Abstract
Objective
To validate a questionnaire focused on REM sleep behavior disorder (RBD) among participants in an aging and dementia cohort.
Background
RBD is a parasomnia that can develop in otherwise neurologically-normal adults as well as in those with a neurodegenerative disease. Confirmation of RBD requires polysomnography (PSG). A simple screening measure for RBD would be desirable for clinical and research purposes.
Methods
We had previously developed the Mayo Sleep Questionnaire (MSQ), a 16 item measure, to screen for the presence of RBD and other sleep disorders. We assessed the validity of the MSQ by comparing the responses of patients’ bed partners with the findings on PSG. All subjects recruited in the Mayo Alzheimer’s Disease Research Center at Mayo Clinic Rochester and Mayo Clinic Jacksonville from 1/00 to 7/08 who had also undergone a PSG were the focus of this analysis.
Results
The study sample was comprised of 176 subjects [150 male; median age 71 years (range 39–90)], with the following clinical diagnoses: normal (n=8), mild cognitive impairment (n=44), Alzheimer’s disease (n=23), dementia with Lewy bodies (n=74), as well as other dementia and/or parkinsonian syndromes (n=27). The core question on recurrent dream enactment behavior yielded a sensitivity (SN) of 98% and specificity (SP) of 74% for the diagnosis of RBD. The profile of responses on four additional subquestions on RBD and one on obstructive sleep apnea improved specificity.
Conclusions
These data suggest that among aged subjects with cognitive impairment and/or parkinsonism, the MSQ has adequate SN and SP for the diagnosis of RBD. The utility of this scale in other patient populations will require further study.
Keywords: sleep disorders, parasomnias, dementia, Alzheimer’s disease, dementia with Lewy bodies, parkinsonism
1. INTRODUCTION
Several sleep disorders associated with neurologic disease can negatively impact mood, cognitive functioning, and quality of life. Such sleep disorders include rapid eye movement (REM) sleep behavior disorder (RBD), periodic limb movements during sleep (PLMS), restless legs syndrome (RLS), sleepwalking (SW), obstructive sleep apnea (OSA), sleep related leg cramps (SRLC), and insomnia. These disorders are treatable and such treatment often results in improved quality of life and improved management of the coexisting neurologic disorder. Hence there is an increasing interest in identifying and treating patients with these conditions.
Current practice in the assessment of sleep disorders involves the clinical interview of patients and their bed partners, physical examination, and in those suspected to have certain sleep disorders, polysomnography (PSG). The history and examination usually require 30–60 minutes for a sleep medicine clinician to complete. PSG is clearly necessary for establishing the diagnosis of RBD, OSA, and PLMS, but the procedure requires appropriate monitoring equipment, including time synchronized video recordings, specially trained technologists, bed availability in a sleep laboratory, and clinicians who can interpret the data. The procedure is costly (>$1000 per study at most centers for a clinical PSG), especially for patients with limited insurance coverage. Subjects must be willing and able to sleep in a sleep laboratory and undergo monitoring. Some patients with coexisting neurologic disorders are too cognitively or physically impaired to tolerate and undergo an adequate study, are too uncooperative to permit all monitoring equipment to remain in place, are at risk for falls during the night, or are institutionalized. While home monitoring may be appropriate for the diagnosis of uncomplicated OSA in some patients, RBD and PLMS cannot be accurately assessed in this way. For clinical and especially research purposes, it would be desirable to screen for the presence of key sleep disorders, using a validated measure, by querying the bed partners of patients who are cognitively impaired, severely disabled or deceased, with PSG remaining as the gold standard for confirming their presence and determining their severity. Seeing how impractical it is to perform PSGs in large numbers of subjects in epidemiologic sleep disorder studies, using a simple, short, reliable, and accurate measure to screen for the presence of various sleep disorders would be highly valuable.
These issues led us to develop the Mayo Sleep Questionnaire (MSQ) in 2001, which is a 16-item measure that poses questions about RBD, PLMS, RLS, SW, OSA, and SRLC. The primary goal of this measure was to assess RBD with adequate sensitivity and specificity. There were two versions initially developed—one completed by the patient and one completed by his/her bed partner/informant. Our early pilot data using the MSQ through 2002 [1, 2], in which responses on the MSQ were compared with the findings on PSG, indicated that the sensitivity and specificity were higher for the bed partner/informant version compared to the patient version, regardless of whether the patient was cognitively impaired or not. Since 2002, we have therefore only used the bed partner/informant version of the MSQ. The MSQ was designed to be used for clinical and research purposes in a variety of settings, such as a Behavioral Neurology Clinic (which involves patients with cognitive/behavioral changes), a Movement Disorder Clinic (which involves patients with parkinsonism and other movement disorders), a Sleep Disorders Center, a research program involving community-dwelling nondemented aged individuals, and a research program involving individuals with normal cognition, mild cognitive impairment, dementia, or parkinsonism. The pilot data were collected on individuals evaluated in a Behavioral Neurology Clinic and Sleep Disorders Center [1, 2]. In this paper, we report validation data on the MSQ compared to PSG focused on RBD. Validation of the MSQ compared to PSG-confirmed data regarding PLMS and OSA, and also MSQ data compared to established clinical diagnostic criteria for RLS, SW, and SRLC, are presented as supplemental data. Because of the relevance of RBD pertaining to aging and neurodegenerative disease, the sample includes normal control subjects and patients with cognitive impairment and/or parkinsonism who are participants in the Mayo Alzheimer’s Disease Research Center at Mayo Clinic Rochester or Mayo Clinic Jacksonville.
2. DESIGN/METHODS
2.1 Mayo Sleep Questionnaire
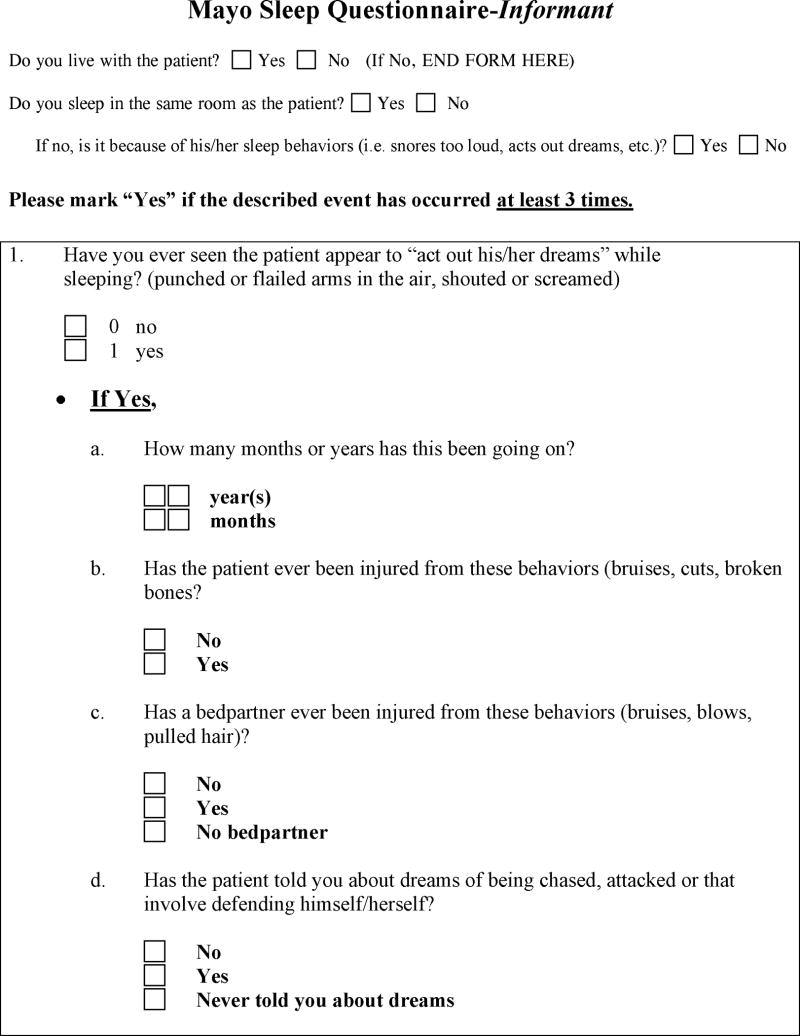
The MSQ is a concise 16 question scale (some questions are ignored depending if certain questions are answered affirmatively or not) that screens for the presence of RBD, PLMs, RLS, SW, OSA, and SRLC. The MSQ was copyrighted in 2009 by the Mayo Foundation for Medical Education and Research. As stated on the measure, permission is granted for non-commercial use in the context of patient care and research provided that no fee is charged. It is therefore available to the public at no expense. It can be downloaded for free at this website: http://www.mayoclinic.org/pdfs/MSQ-copyrightfinal.pdf. The data presented herein refer to the primary question on RBD (Question 1), and if answered affirmatively, the subquestions are asked (subquestions 1b–1e) as shown below:
-
Have you ever seen the patient appear to “act out his/her dreams” while sleeping? (punched or flailed arms in the air, shouted or screamed).
