Abstract
Myotonic dystrophy type 2 (DM2) is a progressive multisystem disease with muscle weakness and myotonia as main characteristics. The disease is caused by a repeat expansion in the zinc-finger protein 9 (ZNF9) gene on chromosome 3q21. Several reports show that patients from European ancestry share an identical haplotype surrounding the ZNF9 gene. In this study, we investigated whether the Dutch DM2 population carries the same founder haplotype. In all, 40 Dutch DM2 patients from 16 families were genotyped for eight short tandem repeat markers surrounding the ZNF9 gene. In addition, the single-nucleotide polymorphism (SNP) rs1871922 located in the first intron of DM2 was genotyped. Results were compared with previously published haplotypes from unrelated Caucasian patients. The repeat lengths identified in this study were in agreement with existing literature. In 36 patients of our population, we identified three common haplotypes. One patient showed overlap with the common haplotype for only one marker closest to the ZNF9 gene. The haplotype from a family originating from Morocco showed overlap with that of the patients of European descent for a region of 222 kb. All patients carried at least one C allele of SNP rs1871922 indicating that all patients carry the European founder haplotype. We conclude that DM2 patients from the Netherlands, including a North-African family, harbor a common haplotype surrounding the ZNF9 gene. This data show that the Dutch patients carry the common founder haplotype and strongly suggest that DM2 mutations in Europe and North Africa originate from a single ancestral founder.
Keywords: myotonic dystrophy type 2, haplotype, ZNF9
Introduction
Myotonic dystrophy type 2 (DM2, OMIM 602668) is an autosomal dominant, multisystem disease, characterized by progressive muscle weakness, myotonia, cataracts, and multiorgan involvement with cardiac conduction defects, gastrointestinal involvement, and endocrine disorders.1, 2 In 2001, the mutation causing DM2 was identified as a CCTG expansion in intron 1 of the zinc-finger protein 9 (ZNF9) gene located on chromosome 3q21.3.3, 4 Expanded DM2 alleles show unprecedented somatic instability, with significant increases in length over time (eg, 2000 base pairs per 3 years). The number of CCTG repeats in healthy individuals is below 30 and can be up to 11 000 in patients, the shortest reported expansion associated with DM2 is (CCTG)75.
Two groups independently showed that European DM2 patients share a common ancestor.5, 6 Liquori et al3 investigated 71 families with DM2, of which 70 families were of Northern European descent and one family from Afghanistan. The majority of the families carried one of the three consensus haplotypes. The haplotype of an Afghan family showed great similarity to the core haplotype, suggesting that the mutation was introduced via the settling of Aryan tribes of Indo–European descent in ancient Afghanistan. Bachinski et al6 studied 17 kindreds from geographically separate populations of European origin; the presence of a single founder mutation in European DM2 patients was indicated in this study as well. On the basis of their data, the authors estimated the age of the DM2 mutation at 4000–11 000 years. Neither the study of Liquori, nor the study of Bachinski included patients from the Netherlands. Recently, a Japanese group identified the first Japanese patient with DM2; this patient carried a haplotype that differs from the haplotype associated with DM2 in the European population.7
In this study, we set out to assess whether Dutch DM2 patients, including a North-African family, carry the common European founder haplotype.
Methods
Patients
All known DM2 patients in the Netherlands were identified using the Dutch neuromuscular database and approached for participation in the study.8 A total of 42 potentially eligible DM2 patients were recruited. One DM2 patient did not consent without specifying the reason, and one registered DM2 patient was found to be deceased. We included 40 DM2 patients from 16 unrelated families in the study (see Supplementary Table 1). All of the patients were Caucasian, with one family ethnically originating from Morocco. The regional ethics review board approved the study and all patients had given written informed consent.
Molecular analysis
All molecular analyses were performed in a CCKL (Co-ordination Committee for the promotion of Quality Control with regard to Laboratory research, http://www.cckl.nl)-accredited laboratory at the Department of Human Genetics at the Radboud University Nijmegen Medical Centre in Nijmegen, The Netherlands.
