set Goal for Week | 9.2 | 70.7 |
| Recommend Stepped Care | 1.7% | 16.5% |
Note: % in each condition with component rated as present;
16% of all recorded calls rated
Analyses of Substance Use Outcomes
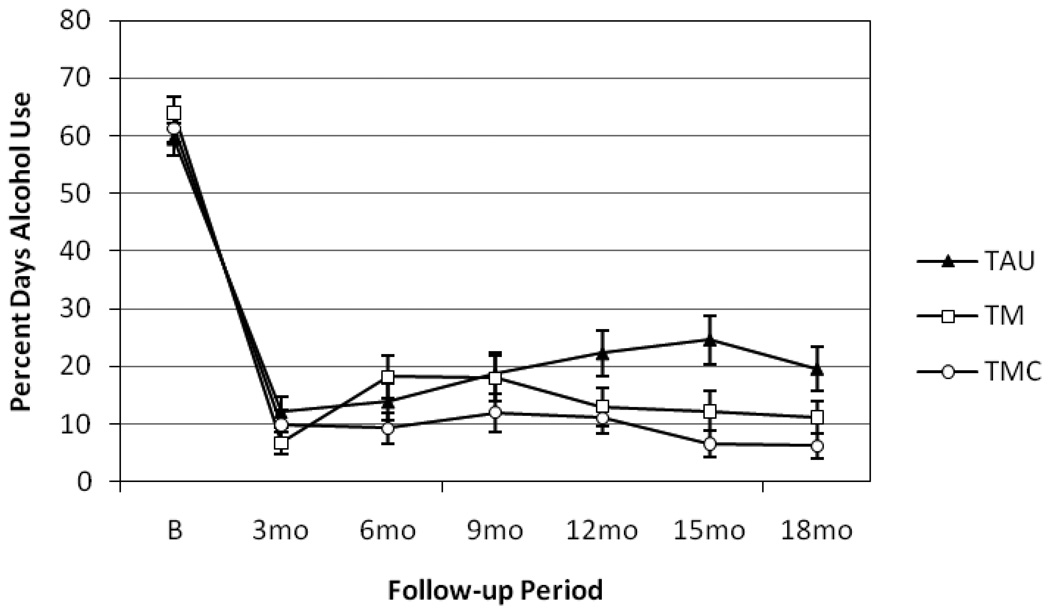
Percent days of alcohol use
Data on percent days of any alcohol use (untransformed) within each continuing care condition are presented in Figure 2. Drinking frequency remained the lowest in TMC over the 18-month follow-up. Conversely, drinking frequency steadily increased in TAU through month 15, with slight declines at month 18. In TM, drinking frequency increased during months 4–6, and decreased to some extent over the remainder of the follow-up. This pattern of results produced a significant treatment condition × time interaction [chi-square (10)= 20.45, p= .025]. Post hoc comparisons indicated that TMC produced fewer days of alcohol use than TAU during months 10–12 [chi-square (1)= 5.57, p= .018; d= 0.42], months 13–15 [chi-square (1)= 13.72, p= .0002; d= 0.65], and months 16–18 [chi-square (1)= 8.41, p< .004; d= 0.50]. In addition, TMC was superior to TM during months 4–6 [chi-square (1)= 5.37, p= .02; d= 0.39]. TM produced fewer days of alcohol use than TAU during months 10–12 [chi-square (1)= 5.39, p= .02; d= 0.41] and months 13–15 [chi-square (1)= 4.53, p= .03; d= 0.39].
Figure 2.
Frequency of Alcohol Use During Follow-up. Mean percent days alcohol use within each three-month period of the follow-up, presented for each treatment condition. Error bars indicate +/− 1 standard error (SE). There is a significant treatment condition × time interaction [chi-square (10)= 20.45, p= .025].