If yes,
-
How many months or years has this been going on?
(data on this subquestion were not analyzed in this analysis)
Has the patient ever been injured from these behaviors (bruises, cuts, broken bones)?
Has a bed partner ever been injured from these behaviors (bruises, blows, pulled hair)?
Has the patient told you about dreams of being chased, attacked or that involve defending himself/herself?
If the patient woke up and told you about a dream, did the details of the dream match the movements made while sleeping?
-
The MSQ is provided to the bed partner by a desk attendant or study coordinator, who is asked to complete the questionnaire in a quiet room prior to meeting with a clinician or investigator; it is usually completed within two minutes. Data on whether the informant lives in the same residence as the patient and whether he/she sleeps in the same room are recorded. If the informant sleeps elsewhere, the reason for sleeping elsewhere is recorded. The MSQ data are considered valid when the informant sleeps in the same room as the patient or has previously slept with the patient for years but currently sleeps in another room of the residence due to the patient’s disruptive snoring or acting out dream behavior (and therefore has knowledge on key factors assessed by the measure). We typically use the MSQ in conjunction with the Epworth Sleepiness Scale (ESS), which measures an individual’s subjective sense of daytime sleepiness [3]. In patients with cognitive impairment and/or parkinsonism, a more accurate reflection of an individual’s chance of dozing is likely better assessed by an informant who is typically also the patient’s bed partner, and thus we request that bed partners complete the ESS based on their perspective of the patient’s tendency to doze.
2.2 Polysomnography
All PSG studies used the following montage according to established guidelines [4]: two alternate electro-oculogram (EOG) derivations, three EEG derivations (Fz-Cz, Cz-Oz, C4-A1), electrocardiogram (ECG), chin and at least two upper and lower limb surface electromyogram (EMG) derivations (right and left anterior tibial, and right and left extensor digitorum communis), oronasal airflow by thermocouple and nasal pressure measurements, sonogram, oxyhemoglobin saturation, and chest and abdomen inductance plethysmography. For those in whom RBD was being assessed, all PSG data were recorded in synchrony with continuous video monitoring. Scoring of sleep stages followed standard guidelines [4, 5].
All PSGs were reviewed by American Board of Sleep Medicine-certified sleep specialists blinded to the responses on the MSQ. Because many of the patients had undergone PSG for clinical purposes—particularly for OSA and not RBD—and therefore scrutiny of EMG tone during REM sleep had not been described in the formal report, all such records were re-reviewed by a single clinician (BFB) blinded to the clinical and MSQ data.
For most patients who undergo PSG, the determination of whether RSWA is present or not is obvious and straight-forward. A significant minority of cases, however, have some degree of increased EMG tone during tonic and/or phasic REM sleep, and since there is no established cut-off of what degree of RSWA is “within normal limits” versus “definitely abnormal” based on data or consensus [6–8], we used the following system for classifying PSG records: 0=clearly normal loss of EMG tone during REM sleep, 1=clearly abnormal increase in EMG tone during REM sleep, and 2=equivocal increase in EMG tone during REM sleep; examples of PSG fragments reflecting these patterns are shown in the Figure.
Figure.
Examples of polysomnographic fragments (30 second epochs) of REM sleep in four different patients, showing definitely normal EMG atonia (A), definitely increased EMG tone and hence definite REM sleep without atonia (B), and equivocally increased EMG tone (C and D). Note the low amplitude EMG activity in C which persists through most of this epoch, and is present in most but not all epochs of REM sleep; the patient has no clinical findings suggesting motor neuron disease or a peripheral neuropathy. The sample in D shows an approximately 10 second fragment during phasic REM with brief bursts of EMG activity (left of double vertical lines), and an approximately 20 second epoch during a REM sleep episode later in the night with more obvious and persistent EMG activity during phasic and tonic REM (right of double vertical lines). Neither patient in C or D exhibited any apparent motor activity on the synchronous video at any time during REM sleep. Note that in cases B, C and D, the equivocal or definitely increased EMG activity was present on the leg derivation, but atonia was normal in each case in the submentalis derivation.
2.3 Definitions
The following definitions were used; these are in accordance with those published in the International Classification of Sleep Disorders – 2nd Edition (ICSD-2) [9] or American Academy of Sleep Medicine Manual [4]. The latter scoring system and definitions were used for PSGs performed after December 2007 as this is when the new system and definitions began being used at our institution.
REM sleep without atonia (RSWA): increased electromyographic (EMG) tone during REM sleep as judged by the sleep clinician certified by the American Board of Sleep Medicine, as described above.
Apparent dream enactment behavior (DEB): obvious motor activity such as punching, grasping, kicking, running in bed, etc., as seen by bed partners in the home setting or by PSG technicians and sleep specialists when observing the patient during PSG.
RBD: a clinical history of recurrent dream enactment behavior plus RSWA on PSG, or the combination of obvious complex motor activity recorded on PSG during REM sleep plus RSWA, in the absence of epileptiform activity in accordance with ICDS-2 guidelines [9]
Apnea: cessation of airflow for 10 seconds or more
Hypopnea: at least 30% reduction in airflow lasting ≥10 seconds associated with ≥ 4% drop in oxygen saturation.
Apnea/hypopnea index (AHI): the number of apneas and hypopneas per hour divided by total sleep time.
