Abstract
Estimation of the GFR (eGFR) using creatinine- or cystatin C–based equations is imperfect, especially when the true GFR is normal or near-normal. Modest reductions in eGFR from the normal range variably predict cardiovascular morbidity. If eGFR associates not only with measured GFR (mGFR) but also with cardiovascular risk factors, the effects of these non–GFR-related factors might bias the association between eGFR and outcome. To investigate these potential non–GFR-related associations between eGFR and cardiovascular risk factors, we measured GFR by iohexol clearance in a sample from the general population (age 50 to 62 years) without known cardiovascular disease, diabetes, or kidney disease. Even after adjustment for mGFR, eGFR associated with traditional cardiovascular risk factors in multiple regression analyses. More risk factors influenced cystatin C–based eGFR than creatinine-based eGFR, adjusted for mGFR, and some of the risk factors exhibited nonlinear effects in generalized additive models (P < 0.05). These results suggest that eGFR, calculated using standard creatinine- or cystatin C–based equations, partially depends on factors other than the true GFR. Thus, estimates of cardiovascular risk associated with small changes in eGFR must be interpreted with caution.
Chronic kidney disease (CKD) has been established as a risk factor for cardiovascular disease (CVD).1 There are reasons to believe that increased risk may be present even at GFRs presently considered as normal or near normal. An association between normal or near normal GFR and CVD or cardiovascular mortality has been found in some studies2–4 but not in others.5–7 The most important limitation of these studies has been the use of creatinine- or cystatin C–based formulas to estimate GFR. Because precise methods for measuring GFR are difficult and costly to implement in large cohorts, estimated GFR (eGFR) has been accepted as a proxy for measured GFR (mGFR).
Different methods for calculating eGFR have given different results. Estimates of GFR based on cystatin C have been found to predict CVD mortality better than creatinine-based eGFR. This has been shown in the elderly, in patients with known CKD or CVD, and in the general population.2,8–13 The reason for the different performance of the two estimates of GFR may be either different abilities to estimate GFR or a dependence on non-GFR confounders.14 More specifically, the effects of non-GFR factors on cystatin C and creatinine might bias the association between eGFR and CVD. The occurrence and strength of such associations have thus far not been studied by an accurate method of GFR measurement in the general population.
In the Renal Iohexol Clearance Survey in Tromsø 6 (RENIS-T6), GFR was measured by iohexol clearance and estimated by creatinine or cystatin C in a middle-aged cohort from the general population. The aim of this cross-sectional study was to explore the validity of using eGFR as a proxy for mGFR in studies of CVD risk. We assessed the associations between traditional cardiovascular risk factors and eGFR when mGFR, measured as iohexol clearance, was adjusted for. We also wanted to study the relationship between mGFR and cardiovascular risk factors.
RESULTS
In the sixth Tromsø population survey (Tromsø 6), 739 of the 3564 participants 50 to 62 years of age reported a previous myocardial infarction, angina pectoris, stroke, diabetes mellitus, or kidney disease. Of the remaining 2825 persons eligible for inclusion, 1632 were investigated in our study. Five were excluded because their iohexol clearance measurements suffered technical failures. This left us with 1627 persons for this analysis (826 women and 801 men). The characteristics of the participants are described in Table 1. Mean mGFR was 87.8 ml/min per 1.73 m2 in women and 95.7 ml/min per 1.73 m2 in men.
Table 1.
Mean (SD) of study population characteristics
| Characteristic | Women (n = 826) | Men (n = 801) |
|---|---|---|
| Age, years | 58.1 (3.9) | 58.0 (3.8) |
| Weight, kg | 72.5 (12.3) | 87.2 (12.4) |
| Height, cm | 164.5 (6.0) | 176.9 (6.2) |
| Body mass index, kg/m2 | 26.8 (4.4) | 27.8 (3.5) |
| Plasma creatinine | ||
| mmol/L | 59.80 (9.40) | 74.50 (10.80) |
| mg/dl | 0.67 (0.10) | 0.84 (0.12) |
| Plasma cystatin C, mg/L | 0.79 (0.11) | 0.80 (0.11) |
| Measured GFR, ml/min per 1.73 m2 | 87.8 (14.0) | 95.7 (13.7) |
| Estimated GFR, ml/min per 1.73 m2 | ||
| MDRD equation | 92.3 (17.1) | 95.9 (15.7) |
| CKD-EPI equation | 94.4 (10.0) | 95.3 (9.0) |
| Rule's cystatin C equation | 93.3 (17.9) | 90.9 (15.8) |
The distributions of cardiovascular risk factors, adjusted for age and medication according to gender and quintiles of mGFR, are shown in Table 2. Multiple linear regression analyses with mGFR as the dependent variable and the cardiovascular risk factors as the independent variables are shown in Table 3. In the fully adjusted model, there were statistically significant associations between mGFR and smoking and diastolic BP. We tested for gender interaction with all variables in the fully adjusted model and found interactions with body mass index (BMI) and HDL cholesterol (P < 0.05). For men, mGFR increased 1.93 ml/min per 1.73 m2 per SD of BMI (P = 0.002) and 1.79 ml/min per 1.73 m2 per SD of HDL cholesterol (P = 0.003). For women, these estimates were not statistically significant. When the same variables as in model 2 (Table 3) were analyzed in a generalized additive model, nonlinear effects of diastolic BP and triglycerides were found (P < 0.05). Diastolic BP greater than about 90 mmHg was associated with reduced mGFR, whereas triglycerides greater than about 2 were associated with increased mGFR (data not shown).
Table 2.