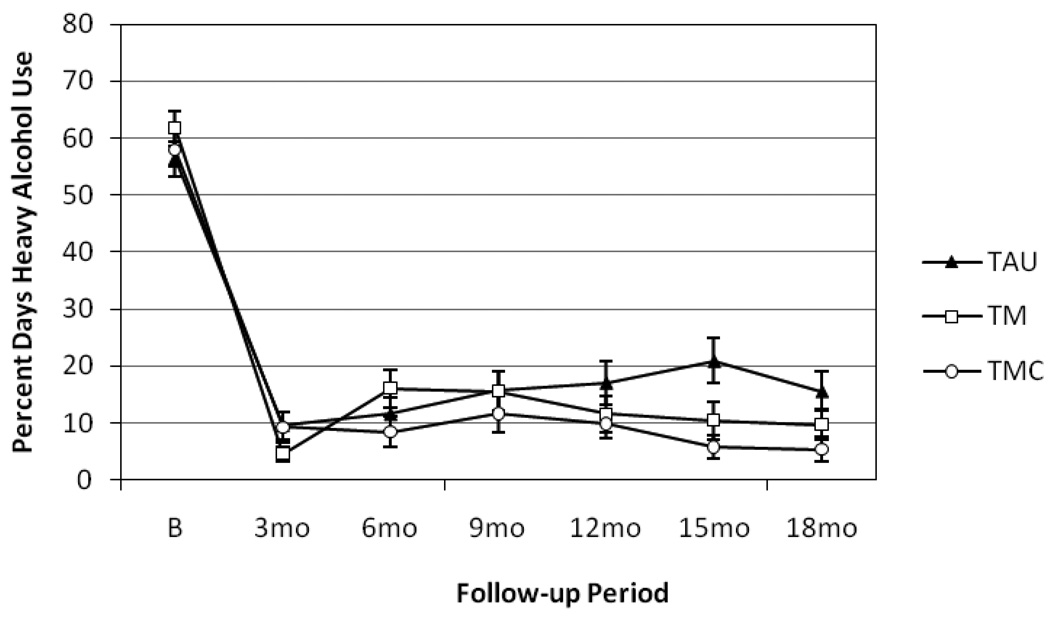
Percent days of heavy alcohol use
Similar findings were obtained with frequency of heavy drinking days (see Figure 3). Once again, a significant treatment condition × time interaction was obtained [chi-square (10) = 21.87, p= .016]. Post hoc comparisons indicated that TMC produced fewer days of heavy alcohol use than TAU during months 13–15 [chi-square (1)= 11.07, p= .0009; d= 0.59] and months 16–18 [chi-square (1)= 7.47, p= .006; d= 0.46], and fewer days of heavy alcohol use than TM during months 4–6 [chi-square (1)= 6.43, p= .01; d= 0.43]. TM and TAU did not differ significantly at any follow-up point.
Figure 3.
Frequency of Heavy Alcohol Use During Follow-up. Mean percent days heavy alcohol use within each three-month period of the follow-up, presented for each treatment condition. Error bars indicate +/− 1 standard error (SE). There is a significant treatment condition × time interaction [chi-square (10)= 21.87, p= .016].
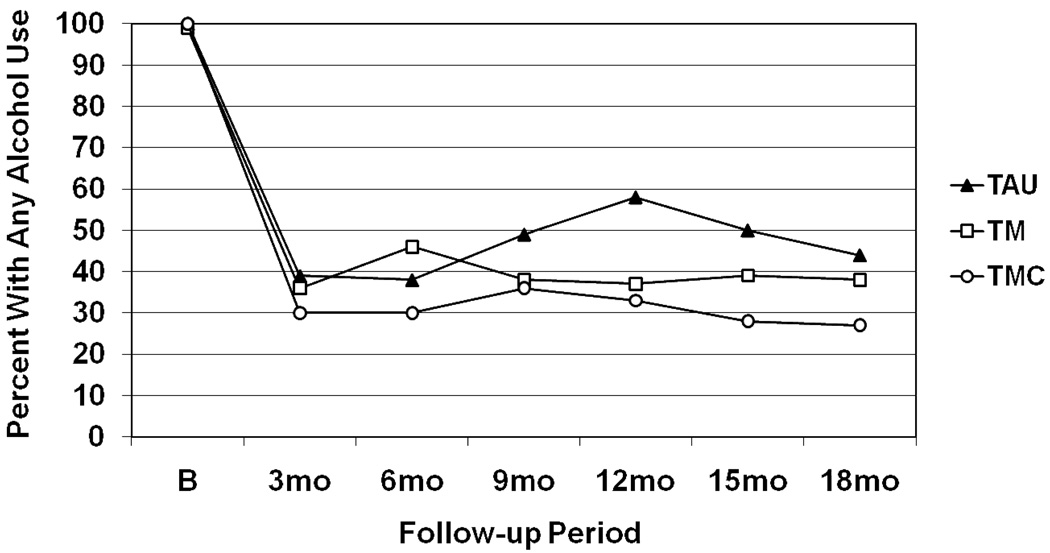
Any alcohol use
The percentage of participants in each treatment condition who reported any alcohol within each 3 months segment of the follow-up is presented in Figure 4. Rates of alcohol use were consistently the lowest in TMC, followed by TM and then TAU. This pattern of results produced a significant treatment condition main effect [chi-square (2)= 6.09, p= .048]. Main effect analyses of differences of least square means indicated TAU produced higher rates of any alcohol use than TMC [chi-square (1) = 5.85, p= .016; OR=1.88, CI=1.13,3.14]. Treatment as usual and TM did not differ [chi-square (1) = .65, p= .42; OR=1.24, CI:=0.73,2.10], nor did TM and TMC [chi-square (1)= 2.31, p= .13; OR=1.52, CI=0.89,2.59].