Obstructive sleep apnea (OSA): the presence of five or more apnea or hypopnea events per hour of sleep
2.4 Subjects
All subjects enrolled in the Mayo Alzheimer’s Disease Research Center (ADRC) at Mayo Clinic Rochester (MCR) or Mayo Clinic Jacksonville (MCJ) from January 1, 2000, to July 30, 2008, who underwent PSG and whose bed partner/informant completed the MSQ were included in the study. Almost all subjects have cognitive impairment and/or parkinsonism and carry one of the following clinical diagnoses based on established criteria: mild cognitive impairment (MCI) [10], clinically probable Alzheimer’s disease (AD) [11], clinically probable dementia with Lewy bodies (DLB) [12], behavioral variant frontotemporal dementia (FTD) [13], progressive nonfluent aphasia syndrome (PNFA) [13], semantic dementia (SD) [13], corticobasal syndrome (CBS) [14], progressive supranuclear palsy (PSP) [15], multiple system atrophy (MSA) [16], or posterior cortical atrophy (PCA) [17]. A minority of subjects was recruited as normal controls; these subjects had no cognitive complaints, their informants had no cognitive concerns about them, they had no other neurologic or psychiatric symptoms or features, and they performed within normal limits on a mental status examination and a comprehensive neuropsychological battery. Subjects recruited into the Mayo ADRC are usually residents of the Midwest (at MCR) or Southeast (at MCJ) regions of the United States and most are Caucasian. The majority of the subjects had undergone PSG for clinical purposes, while some had undergone PSG as part of a research study (NIA AG15866, Alzheimer’s Association IIRG-05-14560).
2.5 Validation and Data Analyses
In order to validate the measure in the manner with which it would likely be used for clinical and research purposes, we attempted to have bed partners complete the MSQ prior to any face-to-face interaction with a clinician. Each subject then underwent a comprehensive sleep interview, physical examination, and PSG. There are instances when the patient had already undergone PSG, and the MSQ was completed later (usually weeks or months later). The validation data for both circumstances—MSQ completed prior to PSG and PSG completed prior to MSQ—were analyzed separately, and then together. For those patients whose bed partners completed the MSQ more than once, the assessment closest in time to the PSG, and preferably prior to undergoing the PSG, were used for this analysis.
For the diagnoses of RBD, the PSG finding of RSWA plus a history of recurrent dream enactment behavior was required, and these features were compared to the corresponding MSQ questions. For most patients, the diagnosis is based on the history and presence of RSWA. Infrequently, the diagnosis is made based purely on the PSG, in which RSWA plus apparent dream enactment behaviors are present on the in-lab PSG but not noted at home by the informant. These criteria are in accordance with the ICSD-2 guidelines.
The primary question (Question 1) on the MSQ relating to RBD involves the tendency for the patient to appear to be acting out dreams. A “yes” response for question 1 regardless of the responses for question 1, items b-e, was compared to PSG. Responses on question 1, items be, were also compared to PSG to determine if any or all provided additional diagnostic information. Since a history of recurrent dream enactment behavior plus RSWA on PSG establishes the diagnosis of RBD [9], a “yes” response to question 1 was considered a true positive when a history of recurrent dream enactment behavior based on the patient’s history was associated with definite RSWA, and a “no” response to this question was considered a true negative when the clinician recorded an absence of recurrent dream enactment behavior and there was definitely normal EMG atonia during REM sleep. A “yes” response to question 1 associated with definitely normal EMG atonia during REM sleep was considered a false positive response. The interpretation is more complicated when a patient has definite RSWA in the absence of a history of recurrent dream enactment behavior, as there is insufficient longitudinal data on such cases to know if this represents “subclinical RBD” or simply a benign PSG finding. Therefore, in accordance with published criteria [9], true RBD was considered present only if both RSWA plus apparent dream enactment behavior was apparent on the PSG; such findings on PSG associated with the clinician’s recorded absence of recurrent dream enactment behavior was considered a false negative response.
Because a significant minority of cases has an equivocal increase in EMG tone during REM sleep, and the interpretation of such cases is unclear, three analyses were undertaken for the RBD diagnosis. Analysis 1 involved only those cases which had definitely normal EMG atonia during REM sleep and definite RSWA on PSG. In analysis 2, the equivocally increased EMG tone cases were considered collectively with the group with RSWA. In analysis 3, the equivocally increased EMG tone cases were considered collectively with the group with normal EMG atonia.
2.6 Statistical Analyses
The sensitivity (SN) and specificity (SP) and associated 95% confidence intervals (95% CI) were calculated for each question. Secondary analyses were performed to test for potential differences in SN and SP based on the timing of MSQ in relation to the PSG (MSQ before PSG versus PSG before MSQ), and the site the patient was evaluated (MCR versus MCJ). Additional comparisons using Chi-square or t-test analyses were also carried out to determine the optimum combination of responses that could differentiate true positives from false positives, and true negatives from false negatives. The data and interpretation relating to RBD are presented below; the methodology, findings and discussion relating to the other sleep disorders assessed by the MSQ are presented in the Supplemental text and data, Supplemental tables, and Supplemental figure.
2.7 Ethics
All procedures and analyses have been approved by the Mayo Foundation Institutional Review Board.
3. RESULTS
3.1 Demographic Features and Clinical Diagnoses
The study sample was comprised of 176 subjects, with the core demographic features and clinical diagnoses shown in Table 1. Most subjects were male, and most were in the 60 – 80-year-old age range. All subjects had bed partners who completed the MSQ, of whom 96% were spouses and the remainder were unwed companions (opposite sex in seven, same sex in one). Eight (4%) were normal controls; all others had some degree of cognitive impairment or dementia, with the diagnoses of MCI, AD, and DLB representing the majority of cases (n=141 or 80%). Parkinsonism was present in 85 cases (48%), with 70 diagnosed with DLB, 10 having PD +/− MCI or dementia, and 5 having parkinsonism as part of CBS or PSP.
Table 1.
Demographic and clinical data
| Frequency | |
|---|---|
| Age (years) | |
| <50 | 2 |
| 50–59 | 21 |
| 60–69 | 61 |
| 70–79 | 72 |
| 80–89 | 18 |
| 90+ | 2 |
| Total | 176 |
| Median | 71 years |
| Sex | |
| Male | 150 (85%) |
| Bedpartner | |
| Spouse | 168 (96%) |
| Neurologic diagnosis | |
| Normal | 8 |
| MCI | 44 |
| SD-amnestic | 25 (3 also with PD) |
| MD-amnestic | 8 (2 also with PD) |
| SD-non-amnestic | 9 (2 also with PD) |
| MD-nonamnestic | 4 (1 also with PD) |
| AD | 23 |
| DLB | 74 |
| PDD | 2 |
| FTD | 5 |
| PPA (PNFA or SD) | 5 |
| CBS | 4 |
| PCA | 2 |
| CNS vasculitis | 1 |
| MSA | 1 |
| PSP | 1 |
| Dementia/Cognitive impairment NOS | 4 |
Abbreviations: AD=Alzheimer disease, CBS=corticobasal syndrome, CNS=central nervous system, DLB=dementia with Lewy bodies, FTD=frontotemporal dementia, MCI=mild cognitive impairment (SD=single domain, MD=multiple domain), MSA=multiple system atrophy, NOS=not otherwise specified, PCA=posterior cortical atrophy, PD=Parkinson disease, PDD=Parkinson disease with dementia, PNFA=progressive nonfluent aphasia, PPA=primary progressive aphasia, PSP=progressive supranuclear palsy
3.2 Validation of the RBD Questions
Since 19 subjects failed to attain REM sleep on their PSG, and hence REM sleep could not be scrutinized for assessing EMG tone, a total of 157 subjects had data that could be analyzed. Ten of these 157 subjects had EMG tone considered equivocally increased (rated as a 2), and hence 147 formed the basis for most analyses. Eighty-one (55%) subjects had recurrent dream enactment behavior either by history or on PSG associated with unequivocally increased EMG tone during REM sleep, thereby confirming the diagnosis of RBD.
