Although not a hernia recurrence, symptomatic bulging after laparoscopic ventral hernia repair requires a new repair.
Keywords: Laparoscopic repair, Ventral incisional hernia, Mesh, Bulging
Abstract
Background and Objectives:
To investigate the prevalence, diagnosis, clinical significance, and treatment strategies for bulging in the area of laparoscopic repair of ventral hernia that is caused by mesh protrusion through the hernia opening, but with intact peripheral fixation of the mesh and actually a still sufficient repair.
Methods:
Medical records of all 765 patients who underwent laparoscopic ventral hernia repair were reviewed, and all patients with a swelling in the repaired area were identified and analyzed.
Results:
Twenty-nine patients were identified. They all underwent a computed tomography assessment. Seventeen patients (2.2% of the total group) had a hernia recurrence; in an additional 12 patients (1.6%), radiologic examinations indicated only bulging of the mesh but no recurrence. Bulging was associated with pain in 4 patients who underwent relaparoscopy and got a new, larger mesh tightly stretched over the entire previous repair. Eight asymptomatic patients decided on “watchful waiting.” All patients remained symptom free during a median follow-up of 22 months.
Conclusion:
Symptomatic bulging, though not a recurrence, requires a new repair and must be considered as an important negative outcome of laparoscopic ventral hernia repair. In asymptomatic patients, “watchful waiting” seems justified.
INTRODUCTION
Every swelling or bulge in the area of previous laparoscopic repair of a ventral or incisional hernia (LRVIH) is by definition suggestive of recurrence but is not obligatory to be so. Even in a sufficient LRVIH with an intact fixation of the edges of the mesh, the latter can protrude through the hernia opening into the hernia sac thereby causing a bulge that is frequently impossible to clinically differentiate from a recurrence. This condition is usually called “bulging.” Exact data on the prevalence of bulging, its clinical significance, and suggested treatment strategies are missing so far. We analyzed our experience on this issue in a large series of patients who underwent LRVIH in our hospital.
MATERIALS AND METHODS
Between January 2001 and March 2010, 2 senior surgeons (JTFJR and SR) performed LRVIH in 765 patients. All patients underwent LRVIH using an expanded polytetrafluoroethylene mesh (DualMesh, WL Gore & Associates, Flagstaff, AZ, USA) tailored to overlap all hernia margins by at least 3cm. The original mesh was used, and no fenestrations were made in it. No effort was made to reapproximate the edges of the hernia opening. The mesh was fixed either by a double circle of tacks (ProTack®, TycoUSS, Norwalk CT, USA), a technique popularly known as a “double crown” (n=455), or with a single circle of tacks along the periphery of the mesh and transabdominal sutures placed equidistant along the perimeter of the mesh (n=310). The size of the hernia did not play a role in selection of the mesh fixation method. During fixation of the mesh, intraabdominal pressure was routinely reduced from a standard 12mm Hg to 8 to 10mm Hg to avoid a protrusion of the mesh into the hernia sac after decompression of the abdomen and to prevent consecutive bulging. With the same goal, care was routinely taken to tightly stretch the mesh over the hernia opening.
All patients were scheduled to return for a follow-up examination at 2, 6, and 12 weeks and thereafter when they had any kind of LRVIH-related problem. The vast majority of patients in this series (n=752/765; 98.3%) were patients who belong to the adherence area of our hospital. It can be assumed that practically all of these patients would return to our hospital for any kind of LRVIH-related problem.
Patients who presented with a swelling in the repaired area were by definition suspected for a recurrence. All these patients underwent a computed tomography (CT) assessment. When relevant, various diameters of meshes, hernia openings, and the abdomen were measured on the CT scans by using the AquariusNet program (TeraRecon, Inc., San Mateo, CA, USA). This was possible due to the property of expanded polytetrafluoroethylene mesh of being revealed by CT. By using the AquarusNet program, an examiner, using a computer mouse, can trace a line precisely over the contour of the mesh or make a line between 2 points, for example between the edges of the hernia opening, whose lengths are then measured by the computer program. As we previously reported,1 in patients with a precisely known transverse diameter of implanted mesh that was put in the horizontal position (thus not angled, it was possible to measure shrinkage of the mesh. Mesh shrinkage was defined as the relative loss of transverse diameter as compared with the original transverse diameter of the mesh.
