Abstract
The Information-Motivation-Behavioral Skills (IMB) model of health behavior change informed the design of a brief, culturally-tailored diabetes self-care intervention for Puerto Ricans with Type 2 diabetes. Participants (n = 118) were recruited from an outpatient, primary care clinic at an urban hospital in the northeast U.S. ANCOVA models evaluated intervention effects on food label reading, diet adherence, physical activity, and glycemic control (HbA1c). At follow-up, the intervention group was reading food labels and adhering to diet recommendations significantly more than the control group. While the mean HbA1c values decreased in both groups (Intervention: 0.48% vs. Control: 0.27% absolute decrease), only the intervention group showed a significant improvement from baseline to follow-up (p < .008) corroborating improvements in self-care behaviors. Findings support the use of the IMB model to culturally tailor diabetes interventions and to enhance patients’ knowledge, motivation, and behavior skills needed for self-care.
Keywords: information motivation behavioral skills model, Puerto Rican, culture, tailored, diabetes self-care, behavior change
Few culturally appropriate diabetes education programs have focused on Puerto Rican Americans (Mauldon, Melkus, & Cagganello, 2006); a population with high rates of diabetes (Whitman, Silva, & Shah, 2006), diabetes-related complications (Lipton et al., 1996) and diabetes-related mortality (Smith & Barnett, 2005). To our knowledge, most culturally appropriate diabetes interventions to date have focused on African American (Anderson et al., 2005), Asian (Wang & Chan, 2005), and Mexican American populations (Brown, Garcia, Kouzekanani, & Hanis, 2002). These interventions have traditionally lacked a strong theoretical behavior change framework and have been more culturally targeted (population-focused) than tailored (personalized) (Sarkisian, Brown, Norris, Wintz, & Mangione, 2003). Tailoring messages, perhaps because they consist of personally relevant content, have been more effective in promoting behavior change than the generic “one size fits all” content that is sometimes delivered in the form of targeted, group-level curricula (Kreuter & Skinner, 2000). Culturally tailored diabetes interventions are needed that are both grounded in behavior change theory and focus on other high risk racial/ethnic minorities with diabetes (Sarkisian et al., 2003).
Theories of behavior change have been used to identify critical factors to target in health promotion interventions. An assumption of the Information-Motivation-Behavioral skills (IMB) model, which appears to have many of the “active ingredients” that have been found to be needed for health behavior change [see Social Cognitive Theory (Bandura, 1989), Theory of Planned Behavior (Ajzen, 1991), and Theory of Reasoned Action (Ajzen & Fishbein, 2005)], is that performing a health promotion behavior is a function of the extent to which someone is well informed about the behavior, motivated to perform the behavior (e.g., has positive personal beliefs and attitudes towards the behavior or outcome, and social support for the behavior), and has the requisite skills to execute the behavior and confidence in their ability to do so across various situations (J.D. Fisher & Fisher, 2000; W. A. Fisher, Fisher, & Harman, 2003; W. A. Fisher & Schachner, in press). Essentially, one who is well informed and motivated to act is thought to develop the skills necessary to enact the behavior at focus, and thus reap the health benefits of doing so (J.D. Fisher & Fisher, 2000; W. A. Fisher et al., 2003; W. A. Fisher & Schachner, in press). The model’s constructs and relationships among them have been well-supported across populations and health promotion behaviors (J.D. Fisher & Fisher, 2000; W. A. Fisher et al., 2003), including diabetes self-care behaviors (Osborn, 2006; Osborn & Egede, 2009).
The IMB model of health behavior change was selected because it provides a comprehensive, theory-based strategy for organizing the correlates identified in the current literature pertaining to the promotion of diabetes self-care behaviors in Puerto Rican Americans. Consistent with the IMB model, diabetes-related information is likely to be a necessary facilitator of performing self-care behaviors. Within the Puerto Rican population, language discrepancies between those delivering health information and those receiving it has contributed to information barriers and have been thought to promote misinformation about diabetes control (Adams, 2003). A lack of information has also been documented in other studies, including not knowing what foods are nutritionally appropriate or that carbohydrate counting is a critical component to a healthy diet, and exercise could improve one’s prognosis (Horowitz, Williams, & Bickell, 2003; von Goeler, Rosal, Ockene, Scavron, & De Torrijos, 2003). Studies have also noted the important role of motivation, as there may be negative health- and diabetes-related attitudes and skepticism regarding the value of self-care within this cultural group (von Goeler et al., 2003); and a lack of social support to engage in such activities (Coffman, 2008). Specific skills found to be important in diabetes management for Puerto Ricans include practical skills that are likely important across diverse cultural groups, such as controlling portion sizes, incorporating affordable foods into one’s diet, and doing physically safe exercises in unsafe neighborhoods (Punzalan et al., 2006), as well as culturally-specific behavioral skills, such as finding, obtaining, or preparing diabetes-appropriate foods that are culturally familiar (Horowitz et al., 2003).
An IMB model of Diabetes Self-Care (IMB-DSC) was articulated within a Puerto Rican population as the core content defining the main areas for barriers, and facilitators, of self-care behaviors. An intervention protocol was developed to address the core barriers and promote facilitators of self-care through an intervention that relied on motivational interviewing strategies to deliver diabetes-related information, motivation, and behavioral skills content (J.D. Fisher et al., 2004; Rollnick, Heather, & Bell, 1992). A randomized controlled trial evaluated the intervention’s effect on diabetes self-care behaviors and glycemic control. Specifically, it was predicted that the intervention group would experience better outcomes than the control group on measures of diet behavior (food label reading and diet adherence, specifically; hypothesis 1), physical activity (hypothesis 2), and glycemic control (hypothesis 3).