The core question on recurrent dream enactment behavior yielded a SN of 98% and SP of 74% (Table 2). These values changed minimally when the 10 cases with equivocal EMG tone findings were considered together with the group with normal EMG atonia [rating of 0] (SN 98%, SP 68%) or with the group with clearly abnormal EMG tone [rating of 1] (SN 95%, SP 74%). SN and SP values were also similar regardless of whether the MSQ was completed before (SN 96%, SP 73%) or after (SN 100%, SP 77%) the PSG, and similar regardless of where the subjects were evaluated (Mayo Clinic Rochester: SN 97%, SP 76%; Mayo Clinic Jacksonville: SN 100%, SP 67%).
Table 2.
Sensitivity and specificity of question 1 on the Mayo Sleep Questionnaire for PSG-proven RBD*
| +DEB plus +RSWA | NOT +DEB plus +RSWA | ||||
|---|---|---|---|---|---|
| MSQ Q1 - Yes | 79 | 17 | SN | 98% | [95%CI: 0.91–0.99] |
| MSQ Q1 - No | 2 | 49 | SP | 74% | [95%CI: 0.63–0.84] |
| Total | 81 | 66 |
Abbreviations: 95%CI = 95% confidence interval, +DEB=dream enactment behavior by history and/or PSG is present, EMG=electromyographic, MSQ=Mayo Sleep Questionnaire, PSG=polysomnography, Q1=question one, RBD=rapid eye movement sleep behavior disorder, +RSWA=rapid eye movement sleep without atonia is present, SN=sensitivity, SP=specificity
Caveats:
19 patients did not attain REM sleep on their PSG and thus their data was not included
81 (55% of cohort) met established criteria for the diagnosis of RBD
10 patients had equivocal EMG findings in REM sleep are their data are excluded from this analysis; their data were analyzed separately – see text for elaboration
6 patients had RSWA without a clinical history of DEB nor any DEB present on PSG
2 patients had false negative responses; 1 has non-amnestic MCI and over time was found to have PSG evidence of narcolepsy plus RBD, and the other has Alzheimer’s disease features but no history of DEB
There were 96 (65%) subjects whose response to question 1 was affirmative, of whom 79 (54%) subjects were considered true positive and 17 subjects (11%) whose response were considered false positive. As shown in Table 3, the frequencies of affirmative responses to subquestions 1b, 1c, 1d, and 1e were different between the true positive and false positive groups. The true positive group was also more likely to have affirmative responses to at least 3, as well as all 4, of these 4 subquestions. The two false positive cases who responded affirmatively to 3 of these 4 questions had AHI values of 36 and 7.
Table 3.
Frequency of endorsement of questions/subquestions pertaining to RBD
| MSQ Item | Total (n=147) | +DEB plus +RSWA (True Positives) | NOT +DEB plus +RSWA (False Positives) | p* |
|---|---|---|---|---|
| 1. Act out dreams | 96 (65%) | 79 (82%) | 17 (18%) | <0.05 |
| 1b. Patient injury | 26 (18%) | 25 (96%) | 1 (4%) | <0.05 |
| 1c. Bedpartner injury | 33 (22%) | 30 (91%) | 3 (9%) | <0.05 |
| 1d. Dream content | 69 (47%) | 58 (84%) | 11 (16%) | <0.05 |
| 1e. Actions mimic dream | 60 (41%) | 50 (83%) | 10 (17%) | <0.05 |
| ≥3 of subquestions 1b–1e | 32 (22%) | 30 (94%) | 2 (6%) | <0.05 |
| All 4 of subquestions 1b–1e | 11 (7%) | 11 (100%) | 0 (0%) | <0.05 |
Based on Chi-square comparisons
Abbreviations: + = present, DEB=dream enactment behavior by history and/or PSG, MSQ=Mayo Sleep Questionnaire, RBD=rapid eye movement sleep behavior disorder, RSWA=rapid eye movement sleep without atonia
Additional comparisons between the true positive vs. false positive groups are shown in Table 4. The true positive group was more likely to respond affirmatively to subquestion 1b regarding prior injuries to the subject (only 1 case in the false positive group had an affirmative response to this question, and her AHI was 63 indicating severe OSA). There was a trend for injuries to the bed partner being more frequent in the true positive group, but this was not statistically significant. The true positive group also had a lower frequency of affirmative responses to hypopnea questions regarding snorting/choking, a lower mean apnea/hypopnea index (AHI), and a lower frequency of AHI≥20 than the false positive group.
Table 4.
Comparison between true positive and false positive responders in relation to MSQ and PSG variables
| True Positives | False Positives | Chi/t | p | |
|---|---|---|---|---|
| N=79 | N=17 | |||
| MSQ items | ||||
| 1b. Patient injury | 25 (32%) | 1 (6%) | 4.70 | <0.04 |
| 1c. Bedpartner injury | 30 (38%) | 3 (17%) | 2.56 | ns |
| 5. Snort/choke awake | 30 (38%) | 12 (71%) | 6.05 | <0.02 |
| 6. Stopped breathing | 32 (41%) | 10 (59%) | 1.90 | ns |
| PSG findings | ||||
| Mean AHI | 11.1 (+/−11) | 22.7 (+/−25) | 3.0 | <0.01 |
| AHI ≤ 5 | 33 (42%) | 6 (35%) | 0.24 | ns |
| AHI ≥ 10 | 32 (41%) | 9 (53%) | 0.89 | ns |
| AHI ≥ 20 | 15 (19%) | 7 (41%) | 3.90 | <0.05 |
Abbreviations: AHI=apnea/hypopnea index, MSQ=Mayo Sleep Questionnaire, ns=not
significant, PSG=polysomnography
Six of the subjects had PSG evidence of unequivocally increased EMG tone during REM sleep but no apparent dream enactment behavior on the PSG. In each case the clinician did not record a history of recurrent dream enactment behavior at the time the PSG was performed, indicating that such patients had evidence of RSWA. The clinical diagnoses at the time of PSG were DLB in 2, AD in 1, MCI in 1, PD in 1, and dementia not otherwise specified in 1. Recurrent dream enactment behavior evolved after the PSG in 4 of these subjects. One of these cases was the AD patient, who develop parkinsonism and visual hallucinations within one year after the onset of recurrent dream enactment behavior, leading to an updated diagnosis of RBD associated with mixed AD/DLB. The MCI case developed recurrent dream enactment behavior along with visual hallucinations and fluctuations, leading to an updated diagnosis of RBD associated with DLB, and she subsequently had Lewy body disease confirmed at autopsy.
4. DISCUSSION
Features of a useful screening test include high sensitivity and adequate specificity, good safety, low cost, easy administration, minimal inconvenience or discomfort upon administration, and acceptability of patients and clinicians. In this patient population, the MSQ satisfies all these criteria for RBD.
4.1 Overview of findings
An affirmative response to question 1 is almost 100% sensitive for RBD, and the specificity is adequate at 74%. False positives tended to occur in those with historical and PSG features of OSA, which is consistent with the known phenomenon of apparent dream enactment behavior in those with untreated OSA [18]. Yet based on these data, the history of injuries to the patient as reflected on subquestion 1b, a history of most core features of RBD as reflected on subquestions 1b–1e, or an absence of OSA features as reflected on question 5, adequately differentiates those with true RBD from those without. If a goal is to use this tool to screen for RBD, then question 1 alone is a highly sensitive means to do this. If a goal is to use this tool to differentiate RBD from OSA, the profile of responses on subquestions 1b–1e and question 5 perform well, although clearly PSG is the optimal method to make this determination. These findings suggest that among older individuals with coexisting cognitive impairment +/− parkinsonism due to an underlying neurodegenerative disorder, the MSQ is an excellent screening tool for the presence or absence of RBD.