Patients with a confirmed recurrence underwent a new LRVIH. Remaining patients had a protrusion of the mesh into the hernia sac with an intact fixation of the edges of the mesh hence having actually a still sufficient repair. These patients represented a “bulging” study group and were analyzed in this report. Available video recordings of the initial repairs that resulted in “bulging” (n=2) were also examined.
Statistical analysis was carried out using the Fisher exact test. P<0.05 was considered statistically significant.
RESULTS
During follow-up-up (mean 32.3±18.3 months), 29 patients presented with a swelling in the repaired area. Seventeen patients (17/765; 2.2%) had a recurrence, and 16 of them underwent laparoscopic re-repair. One symptom-free patient with a recurrent hernia did not want to be treated.
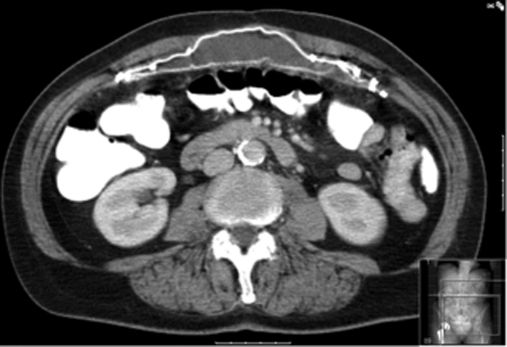
For an additional 12 patients (12/765; 1.6%) with a swelling in the repaired area, the CT scan did not show a recurrence but demonstrated a bulging of the mesh through the hernia opening (Figure 1). Table 1 shows characteristics of these patients, their hernias, and the repairs performed. There was no significant difference in the incidence of bulging according to mesh fixation technique. There was no significant difference in body mass index between patients who developed bulging (30.2±7.2) and patients who did not develop bulging (28.7±5.6). Bulging was observed in a wide range of initial hernia defects, and no relation was observed between hernia defect size and development of bulging.
Figure 1.
Computed tomographic scan demonstrating sufficient repair but with protrusion of the mesh into the hernia.
Table 1.
Patient Characteristics
| Patient Number | Age | Sex | Type of Hernia | Fascia Defect Size | Mesh Size | Fixation Methoda |
|---|---|---|---|---|---|---|
| 1 | 65 | M | Umbilical | 4 cm2 | 10×15 | TAS & T |
| 2 | 33 | M | Incisional | 4 cm2 | 15×15 | TAS & T |
| 3 | 39 | M | Incisional | Multiple defects | 15×19 | TAS & T |
| 4 | 59 | M | Incisional | 25 cm2 | 15×19 | TAS & T |
| 5 | 79 | M | Incisional | 64 cm2 | 15×19 | DC |
| 6 | 64 | F | Incisional | Multiple defects | 20×25 & 10×15 | DC |
| 7 | 67 | F | Incisional | Not specified* | 20×30 | TAS & T |
| 8 | 43 | M | Epigastric | 4 cm2 | 10×15 | DC |
| 9 | 46 | M | Incisional | Multiple defects | 20×30 | DC |
| 10 | 42 | M | Incisional | 150 cm2 | 20×30 | TAS & T |
| 11 | 51 | M | Umbilical | 2.5 cm2 | 10×15 | TAS & T |
| 12 | 48 | M | Diastasis Recti | Not specified | 15×19 | DC |
TAS & T=transabdominal sutures and tacks; DC=double crown of tacks.