Risk factors for cardiovascular disease by gender-specific quintiles of measured glomerular filtration rate
| Quintile 1 | Quintile 2 | Quintile 3 | Quintile 4 | Quintile 5 | P for Linear Trend | ||
|---|---|---|---|---|---|---|---|
| GFR range (ml/min per 1.73 m2) | Female | <77.2 | 77.2–84.5 | 84.5–91.2 | 91.2–98.9 | <98.9 | |
| Male | <84.6 | 84.6–92.0 | 92.0–99.1 | 99.1–106.9 | <106.9 | ||
| Agea mean (95% CI) | Female | 59.4 (58.8 to 60.0) | 58.7 (58.1 to 59.3) | 58.3 (57.7 to 58.8) | 57.5 (56.9 to 58.1) | 56.7 (56.1 to 57.2) | <0.0001 |
| Male | 58.8 (58.2 to 59.4) | 58.4 (57.8 to 58.9) | 57.8 (57.2 to 58.4) | 57.8 (57.2 to 58.4) | 57.4 (56.9 to 58.0) | <0.0001 | |
| Body mass index, kg/m2b mean (95% CI) | Female | 27.3 (26.6 to 27.9) | 27.1 (26.5 to 27.8) | 26.5 (25.9 to 27.2) | 26.5 (25.8 to 27.1) | 26.5 (25.8 to 27.1) | 0.04 |
| Male | 27.7 (27.2 to 28.2) | 27.4 (26.8 to 27.9) | 28.4 (27.9 to 28.9) | 27.5 (27.0 to 28.0) | 28.2 (27.6 to 28.7) | 0.21 | |
| Systolic BP,b mmHg mean (95% CI) | Female | 125.5 (122.9 to 128.1) | 125.3 (122.8 to 127.9) | 125.4 (122.8 to 127.9) | 125.9 (123.4 to 128.5) | 124.9 (122.3 to 127.5) | 0.88 |
| Male | 135.4 (132.9 to 138.0) | 135.8 (133.2 to 138.4) | 133.9 (131.3 to 136.4) | 131.7 (129.1 to 134.3) | 133.4 (130.9 to 136.0) | 0.05 | |
| Diastolic BP,b mmHg mean (95% CI) | Female | 81.7 (80.3 to 83.2) | 80.9 (79.5 to 82.3) | 80.8 (79.4 to 82.2) | 80.2 (78.7 to 81.6) | 80.2 (78.7 to 81.6) | 0.09 |
| Male | 87.5 (86.0 to 88.9) | 87.5 (86.0 to 88.9) | 86.0 (84.5 to 87.4) | 85.1 (83.7 to 86.6) | 85.1 (83.7 to 86.6) | 0.003 | |
| Total cholesterol,c mmol/L mean (95% CI) | Female | 5.73 (5.58 to 5.87) | 5.71 (5.57 to 5.85) | 5.60 (5.46 to 5.74) | 5.75 (5.61 to 5.89) | 5.72 (5.57 to 5.86) | 0.94 |
| Male | 5.50 (5.35 to 5.64) | 5.71 (5.57 to 5.86) | 5.56 (5.41 to 5.70) | 5.62 (5.47 to 5.76) | 5.54 (5.40 to 5.69) | 1.00 | |
| HDL cholesterol,c mmol/L mean (95% CI) | Female | 1.67 (1.61 to 1.74) | 1.71 (1.64 to 1.77) | 1.70 (1.64 to 1.76) | 1.65 (1.59 to 1.71) | 1.64 (1.58 to 1.71) | 0.27 |
| Male | 1.33 (1.27 to 1.39) | 1.42 (1.37 to 1.48) | 1.39 (1.33 to 1.44) | 1.40 (1.34 to 1.45) | 1.40 (1.34 to 1.45) | 0.27 | |
| LDL cholesterol,c mmol/L mean (95% CI) | Female | 3.67 (3.54 to 3.81) | 3.62 (3.48 to 3.75) | 3.52 (3.39 to 3.65) | 3.70 (3.56 to 3.83) | 3.66 (3.53 to 3.80) | 0.78 |
| Male | 3.68 (3.55 to 3.80) | 3.81 (3.68 to 3.94) | 3.66 (3.53 to 3.79) | 3.74 (3.62 to 3.87) | 3.64 (3.51 to 3.77) | 0.54 | |
| Triglycerides,c mmol/L mean (95% CI) | Female | 1.14 (1.05 to 1.22) | 1.04 (0.96 to 1.13) | 1.01 (0.93 to 1.09) | 1.11 (1.03 to 1.20) | 1.16 (1.07 to 1.24) | 0.43 |
| Male | 1.32 (1.21 to 1.44) | 1.27 (1.16 to 1.39) | 1.41 (1.29 to 1.52) | 1.25 (1.13 to 1.36) | 1.31 (1.19 to 1.42) | 0.75 | |
| Current smokers,b % mean (95% CI) | Female | 17.4 (14.5 to 20.2) | 19.9 (16.9 to 23.0) | 22.6 (19.4 to 25.9) | 22.9 (19.6 to 26.1) | 31.6 (27.8 to 35.5) | 0.09 |
| Male | 20.1 (17.0 to 23.2) | 11.2 (8.9 to 13.6) | 18.4 (15.4 to 21.4) | 20.6 (17.5 to 23.7) | 27.4 (23.8 to 31.0) | 0.22 | |
| Physically active,b % mean (95% CI) | Female | 45.2 (40.6 to 49.8) | 44.5 (40.0 to 49.1) | 50.1 (45.3 to 54.9) | 48.7 (43.9 to 53.4) | 44.1 (39.6 to 48.7) | 0.47 |
| Male | 45.5 (40.8 to 50.2) | 42.1 (37.6 to 46.5) | 42.7 (38.2 to 47.3) | 42.0 (37.5 to 46.5) | 27.4 (23.8 to 31.1) | 0.20 | |
| First degree relative with CVD,b % mean (95% CI) | Female | 70.8 (65.1 to 76.6) | 70.4 (64.7 to 76.1) | 62.8 (57.4 to 68.2) | 67.9 (62.3 to 73.5) | 68.0 (62.4 to 73.7) | 0.35 |
| Male | 68.7 (63.0 to 74.4) | 66.5 (60.9 to 72.2) | 67.5 (61.8 to 73.1) | 56.1 (50.9 to 61.2) | 69.0 (63.3 to 74.8) | 0.06 | |
| First degree relative with MI > 60 years,b % mean (95% CI) | Female | 24.6 (21.2 to 28.0) | 21.2 (18.1 to 24.3) | 15.7 (13.0 to 18.4) | 20.7 (17.6 to 23.8) | 21.8 (18.6 to 25.0) | 0.29 |
| Male | 19.9 (16.8 to 23.0) | 17.3 (14.4 to 20.2) | 20.1 (17.0 to 23.2) | 19.6 (16.5 to 22.6) | 18.3 (15.4 to 21.3) | 0.94 |
CI, confidence intervals.
aAdjusted for current use of angiotensin ezyme inhibitors and angiotensin receptor blockers.
bAdjusted for age and current use of angiotensin enzyme inhibitors and angiotensin receptor blockers.
cAdjusted for age and current use of angiotensin enzyme inhibitors, angiotensin receptor blockers, and lipid-lowering medication.
Table 3.