4.2 Utility as a clinical tool
Among patients undergoing evaluation for a slowly progressive disorder affecting cognition and behavior likely on a neurodegenerative basis, a screening tool for the presence or absence of RBD would be diagnostically useful. While RBD is not uniquely associated with any particular neurodegenerative disorder, it occurs far more frequently in the synucleinopathies (e.g., dementia with Lewy bodies and Parkinson disease with dementia) than in the nonsynucleinopathies (e.g., Alzheimer disease, Huntington disease, and the frontotemporal lobar degeneration spectrum disorders due to amyloid, tau, or TDP-43 protein dysfunction) [19–21]. Furthermore, in those with an evolving neurodegenerative disorder, RBD almost always precedes the cognitive and motor aspects of the disorder by years or even decades, and the presence of RBD has been shown by many authors to have diagnostic relevance for those with cognitive impairment and/or parkinsonism [21–26]. RBD is considered a suggestive feature for the clinical diagnosis of DLB [12], and the presence of RBD in dementia even without the other cardinal features of DLB strongly suggests underlying LBD [27]. The majority of patients with dementia obviously have underlying AD, but in those with atypical or frank non-AD features, the presence of RBD would strongly implicate evolving LBD rather than atypical AD or an FTLD-spectrum disorder. The dramatic improvement in some DLB patients with cholinesterase inhibitor therapy, and dramatic deterioration in many patients with conventional neuroleptic drugs directed toward behavioral/psychotic features, underscore the need for early and accurate diagnosis [12]. While it could be debated whether a PSG should be performed in all patients who screen positive on the MSQ for RBD to substantiate the diagnosis of DLB, those who are deemed appropriate (i.e., significant risk for injury, need to differentiate RBD from DEB associated with OSA) could undergo PSG, and in those in whom a PSG cannot be performed or justified, at least the suspicion of RBD (i.e., be labeled “probable RBD”) would make the clinician consider LBD as a diagnostic consideration in a patient’s cognitive decline.
Confidence in determining the evolving underlying neurodegenerative disorder in those with MCI is even more challenging. One classification system which is gaining utility in the syndrome of MCI involves categorizing MCI subjects into one of four subtypes, in which those with prominent memory impairment (e.g., single-domain MCI with amnesia or MCI-A, and multiple-domain MCI with an amnestic component or MD-MCI-A) likely but not always have underlying AD pathology, and those without significant memory impairment (e.g., single-domain MCI without amnesia or SD-MCI-NA, and multiple-domain MCI without amnesia or MD-MCI-NA) likely have a non-AD disorder such as LBD or FTLD [28, 29]. Recent clinicopathologic analyses have led to the hypothesis that those with RBD and MCI, regardless of the MCI subtype, very likely reflect evolving LBD [21, 23, 25, 26, 30]. More clinicopathologic analyses will be needed to substantiate this hypothesis, but these early analyses substantiate the need to assess for RBD in the setting of MCI; the MSQ could facilitate this assessment.
Among patients undergoing evaluation for a slowly progressive parkinsonian disorder likely on a neurodegenerative basis, a screening tool for the presence or absence of RBD would also be diagnostically useful. Among the disorders that primarily manifest as parkinsonism, since RBD is far more common in the synucleinopathies (e.g., PD and MSA) than non-synucleinopathies (e.g., PSP, CBD, and FTDP associated with mutations in MAPT and PGRN) [19], a screening tool for the presence/absence of RBD would be clinically useful.
4.3 Utility as a research tool
The potential of the MSQ as a research tool is promising, and only a few examples will be presented here. Due to the ease of use as a screening tool, and high SN and adequate SP as demonstrated by these analyses, the MSQ could be incorporated into the standard assessment of participants in any dementia research program, with a positive screen for RBD increasing the clinician’s suspicion for DLB if not already having been diagnosed by standard clinical and PSG measures. Clinical investigators are asked to note the presence or absence of RBD in the standard assessment of dementia among participants in the National Alzheimer’s Coordinating Center (NACC) (>20,000 subjects now entered into the Uniform Data Set) [31]. There has been no standardized method for determining the presence or absence of RBD, and the MSQ could be used as a screening tool for this purpose. It could also be used in epidemiologic studies, in which performing PSGs on hundreds or thousands of subjects is impractical and cost-prohibitive, yet the incidence or prevalence of RBD could be determined better than ever before; the only prevalence data (0.05%) on RBD are based on telephone questionnaires [32]. A recent study using the MSQ and many other measures in a Norwegian cohort with mild dementia has shown the utility of the MSQ in clinical research, in which probable RBD and other sleep disorders were shown to be more frequent and associated with more caregiver burden in patients with DLB compared to other dementia syndromes [33]. Preliminary data using the MSQ in the Mayo Clinic Study of Aging—a population-based study of cognition in Olmsted County, Minnesota [29]— has already yielded interesting results, with participants classified as normal controls based on clinical, functional, and neuropsychological data who screen positive for RBD in the Mayo Clinic Study of Aging having a higher frequency of parkinsonism [34], higher frequency of apathy and anxiety [35], and lower scores on measures of attention/executive functioning [36]. The frequency of probable RBD in this cohort of 70 – 89-year-old community-dwelling elderly is approximately 9% [37].
Analogous to mild cognitive impairment (MCI) being viewed as the intermediate stage between normal aging and Alzheimer’s disease, and often the syndrome which precedes the subsequent diagnosis of Alzheimer’s disease [38], the syndrome of mild extrapyramidal signs (MPS) is being viewed as an intermediate stage between normal aging and Parkinson’s disease [39]. The challenge in MCI and MPS is determining which individuals will subsequently develop AD or PD, respectively, and there is great interest in both syndromes at present from the clinical and research perspectives [40–43]. In the setting of mild extrapyramidal signs, using the MSQ could be helpful in much the same way it might be in MCI. Those with subtle parkinsonism plus probable RBD likely represents evolving Parkinson disease [44], those with subtle parkinsonism plus orthostatic hypotension and/or urinary incontinence plus probable RBD likely represents evolving MSA [23], and those with subtle parkinsonism without RBD may be more likely to represent a tauopathy such as PSP or CBD.
Finally, RBD in the 40 – 80 age range may eventually be fruitful to screen for in large scale studies who are otherwise devoid of cognitive and motor problems [45, 46] but are at risk of future development of PD, DLB, or MSA [26]; this will be particularly important when synuclein-active agents are available to test for disease-modifying properties [21, 47].
Since the purpose of this study was to validate the MSQ, only validation data are presented in this paper. Studies similar to that of Rongve et al. could use the MSQ to assess the frequency of probable RBD in populations of interest.
4.4 Comparison with other measures
There are few other measures available to screen for RBD, but each has shown high sensitivity with values in the 96–100% range [48–52] (note that only two of these measures were validated using PSG as the gold standard, which is obviously critical for confirming RBD [48–50]). The high SN likely reflects the rather unique features of the disorder: if any patient has RBD, the features are so consistent across individuals that any questions involving recurrent dream enactment behavior will likely be answered affirmatively and result in a positive screen. Other measures are described in various reports [53, 54], and their utility appears to also be sound, but the specific questionnaires themselves have not been published. Still other measures have one or two questions that likely capture RBD, but no PSG validation data have been published [55]. The main difference between the MSQ and the other measures is that bed partner/informants complete the MSQ whereas the sleepers themselves complete the other measures; hence the MSQ may be preferred if the persons of interest are cognitively impaired.