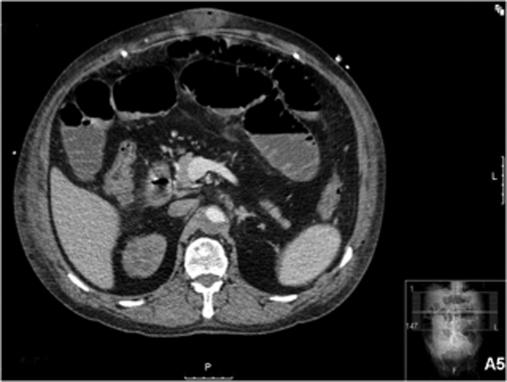
Four of these patients were symptomatic and had pain as their main complaint. They underwent relaparoscopy, which definitely excluded a recurrent hernia and confirmed protrusion or bulging of the mesh into the original hernia. Mesh bulging was corrected by tightly stretching a new, larger DualMesh over the entire previous repair, which was left in place (Figure 2). This new mesh was fixed by using the “double crown” technique. All relaparoscopies were uneventful and without postoperative complications. All these patients remained symptom free and without swelling during a mean follow-up of 17 months (range, 15 to 26).
Figure 2.
Computed tomographic scan 3 months after correction of symptomatic bulging by tightly stretching a new, larger mesh over the entire previous repair that was left in place. Note the presence of seroma between 2 meshes.
The remaining 8 patients were symptom free. After having been explained the nature of the problem, all of these patients opted for “watchful waiting.” These patients remained either asymptomatic (n=6) or with minimal discomfort (n=2). None of them had a progression of the bulge or had a hernia recurrence during a mean follow-up of 22 months (range, 12 to 41).
Review of both existing video recordings of the initial LRVIH demonstrated that the correct operative technique was applied and that the mesh was tightly stretched over the hernia opening at the end of the procedure.
In 9 of 12 patients with bulging, we were able to measure the shrinkage of the mesh. The mean shrinkage was 3.1% (range, 0% to 11%). None of these patients had a larger transverse diameter of mesh at CT than that of the original implant.
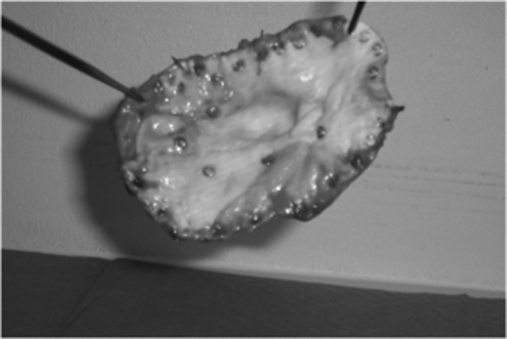
One of the asymptomatic patients, chronologically our first case of bulging, underwent laparotomy on a later occasion because of malignant disease. That procedure demonstrated a sufficient repair but, due to contamination, included removal of the mesh with central bulging into the original umbilical hernia (Figure 3).
Figure 3.
Photograph of the mesh removed at laparotomy shows central bulging of the mesh.
Another asymptomatic patient who originally had a large incisional hernia in the midline presented one year postoperatively with swelling in the repaired area. Simultaneously, we also discovered that one month after LRVIH, on request of another medical specialist, a CT scan was performed for a nonhernia-related indication. Review of that early postoperative CT demonstrated an adequate position of the mesh that was properly stretched over the hernia opening and without any signs of bulging (Figure 4). The weight of the patient was 96kg at that time. Now 10 months after that scan, we performed a new CT scan that demonstrated a sufficient repair, but with bulging of the mesh into the original hernia opening (Figure 5). At that time, the weight of the patient was 91kg. By performing a series of measurements at the same levels on both CT scans, we found out that there was no shrinkage of the mesh and that overlap between the mesh and the abdominal wall remained the same and adequate. However, the transverse diameter of the hernia opening and all other measured abdominal diameters were reduced on the second CT (Table 2). We had the opportunity to follow subsequent CT scans that were requested by other specialists for a nonhernia related indication. At all these scans, the repair remained sufficient but the transverse diameter of the hernia opening was continuously reducing (Table 3).
Figure 4.
Early postoperative computed tomographic scan demonstrating an adequate position of the mesh that is properly stretched over the hernia opening and without any signs of bulging.
Figure 5.
Computed tomographic scan 11 months after laparoscopic repair of a ventral or incisional hernia, demonstrating a still sufficient repair but showing bulging of the mesh into the hernia.
Table 2.