Genetic confirmation of DM2
Affected individuals were identified as DM2 patients using southern blotting according to the protocol as previously described.3, 4 All patients harbored a repeat expansion in the ZNF9 gene.
Microsatellite analysis
Molecular analysis was performed in 40 patients. DNA samples from the study of Liquori et al were included to allow direct comparison of our data with the previously published haplotypes. Three trio's (two affected individuals per trio) each representing one haplotype were analyzed. Genomic DNA was extracted from blood lymphocytes using standard procedures.9 Eight short tandem repeat (STR) markers as previously described by Liquori et al5 were selected for haplotype analysis (CL3N122, CL3N99, CL3N83, CL3N59, CL3N117, CL3N119, CL3N19, and CL3N23). Primers were ordered from Applied Biosystems (Nieuwerkerk aan den IJssel, The Netherlands). The forward primer had a fluorescent dye label (6-FAM, NED, or VIC), whereas the reverse primer contained a proprietary tail that helps stabilize the amplified product. Semiautomated fluorescent genotyping was carried out using the following protocol. Genomic DNA (50 ng) was amplified in a 10 μl reaction using AmpliTaq Gold DNA Polymerase (0.4 U, Applied Biosystems), AmpliTaq PCR Buffer II (Applied Biosystems), dNTPs (250 μ each), magnesium (1.25 or 2.5 m, depending on the primers), and the marker-specific primers (0.5 μ). Amplification was performed using the following protocol: 95°C for 12 min followed by 10 cycles of denaturation for 30 s at 94°C, annealing at 62°C, and primer extension at 72°C for 1 min. A subsequent 22 cycles were performed with 30 s heating at 89°C, 30 s annealing at 62°C and primer extension at 72°C, followed by a final extension at 72°C for 10 min 1 μl of each amplified STR marker was pooled for each patient, and combined with size standard (LIZ-500) before being analyzed on an ABI3730 (Applied Biosystems). GeneMapper v4.0 (Applied Biosystems) was used to analyze the raw results from the ABI3730; a genotype was not considered final until two persons had independently checked the GeneMapper results and both individuals were in agreement.
Single-nucleotide polymorphism (SNP) genotyping
SNP rs1871922 (TSC0873597) was genotyped according to the method described previously by Vallo et al,10 with the following adaptations. For restriction fragment length polymorphism analysis, the PCR products were purified using the NucleoFat 96 PCR plate (BIOKE, Leiden, NL, USA) and incubated overnight at 37°C with 5 U of HaeIII enzyme (New England Biolabs Ltd., Hitchin, UK). One sample of each genotype was sequenced using a 3730 DNA Analyzer (Applied Biosystems) as quality control.
Haplotype construction
Affected haplotypes were established by determining which alleles co-segregated in the families. In case only a proband was available, we assigned the haplotype present in other DM2 patients as the affected haplotype.