Method
Participants
Participants were recruited from an outpatient, primary care clinic at an urban hospital in the northeast U.S. Eligibility criteria included: self-identified Puerto Rican ethnicity, age 18 years or older, and a diabetes diagnosis of Type 2 (T2DM) for > 1 year. Clinic staff members identified and contacted eligible patients by phone. Of the 129 patients who were scheduled, 118 arrived at the clinic to participate in the study.
Procedures
Patients who consented to participate in the study completed a baseline assessment and were randomized to the intervention or usual care control group. Research assistants administered informed consent documents and self-report assessments, and were blind to the random allocation sequence. A qualified staff member tested each patient’s HbA1c level, and took weight and height measurements to calculate BMI. All participants received financially compensation for their time and travel to each visit (up to $65 for three visits: baseline, intervention, and follow-up).
The baseline and follow-up assessments took place separate from the intervention. Patients assigned to the intervention group completed the intervention within five days of the baseline assessment. Patients assigned to the control group maintained care as usual, which included a combination of medical treatment, physician monitoring, and an optional diabetes support group coupled with group-based didactic education delivered in Spanish. This diabetes support/education group was free, available on a month basis, and facilitated by a bilingual diabetes community health worker of Puerto Rican heritage. Group discussion focused on physical activity, meal planning strategies, adherence to medications, and blood glucose monitoring. The presentation of educational content was conducted in groups of 5–15 participants and was specifically not tailored to individual participant needs or organized on the basis of the IMB model. All patients returned three months later to complete the follow-up assessment.
Description of the intervention
The IMB model specifies a set of generalizable operations for constructing, implementing, and evaluating interventions to promote health behaviors (J.D. Fisher & Fisher, 2000; W. A. Fisher et al., 2003). The first step involves elicitation research, in which the target population’s information, motivation, and behavioral skills, behavior, and situational and personal factors (e.g., insurance status, mental health status, and literacy) are assessed to empirically identify deficits in critical determinants of behavioral performance. Based on elicitation research, the second step involves the design and refinement of a conceptually-based, empirically-targeted intervention to address patient deficits in adherence-related information, motivation, and behavioral skills. The third step involves intervention outcome evaluation research to determine if the intervention has been successful in affecting behavior, per se.
Consistent with the guidelines described above, the design of the current intervention began with elicitation work (e.g., focus groups, questionnaires) with patients and providers to identify critical barriers to performing self-care behaviors, as well as facilitators of behavior change. Findings established the core content targeted for improvement and support. As shown in our prior work (J.D. Fisher et al., 2004), collective input from health care providers, behavioral scientists, and patients help make interventions understandable, culturally appropriate, and clinically feasible.
The intervention was delivered by a bilingual medical assistant of Puerto Rican heritage who received approximately forty hours of training in diabetes self-management, motivational interviewing, safety, ethics, and intervention activities from a Registered Dietician/Certified Diabetes Educator (also of Puerto Rican heritage) and a health psychologist. Training focused on didactic session activities, reading materials, videos, role plays, and individual practice with feedback, and emphasized general skills in the use of simple, straight forward language and confirming understanding by asking patients to repeat instruction in their own words (known as the teach-back method) (Villaire & Mayer, 2007). Throughout the training, the interventionist was given feedback and suggestions for improvement to ensure desired effectiveness criteria were met.
The intervention session included all IMB elements interwoven into a seamless 90-minute session (see Table 1). All content was reviewed beforehand to avoid presenting unclear medical terms, and simplify language as necessary. A flipchart, available in English or Spanish (Puerto Rican dialect) presented intervention content and guided the session. Diet-relevant IMB elements preceded exercise-relevant IMB elements in the actual intervention. For ease of understanding, intervention content has been collapsed into information, motivation, and behavioral skills sections in the description presented below.
Table 1.
Content and Strategies for an IMB model-based Intervention
| INTERVENTION SESSION |
|---|
INFORMATION was provided with flip-chart support and interactive discussion pertaining to information pertinent to the targeted group of Puerto Rican. Topics included:
|
MOTIVATION was targeted throughout the session via MI-based strategies designed to enhance motivation (positive attitudes towards self-care, sense of social support for adopting self-care behaviors) including:
|
BEHAVIORAL SKILLS important in Puerto Rican populations with diabetes were specifically targeted through skills building and ‘teach-back’ strategies including how to
|
Introduction
The first five minutes of each session was dedicated to creating a climate of mutual respect, emotional affinity, comfort, openness and positive affirmation of the patient. This was achieved by welcoming the patient, communicating session goals such as the overall aim of the intervention, an overview of the session, respect for confidentiality, and getting acquainted with the patient.
Information
Following the introduction of the intervention session, data on the local prevalence of diabetes among Puerto Rican residents of Hartford, CT was presented. Given the tendency to minimize the seriousness of diabetes through self-protection, it was important to “localize” the diabetes prevalence to the target population. Communicating statistics in this way signaled a more inclusive discourse, allowing the interventionist and patient to engage in a discussion about the local impact of diabetes in the Puerto Rican community. Having set the tone for the discussion of diabetes, the next segment of the session focused on basic diabetes information, such as answering the questions, ‘What are diabetes-related complications?’, ‘What causes these complications?’, and ‘What causes high blood glucose?’ Given the pervasiveness of diabetes myths in the target community, it was also important to dispel common myths—e.g., the belief that only high sugar foods raise blood glucose levels.
