Small bowel lipomas, which can cause intussusception and gastrointestinal bleeding, can be managed with laparoscopic resection when diagnosed preoperatively.
Keywords: Lipoma, Intussusception, Gastrointestinal hemorrhage, Laparoscopic surgery, Video capsule endoscopy
Abstract
Background:
Small bowel tumors are rare entities that often present with nonspecific symptoms. The diagnosis is more likely in patients with occult gastrointestinal bleeding of unknown origin or in adults with small bowel intussusception. Even with exhaustive diagnostic testing, small bowel tumors are often not diagnosed preoperatively. Because 60% to 70% of small bowel tumors are malignant, surgical excision is always recommended.
Methods:
We report the case of a 73-year-old man with occult gastrointestinal bleeding. A small bowel tumor was discovered only after video capsule endoscopy, computed tomography, and multiple endoscopies were performed.
Results:
The patient underwent laparoscopic exploration. An incidental intussusception made the tumor simple to identify. By extending the umbilical port, the tumor was easily removed. The final pathology demonstrated a submucosal lipoma.
Conclusions:
Small bowel lipomas can cause intussusception and gastrointestinal bleeding. When diagnosed preoperatively, laparoscopic resection is feasible.
INTRODUCTION
Neoplasms of the gastrointestinal tract originate from the small bowel only 1% to 2% of the time.1 The majority of these tumors are benign in nature.1 Lipomas of the small bowel are the third most common benign tumor, adenomas being the first.1 Small bowel lipomas are generally asymptomatic. However, obstruction, perforation, intussusception, pain, and bleeding can complicate their presence.2 It is recommended that these tumors be removed when discovered.
CASE REPORT
A 73-year-old man came to our center with iron-deficiency anemia (hemoglobin, 11.7g/Dl) and heme-positive stools. The patient reported no abdominal pain, nausea or vomiting, melena, hematochezia, or change in his bowel habits.
Colonoscopy revealed no cause of bleeding, and upper endoscopy revealed a hiatal hernia, mild gastritis, and duodenitis. He received a course of omeprazole but continued to be anemic (Hg 11.8 g/Dl). Repeat upper endoscopy and push enteroscopy (which uses a longer endoscope up to 260cm) revealed no obvious pathology. Biopsies of the small bowel ruled out celiac disease.
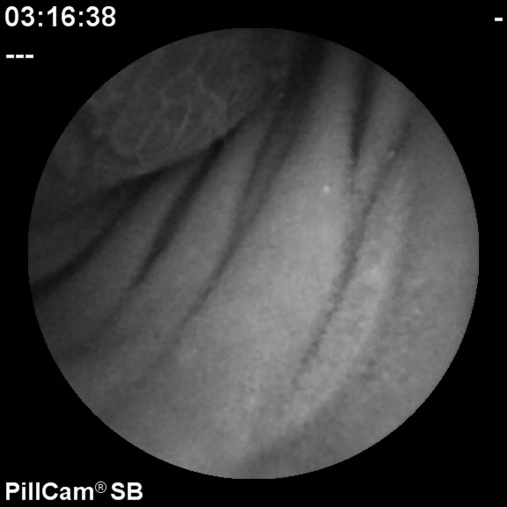
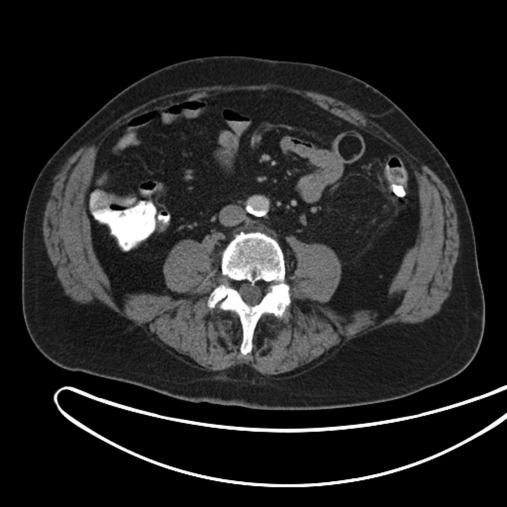
Subsequently, video capsule endoscopy (VCE) revealed a pedunculated mass, likely in the mid small intestine (Figure 1). In an attempt to further localize the tumor, a small bowel series was obtained but could not visualize the mass. Computed tomography (CT) of the abdomen revealed a 2.1-cm polypoid mass resembling a lipoma in the mid-jejunum (Figure 2).
Figure 1.
Figure 2.