Multiple linear regression analysis of measured GFR and cardiovascular risk factors
| Independent Variable | Model 1. Adjusted for Age, Gender, Use of ACE Inhibitors or ARBs |
Model 2. As Model 1 and Adjusted for All Other Independent Variables Except Systolic BP |
||||
|---|---|---|---|---|---|---|
| Estimate (ml/min per 1.73 m2) | (95% CI) | P | Estimate (ml/min per 1.73 m2) | (95% CI) | P | |
| First degree relative with MI < 60 years (yes/no) | −0.57 | (−2.24 to 1.09) | 0.50 | −0.51 | (−2.16 to 1.14) | 0.54 |
| Physically active versus inactive | −1.57 | (−2.91 to −0.23) | 0.02 | −1.06 | (−2.43 to 0.30) | 0.13 |
| Current smoking versus not smoking | 3.37 | (1.75 to 4.98) | <0.0001 | 2.87 | (1.18 to 4.56) | <0.0001 |
| Body mass index per SD increasea | −0.13 | (−0.81 to 0.55) | 0.71 | −0.87 | (−1.80 to 0.06) | 0.07 |
| Systolic BP per SD increase | −0.56 | (−1.27 to 0.14) | 0.12 | |||
| Diastolic BP per SD increase | −1.03 | (−1.73 to −0.34) | 0.003 | −0.94 | (−1.67 to −0.21) | 0.01 |
| LDL cholesterol per SD increase | −0.30 | (−0.96 to 0.36) | 0.38 | −0.27 | (−0.96 to 0.43) | 0.45 |
| HDL cholesterol per SD increaseb | −0.01 | (−0.72 to 0.70) | 0.98 | −1.04 | (−2.09 to 0.01) | 0.05 |
| Triglycerides per SD increase | 0.13 | (−0.55 to 0.80) | 0.72 | 0.31 | (−0.49 to 1.10) | 0.45 |
ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker; CI, confidence intervals.
aSignificant gender interaction for body mass index: Female, estimate = −0.87, P = 0.07. Male, estimate = 1.93, P = 0.002.
bSignificant gender interaction for HDL cholesterol: Female, estimate −1.04, P = 0.05. Male, estimate = 1.79, P = 0.003.
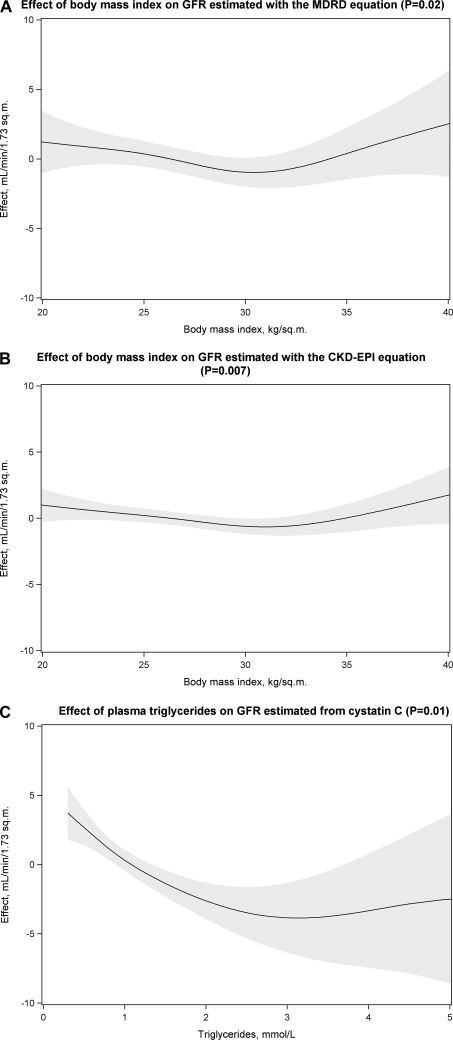
Multiple linear regression analyses with creatinine- and cystatin C–based eGFR as the dependent and cardiovascular risk factors as the independent variables are shown in Table 4. Models 2 and 3 included adjustment for mGFR to assess the effects of cardiovascular risk factors on eGFR not mediated by variation in GFR. In the fully adjusted model 3, only current smoking influenced the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) estimates, whereas the Modification in Renal Disease (MDRD)-estimates were influenced by both current smoking and having a first-degree relative with a myocardial infarction (MI) before the age of 60 years (P < 0.05). Current smoking, BMI, HDL cholesterol, and triglycerides were associated with the cystatin C–based estimates (P < 0.05). No statistically significant interactions between gender and any of the other independent variables were found, except for a small effect of the interaction with LDL cholesterol for the MDRD equation (P = 0.048). Analyses of the same variables as in model 3 with generalized additive models found nonlinear effects of BMI on the MDRD and CKD-EPI estimates and of triglycerides on the cystatin C–based estimates (P < 0.05; Figure 1). Errors-in-variables regression with same variables as in model 3 found the same pattern of statistically significant effects when the reliability of mGFR was set at 0.7, except for a small effect of diastolic BP on the cystatin C–based estimate (P = 0.04). The magnitude of the effects was also similar to those in model 3 (Table 4; data not shown).
Table 4.
Multiple linear regression analyses of association between estimates of GFRs and cardiovascular risk factors
| Dependent Variable | Independent Variable | Model 1. Adjusted for Age, Gender, Use of Angiotensin Converting Enzyme Inhibitors or Angiotensin Receptor Blockers |
Model 2. As Model 1 and Adjusted for Measured GFR |
Model 3. As Model 2 and Adjusted for All Other Independent Variables Except Systolic BP |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate (ml/min per 1.73 m2) | (95% CI) | P | Estimate (ml/min per 1.73 m2) | (95% CI) | P | Estimate (ml/min per 1.73 m2) | (95% CI) | P | ||
| MDRD equation | First degree relative with MI < 60 years (yes/no) | −2.18 | (−4.18 to −0.18) | 0.03 | −1.81 | (−3.48 to −0.13) | 0.03 | −1.75 | (−3.41 to −0.08) | 0.04 |
| Physically active versus inactive | −2.66 | (−4.27 to −1.06) | <0.0001 | −1.63 | (−2.98 to −0.29) | 0.02 | −1.03 | (−2.41 to 0.34) | 0.14 | |
| Current smoking versus not smoking | 6.54 | (4.61 to 8.46) | <0.0001 | 4.36 | (2.73 to 5.99) | <0.001 | 3.87 | (2.15 to 5.58) | <0.0001 | |
| Body mass index per SD increase | −0.70 | (−1.52 to 0.12) | 0.09 | −0.61 | (−1.30 to 0.07) | 0.08 | −0.26 | (−1.02 to 0.51) | 0.51 | |
| Systolic BP per SD increase | −0.91 | (−1.76 to −0.07) | 0.03 | −0.54 | (−1.25 to 0.17) | 0.13 | ||||
| Diastolic BP per SD increase | −1.70 | (−2.54 to −0.87) | <0.0001 | −1.03 | (−1.73 to −0.32) | <0.001 | −0.62 | (−1.36 to 0.12) | 0.10 | |
| LDL cholesterol per SD increase | −0.30 | (−1.10 to 0.50) | 0.46 | −0.10 | (−0.77 to 0.57) | 0.77 | 0.06 | (−0.64 to 0.76) | 0.86 | |
| HDL cholesterol per SD increase | 0.15 | (−0.71 to 1.00) | 0.73 | 0.15 | (−0.56 to 0.87) | 0.68 | 0.06 | (−0.77 to 0.89) | 0.89 | |
| Triglycerides per SD increase | −0.14 | (−0.95 to 0.68) | 0.74 | −0.22 | (−0.90 to 0.46) | 0.53 | −0.20 | (−0.99 to 0.60) | 0.63 | |