Figure 4.
Rates of Any Alcohol Use During Follow. Percentage of participants who report any use of alcohol within a given three-month period of the follow-up, presented for each treatment condition. There was a significant treatment condition main effect [chi-square (2)= 6.32, p= .048]. TMC produced lower rates of any alcohol use than TAU [chi-square (1) = 5.85, p= .016]. Comparisons of TM and TAU and TM and TMC were not significant.
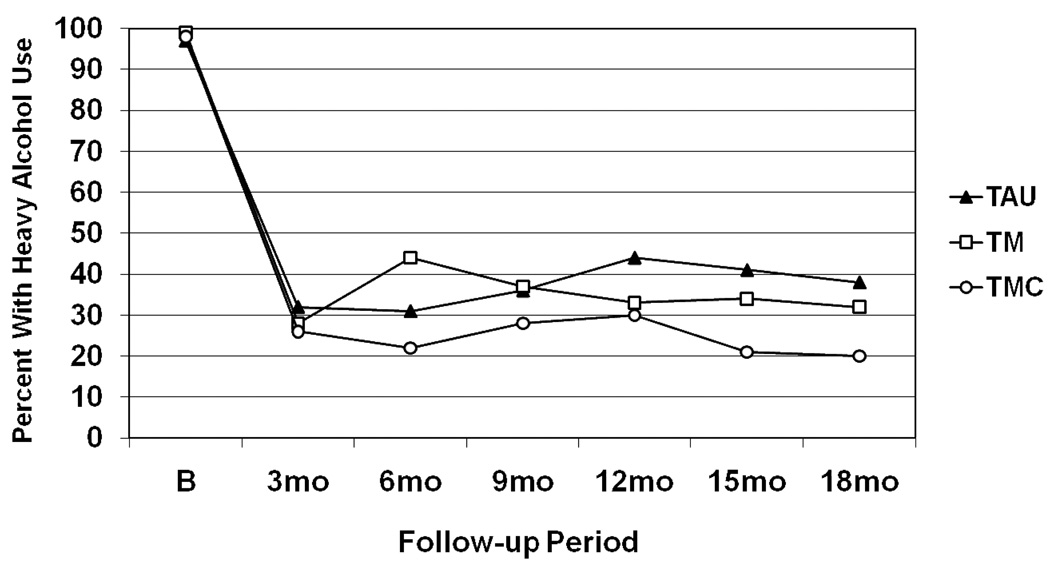
Any heavy alcohol use
Again, the best outcomes on this measure were in TMC, followed by TM and then TAU (see Figure 5). This pattern of results produced a trend toward a treatment condition main effect [chi-square (2)= 5.37, p= .068]. Analyses of differences of least square means indicated TAU produced higher rates of any heavy alcohol use than TMC [chi-square (1) = 4.29, p= .038; OR=1.74, CI=1.03,2.94]. There was also a trend favoring TMC over TM [chi-square (1) = 3.47, p= .063; OR=1.69, CI=0.97,2.92]. TAU and TM did not differ [chi-square (1)= .02, p= .90; OR= 1.03, CI=0.61,1.74].
Figure 5.
Rates of Any Heavy Alcohol Use During Follow. Percentage of participants who report any heavy alcohol use within a given three-month period of the follow-up, presented for each treatment condition. There was a trend toward a treatment condition main effect [chi-square (2)= 5.37, p= .068]. TMC produced lower rates of heavy alcohol use than TAU [chi-square (1) = 4.29, p= .038], and there was a trend favoring TMC over TM [chi-square (1)= 3.47, p= .063]. TM and TAU did not differ.