Results
Haplotype analysis
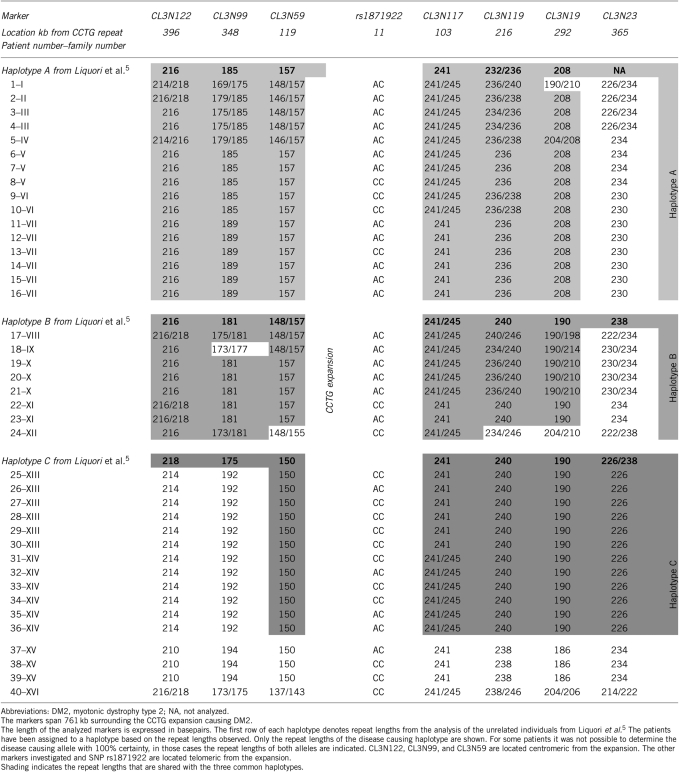
We were unable to obtain a PCR product for marker CL3N83. As this marker was not obligatory to determine if our patients carried similar haplotypes as presented by Liquori et al,5 we excluded this marker from the study. DNA of 40 patients was analyzed for the remaining seven microsatellite markers surrounding the DM2 gene ZNF9. The results of the analysis are shown in Table 1. The lengths of the repeats that we found were in the same range as those reported by Liquori et al.5 The flanking marker CL3N23 and marker CL3N99 showed more variability in repeat length compared with the other markers, which is in agreement with the data of Liquori et al. We were able to assign 90% of the patients to the three previously published haplotypes (Table 1: patients 1–36). Our analysis shows that patients with haplotype C carry different repeat lengths of the markers centromeric from CL3N59 than the previously reported lengths.5
Table 1. Haplotypes of 40 DM2 patients.
Patient one could be assigned under two haplotypes; based on marker CL3N59 and CL3N119 the patients fits with haplotype A. However, on the basis of the length of markers CL3N119, CL3N19, and CL3N23, the patient shares part of the haplotype C group. As the length of CL3N59 is unique for haplotype A we decided to fit the patient under this haplotype.
One patient born in the United States of America (patient 40) showed a haplotype that differs from the common haplotypes identified in the Dutch patient population. The haplotype of the three patients (number 37, 38, and 39) from Morocco was comparable with haplotype C, but only for a region of 222 kb surrounding the ZNF9 gene.
SNP genotyping
SNP rs1871922 is located in intron one of the ZNF9 gene, 11kb telomeric from the expansion. The C allele of this SNP is linked to the European founder mutation and was, therefore, used to investigate if patients carry this mutation.6, 7, 10 SNP genotyping showed that all patients carried at least one C allele.
Discussion
In this study, we show that Dutch DM2 patients share a common haplotype surrounding the DM2 locus, which is the same as the European founder haplotype. The three family members originating from Morocco also carried part of the common European haplotype. Genotype analysis of SNP rs1871922 showed that all patients carried the C allele which strongly indicates that also these patients carry the common European founder mutation.6
Although we designed similar primers for the repeat length analysis as Liquori et al,5 we did observe different fragment sizes than those found in the previous study. This can probably be attributed to the primer design (our primers carried a poly-A tail for stability) and difference in the machines used for the estimation of the fragment lengths. Owing to the inclusion of samples with known repeat lengths, we were able to compare our results directly with the previously published haplotypes. In all, 88% of the patients carried one of the three haplotypes known to be associated with DM2. However, patients carrying haplotype C showed a fragment length 214 bp for marker CL3N122 (expected length 218 bp) and 192 bp for marker CL3N99 (expected length 175 bp). On the basis of this, we can conclude that a recombination occurred between marker CL3N99 and CL3N59 in the Dutch population compared with the patients analyzed in the study by Liquori et al.5
Recently, the first DM2 patient from an East-Asian population was described.7 This patient is the first patient reported with a haplotype different from the European founder haplotype. Three non-European patients originating from Morocco (37–39) were part of our study, the data presented show that these patients carry part of haplotype C (222 kb surrounding the ZNF9 expansion). This is the second non-European family described that carries one of the common founder haplotypes.5, 6 The disease linked haplotype is, however, different from the one described for the family from Afghanistan.5 As Morocco is part of the Mediterranean basin and has had strong historic ties to the Roman Empire and other European colonial powers, we cannot exclude that the presence of the European founder haplotype is a result of genetic admixture.