4.5 REM sleep without atonia
The finding of RSWA in six of the subjects is also noteworthy. Some have suggested that the PSG finding of RSWA may represent “ubclinical” RBD, and the follow-up clinical information in our six cases indicated that four of them indeed developed clinical RBD, with two of them also developing features of DLB (one of them had Lewy body disease subsequently confirmed at autopsy). One could argue that such cases could be viewed as “false negative” cases in our analyses since they had “no” responses to question 1 on the MSQ, but since there was no history of dream enactment behavior at the time the PSG was performed, and no dream enactment behavior present during REM sleep on the PSG, then such cases were appropriately viewed as true negatives. These findings, however, underscore the potential clinical relevance of following patients longitudinally when RSWA is identified on PSG.
4.6 Qualification and limitations
There are some qualifications and limitations to the MSQ and the analyses presented herein that must be acknowledged. The MSQ should not be used as the sole mechanism for making a diagnosis of any of the sleep disorders queried by the measure; rather, it was developed as a screening tool that can increase or decrease the suspicion of key sleep disorders so that clinicians can then decide in whom further assessment by sleep medicine clinicians should be pursued, and proceed to PSG in those who are appropriate. The validation was performed in a retrospective fashion using responses on the MSQ compared to the gold standards of clinical assessment and PSG, and inaccuracies can arise from chart reviews of non-standardized clinical assessments by multiple clinicians. A prospective approach using multiple reviewers and consensus diagnoses or Kappa coefficients generated to reflect the degree of agreement would be reasonable for future analyses. Also, since the frequency of some sleep disorders such as sleepwalking was so low, the imbalance between those with and without the disorder may inflate the SN and SP values. While the MSQ was developed to screen for several sleep disorders regardless of whether coexisting medical or neurologic disorders are present or not, the analyses in this paper primarily involved older male individuals with a coexisting neurodegenerative disorder. The high frequency of RBD in this cohort likely reflects the high frequency of subjects with DLB, and the high frequency of OSA likely reflects the high frequency of older males, and the low frequency of sleepwalking likely reflects the aged nature of this cohort. Therefore, the SN and SP may vary depending on the setting and population of patients in any validation analysis. Since the positive predictive value and negative predictive value of this scale will also vary depending on patient populations, the MSQ should be validated prospectively using standardized clinical assessments and PSGs in a variety of subjects, ages, and populations, including individuals with no sleep complaints. Data on the MSQ for screening for RBD in a community-based sample of elderly subjects have recently been presented, and the SN and SP were high in this patient population as well [56]. Our findings therefore indicate that among aged subjects with cognitive impairment and/or parkinsonism, the MSQ has adequate SN and SP for the diagnosis of RBD.
Supplementary Material
Mayo Sleep Questionnaire-Informant.
Permission is granted for non-commercial use in the context of patient care and research provided that no fee is charged. ©2009 Mayo Foundation for Medical Education and Research. All Rights Reserved.
Acknowledgments
Supported by grants P50 AG16574 and RO1 AG15866 from the National Institute on Aging, IIRG-05-14560 from the Alzheimer’s Association, and the Robert H. and Clarice Smith and Abigail Van Buren Alzheimer’s Disease Research Program of the Mayo Foundation. We thank our staff at the Mayo Center for Sleep Medicine and Mayo Alzheimer’s Disease Research Center for their evaluation and education/counseling for many of the patients in this report. We particularly extend our gratitude to the patients and their families for participating in research on aging and dementia.
ABBREVIATIONS
- AD
clinically probable Alzheimer’s disease
- ADRC
Alzheimer’s Disease Research Center
- AHI
apnea/hypopnea index
- CBS
corticobasal syndrome
- DLB
Dementia with Lewy bodies (as defined by the clinical syndrome)
- EMG
electromyography
- ESS
Epworth Sleepiness Scale
- FTD
behavioral variant frontotemporal dementia
- FTDP
frontotemporal dementia with parkinsonism
- FN
false negative
- FP
false positive
- LBD
Lewy body disease (as defined by pathology)
- MAPT
microtubule associated protein tau
- MCI
mild cognitive impairment
- MCJ
Mayo Clinic Jacksonville
- MCR
Mayo Clinic Rochester
- MSA
multiple system atrophy
- MSQ
Mayo Sleep Questionnaire
- OSA
obstructive sleep apnea
- PCA
posterior cortical atrophy
- PD
Parkinson’s disease
- PGRN
progranulin
- PLMS
periodic limb movements during sleep
- PNFA
progressive nonfluent aphasia
- PSG
polysomnography
- PSP
progressive supranuclear palsy
- RBD
REM sleep behavior disorder
- REM
rapid eye movement
- RLS
restless legs syndrome
- RSWA
REM sleep without atonia
- SD
semantic dementia
- SN
sensitivity
- SP
specificity
- SRLC
sleep related leg cramps
- SW
sleepwalking
- TN
true negative
- TP
true positive
Footnotes
DISCLOSURES
Bradley F. Boeve, MD – is an investigator in a clinical trial sponsored by Cephalon, Inc.
Jennifer R. Molano, MD – nothing to disclose
Tanis J. Ferman, PhD – nothing to disclose
Glenn E. Smith, PhD – nothing to disclose
Siong-Chi Lin, MD – nothing to disclose
Kevin Bieniek – nothing to disclose
Wail Haidar, MD – nothing to disclose
Maja Tippmann-Peikert, MD – nothing to disclose
David S. Knopman, MD - served on a Data Safety Monitoring Board for Sanofi Aventi, and is an investigator in clinical trials sponsored by Elan Pharmaceuticals and by Forest Laboratories.
Neill R. Graff-Radford, M.B.Ch.B. - consultant to Codman and is/was an investigator in clinical trials sponsored by Myriad Pharmaceuticals, Elan Pharmaceuticals, and Pfizer Pharmaceuticals.
John A. Lucas, PhD – nothing to disclose
Ronald C. Petersen, PhD, MD - consultant to GE Healthcare and Elan
Pharmaceuticals, has served on a data safety monitoring boards a clinical trial sponsored by Elan Pharmaceuticals and Wyeth Pharmaceuticals.
