Abstract
The global population is aging. With the high prevalence of dementia and functional decline in older Americans, many aging adults with disabilities reside in nursing homes in their final stage of life. Immunosenescence, multiple comorbid disease, and grouped quarter living all coalesce in nursing home residents to increase the risk for infectious disease. The unique issues involved with diagnosis, prognosis, and management of infectious diseases in nursing home residents make research based in the nursing home setting both necessary and exciting for the physician investigator. This review discusses the opportunities and challenges involved with research of the evolving public health problem of infections among nursing home residents.
The Aging Population and Nursing Home Care
Until the early 20th century, infectious diseases were primarily responsible for mortality in the United States, resulting in an average life expectancy of 47 years [1]. With the advent of antiseptic techniques, vaccinations, antibiotics, and other public health measures, life expectancy in the early 21st century has risen to 76 to 80 years in most developed nations [2]. Life expectancy has also risen in less developed nations, but to a lesser extent. Consequently, by the year 2030 in the United States, it is estimated that 70 million people will be ≥ 65 years old [3]. This epidemiologic transition has shifted the national burden of morbidity from infectious diseases and acute illness to chronic diseases and degenerative illness [2]. However, with multiple comorbid diseases, many older persons develop functional decline and dependency requiring full time care within nursing homes. Recent estimates reveal that there are over 16,000 nursing home facilities in the United States. Although the total number of nursing home beds available has reduced from 1.9 million in 1999 to 1.7 million in 2004, by 2050, the number of Americans requiring long-term care (including assisted living) is expected to double [4].
Unique Risks for Infectious Diseases in Nursing Home Residents
Nursing home residents are at particular risk for infectious diseases because of host risk factors, as well as risks inherent to grouped living quarters. Host risk factors, including age-associated changes in adaptive (e.g., B and T cell function) and innate immunity (e.g., surface expression or function of pattern recognition receptors), may account for reduced responsiveness to vaccinations (e.g., influenza, S. pneumoniae, and varicella-zoster vaccines), increased susceptibility to systemic infection from specific pathogens (e.g., Listeria) and reactivation of latent infections (e.g., Mycobacteria, and varicella-zoster virus) [5–7]. Additionally, multiple comorbid diseases (e.g., diabetes mellitus, chronic obstructive pulmonary disease, impaired dentition) and degenerative disease requiring the insertion of prosthetic devices (e.g., joint prostheses, implantable cardiac devices) place nursing home residents at increased risk of common community-acquired infections including pneumonia, UTI, prosthetic joint infection, and infected endovascular foreign bodies with bacteremia. Grouped residence within a nursing home unit promotes common source respiratory (e.g., influenza, respiratory syncitial virus) and gastrointestinal (e.g., norovirus) outbreaks. Empiric antibiotics commonly prescribed for nursing home residents with infectious syndromes place them at increased risk of subsequent infection with antibiotic-resistant pathogens (e.g., methicillin-resistant Staphylococcus aureus, vancomycin-resistant Enterococcus species, multidrug-resistant gram-negative bacilli) and Clostridium difficile colitis [8]. These antibiotic resistant pathogens can subsequently be secondarily transmitted to uninfected residents of the same nursing home, as well as to hospitalized patients when nursing home residents are admitted for non-infection related acute illness. Health care workers colonized with resistant pathogens can also contribute to colonization of nursing home residents because of prolonged contact with residents. Therefore, nursing home residents can serve as unintentional vectors that shuttle clinically relevant pathogens from the nursing home to the hospital, and back to the nursing home, and impact on the infectious disease burden of an entire community. Given the recently recognized expansion of alternative grouped quarter living opportunities (e.g., assisted living facilities, home care), the demographics of nursing home residents have shifted to the oldest adults with extensive comorbid disease and functional disabilities who are most vulnerable to infection. This reality has created a mandate for investigation of this high risk population for infectious disease.
Common Infections among Nursing Home Residents
Among institutionalized older adults with multiple comorbidities, functional decline, and cognitive impairment, the clinical manifestations of infectious diseases may be subtle. Overt clinical signs (e.g., fever) may be absent or diminished [9]. Availability of diagnostic testing is often limited, and empiric therapy for many clinical infectious disease syndromes is standard of care. Goals of care (e.g., comfort measures, do-not-resuscitate orders) may help inform the degree of aggressive investigative and treatment options, and serve to support the preference for site of care for the acute infectious illness (i.e., hospital vs. nursing home).