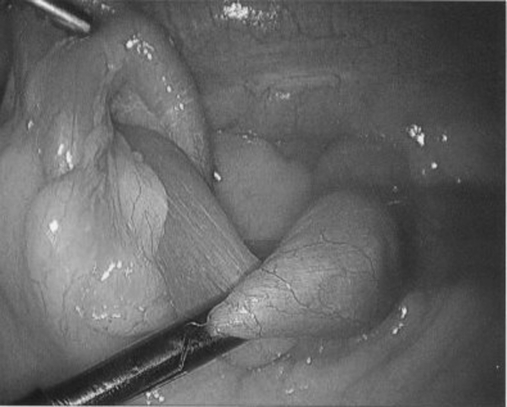
The patient underwent an exploratory laparoscopy. We used a 10-mm umbilical port as part of an open Hasson technique and placed two 5-mm ports in both lower quadrants of the abdomen. By grasping a loop of small bowel, we were able trace it back to the ligament of Treitz. Then, we closely examined the small bowel and palpated it with the blunt graspers. An intussusception was identified in the mid-jejunum (Figure 3). To mark the area in question, we looped a Penrose drain around the bowel and secured the drain with an Endoclip. We inspected the remaining bowel but found no pathology.
Figure 3.
Intracorporal reduction was not attempted. The intussuscepted bowel segment was externalized by extending the umbilical trocar site. The segment was resected en bloc, and a stapled anastomosis was performed extracorporeally. Back-table inspection of the excised segment confirmed our preoperative suspicion of a small bowel lipoma (Figure 4). The mass was submucosal and firm, with excoriation of the mucosa. The final pathologic diagnosis confirmed sheets of adipocytes consistent with lipoma.
Figure 4.
The patient recovered well and was discharged home on postoperative day 3. His blood counts returned to normal.
DISCUSSION
Up to 60% to70% of small bowel tumors are malignant, according to a large operative series.1 In that series, adenocarcinoma was the most common type, followed by carcinoid, lymphoma, and malignant gastrointestinal stromal tumors (GISTs).1 Of the small bowel tumors removed at surgery in that series, 30% to 40% were benign; the most frequent benign tumors were GISTs and adenomas, whereas lipomas were only discovered 4% to 6% of the time.1
The lack of specific symptoms makes the identification of small bowel tumors difficult.1 Over 50% of new diagnoses are incidental findings in asymptomatic patients. Pain, distention, nausea, and vomiting are associated with intraluminal obstruction. Intermittent cramping pain and guaiac-positive stools can be related to intussusception caused by small bowel tumors. Malignancy can cause similar symptoms, as well as in patients with advanced cancer, melena, weight loss, or perforation. Small bowel tumors account for 5% of gastrointestinal tract tumors and often present with occult gastrointestinal bleeding (GIB).2 When assessing patients with such symptoms, small bowel neoplasia, though rare, should be considered in the differential diagnosis.
Our patient had occult GIB as the only suggestion of a small bowel origin. When the source of occult GIB has not been found by conventional upper and lower endoscopy, the search for its cause is often frustrating. Once the stomach, duodenum, and colon have been eliminated as possible sources, the entire small bowel remains to be examined. Push enteroscopy can examine 60cm past the ligament of Treitz with a small flexible scope. A small bowel series is useful in finding strictures and inflammation1 but often cannot detect small submucosal tumors such as lipomas. Enteroclysis, which involves injecting a thin stream of barium through a nasojejunal tube directly into the area of question, helped diagnose the cause of occult GIB in 11% of the patients in the aforementioned series.1
In our patient, VCE proved useful. A study using VCE as the initial investigation in patients with occult GIB showed a positive predictive value of 94.4% and a negative predictive value of 100%.4 In a recent review, patients with small bowel tumors underwent an average of 4.2 nondiagnostic tests before diagnosis with VCE.4 In another study, VCE identified significantly more sources of small bowel bleeding than did push enteroscopy and was better tolerated by patients; in addition to small bowel tumors, it was also able to detect other lesions originally missed by upper and lower endoscopy.5
Small bowel tumors often serve as lead points for intussusception in adults. The most common symptom is pain (80%), followed by distention and nausea.6 Our patient had an incidental intussusception, found at the time of the operation. In a review of 58 adults with intussusception, 93% were found to have a pathologic lesion, 52% benign and 48% malignant.7 That high rate reinforces the convention of resecting all adult intussusceptions. If intussusception is suspected, ultrasound, CT, or magnetic resonance (MR) imaging is useful. In a retrospective review of 33 adults with intussusception, all of the intussusceptions were visible on CT or MR imaging.8
Laparoscopic surgery for management of small bowel obstruction has been described widely.9–14 In a recent large series, the primary causes were adhesive disease (37.9%) and incarcerated ventral hernia (32.4%).9 Small bowel tumors were a rare discovery during laparoscopy. In our review of the literature, we found only 1 case of laparoscopic resection of a small bowel lipoma. Small bowel lipomas in particular tend to be submucosal, making them difficult to diagnose laparoscopically unless they are large or associated with intussusception. The rate of conversion from laparoscopy to an open procedure for treatment of small bowel obstruction ranges from 0% to 16.7%.11–13 If locating a small bowel tumor is difficult with laparoscopy, converting to an open procedure should be done quickly.