Michael H. Silber, MBChB – nothing to disclose
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Boeve B, Silber M, Ferman T, Smith G. Validation of a questionnaire for the diagnosis of REM sleep behavior disorder. Sleep. 2002;25(abstr suppl):A486. [Google Scholar]
- 2.Boeve B, Silber M, Ferman T, Smith G, Petersen R. Validation of a questionnaire for the diagnosis of REM sleep behavior disorder. Neurology. 2002;58(suppl 3):A509. [Google Scholar]
- 3.Johns M. A new method for measuring daytime sleepiness: the Epworth Sleepiness Scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 4.Iber C, Ancoli-Israel S, Chesson A, Quan S Medicine, ftAAoS. The AASM manual for the scoring of sleep and associated events: rules, terminology and technical specifications. Westchester, IL: American Academy of Sleep Medicine; 2007. [Google Scholar]
- 5.Rechtschaffen A, Kales A. A manual of standardized terminology, techniques and scoring system for sleep stages of human subjects. Los Angeles: Brain Information Service, Brain Research Institute; 1968. [Google Scholar]
- 6.Ferri R, Franceschini C, Zucconi M, Vandi S, Poli F, Bruni O, et al. Searching for a marker of REM sleep behavior disorder: submentalis muscle EMG amplitude analysis during sleep in patients with narcolepsy/cataplexy. Sleep. 2008;31:1409–1417. [PMC free article] [PubMed] [Google Scholar]
- 7.Frauscher B, Iranzo A, Högl B, Casanova-Molla J, Salamero M, Gschliesser V, et al. Quantification of electromyographic activity during REM sleep in multiple muscles in REM sleep behavior disorder. Sleep. 2008;31:724–731. doi: 10.1093/sleep/31.5.724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mayer G, Kesper K, Ploch T, Canisius S, Penzel T, Oertel W, et al. Quantification of tonic and phasic muscle activity in REM sleep behavior disorder. J Clin Neurophysiol. 2008;25:48–55. doi: 10.1097/WNP.0b013e318162acd7. [DOI] [PubMed] [Google Scholar]
- 9.International Classification of Sleep Disorders: Diagnostic and Coding Manual. 2. Westchester, IL: American Academy of Sleep Medicine; 2005. [Google Scholar]
- 10.Petersen R. Mild cognitive impairment as a diagnostic entity. J Intern Med. 2004;256:183–194. doi: 10.1111/j.1365-2796.2004.01388.x. [DOI] [PubMed] [Google Scholar]
- 11.McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan E. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA work group under the auspices of the Department of Health and Human Services Task Force on Alzheimer’s disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- 12.McKeith I, Dickson D, Lowe J, Emre M, O’Brien J, Feldman H, et al. Dementia with Lewy bodies: Diagnosis and management: Third report of the DLB Consortium. Neurology. 2005;65:1863–1872. doi: 10.1212/01.wnl.0000187889.17253.b1. [DOI] [PubMed] [Google Scholar]
- 13.Neary D, Snowden J, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–1554. doi: 10.1212/wnl.51.6.1546. [DOI] [PubMed] [Google Scholar]
- 14.Boeve B, Lang A, Litvan I. Corticobasal degeneration and its relationship to progressive supranuclear palsy and frontotemporal dementia. Ann Neurol. 2003;54:S15–S19. doi: 10.1002/ana.10570. [DOI] [PubMed] [Google Scholar]
- 15.Litvan I, Agid Y, Calne D, Campbell G, Dubois B, Duvoisin R, et al. Clinical research criteria for the diagnosis of progressive supranuclear palsy (Steele-Richardson-Olszewski syndrome): Report of the NINDS-SPSP International Workshop. Neurology. 1996;47:1–9. doi: 10.1212/wnl.47.1.1. [DOI] [PubMed] [Google Scholar]
- 16.Gilman S, Low P, Quinn N, Albanese A, Ben-Shlomo Y, Fowler C, et al. Consensus statement on the diagnosis of multiple system atrophy. J Neurol Sci. 1999;163:94–98. doi: 10.1016/s0022-510x(98)00304-9. [DOI] [PubMed] [Google Scholar]
- 17.Tang-Wai D, Graff-Radford N, Boeve B, Dickson D, Parisi J, Crook R, et al. Clinical, genetic, and neuropathologic characteristics of posterior cortical atrophy. Neurology. 2004;63:1168–1174. doi: 10.1212/01.wnl.0000140289.18472.15. [DOI] [PubMed] [Google Scholar]
- 18.Iranzo A, Santamaria J. Severe obstructive sleep apnea/hypopnea mimicking REM sleep behavior disorder. Sleep. 2005;28:203–206. doi: 10.1093/sleep/28.2.203. [DOI] [PubMed] [Google Scholar]
- 19.Boeve B, Silber M, Ferman T, Lucas J, Parisi J. Association of REM sleep behavior disorder and neurodegenerative disease may reflect an underlying synucleinopathy. Mov Disord. 2001;16:622–630. doi: 10.1002/mds.1120. [DOI] [PubMed] [Google Scholar]
- 20.Boeve B, Silber M, Parisi J, Dickson D, Ferman T, Benarroch E, et al. Synucleinopathy pathology and REM sleep behavior disorder plus dementia or parkinsonism. Neurology. 2003;61:40–45. doi: 10.1212/01.wnl.0000073619.94467.b0. [DOI] [PubMed] [Google Scholar]
- 21.Boeve B, Silber M, Saper C, Ferman T, Dickson D, Parisi J, et al. Pathophysiology of REM sleep behaviour disorder and relevance to neurodegenerative disease. Brain. 2007;130:2770–2788. doi: 10.1093/brain/awm056. [DOI] [PubMed] [Google Scholar]
- 22.Schenck CH, Bundlie SR, Mahowald MW. Delayed emergence of a parkinsonian disorder in 38% of 29 older men initially diagnosed with idiopathic rapid eye movement sleep behaviour disorder. Neurology. 1996;46:388–393. doi: 10.1212/wnl.46.2.388. [DOI] [PubMed] [Google Scholar]
- 23.Iranzo A, Molinuevo J, Santamaría J, Serradell M, Martí M, Valldeoriola F, et al. Rapid-eye-movement sleep behaviour disorder as an early marker for a neurodegenerative disorder: a descriptive study. Lancet Neurol. 2006;5:572–577. doi: 10.1016/S1474-4422(06)70476-8. [DOI] [PubMed] [Google Scholar]
- 24.Postuma R, Gagnon J, Vendette M, Fantini M, Massicotte-Marquez J, Montplaisir J. Quantifying the risk of neurodegenerative disease in idiopathic REM sleep behavior disorder. Neurology. 2009 Jan 7; doi: 10.1212/01.wnl.0000340980.19702.6e. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Boeve B. REM sleep behavior disorder: Updated review of the core features, the REM sleep behavior disorder-neurodegenerative disease association, evolving concepts, controversies, and future directions. Ann NY Acad Sci. 2010;1184:17–56. doi: 10.1111/j.1749-6632.2009.05115.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Claassen D, Josephs K, Ahlskog J, Smith G, Silber M, Tippmann-Peikert M, et al. REM sleep behavior disorder preceding other aspects of synucleinopathies by up to half a century. Neurology. 2010;75:494–499. doi: 10.1212/WNL.0b013e3181ec7fac. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ferman T, Boeve B, Smith G, Silber M, Lucas J, Graff-Radford N, et al. Dementia with Lewy bodies may present as dementia with REM sleep behavior disorder without parkinsonism or hallucinations. J Internat Neuropsychol Soc. 2002;8:907–914. doi: 10.1017/s1355617702870047. [DOI] [PubMed] [Google Scholar]
- 28.Winblad B, Palmer K, Kivipelto M, Jelic V, Fratiglioni L, Wahlund L, et al. Mild cognitive impairment. J Intern Med. 2004;256:180–246. doi: 10.1111/j.1365-2796.2004.01380.x. [DOI] [PubMed] [Google Scholar]