| CKD-EPI equation | First degree relative with MI < 60 years (yes/no) | −1.16 | (−2.28 to −0.04) | 0.04 | −0.95 | (−1.89 to −0.01) | 0.047 | −0.92 | (−1.85 to 0.02) | 0.06 |
| Physically active versus inactive | −1.33 | (−2.22 to −0.43) | <0.0001 | −0.76 | (−1.52 to 0.00) | 0.050 | −0.53 | (−1.30 to 0.25) | 0.18 | |
| Current smoking versus not smoking | 3.10 | (2.02 to 4.18) | <0.0001 | 1.90 | (0.98 to 2.81) | <0.001 | 1.63 | (0.67 to 2.59) | <0.0001 | |
| Body mass index per SD increase | −0.44 | (−0.90 to 0.02) | 0.06 | −0.39 | (−0.78 to −0.01) | 0.046 | −0.21 | (−0.64 to 0.22) | 0.33 | |
| Systolic BP per SD increase | −0.54 | (−1.02 to −0.07) | 0.02 | −0.34 | (−0.74 to 0.06) | 0.09 | ||||
| Diastolic BP per SD increase | −0.91 | (−1.38 to −0.45) | <0.0001 | −0.54 | (−0.94 to −0.15) | 0.01 | −0.33 | (−0.74 to 0.09) | 0.13 | |
| LDL cholesterol per SD increase | −0.20 | (−0.65 to 0.25) | 0.38 | −0.09 | (−0.47 to 0.28) | 0.63 | 0.02 | (−0.37 to 0.42) | 0.91 | |
| HDL cholesterol per SD increase | 0.12 | (−0.35 to 0.60) | 0.61 | 0.13 | (−0.27 to 0.53) | 0.53 | 0.01 | (−0.46 to 0.47) | 0.98 | |
| Triglycerides per SD increase | −0.16 | (−0.61 to 0.29) | 0.49 | −0.21 | (−0.59 to 0.18) | 0.29 | −0.16 | (−0.61 to 0.28) | 0.47 | |
| Rule's cystatin C equation | First degree relative with MI < 60 years (yes/no) | −0.30 | (−2.33 to 1.74) | 0.78 | 0.08 | (−1.64 to 1.80) | 0.93 | 0.36 | (−1.23 to 1.95) | 0.66 |
| Physically active versus inactive | 1.44 | (−0.20 to 3.08) | 0.08 | 2.47 | (1.09 to 3.86) | <0.001 | 0.04 | (−1.27 to 1.36) | 0.95 | |
| Current smoking versus not smoking | −6.56 | (−8.52 to −4.60) | <0.0001 | −8.85 | (−10.48 to −7.22) | <0.001 | −8.94 | (−10.58 to −7.30) | <0.0001 | |
| Body mass index per SD increase | −3.35 | (−4.17 to −2.53) | <0.0001 | −3.26 | (−3.95 to −2.57) | <0.001 | −2.81 | (−3.54 to −2.08) | <0.0001 | |
| Systolic BP per SD increase | −0.33 | (−1.20 to 0.53) | 0.45 | 0.04 | (−0.69 to 0.77) | 0.92 | ||||
| Diastolic BP per SD increase | −0.81 | (−1.66 to 0.05) | 0.06 | −0.13 | (−0.86 to 0.59) | 0.72 | 0.32 | (−0.39 to 1.03) | 0.37 | |
| LDL cholesterol per SD increase | −1.31 | (−2.12 to −0.50) | <0.0001 | −1.11 | (−1.80 to −0.43) | <0.001 | 0.00 | (−0.67 to 0.66) | 0.99 | |
| HDL cholesterol per SD increase | 3.53 | (2.68 to 4.39) | <0.0001 | 3.54 | (2.82 to 4.25) | <0.001 | 1.63 | (0.83 to 2.42) | <0.0001 | |
| Triglycerides per SD increase | −3.00 | (−3.82 to −2.19) | <0.0001 | −3.09 | (−3.77 to −2.40) | <0.001 | −1.29 | (−2.06 to −0.53) | 0.001 | |
Each row gives the estimates of the regression coefficients from three different models where the dependent variable is given in the first column and the independent variable in the second. Each of the three models was adjusted for different covariates, as indicated in the column headings. CI, confidence interval.
Figure 1.
The nonlinear relationships between estimated GFR and cardiovascular risk factors after adjustment for measured GFR. The gray area indicates the 95% confidence interval.
Table 5 shows the 10-year risk of coronary heart disease estimated with the Framingham equation according to gender- and method-specific quintiles. The risk in women fell with decreasing mGFR and with both the creatinine-based eGFRs (P < 0.05). In contrast, in both genders, the CVD risk increased substantially with decreasing cystatin C–based eGFR (P < 0.0001). When the risk was adjusted for smoking, the differences in the risk estimates across the quintiles for mGFR and creatinine-based eGFR were not statistically significant, whereas the differences for cystatin C–based eGFR were attenuated but still significant (P for linear trend 0.001 for women, <0.0001 for men; data not shown).
Table 5.
Ten-year cardiovascular riska (%) estimated with the Framingham equation by gender- and method-specific quintiles of measured or estimated GFR
| GFR Method | Quintile 1 (95% CI) | Quintile 2 (95% CI) | Quintile 3 (95% CI) | Quintile 4 (95% CI) | Quintile 5 (95% CI) | P for Linear Trend | |
|---|---|---|---|---|---|---|---|
| Measured GFR | Female | 5.6 (5.1 to 6.1) | 5.5 (5.0 to 6.0) | 5.5 (5.0 to 6.1) | 6.1 (5.6 to 6.6) | 6.2 (5.7 to 6.8) | 0.02 |
| Male | 21.7 (19.6 to 23.9) | 19.7 (17.5 to 21.8) | 20.1 (18.0 to 22.3) | 20.4 (18.2 to 22.5) | 21.4 (19.2 to 23.5) | 1.00 | |
| MDRD equation | Female | 5.6 (5.1 to 6.1) | 5.5 (5.0 to 6.0) | 5.6 (5.1 to 6.1) | 5.9 (5.4 to 6.5) | 6.3 (5.8 to 6.8) | 0.02 |
| Male | 20.6 (18.4 to 22.8) | 20.5 (18.3 to 22.7) | 19.5 (17.4 to 21.7) | 21.5 (19.3 to 23.6) | 21.2 (19.1 to 23.4) | 0.52 | |
| CKD-EPI equation | Female | 5.5 (5.0 to 6.0) | 5.7 (5.2 to 6.3) | 5.3 (4.8 to 5.8) | 5.9 (5.4 to 6.4) | 6.5 (6.0 to 7.1) | 0.01 |
| Male | 21.0 (18.8 to 23.1) | 19.3 (17.1 to 21.5) | 21.3 (19.1 to 23.4) | 20.3 (18.2 to 22.5) | 21.4 (19.2 to 23.7) | 0.58 | |
| Rule's cystatin C equation | Female | 6.7 (6.1 to 7.2) | 6.2 (5.7 to 6.7) | 5.4 (4.9 to 5.9) | 5.7 (5.3 to 6.2) | 5.0 (4.5 to 5.5) | <0.0001 |
| Male | 25.4 (23.3 to 27.6) | 22.3 (20.2 to 24.4) | 21.8 (19.6 to 24.0) | 18.5 (16.5 to 20.5) | 16.0 (13.9 to 18.1) | <0.0001 |
Quintile 1 is the lowest, and quintile 5 the highest. CI, confidence interval.
aThere were no diabetics included in the study population.