To enhance information, patients were taught what types of culturally-familiar foods raise blood glucose levels and the importance of monitoring carbohydrate intake and controlling portion sizes throughout the day to control blood glucose levels. To enhance exercise information, patients were taught how inactivity increases one’s risk for complications; what the benefits are of exercising for people with diabetes; and how lifestyle activity (e.g., house or yard work, walking a pet, or walking around town to complete errands) can serve as an alternative to traditional, regimented exercise.
Motivation
The interventionist used motivational interviewing (MI) to deliver intervention content and enhance patients’ motivation to change. MI is a patient-centered counseling technique that enhances intrinsic motivation to change by exploring and resolving patients’ barriers and ambivalence to change (Rollnick et al., 1992). MI is also an operationally effective way to deliver IMB model-based content in clinical care settings, and ensure the structural uniformity of an intervention across patients (Cornman et al., 2008; J. D. Fisher et al., 2006). The specific MI techniques used during the session included (1) providing personal feedback, (2) asking open-ended questions, (3) reflective listening, (4) affirming existing desirable behaviors, and (5) working at each individual’s pace to maximize comprehension and retention of intervention content.
Following the principles of MI, the interventionist introduced the concept of personal risk for diabetes-related complications. A personal feedback report was created for each patient that contained critical data gathered at baseline (e.g., current diabetes self-care behaviors, diabetes-related symptoms, weight, and HbA1c level). The interventionist reviewed this report during the intervention, highlighting the patient’s risk factors for diabetes-related complications. This critical, personal feedback, delivered in the context of a supportive relationship and positioned in the context of strategies to support adherence to self-care recommendations, was intended to enhance the patient’s motivation to change.
Patients were also asked to rate their level of importance and confidence to perform diet and exercise behaviors on a scale from 1 = low to 10 = high. Low importance scores generally reflect deficits in critical information and/or motivation to change (J.D. Fisher et al., 2004; J. D. Fisher et al., 2006). Patients with low importance scores (< 5) were asked “what it would take” for them to raise their score by a few points. Responses were used to generate discussion on what types of information or motivational elements would facilitate change, while addressing ambivalence to change. Patients were also asked why their importance score was X (the score they reported) and not X-2, in order to generate self-motivating statements. Patient-specific needs, limitations, and barriers to change were considered throughout the intervention to increase interest and to keep the patient actively engaged, thus more motivated to change. A critical feature of this intervention was the development and distribution of culturally-tailored, individualized meal plan booklets. Dietetic internists used baseline height and weight data to calculate person-specific caloric needs, establish recommended food servings in a single day, and then distribute and document serving values across three meals in the meal plan booklet. During the intervention session, patients were instructed on how to select foods illustrated in the booklet that were consistent with the dietetic internist’s recommendations. The individualized, culturally-relevant meal plan was intended to promote positive attitudes about adhering to diet recommendations, and thus enhance patients’ personal motivation to change.
Behavioral skills
For the behavioral skills building component, patients also rated on a scale from 1 to 10 their confidence in performing the diabetes self-care behavior of interest. Low confidence scores generally reflect insufficient behavioral skills to perform the behavior. Those with low confidence scores (< 5) were asked “what it would take” to increase their score. Responses to this question were used to generate discussion on what types of behavioral skills elements would facilitate change, while addressing barriers to change. Patients were also asked why their confidence score was X (the score they reported) and not X-2. Responses to this question were believed to increase confidence in the ability to perform the behavior. Patient-specific importance and confidence scores were documented on the personal feedback report.
The interventionist then engaged patients in a functional analysis of their harmful, unhealthy behaviors. Patients discussed personal behaviors and cues related to triggering situations (e.g., stressful life events, cultural norms, family expectations, etc.) and were asked to think of ways to manage factors that may contribute to these triggers. There was also a focus on identifying barriers to reduce vulnerability in triggering situations, such as family expectations, and cultural barriers.
Patients were instructed on how to read food labels, monitor carbohydrates, eat small portions throughout the day, and integrate physical activity into daily life within the context of the individualized session. Training was provided on the three steps to reading carbohydrate information on food labels: look at the serving size; look at the total carbohydrate grams; and determine how much to eat. Patients performed these three steps with multiple food labels, including some that were culturally-specific, using a “teach back” technique to confirm understanding (i.e., patients role played and instructed the interventionist on how to perform the three steps). Patients were also trained on how to control carbohydrate portion sizes by using measuring cups; sectioning a plate (e.g., 1/2 of the plate filled with vegetables, 1/4 with protein and 1/4 with beans or rice); using their hand (e.g., 3 oz of meat = palm of hand, 1 cup of fruit = tight, clenched fist); or imagining familiar objects (e.g., 1 cup of rice or beans = tennis ball). Further, patients received training on how to increase activity by adding speed or additional movement to everyday behaviors. The performance of lifestyle activity (e.g., doing more housework or yard work at a faster pace, or walking instead of taking the bus or driving) appeared to require more simple behavioral skills than was needed to change diet behaviors. Because the intervention was designed to be brief, behavioral skills training for exercise was much less than that which was provided for diet.
To reinforce newly acquired skills, patients rehearsed them by role-playing a triggering situation from the past. The interventionist, playing the role of the patient’s closest source of support, perhaps, for these behaviors, in everyday life, aided them to enact new, healthy responses to previously triggering situations. Role-plays provided opportunities for hands-on practice and development, and the development of self-efficacy. The session concluded by asking the patient to formulate two realistic goals that were within the realm of intervention content, possible to reach, and thus linked to the primary outcomes.