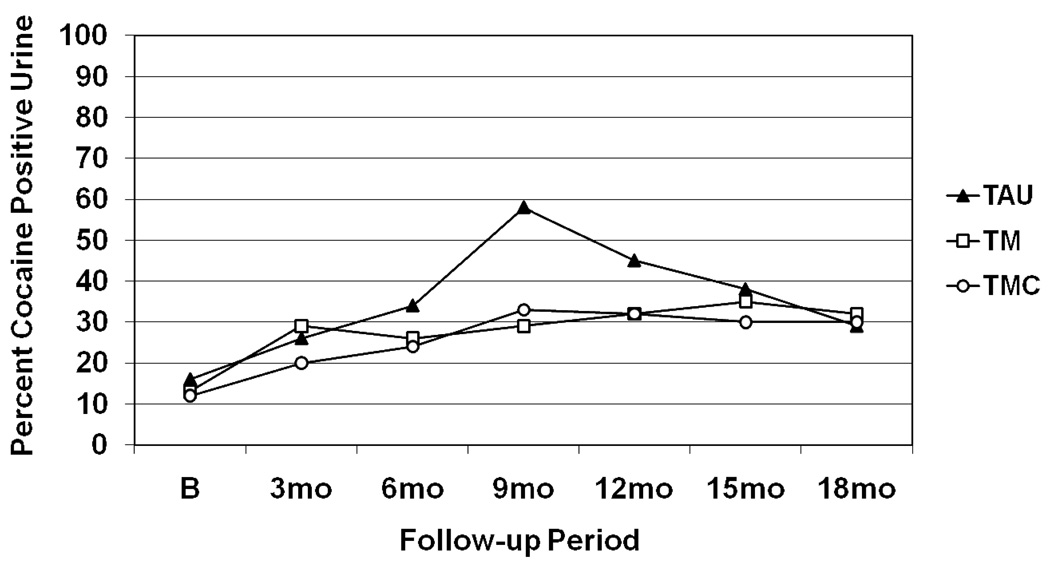
Cocaine use
All participants who met criteria for lifetime cocaine dependence (N=199) were asked to provide a urine sample at baseline and at each follow-up to test for recent cocaine use. Over the complete sample, rates of cocaine positive urines ranged from 13.7% at baseline to 40.0% at the 9 month follow-up. As can be seen in Figure 6, the TAU condition had a higher rate of cocaine positive urines in the middle of the follow-up (i.e., 6–15 months) than the two telephone conditions. However, when the combination of the TMC and TM conditions was compared to TAU, this difference was only significant at the 9 month follow-up [chi-square (1)= 4.94, p= .026; OR=2.58, CI=1.12,5.97], and the main effect analysis result did not approach significance [chi-square (1)= 1.27, p= .26; OR= 1.39, CI=0.79,2.47].
Figure 6.
Rates of Cocaine Positive Urine Samples. Percentage of participants with a cocaine positive urine sample at each follow-up for each treatment condition, in those with cocaine dependence (N=199). Follow-up rates ranged from 60.2% to 69.8% of those with cocaine dependence. Treatment condition main effects were not significant.
Effects of Missing Data
The three treatment conditions did not differ on pattern of missing data across the seven assessment points [chi-square (12)= 10.84, p= .54] or on time to dropout from research assessments [chi-square (2)= 1.61, p= .45]. The pattern mixture analyses did not find any significant interactions between research dropout status and any of the terms and interactions in the analyses. Therefore, missing data did not appear to be biasing the results.
Additional Treatment and Self-Help Participation during Follow-up
The three continuing care conditions did not differ on the amount of IOP or OP treatment received [chi-square (2)= 0.41, p= .81] or self-help group participation [chi-square (2)= 0.18, p= .91] over the 18 month follow-up.
Adverse Events
There were many hospitalizations among participants for medical and substance abuse-related problems during the course of the study, which was not unexpected given the characteristics of the participants. None of these serious adverse events were judged by the IRB to be related to study participation.
Discussion
This study evaluated the effectiveness of two telephone-based, extended continuing care interventions, which were compared to what has become standard care for substance dependent patients with at least moderate severity who seek publicly funded treatment—intensive outpatient programs, or IOPs. One continuing care intervention provided standardized monitoring of current symptoms and status, feedback, CBT-based counseling linked to the monitoring results, and stepped care as needed. The second intervention provided monitoring and feedback only. The participants all were alcohol dependent and had achieved initial engagement in IOP, as evidenced by regular attendance for three weeks. In this paper, we examined substance use outcomes over the 18 months in which the continuing care interventions were provided.
The results indicated that the telephone intervention that included counseling (i.e., TMC) yielded better outcomes than standard care on each of the four alcohol use measures examined. On the frequency of alcohol use and heavy alcohol use measures, these differences were largest over the last six months of the follow-up (i.e., months 13–18), with effect sizes ranging from .46 to .65. These effects translated into a difference between TMC and TAU of 14 percentage points on alcohol use and 11 percentage points on heavy alcohol use outcomes at 18 months, with slightly larger differences at 12 or 15 month follow-ups. On the categorical measures of alcohol use, rates of any alcohol use and any heavy alcohol use at 18 months were 17 and 18 percentage points higher, respectively, in TAU than in TMC, again with somewhat larger differences at 12 or 15 month follow-ups. These differences clearly exceed the effect sizes that have been found to be clinically meaningful to therapists (Miller & Manuel, 2008), although it should be acknowledged that these descriptive percentages are not standard effect size measures, which were presented earlier. There was considerably less evidence that the telephone intervention that consisted of monitoring and feedback only produced better outcomes than standard care. TM did not improve heavy alcohol use outcomes over what was obtained in TAU, and reductions in frequency of any alcohol use relative to TAU were observed at only two of six follow-ups.