DISCUSSION
We found that eGFR based on either creatinine or cystatin C was influenced by traditional cardiovascular risk factors even after adjusting for mGFR, indicating that the mechanisms for these associations were independent of GFR. This was especially true for eGFR based on cystatin C, which was associated with several cardiovascular risk factors in a fully adjusted model (Table 4, model 3). The creatinine-based MDRD and CKD-EPI equations seemed to be less influenced, but both exhibited a nonlinear relationship with BMI, which resulted in an increased eGFR for persons with a BMI exceeding about 30 kg/m2 (Figure 1, A and B). This could bias the estimated cardiovascular risk from reduced GFR in obese persons in longitudinal studies. There was also a nonlinear effect of triglycerides on eGFR from cystatin C (Figure 1C).
Associations between cystatin C and cardiovascular risk factors have been found in at least two recent studies.15,16 When adjusting for GFR measured as creatinine clearance, Knight et al.15 found that cystatin C was associated with age, gender, weight, height, and current smoking but not with hyperlipidemia. The limited precision of creatinine clearance for measuring GFR and the inclusion of persons with prevalent cardiovascular disease may account for the differences from our study. Stevens et al.16 found associations between cystatin C and BMI and systolic BP after adjusting for GFR measured as iothalamate or Cr-EDTA clearance. In the same study, the authors found associations between creatinine and BMI. HDL cholesterol and triglycerides were not examined in this study. The results are not directly comparable to this study because the study population consisted of CKD patients with a mean GFR of 44 ml/min per 1.73 m2 and because the associations were not analyzed in multiple regression analyzes. Neither Knight et al. nor Stevens et al. tested for nonlinear effects.
When examining the relationships between cardiovascular risk factors and GFR measured as iohexol clearance, complex associations were found in this healthy middle-aged study population (Table 3). The impact of BMI and HDL cholesterol was different in men and women. To our knowledge, RENIS-T6 is the first study where an accurate method for measuring GFR has been used in a large cohort from the general population. All previous studies of the relationship between cardiovascular risk factors and GFR in the general population have relied on estimates based on creatinine or creatinine clearance.2,6,17–19 In some of these studies, the relationships were confounded by the inclusion of persons with established CVD or kidney disease,2,17–19 some did not perform multiple regression analyses,2,6,17 or, in some, the interactions between gender and the risk factors were not tested.2,6,17,19 However, Nitsch et al.18 found interactions between gender and several cardiovascular risk factors in a cross-sectional study from a Swiss population. U-shaped relationships between creatinine-clearance and systolic BP, diastolic BP, serum triglycerides, and C-reactive protein were found in the Prevention of Renal and Vascular Disease study.
We found a positive association between current smoking and increasing mGFR. This confirms findings in several studies using creatinine-based eGFR.2,6,17,18,20,21 In these studies, a possible explanation was that GFR had been overestimated in smokers because they have lower muscle mass and lower creatinine than nonsmokers, but our results show that current smoking is truly associated with an increase in GFR. However, an association between smoking and creatinine-based eGFR persisted even after adjustment for mGFR, which means that reduced muscle mass and creatinine production are partly responsible for the relationship between smoking and eGFR (Table 4, models 2 and 3). The mechanism for smoking-induced hyperfiltration is uncertain because several experimental studies have shown a reduced GFR immediately after smoking or the administration of nicotine.22,23 Because our subjects had been instructed to avoid tobacco before the measurement of iohexol clearance, the higher mGFR in smokers may have been caused by a withdrawal phenomenon.
To explore the magnitude of the combined effect of the traditional risk factors with both mGFR and eGFR, we studied the distribution of the 10-year risk of coronary heart disease estimated with the Framingham equation across method-specific quintiles of GFR. Although both mGFR and creatinine-based eGFR exhibited similar patterns with an increasing risk for women with increasing GFR quintiles, there was a marked gradient in the opposite direction for cystatin C–based eGFR for both genders (Table 5). However, after adjustment for smoking, there was nonsignificant differences in the 10-year risk for coronary heart disease across the quintiles of mGFR and creatinine-based eGFR, but the difference between the cystatin C–based quintiles remained statistically significant. These findings suggest that correct adjustment for confounding cardiovascular risk factors in survival analysis is more critical for GFR estimates based on cystatin C than for creatinine-based estimates.
eGFR has been accepted as a proxy for mGFR in epidemiologic studies because of the lack of GFR measurements. Longitudinal studies of eGFR as a cardiovascular risk factor have used linear adjustments for the traditional risk factors. None of them incorporated nonlinear effects,2–4,6 and gender-specific analyses were only reported in the study of Astor et al. Thus, there is a possibility of residual confounding from cardiovascular risk factors in these survival analyses, but it is difficult to assess the size and direction of the resulting bias. Although the magnitude of most of the nonlinear relationships found in this study was modest, even small effects may result in biased estimates in large studies and should be considered. The dependence of eGFR on cardiovascular risk factors in addition to GFR makes it difficult to interpret risk estimates and might limit the usefulness of eGFR as proxy for GFR in longitudinal studies of persons with near-normal GFR.
The most important strength of this study was its use of GFR measurements rather than estimates in a large cohort from the general population. Plasma iohexol clearance is an accurate method for measuring GFR.24 The single-sample method we used has been found to be at least as reliable as the multi-sample method when both were compared with CrEDTA-clearance, especially for GFR >60 ml/min per 1.73 m2.25 Even so, measurement error and day-to-day variation in GFR could conceivably have introduced bias in our analyses. However, the results of errors-in measurements regression, which takes measurement error in independent variables into account, gave results very similar to those given in Table 4. Because we did not include repeat measurements of GFR in the same persons in this study, the reliability of mGFR used in these analyses was set at values far lower than found in the literature to provide a conservative assessment of possible bias.