Patient 40 carried only the small common region shared by all patients (from the CCTG expansion to CL3N117). Therefore, the patient could not be assigned to one of the three common haplotypes. This can be attributed to the ethnicity of the patient. The patient originated from America and his great grandparents originated from Germany and Russia.
In conclusion, our data shows that Dutch patients carry the common founder haplotype and strongly suggest that European and North-African DM2 patients share an identical haplotype. Further studies in African and other non-European DM2 patients are required to confirm this latter result. It may be worthwhile at least for counseling patients to investigate whether DM2 patients of different ethnic backgrounds who share an identical haplotype have a comparable phenotype.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on European Journal of Human Genetics website (http://www.nature.com/ejhg)
Supplementary Material
References
- Harper P.Myotonic Dystophy5th ednW.B. Saunders: London; 2001 [Google Scholar]
- Tieleman AA, van Vliet J, Jansen JB, van der Kooi AJ, Borm GF, van Engelen BG. Gastrointestinal involvement is frequent in myotonic dystrophy type 2. Neuromuscul Disord. 2008;18:646–649. doi: 10.1016/j.nmd.2008.05.010. [DOI] [PubMed] [Google Scholar]
- Liquori CL, Ricker K, Moseley ML, et al. Myotonic dystrophy type 2 caused by a CCTG expansion in intron 1 of ZNF9. Science. 3-8-2001;293:864–867. doi: 10.1126/science.1062125. [DOI] [PubMed] [Google Scholar]
- Day JW, Ricker K, Jacobsen JF, et al. Myotonic dystrophy type 2: molecular, diagnostic and clinical spectrum. Neurology. 25-2-2003;60:657–664. doi: 10.1212/01.wnl.0000054481.84978.f9. [DOI] [PubMed] [Google Scholar]
- Liquori CL, Ikeda Y, Weatherspoon M, et al. Myotonic dystrophy type 2: human founder haplotype and evolutionary conservation of the repeat tract. Am J Hum Genet. 2003;73:849–862. doi: 10.1086/378720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bachinski LL, Udd B, Meola G, et al. Confirmation of the type 2 myotonic dystrophy (CCTG)n expansion mutation in patients with proximal myotonic myopathy/proximal myotonic dystrophy of different European origins: a single shared haplotype indicates an ancestral founder effect. Am J Hum Genet. 2003;73:835–848. doi: 10.1086/378566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saito T, Amakusa Y, Kimura T, et al. Myotonic dystrophy type 2 in Japan: ancestral origin distinct from Caucasian families. Neurogenetics. 2008;9:61–63. doi: 10.1007/s10048-007-0110-4. [DOI] [PubMed] [Google Scholar]
- van Engelen BG, van Veenendaal H, van Doorn PA, et al. The Dutch neuromuscular database CRAMP (computer registry of all myopathies and polyneuropathies): development and preliminary data. Neuromuscul Disord. 2007;17:33–37. doi: 10.1016/j.nmd.2006.09.017. [DOI] [PubMed] [Google Scholar]
- Miller SA, Dykes DD, Polesky HF. A simple salting out procedure for extracting DNA from human nucleated cells. Nucleic Acids Res. 11-2-1988;16:1215. doi: 10.1093/nar/16.3.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vallo L, Bonifazi E, Borgiani P, Novelli G, Botta A. Characterization of a single nucleotide polymorphism in the ZNF9 gene and analysis of association with myotonic dystrophy type II (DM2) in the Italian population. Mol Cell Probes. 2005;19:71–74. doi: 10.1016/j.mcp.2004.09.003. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.