Supplemental materials
Immediately following the intervention, patients were given a copy of their personal feedback report that contained: personal risk information; ratings of ‘importance’ and ‘confidence’ to perform diabetes self-care behaviors; a self-generated list of reasons to change and corresponding barriers to change; and two attainable behavior change goals that were within the realm of intervention content. Patients were also provided with 0–3 handouts depending on the extent of their personal relevance, which was determined by the interventionist: (1) saving money on meals, (2) ideas for eating breakfast, and/or (3) doing chair exercises for people with physical limitations. Handouts were available in English and Spanish (Puerto Rican dialect) and designed to enhance patients’ motivation and behavioral skills for purchasing healthy food, eating throughout the day, and doing affordable, physically safe activity in unsafe neighborhoods. To supplement the intervention’s diet content, all patients received a brochure of culturally familiar foods, arranged in different food groups, with recommended serving sizes; a set of measuring cups; and their individualized, culturally-tailored meal plan booklet. No further support was offered post intervention, although usual care for all patients remained in place.
Measures
Demographics
Demographic information pertained to gender, age, education, employment, English proficiency, language spoke most often at home, number of years in the U.S, insurance status, years diagnosed with diabetes, perceived health status, and body mass index (measures of height and weight were collected). Patients were also asked if they had ever participated in the optional diabetes support group available at the clinic. Response options were never, less than 3 months ago, 4–6 months ago, 7–9 months ago, 10–12 months ago, 1–2 years ago, and less than 2 years ago.
Food label reading
Reading carbohydrate content on food labels is critical to point-of-purchase decisions and making healthy food choices in persons with diabetes. Four items were created that asked, “In the last 30 days, how often did you: look at the serving size information on a food label, look at food labels to look at the total carbohydrate content, count carbohydrates, and select foods that are low in carbohydrates.” Response options were in Likert-type format, ranging from 1 = never to 5 = always. The mean score represented the frequency of food label reading behavior. High internal consistency was demonstrated at pre- and posttest (α = .92 –.94).
Diet adherence
The diet subscale of the Summary of Diabetes Self-Care Activities questionnaire (SDSCA) is a standardized measure of diabetes-relevant diet behavior (Toobert, Hampson, & Glasgow, 2000). Response options range from 0–7 to correspond to the number of days in a week. The mean score represents the frequency of adhering to diet recommendations in the past seven days.
Physical activity
The exercise subscale of the SDSCA is a standardized measure of physical activity in diabetes (Toobert et al., 2000). Response options range from 0–7 to correspond to the number of days in a week. The mean score represents the frequency of being physically active in the past seven days.
Glycemic control
HbA1c was measured with a National Glycohemoglobin Standardized Program (NGSP) certified, point-of-care immunoassay device (Kennedy & Herman, 2005).
Analyses
All analyses were performed using SPSS version 17.0. Pearson’s chi-square tests and Student’s t-tests assessed baseline group equivalence. Analysis of covariance (ANCOVA) models tested the intervention’s effect on post-intervention food label reading, diet adherence, physical activity, and glycemic control controlling for baseline values. First, univariate models examined the homogeneity of regression assumption on each dependent variable. When violated, the interactive model was retained. When satisfied, a full factor ANCOVA model evaluated the group differences on the follow-up score adjusting for the baseline score.
Results
There were 118 patients enrolled in the study. Adopting an ‘on protocol’ approach, patients who did not return at follow-up (n = 22), or complete the intervention (n = 5) were excluded from the analyses, resulting in a sample of participants who completed all phases of the research (n = 91). Loss of randomized participants from the analyzed data set was generally comparable across conditions (11 and 16 in treatment and control arm, respectively) and evaluation of pre-intervention group equivalence did not reveal differences in the measured variables (see Table 2).
Table 2.
Baseline Characteristics by Randomization Group of Completers
| Variable N = 91 |
Intervention n = 48 |
Control n = 43 |
p value |
|---|---|---|---|
| Age, years, M(SD) | 56.9 +/− 11.3 | 58.4 +/− 10.1 | .508 |
| Female, n(%) | 38 (79) | 30 (70) | .303 |
| Education, n(%) | |||
| ≤ 8th grade | 26 (54) | 28 (65) | .288 |
| 9th – HS degree or GED | 17 (36) | 11 (26) | .310 |
| ≥ HS degree or GED | 5 (10) | 4 (9) | .859 |
| Employment, n(%) | |||
| Employed | 2 (5) | 2 (5) | .910 |
| Unemployed | 17 (35) | 16 (37) | .859 |
| Disabled | 29 (60) | 25 (58) | .825 |
| English proficiency, 0 = poor to 5 = excellent | 1.8 +/− 1.7 | 1.5 +/− 1.4 | .294 |
| Speaks only Spanish at home, n(%) | 42 (81) | 37 (79) | .838 |
| Years in United States | 25.1 +/− 4.4 | 24.9 +/− 12.4 | .945 |
| Health insurance, n(%) | 42 (96) | 39 (91) | .471 |
| Years with diabetes | 13.2 +/− 12.0 | 12.3 +/− 9.4 | .693 |
| Have you ever participated in the diabetes support/education group? n(%) | |||
| Never | 13 (27) | 7 (16) | .214 |
| < 3 months ago | 12 (25) | 9 (21) | .645 |
| 4–6 months ago | 6 (13) | 9 (21) | .279 |
| 7–9 months ago | 3 (6) | 2 (5) | .738 |
| 10–12 months ago | 4 (8) | 3 (7) | .808 |
| 1–2 years ago | 7 (15) | 7 (16) | .823 |
| > 2 years ago | 3 (6) | 6 (14) | .219 |
| Perceived health status, 0 = poor to 5 = excellent | 2.2 +/− 1.5 | 2.7 +/− 1.6 | .086 |
| Body mass index | 35.4 +/− 6.9 | 36.7 +/− 8.7 | .417 |
| Hemoglobin HbA1c | 7.8 +/− 1.4 | 7.3+/− 1.6 | .316 |
Note: Data are means +/− SD unless otherwise indicated. Baseline group equivalence was evaluated with chi-square tests for categorical variables and t-tests for continuous. There were no significant differences between the two groups at baseline.