One limitation of this study was its cross-sectional design. A definitive assessment of the confounding effects of non-GFR factors in cohort studies of eGFR and CVD can only be made in survival analyses comparing the effects of mGFR and eGFR directly, but data on endpoints is not available at this time. The inclusion of only middle-aged participants was another limitation. Nonlinear associations have been found in studies with wider age ranges, however, and we expect that our findings are valid for other age groups than those examined. Because no non-whites were included, generalizability to other ethnic groups may also be limited.
We conclude that GFR estimated by either creatinine or cystatin C is dependent on non–GFR-related factors in addition to GFR. Some of these associations were nonlinear. The possibility of residual confounding from these factors in studies of GFR and cardiovascular risk in persons with a GFR close to the normal range cannot be ruled out. The estimates of the effect of eGFR on CVD in these studies should be interpreted with caution.
CONCISE METHODS
Study Population and Data Collection
The Tromsø study is a population-based, prospective study with repeated health surveys of inhabitants of the municipality of Tromsø in northern Norway. In the sixth Tromsø study (Tromsø 6), which was performed in 2007/2008, an age-stratified random sample of all inhabitants between 40 and 87 years of age were invited. Of the 65,286 inhabitants in Tromsø county, 12,984 persons met for the examination. The attendance rate for the invited participants was 66%. They answered an extensive questionnaire about smoking habits, physical activity, medication, and sociodemographic characteristics.
In the age group between 50 and 62 years, a total of 3564 participants completed the main part of Tromsø 6. Based on answers from the self-administered questionnaire, participants who reported no previous MI, angina pectoris, stroke, diabetes mellitus, or any renal disease (except urinary tract infection) were invited to the RENIS-T6. They were stratified according to age and gender and included to a predetermined target of 1600 participants. Pregnant women and individuals reporting allergies to radiocontrast, iodine, or latex were excluded.
Measurements
All investigations for this study took place at the clinical research unit at the University Hospital of North Norway. Participants met between 8:00 and 10:00 am. They were instructed to avoid large meals with meat and nonsteroid anti-inflammatory drugs in the 48 hours before examination. Smokers were asked to be abstinent from tobacco for the 8 hours before they met. The participants were fasting, but they were instructed not to restrict fluid intake by drinking two to three glasses of water before their arrival at the clinical research unit. If the person had an acute illness on arrival, the examination was rescheduled.
Fasting plasma samples were obtained for analyses of creatinine, cystatin C, triglycerides, total cholesterol, HDL cholesterol, and LDL cholesterol. These analyses were performed on the same day at our laboratory at the University Hospital of North Norway.
Five milliliters of iohexol (Omnipaque 300 mg I/ml) was administered through a Teflon catheter placed in an antecubital vein. The syringe was weighed before and after administration. The catheter was flushed with 30 ml of isotonic saline. The sample for iohexol concentration measurement was drawn through the same catheter. After injection of the iohexol, the participants were given a light breakfast and allowed to walk about until it was time to obtain the blood sample for measuring the iohexol concentration. The optimal time for sampling was calculated by Jacobsson's method based on GFR estimated from plasma creatinine measured previously in Tromsø 6.26 The exact time in minutes from injection to sampling was measured with a separate stopwatch for each person.
The serum iohexol concentration was measured by HPLC, as described previously by Niellson-Ehle and Grubb.27 The interassay coefficient of variation (CV) for the iohexol analysis with HPLC during the study period was 3.0%. External quality control was provided by Equalis (Equalis AB, Uppsala, Sweden).
The GFR was calculated using the formula described by Jacobsson.26 Extracellular volume was estimated by Graneus' equation.28 Extrarenal iohexol clearance was ignored in accordance with the practice of other authors. GFR was normalized to 1.73 m2 body surface area, which was estimated using Dubois' equation.29
Plasma creatinine analyses were performed with an enzymatic method that has been standardized against isotope dilution mass spectroscopy (CREA Plus; Roche Diagnostics, Mannheim, Germany). Interassay CV for creatinine in the study period was 2.3%. Cystatin C was measured with a particle-enhanced turbidimetric immunoassay using reagents from Gentian (Moss, Norway) on a Modular E analyzer (Roche Diagnostics). Interassay CV for cystatin C was 3.1%, which was the same as reported for this assay by Delanaye et al. and similar to their results for the Siemens/Dade-Behring nephelometric immunoassay.30 Cholesterol, HDL, and LDL were analyzed using an enzymatic colorimetric method, and plasma triglycerides were analyzed with a colorimetric method.
BP was measured in a seated position after 2 minutes of resting using an automatic device (model UA 799; A&D). BP was measured three times with 1 minute between measurements. The average of the second and third measurements was used in the analyses. Anthropometric measures were obtained by trained personnel. BMI was calculated as body weight in kilograms divided by the square of height measured in meters.
The investigated creatinine-based equations in this study were the recalibrated four-variable MDRD equation and the CKD-EPI equation.31,32 The equation used for estimation of GFR based on cystatin C was developed by Rule et al.33 (Table 6). A previous validation found bias <3.0 ml/min per 1.73 m2 for all these three equations in the RENIS-T6 cohort.34
Table 6.
Equations for estimating GFR
| Rule | 66.8 × cystatin C−1.30 |
|---|---|
| MDRD | 175 × Scr−1.154 × age−0.203 × 0.742 [if female] × 1.272[if black] |
| CKD-EPI | 141 × min(Scr/k, 1)<101> × max(Scr/k, 1)−1.209 × 0.993age × 1.018[if female] × 1.159[if black] |
Scr is serum creatinine, k is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/k, and max indicates the maximum of Scr/k.
The following covariates were obtained from the questionnaire. Smoking status was divided into current smokers or nonsmokers (former smokers were included in the group of nonsmokers). They were registered with a family history of cardiovascular disease if a first-degree relative had had MI, angina pectoris, cerebral stroke, and/or cerebral hemorrhage. Family history of early MI was defined as a first-degree relative with MI before the age of 60 years. Physically active participants were defined as those performing hard physical activity for >1 h/wk (with prominent perspiration or breathlessness) and/or light physical activity for >3 h/wk (without prominent perspiration or breathlessness). Physical activity during working hours was not included in the analysis.
Statistical Analysis
The participants were divided into gender-specific quintiles for mGFR, and differences across the quintiles for the cardiovascular risk factors were analyzed with analysis of covariance for the continuous variables and logistic regression for the dichotomous variables. The analyses were adjusted for age and current use of angiotensin converting enzyme inhibitors or angiotensin receptor blockers. Analyses of serum lipids were also adjusted for lipid-lowering medication. Linear and quadratic trends across the quintiles were tested.