Formal analyses of mediation effects have not been conducted, so any comments on potential mechanisms of action in TMC are necessarily speculative at this point. As noted earlier, mediation analyses in our prior study of telephone continuing care indicated that its effects were mediated by initial increases in self-help involvement, relative to standard care, followed by increases in self-efficacy and commitment to abstinence (Mensinger et al., 2007). These factors may have at least partially accounted for the positive effect of TMC observed here.
The TMC intervention evaluated in the present study differed in several ways from the earlier telephone intervention. Specifically, TMC included the progress assessment and feedback process, and the results of the assessment were used to structure the rest of the session. The process of assessing current status, providing feedback, and utilizing the data to focus the content of the session is used in a number of effective behavioral treatments for substance use disorders, including Motivational Enhancement Therapy (MET) (Miller, Zweben, DiClemente, & Rychtarik, 1995). In addition, the extended contact and support provided during the individual TMC sessions with counselors over as long as 18 months can be seen as examples of “general factors” that appear to account for much of the benefit of behavioral therapies (Morgenstern & McKay, 2007; Wampold, 2001).
The benefits of TMC appeared to be stronger between months 10 and 15 of the follow-up, with deterioration of effects over the final 3 months. It is possible that the smaller effects in the final 3 months were due to the fact that most participants in TMC were no longer receiving the intervention in the last six months of the follow-up. However, the data in Figure 2–Figure 5 suggest that the reduction in effects was due to improvements in the TAU condition, not to deterioration in TMC. The follow-up rate in TAU was not lower than that in the other two conditions, so the improvement in TAU is not an artifact created by differential study dropout. Rather, it could reflect the cycling between periods of relatively light use and heavy use observed in similar populations over periods of several years (Dennis & Scott, 2007) as well as regression to the mean.
The strong performance of TMC relative to standard care was particularly impressive given that participants in all three conditions averaged 36 IOP and OP treatment sessions over the first six months of the follow-up. This dose of treatment exceeds what most patients receive in publicly funded outpatient programs (SAMHSA, 2008). Alcohol use in participants who received standard care only began to increase after either the three or the six month follow-up, depending on the outcome measure, whereas good alcohol use outcomes were sustained for 18 months in participants who received the TMC intervention. This suggests that even patients who receive a considerable amount of more intensive treatment initially can benefit from an extended telephone-based continuing care intervention.
Although the results consistently indicated that TMC was superior to standard care whereas TM was generally not, there was little evidence that TMC produced significantly better outcomes than TM. TMC did produce fewer days of alcohol use and fewer days of heavy alcohol use than TM during months 4–6 of the follow-up, and there was also a main effect trend favoring TMC over TM on the categorical measure of any heavy drinking (p= .06, OR=1.69). However, other differences between TMC and TM were small and did not approach statistical significance. It is possible that larger sample sizes are needed to find further evidence of reliable differences between TMC and TM.
In contrast to what was observed with the alcohol use outcomes, the continuing care conditions did not produce better cocaine use outcomes than standard care, as indicated by urine test results. These results therefore do not replicate our prior study, in which telephone continuing care produced lower rates of cocaine positive urines during follow-up than standard care (McKay et al., 2005). The lack of better results with cocaine use may have been due to a number of factors, including the study’s focus on alcohol use and the limitations in the implementation of the telephone conditions, which are discussed below. In addition, the follow-up rates for the cocaine urine toxicology tests were lower than those for the self-report data, which may have affected the results of the analyses.
Study Limitations
The study had a number of strengths, including documented adherence to the treatment manuals and clear differences between the two continuing care interventions (Carroll et al., 2000), availability of some data to corroborate participant self-reports, six outcome assessments over an 18 month period, and a good follow-up rate. At the same time, the study had several limitations, which we discuss briefly here.
The two telephone continuing care interventions were designed to increase sustained treatment participation by providing a relatively low burden, “user friendly” approach to continuing care. Given these goals, the rates of continuing care participation we obtained in the study were somewhat disappointing. About 25% of the participants who were eligible for the interventions never initiated participation in them at any point in the 18 month window. In those who did initiate participation, the average number of sessions received was about 10 out of 36 possible. On the other hand, 38% of those who initiated participation in the protocol had at least one continuing care session in months 13–18. Therefore, significant numbers of participants continued active participation in the protocol into the second year, even if their contacts were at a lower frequency than was intended. It is notable that the TMC intervention achieved such good alcohol use outcomes relative to standard care, given the relatively small numbers of sessions delivered over the 18 month duration of the intervention.