Measurements of Various Abdominal Diameters on Computed Tomograhphic Scans
| Measured diameter (mm) | 1 month Postoperatively | 11 months Postoperatively |
|---|---|---|
| Outside abdominal perimeter at level of 3rd lumbal vertebra (L3) | 1200 | 1119 |
| Inside abdominal perimeter passing through L3 | 1106 | 1051 |
| Sagittal body diameter at L3 level | 350 | 302 |
| Hernia opening at L3 levela | 109 | 93 |
Distance between medial sides of rectus muscles.
Table 3.
Transverse Diameter of Hernia Opening Measured on the Same Level on Computed Tomographic Scansa
| CT Scan Performed | Measured Transverse Diameter (mm) |
|---|---|
| May 2007 | 109 |
| March 2008 | 93 |
| August 2008 | 89 |
| April 2009 | 84 |
| December 2009 | 78 |
Operation performed in April 2007.
DISCUSSION
After LRVIH, bulging occurs almost as often as recurrence and must be considered as an important adverse outcome of LRVIH. In a patient presenting with swelling in the area of previous LRVIH, it is frequently impossible to clinically make a distinction between a recurrence and a bulging of the mesh. This emphasizes the importance of radiological examinations in establishing a correct diagnosis. Meshes that can be revealed by high resolution imaging techniques, such as computed tomography (CT) and magnetic resonance imaging, allow the clinician to determine whether the patient has a recurrence or bulging from a mesh protrusion. In symptomatic patients, differentiating between a hernia recurrence and bulging is somewhat therapeutically irrelevant, because both conditions usually require a new repair. In asymptomatic patients, however, radiologically confirmed diagnosis of bulging may avoid unnecessary reoperation for, actually, only a cosmetic problem.
Traditionally, the development of bulging was considered a failure of the correct surgical technique to tightly stretch the mesh over the hernia opening.2 A loosely stretched mesh can protrude into the hernia defect when the pneumoperitoneum is released, thereby causing bulging. Bulging may be particularly noticeable if the defect is small. In such defects, even minimal laxity may allow the mesh to protrude into the hernia. In larger hernias, more laxity would be necessary for the mesh to protrude into the defect, and the protrusion would probably not be as noticeable because the curvature of the bulge would be more gradual. In larger defects, some authors suggest a larger overlap of mesh to resist the intraabdominal forces that act to push the mesh into the hernia defect.3,4 Since a certain difference in abdominal circumference exists between the insufflated and desufflated abdomen, partial desufflation of the abdomen before fixation of tightly stretched mesh has been advised so that when the pneumoperitoneum is evacuated, there is a tension-free repair without protrusion of the mesh into the hernia defect.5
All principles mentioned above were also carefully applied in our patients who developed bulging, thereby suggesting the role of some other mechanisms in the genesis of this adverse outcome of LRVIH. A feature of the LRVIH technique that we and most other surgeons use is that no effort is made to close the actual hernia defect. The lack of any fascial or muscular covering of the defect has the consequence that only the mesh buttresses the defect against intraabdominal pressure. That may predispose to protrusion of the mesh into the hernia. Consequently, a possible way to prevent bulging of the mesh might be closure of the hernia defect, as suggested by some authors.6,7 Indeed, these authors have not reported on bulging as a problem after LRVIH. However, closure of, especially larger, defects results in no longer a “tension free” repair and that is contradictory to one of the basic principles of modern hernia repair. Comparative studies on the issue of closing a hernia defect before LVIHR are missing and at this moment, it is impossible to make any reliable clinical conclusions.
Theoretically, protrusion of a properly stretched mesh into the hernia can be caused by 2 factors: (1) elongation of the mesh or (2) reduction of the hernia defect herewith the mesh becoming too large. Sufficient tensile strength of currently used meshes has not been questioned so far. Even if we assume that all prosthetic materials can elongate to some minor degree when placed under appropriate force for a prolonged period of time, our CT measurements did not lend any support to this hypothesis.1 Another possibility–reduction of the hernia opening–seems much more realistic. Spontaneous approximation of the fascial edges of the hernia opening occurs in most patients after LRVIH.8 Our findings strongly support that possibility. This process is not well understood, but it definitely has a potential to induce some late laxity of an initially appropriately stretched mesh. In a similar way, weight loss and consecutive reduction of body diameters including size of the hernia opening, such as was demonstrated in our patient, may cause the same result. Medialization of the rectus muscles, the most probable cause of bulging after correct LRVIH, does appear to occur early in the postoperative period, and the extent of medialization does not appear to be related to the follow-up interval.6,8 Our clinical experience provides support to a previous observation: once “bulging” occurs, it has neither the tendency for further enlargement nor seems to lead to the development of recurrences.