- 29.Roberts R, Geda Y, Knopman D, Cha R, Pankratz V, Boeve B, et al. The Mayo Clinic Study of Aging: design and sampling, participation, baseline measures and sample characteristics. Neuroepidemiology. 2008;30:58–69. doi: 10.1159/000115751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Molano J, Boeve B, Ferman T, Smith G, Parisi J, Dickson D, et al. Mild cognitive impairment +/− subsequent dementia associated with underlying Lewy body disease. Neurology. 2009;72:A248. [Google Scholar]
- 31.Kukull W. National Alzheimer’s Coordinating Center; [Accessed August, 2010]. http://www.alz.washington.edu/ [Google Scholar]
- 32.Ohayon M, Caulet M, Priest R. Violent behavior during sleep. J Clin Psychiatr. 1997;58:369–376. [PubMed] [Google Scholar]
- 33.Rongve A, Boeve B, Aarsland D. Frequency and correlates of caregiver-reported sleep disturbances in a sample of persons with early dementia. J Am Geriatr Soc. 2010;58:480–486. doi: 10.1111/j.1532-5415.2010.02733.x. [DOI] [PubMed] [Google Scholar]
- 34.Mihci E, Molano J, Boeve B, Roberts R, Geda Y, Knopman D, et al. Parkinsonism is associated with probable REM sleep behavior disorder in cognitively normal elderly subjects: The Mayo Clinic Study of Aging. Neurology. 2008;70(Suppl 1):A150. [Google Scholar]
- 35.Molano J, Mihci E, Boeve B, Roberts R, Geda Y, Knopman D, et al. Anxiety and apathy are associated with probable REM sleep behavior disorder among cognitively normal elderly subjects: The Mayo Clinic Study of Aging. Neurology. 2008;70(Suppl 1):A146. [Google Scholar]
- 36.Molano J, Mihci E, Boeve B, Roberts R, Geda Y, Knopman D, et al. Lower scores in attention/executive functioning is associated with probable REM sleep behavior disorder among cognitively normal elderly subjects: The Mayo Clinic Study of Aging. Neurology. 2008;70(Suppl 1):A66. [Google Scholar]
- 37.Molano J, Boeve B, Roberts R, Geda Y, Christrianson T, Knopman D, et al. Frequency of sleep disorders in the community-dwelling elderly: The Mayo Clinic Study of Aging. Neurology. 2009;72 (Suppl 3):A107. [Google Scholar]
- 38.Petersen RC. Mild cognitive impairment: current research and clinical implications. Semin Neurol. 2007;27:22–31. doi: 10.1055/s-2006-956752. [DOI] [PubMed] [Google Scholar]
- 39.Louis E, Bennett D. Mild Parkinsonian signs: An overview of an emerging concept. Mov Disord. 2007;22:1681–1688. doi: 10.1002/mds.21433. [DOI] [PubMed] [Google Scholar]
- 40.Petersen R, Aisen P, Beckett L, Donohue M, Gamst A, Harvey D, et al. Alzheimer’s Disease Neuroimaging Initiative (ADNI): clinical characterization. Neurology. 2010;74:201–209. doi: 10.1212/WNL.0b013e3181cb3e25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.De Meyer G, Shapiro F, Vanderstichele H, Vanmechelen E, Engelborghs S, De Deyn P, et al. Diagnosis-independent Alzheimer disease biomarker signature in cognitively normal elderly people. Arch Neurol. 2010;67:949–956. doi: 10.1001/archneurol.2010.179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Molano J, Boeve B, Ferman T, Smith G, Parisi J, Dickson D, et al. Mild cognitive impairment associated with limbic and neocortical Lewy body disease: A clinicopathological study. Brain. 2009 Nov 4; doi: 10.1093/brain/awp280. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Louis E, Tang M, Schupf N. Mild parkinsonian signs are associated with increased risk of dementia in a prospective, population-based study of elders. Mov Disord. 2010;25:172–178. doi: 10.1002/mds.22943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Postuma R, Lang A, Massicotte-Marquez J, Montplaisir J. Potential early markers of Parkinson disease in idiopathic REM sleep behavior disorder. Neurology. 2006;66:845–851. doi: 10.1212/01.wnl.0000203648.80727.5b. [DOI] [PubMed] [Google Scholar]
- 45.Uchiyama M, Isse K, Tanaka K, Yokota N, Hamamoto H, Aida S, et al. Incidental Lewy body disease in a patient with REM sleep behavior disorder. Neurology. 1995;45:709–712. doi: 10.1212/wnl.45.4.709. [DOI] [PubMed] [Google Scholar]
- 46.Boeve B, Dickson D, Olson E, Shepard J, Silber M, Ferman T, et al. Insights into REM sleep behavior disorder pathophysiology in brainstem-predominant Lewy body disease. Sleep Med. 2007;8:60–64. doi: 10.1016/j.sleep.2006.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Boeve B, Saper C. REM sleep behavior disorder: A possible early marker for synucleinopathies. Neurology. 2006;66:796–797. doi: 10.1212/01.wnl.0000209264.61035.bb. [DOI] [PubMed] [Google Scholar]
- 48.Ohayon M, Guilleminault C, Zulley J, Palombini L, Raab H. Validation of the sleep-EVAL system against clinical assessments of sleep disorders and polysomnographic data. Sleep. 1999;22:925–930. doi: 10.1093/sleep/22.7.925. [DOI] [PubMed] [Google Scholar]
- 49.Consens FB, Chervin RD, Koeppe RA, Little R, Liu S, Junck L, et al. Validation of a polysomnographic score for REM sleep behavior disorder. Sleep. 2005;28:993–997. doi: 10.1093/sleep/28.8.993. [DOI] [PubMed] [Google Scholar]
- 50.Stiasny-Kolster K, Mayer G, Schäfer S, Möller J, Heinzel-Gutenbrunner M, Oertel W. The REM sleep behavior disorder screening questionnaire--a new diagnostic instrument. Mov Disord. 2007;22:2386–2393. doi: 10.1002/mds.21740. [DOI] [PubMed] [Google Scholar]
- 51.Fulda S, Hornyak M, Muller K, Cerny L, Beitinger P, Wetter T. Development and validation of the Munich Parasomnia Screening (MUPS): A questionnaire for parasomnias and nocturnal behaviors. Somnologie. 2008;12:56–65. [Google Scholar]
- 52.Roth T, Zammit G, Kushida C, Doghramji K, Mathias S, Wong J, et al. A new questionnaire to detect sleep disorders. Sleep Med. 2002;3:99–108. doi: 10.1016/s1389-9457(01)00131-9. [DOI] [PubMed] [Google Scholar]
- 53.Comella C, Nardine T, Diederich N, Stebbins G. Sleep-related violence, injury, and REM sleep behavior disorder in Parkinson’s disease. Neurology. 1998;51:526–529. doi: 10.1212/wnl.51.2.526. [DOI] [PubMed] [Google Scholar]
- 54.Scaglione C, Vignatelli L, Plazzi G, Marchese R, Negrotti A, Rizzo G, et al. REM sleep behaviour disorder in Parkinson’s disease: a questionnaire-based study. Neurol Sci. 2005;25:316–321. doi: 10.1007/s10072-004-0364-7. [DOI] [PubMed] [Google Scholar]
- 55.Chaudhuri K, Pal S, Dimarco A, Whately-Smith C, Bridgman K, Mathew R, et al. The Parkinson’s disease sleep scale: a new instrument for assessing sleep and nocturnal disability in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2002;73:629–635. doi: 10.1136/jnnp.73.6.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Boeve B, Molano J, Ferman T, Smith G, Lin S, Bieniek K, et al. Screening for REM sleep behavior disorder in the community-dwelling elderly: Validation of the Mayo Sleep Questionnaire in the Mayo Clinic Study of Aging. Neurology. 2010;74 (suppl 2):A432. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.