CONCLUSION
Small bowel tumors are an infrequent finding in general surgery. However, when assessing a patient with nonspecific GI symptoms, particularly occult GIB, small bowel tumors should be high on the differential diagnosis list. In such patients, VCE is a viable diagnostic tool. In adults with small bowel tumors, resection is mandatory, because such tumors serve as lead points for intussusception more than 66% of the time. Laparoscopic resection of small bowel tumors is the treatment of choice.
Contributor Information
Layla C. Lucas, The University of Arizona, Department of Surgery, Tucson, Arizona, USA..
Ronnie Fass, Southern Arizona VA Healthcare System, Department of Surgery, Tucson, Arizona..
Robert S. Krouse, Southern Arizona VA Healthcare System, Department of Surgery, Tucson, Arizona..
References:
- 1. Ashley SW, Wells SA., Jr Tumors of the small intestine. Semin Oncol. 1988; 15: 116–128 [PubMed] [Google Scholar]
- 2. Chou J, Feng C, Lai H, et al. Obscure gastrointestinal bleeding caused by small bowel lipoma. Inter Med. 2008; 47: 1601–1603 [DOI] [PubMed] [Google Scholar]
- 3. Delvaux M, Fassler I, Gay G. Clinical usefulness of the endoscopic video capsule as the initial intestinal investigation in patients with obscure digestive bleeding: validation of a diagnostic strategy based on the patient outcome after 12 months. Endoscopy. 2004; 36 (12): 1067–1073 [DOI] [PubMed] [Google Scholar]
- 4. Cobrin GM, Pittman RH, Lewis BS. Increased diagnostic yield of small bowel tumors with capsule endoscopy. Cancer. 2006; 107: 22–27 [DOI] [PubMed] [Google Scholar]
- 5. Mylonaki M, Fritscher-Ravens A, Swain P. Wireless capsule endoscopy: a comparison with push enteroscopy in patients with gastroscopy and colonoscopy negative gastrointestinal bleeding. Gut. 2003; 52: 1122–1126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wang L, Wu C, Yu J, Hsiao C, Hsu C, Jao S. Clinical entity and treatment strategies for adult intussusceptions: 20 years' experience. Dis Colon Rectum. 2007; 50: 1941–1949 [DOI] [PubMed] [Google Scholar]
- 7. Azar T, Berger DL. Adult intussusception. Ann Surg. 1997; 226 (2): 134–138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Warshauer DM, Lee JKT. Adult intussusception detected at CT or MR imaging: clinical –imaging correlation. Radiology. 1999; 212: 853–860 [DOI] [PubMed] [Google Scholar]
- 9. Chowbey PK, Panse R, Sharma A, Khullar R, Soni V, Baijal M. Elective laparoscopy in diagnosis and treatment of recurrent small bowel obstruction. Surg Lapaosc Endovasc Percutan Tech. 2006; 16: 416–422 [DOI] [PubMed] [Google Scholar]
- 10. Ishibashi Y, Yamamoto S, Yamada Y, Fujita S, Akasu T, Moriya Y. Laparoscopic resection for malignant lymphoma of the ileum causing ileocecal intussusception. Surg Laparosc Endosc Percutan Tech. 2007; 5: 444–446 [DOI] [PubMed] [Google Scholar]
- 11. Palanivelu C, Rangarajan M, Senthilkumar R, Madankumar MV. Minimal access surgery for adult intussusception with subacute intestinal obstruction. Surg Laparosc Endosc Percutan Tech. 2007; 17: 487–491 [DOI] [PubMed] [Google Scholar]
- 12. Kirshtein B, Roy-Shapira A, Lantsberg L, Avinoach E, Mizrahi S. Laparoscopic management of acute small bowel obstruction. Surg Endosc. 2005; 19: 464–467 [DOI] [PubMed] [Google Scholar]
- 13. Zerey M, Sechrist CW, Kercher KW, Sing RF, Matthews BD, Heniford BT. The laparoscopic management of small-bowel obstruction. Am J Surg. 2007; 194: 882–888 [DOI] [PubMed] [Google Scholar]
- 14. Tsushimi T, Matsui N, Kurazumi H, et al. Laparoscopic resection of an ileal lipoma: report of a case. Surg Today. 2006; 36: 1007–1011 [DOI] [PubMed] [Google Scholar]