Given the high prevalence of functional disability, dementia, incontinence, poor oral hygiene, and swallowing difficulties, the most common infections in nursing home residents are pneumonia, urinary tract infection (UTI), and skin and soft tissue infection. Pneumonia remains a leading cause of morbidity and mortality in older adults, resulting in almost half of all infectious disease related hospitalizations and deaths [10–11]. Recent data from the Centers for Disease Control and Prevention show that hospitalization rates for pneumonia among 65 to 84 year olds have increased, while rates have remained consistently high for those aged ≥ 85 years [12]. Among residents ≥ 65 years, the rate of nursing home acquired pneumonia is as high as 365 cases per 1,000 person-years; this rate is 10-fold greater than the rate among elderly community dwellers [13]. Although UTI does not result in as much mortality as pneumonia among nursing home residents, it is the second most common reason for infectious disease admission to the hospital [10]. Additionally, it is the most common reason indicated for antibiotic prescriptions in the nursing home setting, and it is the most costly and resource intensive condition among Medicare beneficiaries [14]. Skin and soft tissue infections (SSTI) are the third most common infection in nursing home residents, primarily occurring because of skin breakdown secondary to physical trauma, maceration related to immobility, or device use. Because of multiple comorbidities and disabilities, nursing home residents are more likely to require invasive medical devices (e.g., feeding tube, tracheostomy, chronic indwelling urinary catheter, cardiac devices). Feeding tubes are present in 7–41% of cognitively impaired nursing home residents, and urinary catheterization rates range from 11–12%. Device use has been associated with both colonization and infection with antibiotic-resistant organisms in nursing home residents [15–16], and repeated courses of empiric antimicrobial therapy foster the emergence of resistant pathogens.
Epidemiologic risk factors and environmental exposures within the nursing home have created a major public health burden of infectious disease among an expanding population of unique hosts. Rigorous investigation of infections within the nursing home setting is needed to improve the rigor of diagnostic criteria, prognostic estimation of outcomes, and development of effective targeted prevention strategies. The opportunities for investigation include studies on the epidemiology, diagnosis, treatment, prognosis, and prevention of the most common infectious diseases (e.g., pneumonia, UTI, SSTI, diarrheal disease) as well as studies focusing on cost effectiveness and transmission of resistant pathogens (see Figure 1).
Figure 1.
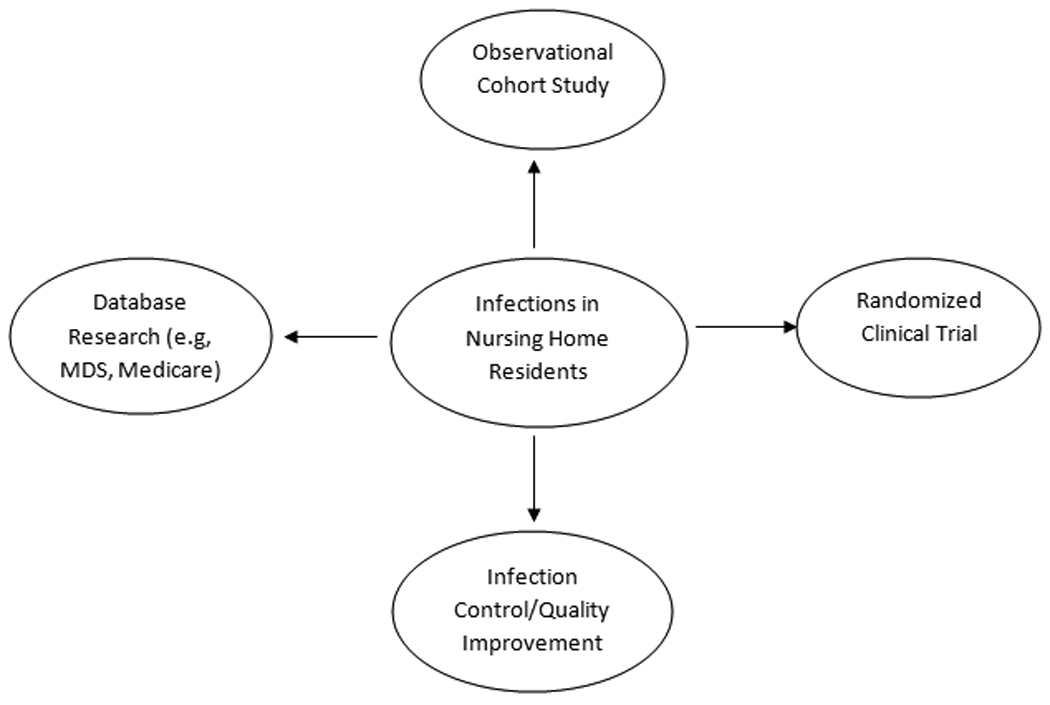
Conceptual Model of Research in Nursing Homes
Conducting Research of Infectious Diseases in the Nursing Home Setting
For decades, investigators have studied risk factors, clinical presentation, outcomes, interventions, and prevention strategies for infections in the nursing home setting. Recent observational cohort studies have more rigorously defined clinical syndromes (e.g., UTI) [13, 17–19] and validated modifiable risk factors for common infections (e.g., pneumonia). All of these studies have fostered preventive strategies that have been and are currently being tested in clinical trials [20–24]. As with many other research environments, utilization of large administrative databases and observational cohort studies has been easier to conduct than randomized clinical trials. However, there are several generic challenges involved with conducting research protocols in the nursing home setting, including observational, quality improvement, and interventional cohort studies. These challenges involve recruitment of nursing homes to participate, staff turnover issues, subject consent procedures, blinded surveillance for outcomes, high mortality rates of subjects, and unique sample size considerations (see Table 1).