In multiple linear regression analyses, the association between mGFR as a dependent variable and cardiovascular risk factors as independent variables was explored. Each risk factor was first examined separately in a model adjusting only for gender, age, and the use of angiotensin converting enzyme inhibitors or angiotensin receptor blockers and then in a model adjusting for all of the other investigated risk factors as well. Systolic BP was not included in the full model because of colinearity with diastolic BP. The regression coefficients for continuous independent variables were given per SD of the variable. Interactions between gender and all of the other independent variables were tested in the full model. Possible nonlinear relationships were explored with generalized additive models using smoothing with cubic splines.35
The same analyses were performed for eGFR as outlined above for mGFR, but adjustment for mGFR was added to the models to study possible non–GFR-related effects. In addition, the fully adjusted models were analyzed with errors-in-variables regression assuming reduced reliability for mGFR.36 Reliability was estimated as 1 − (noise variance/total variance). With noise variance calculated from the within-subject CV of 5.5% found by others in repeated measurements of plasma iohexol clearance and total variance set at the population variance of mGFR in the RENIS-T6 cohort, the reliability of mGFR was estimated at 0.87.37,38 to allow for the possibility of a higher within-subject CV in our study, we performed the errors-in-variables regression analyses with a mGFR reliability set at 0.70.
Based on the Framingham risk score, the 10-year risk for coronary heart disease was estimated. The Framingham risk score includes age, gender, BP, total serum cholesterol, HDL cholesterol, smoking status, diabetes, and electrocardiogram-left ventricular hypertrophy as predictors.39 Information about electrocardiogram-left ventricular hypertrophy was not available for this analysis, and we set all participants as having no left ventricular hypertrophy as specified in the risk score algorithm.39 All participants were set as not having diabetes because diabetics were excluded from the study.
P < 0.05 was considered statistically significant. The statistical analyses were run using SPSS software version 16.0 (SPSS, Chicago, IL) for Windows. Generalized additive models were analyzed using PROC GAM in SAS version 9.2. (SAS Institute, Cary, NC) and errors-in-variables regression using STATA 11.0 (StataCorp, College Station, TX).
This study was approved by the Norwegian Data Inspectorate and the Regional Ethics Committee of North Norway. All subjects gave written consent.
DISCLOSURES
None.
Acknowledgments
We thank Britt-Ann Winther Eilertsen, Bjørg Skog Høgset, Saskia van Heusden, and the rest of the staff at the Clinical Resarch Unit (University Hospital of North Norway) for performing the study; Harald Strand and the staff at the Department of Medical Biochemistry (University Hospital of North Norway) for HPLC analyses of iohexol; Inger Sperstad and Ingrid Dorthea Sandstad (Clinical Research Centre, University Hospital of North Norway) for database support; and Tom Wilsgaard, Sriharan Sivasingarajah, and Kurt Jøran Nyland (Institute of Community Medicine, University of Tromsø) for identifying eligible subjects from the Tromsø 6 cohort.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
See related editorial, “Cystatin C Is More than GFR, and This May Be a Good Thing,” on pages 795–797.
REFERENCES
- 1. Schiffrin EL, Lipman ML, Mann JFE: Chronic kidney disease: Effects on the cardiovascular system. Circulation 116: 85–97, 2007 [DOI] [PubMed] [Google Scholar]
- 2. Astor BC, Levey AS, Stevens LA, Van Lente F, Selvin E, Coresh J: Method of glomerular filtration rate estimation affects prediction of mortality risk. J Am Soc Nephrol 20: 2214–2222, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Manjunath G, Tighiouart H, Ibrahim H, MacLeod B, Salem DN, Griffith JL, Coresh J, Levey AS, Sarnak MJ: Level of kidney function as a risk factor for atherosclerotic cardiovascular outcomes in the community. J Am Coll Cardiol 41: 47–55, 2003 [DOI] [PubMed] [Google Scholar]
- 4. Van Biesen W, De Bacquer D, Verbeke F, Delanghe J, Lameire N, Vanholder R: The glomerular filtration rate in an apparently healthy population and its relation with cardiovascular mortality during 10 years. Eur Heart J 28: 478–483, 2007 [DOI] [PubMed] [Google Scholar]
- 5. Culleton BF, Larson MG, Wilson PWF, Evans JC, Parfrey PS, Levy D: Cardiovascular disease and mortality in a community-based cohort with mild renal insufficiency. Kidney Int 56: 2214–2219, 1999 [DOI] [PubMed] [Google Scholar]
- 6. Di Angelantonio E, Danesh J, Eiriksdottir G, Gudnason V: Renal function and risk of coronary heart disease in general populations: New prospective study and systematic review. PLoS Med 4: e270, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Garg AX, Clark WF, Haynes RB, House AA: Moderate renal insufficiency and the risk of cardiovascular mortality: Results from the NHANES I. Kidney Int 61: 1486–1494, 2002 [DOI] [PubMed] [Google Scholar]
- 8. Ix JH, Shlipak MG, Chertow GM, Whooley MA: Association of cystatin C with mortality, cardiovascular events, and incident heart failure among persons with coronary heart disease: Data From the Heart and Soul Study. Circulation 115: 173–179, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Koenig W, Twardella D, Brenner H, Rothenbacher D: Plasma concentrations of cystatin C in patients with coronary heart disease and risk for secondary cardiovascular events: More than simply a marker of glomerular filtration rate. Clin Chem 51: 321–327, 2005 [DOI] [PubMed] [Google Scholar]
- 10. Menon V, Shlipak MG, Wang X, Coresh J, Greene T, Stevens L, Kusek JW, Beck GJ, Collins AJ, Levey AS, Sarnak MJ: Cystatin C as a risk factor for outcomes in chronic kidney disease. Ann Intern Med 147: 19–27, 2007 [DOI] [PubMed] [Google Scholar]
- 11. Sarnak MJ, Katz R, Stehman-Breen CO, Fried LF, Jenny NS, Psaty BM, Newman AB, Siscovick D, Shlipak MG, the Cardiovascular Health Study: Cystatin C: Concentration as a risk factor for heart failure in older adults. Ann Intern Med 142: 497–505, 2005 [DOI] [PubMed] [Google Scholar]