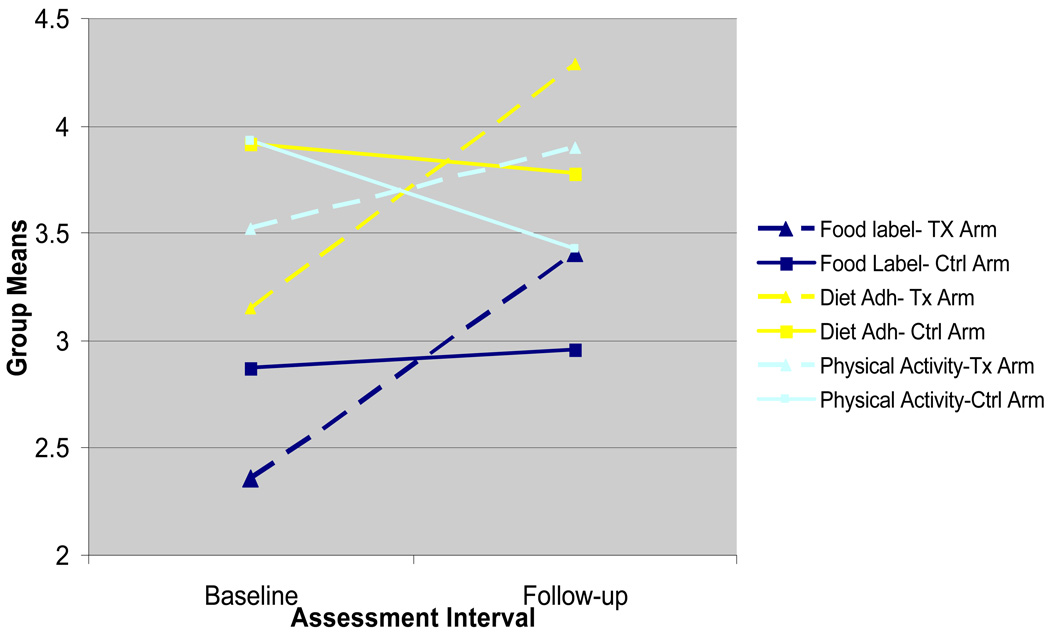
Diabetes Self-Care
Self-care behaviors were examined in terms of food label reading, diet adherence, and physical activity. The first ANCOVA models showed a significant effect of group over time on food label reading at three months (p < .008). As can be seen in Figure 1, after adjusting for baseline differences on food label reading (Intervention: M = 2.36, SD = 1.30 vs. Control: M = 2.87, SD = 1.41), patients in the intervention group (M = 3.50, SD = 1.11) were reading food labels significantly more than patients in the control group at follow-up (M = 2.86, SD = 1.29), F(1,88) = 7.65, p < .01. The second ANCOVA model showed significant effect of group over time on diet adherence at three months (p <.04). As seen in Figure 1, after adjusting for baseline differences on diet adherence (Intervention: M = 3.15, SD = 1.89 vs. Control: M = 3.92, SD = 2.00), patients in the intervention group (M = 4.42, SD = 1.82) were adhering to diet recommendations significantly more than patients in the control group at follow-up (M = 3.65, SD = 1.93), F(1,88) = 4.11, p < .05. Although physical activity scores were in the predicted direction as seen in Figure 1, the final ANCOVA model showed no group effect on physical activity at follow-up (p = 0.23).
Figure 1.
Baseline and post intervention group means for measures of self-care behaviors.
Glycemic Control
A significant baseline HbA1c by group interaction (p <.04) required the retention of the interactive model. Four t-tests with a Bonferroni adjustment (p < .01) were performed to test the group effect on baseline HbA1c scores and follow-up HbA1c scores, and the effect of time on each group’s HbA1c scores. HbA1c scores did not differ between groups at baseline (p = 0.32) or at follow-up (p = 0.76). The mean HbA1c score decreased in both groups, but only the intervention group showed significant improvement from baseline (M = 7.76, SD = 1.37) to follow-up (M = 7.28, SD = 1.29), (p < .008). The control group’s decrease from baseline (M = 7.45, SD = 1.58) to follow-up (M = 7.18, SD = 1.54) was not significant with a Bonferroni adjustment of .01, (p < .047).
Discussion
An IMB model-based intervention to improve diabetes self-care behaviors (food label reading, diet adherence, physical activity) and glycemic control in Puerto Ricans with T2DM was designed, implemented, and evaluated in a randomized control trial. To our knowledge, this study was the first to apply the IMB model framework to promote diabetes self-care behaviors in any population with diabetes. At the time the study was conducted, it was also the first theory-based, culturally tailored diabetes self-care intervention for Puerto Ricans specifically.