The suggestion that possible shrinkage of meshes might play a role in development of bulging after LVIHR remains without any supportive evidence.1
When symptomatic, the only treatment solution for bulging is a new repair. We could not find any rational argument for removal of the primary mesh. In addition, the mesh with bulging, still sufficiently fixed to the abdominal wall, may provide a certain support from outside for a new mesh, in balancing increases in intraabdominal pressure. Our experience indicates that that “repair over repair” seems to provide a good and durable symptomatic and cosmetic result.
In asymptomatic patients, “watchful waiting” seems to be a reasonable option.
CONCLUSION
Symptomatic bulging, though strictly not a recurrence, must be considered an important adverse outcome of LRVIH. Correct operative technique cannot always prevent development of bulging thereby suggesting the role of some other mechanisms. Reduction of the hernia opening either due to a medialization of the edges of the hernia defect or due to weight loss might be the most important of them. Clinical distinction between a recurrence and a bulging of the mesh is frequently impossible, thus emphasizing the importance of radiological examinations in establishing a correct diagnosis. In symptomatic patients, this might be somewhat therapeutically irrelevant, because both conditions usually require a new repair. In asymptomatic patients, however, radiologically confirmed diagnosis of bulging may avoid unnecessary reoperation for, actually, only a cosmetic problem. For realistic evaluation of postoperative results of LRVIH, a symptomatic bulging should be considered as a recurrence.
References:
- 1. Schoenmaeckers EJ, van der Valk SB, van den Hout HW, Raymakers JF, Rakic S. Computed tomographic measurements of mesh shrinkage after laparoscopic ventral incisional hernia repair with an expanded polytetrafluoroethylene mesh. Surg Endosc. 2009. July;23(7):1620–1623 [DOI] [PubMed] [Google Scholar]
- 2. Voeller GB. Repair of incisional hernias and midline defects. In: Bendavid RB, Abrahamson J, Arregui ME, Flamant JB, Philips EH, et al., eds. Abdominal Wall Hernias: Principles and Management. New York, NY: Springer Verlag; 2001; 77: 519–524 [Google Scholar]
- 3. Cobb WS, Kercher KW, Matthews BD, et al. Laparoscopic ventral hernia repair: a single center experience. Hernia. 2006. June;10(3):236–242 [DOI] [PubMed] [Google Scholar]
- 4. Heniford BT, Park A, Ramshaw BJ, Voeller G. Laparoscopic repair of ventral hernias: nine years' experience with 850 consecutive hernias. Ann Surg. 2003. September;238(3):391–399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Perrone JM, Soper NJ, Eagon JC, et al. Perioperative outcomes and complications of laparoscopic ventral hernia repair. Surgery. 2005. October;138(4):708–715 [DOI] [PubMed] [Google Scholar]
- 6. Chelala E, Thoma M, Tatete B, Lemye AC, Dessily M, Alle JL. The suturing concept for laparoscopic mesh fixation in ventral and incisional hernia repair: Mid-term analysis of 400 cases. Surg Endosc. 2007; 21 (3): 391–395 [DOI] [PubMed] [Google Scholar]
- 7. Franklin ME, Jr., Gonzalez JJ, Glass JL, Manjarrez A. Laparoscopic ventral and incisional hernia repair: an 11-year experience. Hernia. 2004; 8 (1): 23–27 [DOI] [PubMed] [Google Scholar]
- 8. Sickle KR, Baghai M, Mattar SG, et al. What happens to the rectus abdominus fascia after laparoscopic ventral hernia repair? Hernia. 2005; 9 (4): 358–362 [DOI] [PubMed] [Google Scholar]