- 12. Shlipak MG, Sarnak MJ, Katz R, Fried LF, Seliger SL, Newman AB, Siscovick DS, Stehman-Breen C: Cystatin C and the risk of death and cardiovascular events among elderly Persons. N Engl J Med 352: 2049–2060, 2005 [DOI] [PubMed] [Google Scholar]
- 13. Shlipak MG, Katz R, Sarnak MJ, Fried LF, Newman AB, Stehman-Breen C, Seliger SL, Kestenbaum B, Psaty B, Tracy RP, Siscovick DS: Cystatin C and prognosis for cardiovascular and kidney outcomes in elderly persons without chronic kidney disease. Ann Intern Med 145: 237–246, 2006 [DOI] [PubMed] [Google Scholar]
- 14. Taglieri N, Koenig W, Kaski JC: Cystatin C and cardiovascular risk. Clin Chem 55: 1932–1943, 2009 [DOI] [PubMed] [Google Scholar]
- 15. Knight EL, Verhave JC, Spiegelman D, Hillege HL, De Zeeuw D, Curhan GC, de Jong PE: Factors influencing serum cystatin C levels other than renal function and the impact on renal function measurement. Kidney Int 65: 1416–1421, 2004 [DOI] [PubMed] [Google Scholar]
- 16. Stevens LA, Schmid CH, Greene T, Li L, Beck GJ, Joffe MM, Froissart M, Kusek JW, Zhang Y, Coresh J, Levey AS: Factors other than glomerular filtration rate affect serum cystatin C levels. Kidney Int 75: 652–660, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Desbien AM, Chonchol M, Gnahn H, Sander D: Kidney function and progression of carotid intima-media thickness in a community study. Am J Kidney Dis 51: 584–593, 2008 [DOI] [PubMed] [Google Scholar]
- 18. Nitsch D, Dietrich DF, von Eckardstein A, Gaspoz JM, Downs SH, Leuenberger P, Tschopp JM, Brandli O, Keller R, Gerbase MW, Probst-Hensch NM, Stutz EZ, Ackermann-Liebrich U, the SAPALDIA team: Prevalence of renal impairment and its association with cardiovascular risk factors in a general population: Results of the Swiss SAPALDIA study. Nephrol Dial Transplant 21: 935–944, 2006 [DOI] [PubMed] [Google Scholar]
- 19. Verhave JC, Hillege HL, Burgerhof JGM, Gansevoort RT, Zeeuw Dd, Jong PED: The association between atherosclerotic risk factors and renal function in the general population. Kidney Int 67: 1967–1973, 2005 [DOI] [PubMed] [Google Scholar]
- 20. Ishizaka N, Ishizaka Y, Toda Ei, Shimomura H, Koike K, Seki G, Nagai R, Yamakado M: Association between cigarette smoking and chronic kidney disease in Japanese men. Hypertens Res 31: 485–492, 2008 [DOI] [PubMed] [Google Scholar]
- 21. Pinto-Sietsma SJ, Mulder J, Janssen WMT, Hillege HL, De Zeeuw D, de Jong PE: Smoking is related to albuminuria and abnormal renal function in nondiabetic persons. Ann Intern Med 133: 585–591, 2000 [DOI] [PubMed] [Google Scholar]
- 22. Halimi JM, Giraudeau B, Vol S, Caces E, Nivet H, Lebranchu Y, Tichet J: Effects of current smoking and smoking discontinuation on renal function and proteinuria in the general population. Kidney Int 58: 1285–1292, 2000 [DOI] [PubMed] [Google Scholar]
- 23. Ritz E, Benck U, Franek E, Keller C, Seyfarth M, Clorius J: Effects of smoking on renal hemodynamics in healthy volunteers and in patients with glomerular disease. J Am Soc Nephrol 9: 1798–1804, 1998 [DOI] [PubMed] [Google Scholar]
- 24. Stevens LA, Levey AS: Measured GFR as a confirmatory test for estimated GFR. J Am Soc Nephrol 20: 2305–2313, 2009 [DOI] [PubMed] [Google Scholar]
- 25. Bird NJ, Peters C, Michell AR, Peters AM: Comparison of GFR measurements assessed from single versus multiple samples. Am J Kidney Dis 54: 278–288, 2009 [DOI] [PubMed] [Google Scholar]
- 26. Jacobsson L: A method for the calculation of renal clearance based on a single plasma sample. Clin Physiol 3: 297–305, 1983 [DOI] [PubMed] [Google Scholar]
- 27. Nilsson-Ehle P: Iohexol clearance for the determination of glomerular filtration rate: 15 years' experience in clinical practice. eJIFCC 13(2): http://www.ifcc.org/index.asp?cat=Publications&scat=eJIFCC_&rif=6&dove=1 Accessed January 6, 2011 [PMC free article] [PubMed] [Google Scholar]
- 28. Boijsen M, Jacobsson L, Tylen U: Glomerular filtration rate estimated from a single plasma sample after contrast-enhanced radiological examinations. Clin Physiol 8: 309–316, 1988 [DOI] [PubMed] [Google Scholar]
- 29. Du Bois D, Du Bois EF: The measurement of the surface area of man. Arch Intern Med 15: 868–881, 1915 [Google Scholar]
- 30. Delanaye P, Pieroni L, Abshoff C, Lutteri L, Chapelle JP, Krzesinski JM, Hainque B, Cavalier E: Analytical study of three cystatin C assays and their impact on cystatin C-based GFR-prediction equations. Clin Chim Acta 398: 118–124, 2008 [DOI] [PubMed] [Google Scholar]
- 31. Levey AS, Corsh J, Greene T: Using standardized serum creatinine values in the modification of diet in renal disease study equation for estimating glomerular filtration rate. Ann Intern Med 145: 247–254, 2006 [DOI] [PubMed] [Google Scholar]
- 32. Levey AS, Stevens LA, Schmid CH, Zhang Y, Castro AF, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J: A new equation to estimate glomerular filtration rate. Ann Intern Med 150: 604–612, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rule AD, Bergstralh EJ, Slezak JM, Bergert J, Larson TS: Glomerular filtration rate estimated by cystatin C among different clinical presentations. Kidney Int 69: 399–405, 2006 [DOI] [PubMed] [Google Scholar]
- 34. Eriksen BO, Mathisen UD, Melsom T, Ingebretsen OC, Jenssen TG, Njolstad I, Solbu MD, Toft I: Cystatin C is not a better estimator of GFR than plasma creatinine in the general population. Kidney Int 78: 1305–1311, 2010 [DOI] [PubMed] [Google Scholar]
- 35. Hastie TJ, Tibshirmai RJ: Generalized Additive Models, Boca Raton, Chapman & Hall/CRC, 1990 [Google Scholar]
- 36. Draper NR, Smith H: Applied Regression Analysis, 3rd. ed, New York, Wiley, 1998 [Google Scholar]
- 37. Gaspari F, Perico N, Matalone M, Signorini O, Azzollini N, Mister M, Remuzzi G: Precision of plasma clearance of iohexol for estimation of GFR in patients with renal disease. J Am Soc Nephrol 9: 310–313, 1998 [DOI] [PubMed] [Google Scholar]
- 38. Tan GD, Lewis AV, James TJ, Altmann P, Taylor RP, Levy JC: Clinical usefulness of cystatin C for the estimation of glomerular filtration rate in type 1 diabetes: reproducibility and accuracy compared with standard measures and iohexol clearance. Diabetes Care 25: 2004–2009, 2002 [DOI] [PubMed] [Google Scholar]
- 39. Anderson KM, Odell PM, Wilson PWF, Kannel WB: Cardiovascular disease risk profiles. Am Heart J 121: 293–298, 1991 [DOI] [PubMed] [Google Scholar]