Because the study was an evaluation of continuing care interventions, we only included those IOP participants who attended treatment regularly for three weeks. The study therefore followed a fairly traditional model of substance use disorder treatment in which continuing care is offered only to those patients who graduate from, or at least complete a significant part of, a more intensive, initial level of care. However, it actually might be more effective to enroll all patients who enter treatment into a continuing care protocol, because those individuals who drop out of treatment early may be the ones who are most in need of disease management. In this study, for example, about 27% of those screened dropped out of IOP prior to achieving the three week retention criterion for entrance into the study. It is possible that some of these early dropouts would have been open to receiving treatment via the telephone, and that the calls could have been used to provide support and encouragement for re-entry into clinic-based treatment.
Overall, only about 25% of participants screened for the study were ultimately enrolled in it. This raises questions about how representative the study sample was of typical patients in publicly funded IOPs. Unfortunately, data are not available to compare patients who were excluded from the study with those who were enrolled on factors other than those that were evaluated during the screening.
Another limitation was the lack of more complete data to corroborate the participants’ self-reports of alcohol use. Although the data that were available suggested that rates of patient underreporting of alcohol use were relatively low (around 16%), data from collaterals was available for only 32% of the participants who provided data at the 12 month follow-up. Given that participants with more intact social networks were more likely to have family members or friends who were able and willing to serve as collaterals, there were questions regarding to what extent the results of the analyses would generalize to the full sample. However, follow-up analyses indicted very little evidence of differences at baseline between participants with and without collaterals, and participants without collaterals did not report less drinking or have fewer cocaine positive urine samples during follow-up than those who did have a collateral. Moreover, a number of reviews have substantiated the validity of self-reports of alcohol use in treatment samples, particularly when the data are collected with calendar methods such as the TLFB in the context of research studies (Babor et al., 2000).
Final Conclusions
The addition of extended telephone-based continuing care produced significantly better alcohol use outcomes than standard care in alcohol dependent patients receiving treatment in publicly funded intensive outpatient programs. The intervention reduced both the incidence and frequency of any alcohol use and heavy alcohol use, relative to standard care, with clinically significant effects still present at 18 months. Conversely, shorter telephone calls that provided monitoring and feedback but no counseling conferred little benefit with regard to frequency of alcohol use and no benefit with regard to incidence or frequency of heavy alcohol use. Neither intervention significantly reduced cocaine use in patients with co-occurring cocaine dependence. Most patients who were offered the intervention initiated participation, and a significant percentage continued with the intervention for 12 months or more.
However, utilization of the interventions was less than optimal, as patients who initiated the protocol received less than a third of the available sessions. Although protocols have been developed that increase participation in continuing care (Lash et al., 2007; McKay, 2009a), more work in this area is clearly needed. In related research, we have found that providing similar patients with low level incentives for participation (e.g., $10 gift coupons for each call completed) increases the percentage of patients who initiate the continuing care intervention and greatly increases the percentage of possible calls completed (McKay, Ivey, Lynch, Van Horn, & Oslin, 2009).
It is also important to determine the costs and economic impact of the two telephone interventions. A key question is whether the improvements in alcohol use outcomes generate sufficient cost savings to pay for a significant portion of the added costs of the interventions. Future analyses will investigate the cost-effectiveness and cost-benefit of the two telephone interventions relative to standard care.