The intervention was brief, a 90 minute single session that allocated 60 minutes to diet content and 30 minutes to exercise content, and effectively improved food label reading and diet adherence at three months post intervention. Brief interventions have effectively improved diet outcomes; and, consistent with our findings, were less effective in improving physical activity (Clark, Hampson, Avery, & Simpson, 2004). While the intervention group’s HbA1c improved from baseline to follow-up, adjusted follow-up HbA1c values did not differ between the intervention and control groups. In a meta-analysis of 72 diabetes education interventions, patient contact was the only significant predictor of changes in HbA1c, with 23.6 hours of contact time needed for a clinically meaningful change of 1% absolute decrease (Norris, Lau, Smith, Schmid, & Engelgau, 2002). If the intervention group’s 0.48% absolute decrease in HbA1c is in fact the result of the intervention, then it took only 1.5 hours of contact time to achieve it compared to the 11.8 hours suggested by Norris et al. (2002).
Although high rates of uncontrolled blood glucose levels have been reported in Puerto Ricans with diabetes (Lipton et al., 1996), baseline HbA1c levels were near normal in this study. There was a baseline HbA1c covariate by group interaction, suggesting intervention impact varied according to initial HbA1c levels. Although not reported, secondary analyses did show the intervention’s impact was strongest for those with the highest baseline HbA1c levels. This is consistent with studies showing that improved HbA1c is much more likely when initial HbA1c levels are > 10% (Sarkisian et al., 2003).
The intervention described here is similar to others that have reduced HbA1c levels in Hispanic groups. Like our intervention, successful interventions have included one-to-one counseling, cultural-specific elements, and have focused on behavior change (Brown et al., 2002; Brown & Hanis, 1999; Corkery et al., 1997). Unlike other interventions, our intervention was individually-tailored to the needs of each patient, and grounded in a well-validated theoretical model (i.e., the model drove the intervention’s design, content, delivery, and evaluation). It also differed by being much briefer than previous interventions, and thus much more time and cost effective. A review of 72 diabetes education interventions found that intensive interventions do not necessarily produce significant reductions in HbA1c, despite their regular contact with patients (Norris, Engelgau, & Narayan, 2001).
There are several study limitations that should be acknowledged. First, we relied on self-reported measures of behavior. Although HbA1c outcomes corroborated self-reported changes in a behavior, it is important to note that the four-item food label measure was developed to overlap with intervention content. Although this measure demonstrated high internal consistency, additional psychometric evaluation is needed. Third, a larger sample size would generate greater confidence in the results, and allow for targeted exploration of retention and/or attrition effects, and meditational analyses to see if changes in levels information, motivation, and behavioral skills produced changes in behavior. In addition, follow-up data was limited to three months. While other brief interventions have shown continued improvement on multiple measures of diet behavior at twelve months (Clark et al., 2004), longer follow up periods are needed to explore the sustainability of intervention effects on diet behavior, physical activity, and glycemic control. Lastly, we did not address nor control for diabetes comorbidities (e.g., depression, hypertension, and dyslipidemia, obesity) or other self-care behaviors in the design, content, or assessment of the intervention. Future interventions for racial/ethnic minority groups should include both content to address, and assessments to monitor the impact of educational material on depressive symptoms, blood pressure, lipids, and changes in weight and other self-care behaviors. Despite these limitations, this study provides the preliminary data necessary to begin to assess the potential usefulness of the IMB model in designing culturally tailored intervention diabetes self-care interventions.
Conclusions
The intervention described here also incorporated the language, customs, attitudes, perceptions, and behaviors of the target population. It was carried out by a bilingual, medical assistant from patients’ country of origin who had been trained by a Registered Dietician and Certified Diabetes Educator also from patients’ country of origin. In addition, educational materials and health messages were available in Spanish and English, and took into consideration patient-specific barriers to self-care. As seen here, adapting diet recommendations that incorporate culturally familiar foods, and modifying rather than replacing individual’s culturally familiar diets may improve adherence to diet recommendations. Offering brief follow-up sessions or phone calls, and allocating more time to exercise behavior change may improve upon the existing intervention. While we found evidence of diet behavior change as a result of our intervention, our findings suggest that a single session intervention session, regardless of its length or depth is not enough to generate and sustain multiple behavioral changes. Yet, promising is the notion that this 90 minute intervention maybe more effective if it included several follow-up booster sessions, and possibly in-home sessions over an extended period of time.
Implications for Practice
Aspects of the evaluated IMB model-based intervention that may have contributed to its modest success include: sensitivity to patients with limited literacy and numeracy skills (Hosler & Melnik, 2005; Lipton, Losey, Giachello, Mendez, & Girotti, 1998); presentation of content in easy to read formats or in large print for those with impaired vision (Lipton et al., 1998; von Goeler et al., 2003); targeting single concept messages (e.g., eat less carbohydrates) embedded throughout the intervention to minimize failure in learners with limited literacy skills and those with memory problems; and the use of “teach back” techniques, where the interventionist explained/demonstrated new information, assessed patient recall and comprehension by asking patients to explain or demonstrate the concept, clarified the explanation to improve patient understanding, and reassessed patient recall and comprehension post explanation/demonstration. Finally, one intensive session may not be enough to produce sustained health behavior change, and educators will need to develop strategies for follow-up educational opportunities to be most successful.
Although further research is needed to establish the generalizability and durability over time of the demonstrated positive effects of this intervention, our initial outcomes are promising. Moreover, our results lend support to the growing body of literature and recommendations of tailoring health promotion interventions to the socio-cultural context in which patients must negotiate their self-care on a daily basis (Osborn & Fisher, 2008). Future work should specify the most valuable IMB model-based intervention content needed to initiate and sustain diabetes self-care behaviors across different patient samples. While we anticipate that the general content of the current intervention and its underling theoretical model could be articulated to a number of diverse populations, we strongly support a close examination of the extent to which the intervention and/or model can speak to the cultural beliefs and systems that influence diet, food choice, and physical activity across populations. Improvements to the current intervention include extending the contact time to > 90 minutes; expanding the amount of time spent on exercise; evaluating effectiveness for longer than three months; and including both content to address and assessments to monitor the impact of the intervention on depressive symptoms, blood pressure, lipids, weight, and other diabetes self-care behaviors.