Acknowledgments
This research was supported by grants R01AA14850 and P01AA016821 from the National Institute on Alcohol Abuse and Alcoholism, and grant K02 DA000361 from the National Institute on Drug Abuse. Additional support was provided by the Medical Research Service of the Department of Veterans Affairs.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/ccp
References
- Anglin MD, Hser Y-I, Grella CE. Drug addiction and treatment careers among clients in the Drug Abuse Treatment Outcome Study (DATOS) Psychology of Addictive behavior. 1997;11:308–323. [Google Scholar]
- Babor TF, Steinberg K, Anton R, Del Boca F. Talk is cheap: Measuring drinking outcomes in clinical trials. Journal of Studies on Alcohol. 2000;61:55–63. doi: 10.15288/jsa.2000.61.55. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Nich C, Sifry RL, Nuro KF, Frankforter TL, Ball SA, Fenton L, Rounsaville BJ. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug and Alcohol Dependence. 2000;57:225–238. doi: 10.1016/s0376-8716(99)00049-6. [DOI] [PubMed] [Google Scholar]
- Clifford PR, Maisto SA, Davis CM. Alcohol treatment research assessment exposure reactivity effects: part 1. Alcohol use and related consequences. Journal of Studies on Alcohol and Drugs. 2007;68:519–528. doi: 10.15288/jsad.2007.68.519. [DOI] [PubMed] [Google Scholar]
- Coviello DM, Zanis DA, Wesnoski SA, Alterman AI. The effectiveness of outreach case management in re-enrolling discharged methadone patients. Drug and Alcohol Dependence. 2006;85:56–65. doi: 10.1016/j.drugalcdep.2006.03.009. [DOI] [PubMed] [Google Scholar]
- Dennis ML, Scott CK. Managing addiction as a chronic condition. Addiction Science and Clinical Practice. 2007 December;:45–55. doi: 10.1151/ascp074145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML, Scott CK, Funk R. An experimental evaluation of recovery management checkups (RMC) for people with chronic substance use disorders. Evaluation and Program Planning. 2003;26:339–352. doi: 10.1016/S0149-7189(03)00037-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehrman RN, Robbins SJ. Reliability and validity of six-month timeline reports of cocaine and heroin use in a methadone population. Journal of Consulting and Clinical Psychology. 1994;62:843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Biometrics Research Department. New York State Psychiatric Institute, NY: 1996. Structured Clinical Interview for DSM-IV Axis I Disorders—patient edition (SCID-I/P, version 2.0) [Google Scholar]
- Foote A, Erfurt JC. Effects of EAP follow-up on prevention of relapse among substance abuse clients. Journal of Studies on Alcohol. 1991;52:241–248. doi: 10.15288/jsa.1991.52.241. [DOI] [PubMed] [Google Scholar]
- Godley MD, Godley SH, Dennis ML, Funk RR, Passetti LL. The effect of assertive continuing care on continuing care linkage, adherence, and abstinence following residential treatment for adolescents with substance use disorders. Addiction. 2006;102:81–93. doi: 10.1111/j.1360-0443.2006.01648.x. [DOI] [PubMed] [Google Scholar]
- Hedeker D, Gibbons R. Applications of random-effects pattern-mixture models for missing data in longitudinal studies. Psychological Methods. 1997;2:64–78. [Google Scholar]
- Hser YI, Longshore D, Anglin MD. The life course perspective on drug use: a conceptual framework for understanding drug use trajectories. Evaluation Review: A journal of Applied Social Research. 2007;31:515–547. doi: 10.1177/0193841X07307316. [DOI] [PubMed] [Google Scholar]
- Humphreys K, Tucker JA. Toward more responsive and effective intervention systems for alcohol-related problems. Addiction. 2002;97:126–132. doi: 10.1046/j.1360-0443.2002.00004.x. [DOI] [PubMed] [Google Scholar]
- Lash SJ, Stephens RS, Burden JL, Grambow SC, DeMarce JM, Jones ME, et al. Contracting, prompting, and reinforcing substance use disorder continuing care: A randomized clinical trial. Psychology of Addictive Behaviors. 2007;21:387–397. doi: 10.1037/0893-164X.21.3.387. [DOI] [PubMed] [Google Scholar]
- Maisto SA, Sobell LC, Sobell MB. Comparison of alcoholics' self-reports of drinking behavior with reports of collateral informants. Journal of Consulting and Clinical Psychology. 1979;47:106–122. [PubMed] [Google Scholar]
- McKay JR. Is there a case for extended interventions for alcohol and drug use disorders? Addiction. 2005;100:1594–1610. doi: 10.1111/j.1360-0443.2005.01208.x. [DOI] [PubMed] [Google Scholar]
- McKay JR. Treating substance use disorders with adaptive continuing care. Washington DC: American Psychological Association; 2009a. [Google Scholar]
- McKay JR. Continuing care research: What we've learned and where we’re going. Journal of Substance Abuse Treatment. 2009b;36:131–145. doi: 10.1016/j.jsat.2008.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKay JR, Alterman AI, McLellan AT, Snider E. Treatment goals, continuity of care, and outcome in a day hospital substance abuse rehabilitation program. American Journal of Psychiatry. 1994;151:254–259. doi: 10.1176/ajp.151.2.254. [DOI] [PubMed] [Google Scholar]