Acknowledgements
We thank Demetria N. Cain, Luis Casillas, Andrew Dudley, Matt Dudley, Jill Irvine, Melissa Johnson, Beth La Pierre, Scott McCarthy, Erin Paice, Jane Quale, and Iliri Ibrahimi for their assistance in preparing intervention materials. Special thanks to Carmen Aponte, Chariunis Perez, and Rosemary Perez for study recruitment, and collecting and managing data; and Charlene Aponte for delivering the intervention. The study was supported by an American Psychological Association dissertation award and a pilot grant award from the Center for Health Intervention and Prevention at the University of Connecticut, Storrs, CT. Dr. Osborn conducted this research under an NIH/NIDDK National Research Service Award (F31 DK067022), and is currently supported by a Diversity Supplement Award (NIDDK P60 DK020593-30S2). Dr. Pérez-Escamilla’s contribution to this manuscript was partially supported by the Connecticut Center for Eliminating Health Disparities among Latinos with funding from the NIH/NCMHD (P20 MD001765).
Footnotes
The authors have no conflict of interest.
References
- Adams CR. Lessons learned from urban Latinas with type 2 diabetes mellitus. Journal of Transcultural Nursing. 2003;14(3):255–265. doi: 10.1177/1043659603014003012. [DOI] [PubMed] [Google Scholar]
- Ajzen I. The theory of planned behavior. Organizational Behavior and Human Decision Processes. Special Issue: Theories of cognitive self-regulation. 1991;50(2):179–211. [Google Scholar]
- Ajzen I, Fishbein M. The influence of attitudes on behavior. In: Albarracin D, Johnson BT, Zanna MP, editors. The handbook of attitudes. Mahwah, NJ: Lawrence Erlbaum Associates; 2005. pp. 173–221. [Google Scholar]
- Anderson RM, Funnell MM, Nwankwo R, Gillard ML, Oh M, Fitzgerald JT. Evaluating a problem-based empowerment program for African Americans with diabetes: results of a randomized controlled trial. Ethnicity and Disease. 2005;15(4):671–678. [PubMed] [Google Scholar]
- Bandura A. Human agency in social cognitive theory. The American Psychologist. 1989;44(9):1175–1184. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Brown SA, Garcia AA, Kouzekanani K, Hanis CL. Culturally competent diabetes self-management education for Mexican Americans: the Starr County border health initiative. Diabetes Care. 2002;25(2):259–268. doi: 10.2337/diacare.25.2.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SA, Hanis CL. Culturally competent diabetes education for Mexican Americans: the Starr County Study. The Diabetes Educator. 1999;25(2):226–236. doi: 10.1177/014572179902500208. [DOI] [PubMed] [Google Scholar]
- Clark M, Hampson SE, Avery L, Simpson R. Effects of a tailored lifestyle self-management intervention in patients with type 2 diabetes. British Journal of Health Psychology. 2004;9(Pt 3):365–379. doi: 10.1348/1359107041557066. [DOI] [PubMed] [Google Scholar]
- Coffman MJ. Effects of tangible social support and depression on diabetes self-efficacy. Journal of Gerontological Nursing. 2008;34(4):32–39. doi: 10.3928/00989134-20080401-02. [DOI] [PubMed] [Google Scholar]
- Corkery E, Palmer C, Foley ME, Schechter CB, Frisher L, Roman SH. Effect of a bicultural community health worker on completion of diabetes education in a Hispanic population. Diabetes Care. 1997;20(3):254–257. doi: 10.2337/diacare.20.3.254. [DOI] [PubMed] [Google Scholar]
- Cornman DH, Kiene SM, Christie S, Fisher WA, Shuper PA, Pillay S, et al. Clinic-based intervention reduces unprotected sexual behavior among HIV-infected patients in KwaZulu-Natal, South Africa: results of a pilot study. Journal of Acquired Immune Deficiency Syndromes. 2008;48(5):553–560. doi: 10.1097/QAI.0b013e31817bebd7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fisher JD, Cornman DH, Osborn CY, Amico KR, Fisher WA, Friedland GA. Clinician-initiated HIV risk reduction intervention for HIV-positive persons: Formative research, acceptability, and fidelity of the Options Project. Journal of Acquired Immune Deficiency Syndromes. 2004;37 Suppl 2:S78–S87. doi: 10.1097/01.qai.0000140605.51640.5c. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change. In: Peterson JL, DiClemente RJ, editors. Handbook of HIV prevention. New York: Kluwer Academic/Plenum Press; 2000. pp. 3–55. [Google Scholar]
- Fisher JD, Fisher WA, Cornman DH, Amico RK, Bryan A, Friedland GH. Clinician-delivered intervention during routine clinical care reduces unprotected sexual behavior among HIV-infected patients. Journal of Acquired Immune Deficiency Syndromes. 2006;41(1):44–52. doi: 10.1097/01.qai.0000192000.15777.5c. [DOI] [PubMed] [Google Scholar]
- Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Malden, MA: Blackwell; 2003. pp. 82–106. [Google Scholar]
- Fisher WA, Schachner H. Self-monitoring of blood glucose in diabetic children and adolescents--barriers, behaviors, and the search for solutions. US Endocrinology. (in press) [Google Scholar]