- McKay JR, Ivey M, Lynch KG, Van Horn D, Oslin D. Effectiveness of extended telephone continuing care. San Francisco. Presented at the Addiction Health Services Research Conference.2009. Oct 29, [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Pettinati HM. The effectiveness of telephone based continuing care for alcohol and cocaine dependence: 24 month outcomes. Archives of General Psychiatry. 2005;62:199–207. doi: 10.1001/archpsyc.62.2.199. [DOI] [PubMed] [Google Scholar]
- McKay JR, Lynch KG, Shepard DS, Ratichek S, Morrison R, Koppenhaver J, Pettinati HM. The effectiveness of telephone-based continuing care in the clinical management of alcohol and cocaine use disorders: 12 month outcomes. Journal of Consulting and Clinical Psychology. 2004;72:967–979. doi: 10.1037/0022-006X.72.6.967. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Lewis DC, O’Brien CP, Kleber HD. Drug dependence, a chronic medical illness: Implications for treatment, insurance, and outcomes evaluation. Journal of the American Medical Association. 2000;284:1689–1695. doi: 10.1001/jama.284.13.1689. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola J, Griffith J, Evans F, Barr H, O’Brien CP. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous and Mental Disease. 1985;173:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Woody GE, O’Brien CP. An improved diagnostic evaluation instrument for substance abuse patients: The Addiction Severity Index. Journal of Nervous and Mental Disease. 1980;168:26–33. doi: 10.1097/00005053-198001000-00006. [DOI] [PubMed] [Google Scholar]
- Mensinger JL, Lynch KG, TenHave TR, McKay JR. Mediators of telephone-based continuing care for alcohol and cocaine dependence. Journal of Consulting and Clinical Psychology. 2007;75:775–784. doi: 10.1037/0022-006X.75.5.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller WR, Manuel JK. How large must a treatment effect be before it matters to practitioners?. An estimation method and demonstration. Drug and Alcohol Review. 2008;27:524–528. doi: 10.1080/09595230801956165. [DOI] [PubMed] [Google Scholar]
- Miller WR, Weisner C. Integrated care. In: Miller WR, Weisner CM, editors. Changing substance abuse through health and social systems. New York: Kluwer Academic/Plenum; 2002. pp. 243–253. [Google Scholar]
- Miller WR, Zweben A, DiClemente CC, Rychtarik RG. Motivational enhancement therapy manual. NIH Publication No. 94-3723. Rockville MD: U.S. Department of Health and Human Services, National Intitute on Alcohol Abuse and Alcoholism; 1995. [Google Scholar]
- Moos RH, Finney JW, Cronkite RC. Alcoholism treatment: Context, process, and outcome. New York: Oxford University Press; 1990. [Google Scholar]
- Morgenstern J, McKay JR. Rethinking the paradigms that inform behavioral treatment research for substance use disorders. Addiction. 2007;102:1377–1389. doi: 10.1111/j.1360-0443.2007.01882.x. [DOI] [PubMed] [Google Scholar]
- O’Farrell TJ, Choquette KA, Cutter HSG. Couples relapse prevention sessions after behavioral marital therapy for male alcoholics: Outcomes during the three years after starting treatment. Journal of Studies on Alcohol. 1998;59:357–370. doi: 10.15288/jsa.1998.59.357. [DOI] [PubMed] [Google Scholar]
- Patterson DG, MacPherson J, Brady NM. Community psychiatric nurse aftercare for alcoholics: A five-year follow-up study. Addiction. 1997;92:459–468. [PubMed] [Google Scholar]
- Scott CK, Dennis ML. Results from two randomized clinical trials evaluating the impact of quarterly recovery management checkups with adult chronic substance users. Addiction. 2009;104:959–971. doi: 10.1111/j.1360-0443.2009.02525.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sobell LC, Maisto SA, Sobell MB, Cooper AM. Reliability of alcohol abusers' self-reports of drinking behavior. Behavior Research and Therapy. 1979;17:157–160. doi: 10.1016/0005-7967(79)90025-1. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: Assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. British Journal of Addictions. 1988;83:393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- Stout RL, Beattie MC, Longabaugh R, Noel N. Factors affecting correspondence between patient and significant other reports of drinking [abstract] Alcoholism: Clinical and Experimental Research. 1989;12:336. [Google Scholar]
- Substance Abuse and Mental Health Services Administration, Office of Applied Studies. Treatment Episode Data Set (TEDS): 2005. Discharges from Substance Abuse Treatment Services. Rockville, MD: DASIS Series: S-41, DHHS Publication No. (SMA) 08-4314; 2008. [Google Scholar]
- Wampold B. The great psychotherapy debate: Models, methods, and findings. Madison: Lawrence Erlbaum Associates; 2001. [Google Scholar]
- Williams JB, First MB, Spitzer RL, Davis M, Borus J, Howes MJ, Kane J, Pope HG, Rounsaville B, Wittchen HU. The Structured Clinical Interview for DSM-III-R (SCID): II. Multisite test-retest reliability. Archives of General Psychiatry. 1992;49:630–636. doi: 10.1001/archpsyc.1992.01820080038006. [DOI] [PubMed] [Google Scholar]