- Horowitz CR, Williams L, Bickell NA. A community-centered approach to diabetes in East Harlem. Journal of General Internal Medicine. 2003;18(7):542–548. doi: 10.1046/j.1525-1497.2003.21028.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosler AS, Melnik TA. Population-based assessment of diabetes care and self-management among Puerto Rican adults in New York City. The Diabetes Educator. 2005;31(3):418–426. doi: 10.1177/0145721705276580. [DOI] [PubMed] [Google Scholar]
- Kennedy L, Herman WH. Glycated hemoglobin assessment in clinical practice: comparison of the A1cNow point-of-care device with central laboratory testing (GOAL A1C Study) Diabetes Technology and Therapeutics. 2005;7(6):907–912. doi: 10.1089/dia.2005.7.907. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, Skinner C. What's in a name? Health Education Research. 2000;15:1–4. doi: 10.1093/her/15.1.1. [DOI] [PubMed] [Google Scholar]
- Lipton RB, Losey L, Giachello AL, Corral M, Girotti MH, Mendez JJ. Factors affecting diabetes treatment and patient education among Latinos: results of a preliminary study in Chicago. Journal of Medical Systems. 1996;20(5):267–276. doi: 10.1007/BF02257040. [DOI] [PubMed] [Google Scholar]
- Lipton RB, Losey LM, Giachello A, Mendez J, Girotti MH. Attitudes and issues in treating Latino patients with type 2 diabetes: views of healthcare providers. Diabetes Educ. 1998;24(1):67–71. doi: 10.1177/014572179802400109. [DOI] [PubMed] [Google Scholar]
- Mauldon M, Melkus GD, Cagganello M. Tomando Control: a culturally appropriate diabetes education program for Spanish-speaking individuals with type 2 diabetes mellitus--evaluation of a pilot project. The Diabetes Educator. 2006;32(5):751–760. doi: 10.1177/0145721706291999. [DOI] [PubMed] [Google Scholar]
- Norris SL, Engelgau MM, Narayan KM. Effectiveness of self-management training in type 2 diabetes: a systematic review of randomized controlled trials. Diabetes Care. 2001;24(3):561–587. doi: 10.2337/diacare.24.3.561. [DOI] [PubMed] [Google Scholar]
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25(7):1159–1171. doi: 10.2337/diacare.25.7.1159. [DOI] [PubMed] [Google Scholar]
- Osborn CY. Using the IMB model of health behavior change to promote self-management behaviors in Puerto Ricans with diabetes. Dissertation Abstracts International Section A: Humanities and Social Sciences. 2006;Vol, 67(6-A):2064. [Google Scholar]
- Osborn CY, Egede LE. Validation of an Information-Motivation-Behavioral Skills model of diabetes self-care (IMB-DSC) Patient Education and Counseling. 2009 doi: 10.1016/j.pec.2009.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Osborn CY, Fisher JD. Diabetes education: Integrating theory, cultural considerations, and individually tailored content. Clinical Diabetes. 2008;26(4):148–150. [Google Scholar]
- Punzalan C, Paxton KC, Guentzel H, Bluthenthal RN, Staunton AD, Mejia G, et al. Seeking community input to improve implementation of a lifestyle modification program. Ethnicity and Disease. 2006;16(1 Suppl 1):S79–S88. [PubMed] [Google Scholar]
- Rollnick S, Heather N, Bell A. Negotiating behavior change in medical settings: The development of brief motivational interviewing. Journal of Mental Health. 1992;1:25–37. [Google Scholar]
- Sarkisian CA, Brown AF, Norris KC, Wintz RL, Mangione CM. A systematic review of diabetes self-care interventions for older, African American, or Latino adults. The Diabetes Educator. 2003;29(3):467–479. doi: 10.1177/014572170302900311. [DOI] [PubMed] [Google Scholar]
- Smith CA, Barnett E. Diabetes-related mortality among Mexican Americans, Puerto Ricans, and Cuban Americans in the United States. Pan American Journal of Public Health. 2005;18(6):381–387. doi: 10.1590/s1020-49892005001000001. [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Hampson SE, Glasgow RE. The summary of diabetes self-care activities measure: results from 7 studies and a revised scale. Diabetes Care. 2000;23(7):943–950. doi: 10.2337/diacare.23.7.943. [DOI] [PubMed] [Google Scholar]
- Villaire M, Mayer G. Low health literacy: the impact on chronic illness management. Professional Case Management. 2007;12(4):213–216. doi: 10.1097/01.PCAMA.0000282907.98166.93. quiz 217–218. [DOI] [PubMed] [Google Scholar]
- von Goeler DS, Rosal MC, Ockene JK, Scavron J, De Torrijos F. Self-management of type 2 diabetes: a survey of low-income urban Puerto Ricans. The Diabetes Educator. 2003;29(4):663–672. doi: 10.1177/014572170302900412. [DOI] [PubMed] [Google Scholar]
- Wang CY, Chan SM. Culturally tailored diabetes education program for Chinese Americans: a pilot study. Nursing Research. 2005;54(5):347–353. doi: 10.1097/00006199-200509000-00009. [DOI] [PubMed] [Google Scholar]
- Whitman S, Silva A, Shah AM. Disproportionate impact of diabetes in a Puerto Rican community of Chicago. Journal of Community Health. 2006;31(6):521–531. doi: 10.1007/s10900-006-9023-7. [DOI] [PubMed] [Google Scholar]