Table 1.
Challenges in Nursing Home Research
| Unique Challenge | Suggested Strategies | Advantages | Disadvantages |
|---|---|---|---|
| Recruitment of nursing homes | Partnering with administrators | Building relationships | Time consuming for principal investigator |
| Recruitment of subjects through surrogate consent | Letter, phone call, and group meeting contacts with surrogates | Higher recruitment rates | Time consuming for research staff |
| Engagement of nursing home staff | Educational sessions, professional incentives, and personal incentives | Higher recruitment and retention rates, improved protocol adherence | Cost, time consuming for research staff, time consuming for nursing staff |
| High turnover of nursing home staff | Repeated in-service sessions | Improved protocol adherence | Time consuming for research staff |
| Surveillance for outcomes and adverse events | Educational sessions, professional incentives, and personal incentives | Improved outcome detection | Cost, time consuming for research staff, time consuming for nursing staff |
| High attrition rate of participants | Increase recruitment of participants | Sustain power of study | Increase need for resources of research personnel |
Approaching Nursing Home Leadership to Participate in Research
In contrast to research in community dwelling or hospital cohorts, the first challenge in nursing home research is engaging the leadership of nursing homes to understand the need for research of common infectious diseases, the benefits of creating new knowledge, and the value of participation in developing improved models of care and disease prevention [16, 21, 25]. Some nursing homes are owned by larger corporations while others are managed as small family businesses. The primary individuals in leadership positions responsible for the day-to-day functions at a home typically include the administrator, director of nurses, and a physician medical director. Patient care roles within individual homes are staffed primarily by nurses and nurses’ aides, with frequent outsourcing of specialty needs (e.g., dental care, podiatry services, radiology, and clinical laboratory testing). Due to the common fiscal instability of nursing homes, inadequate staffing, and regulatory burdens, there is a disturbingly high turnover of ownership, administrators, and nursing staff [26]. Therefore, a nursing home may agree to participate in a study initially, but by the time a study is ready to begin recruiting subjects, the leadership may have changed and efforts and resources are required to repeatedly solicit participation. In one of our recent experiences, eligibility screening had begun at one nursing home and two days later, the administrator and director of nurses abruptly resigned causing an indefinite delay in the initiation of the project at that nursing home (ClinicalTrials.gov Identifier NCT01033383). Concerns of nursing home leadership when considering participation in research include: interruption of daily activities for nurses and residents, time commitment required by their staff for study participation, privacy regulations (i.e., HIPAA violations), perceived increased risk of litigation, and how research participation may complicate individual state audits. Nonetheless, our experience has been that the majority of administrative leaders of nursing homes are enthusiastic about participation in infectious disease research, particularly protocols that emphasize practical approaches to disease prevention. Efforts by investigators to meet personally with administrators, directors and assistant directors of nursing, infection control nurses, and medical directors, to educate them regarding the imperative of the investigative question, to have open lines of continuous communication, and to provide incentives (e.g. certificates of research participation to demonstrate during state audits), all represent time well spent to ensure a continued partnership and rigorous study completion.
Recruitment of Nursing Home Residents as Research Subjects
Despite the almost uniform enthusiasm by administrative leaders of nursing homes, subject recruitment remains a challenge for several reasons. First, the nursing staff members primarily affected by the actual conduct of the study are often initially less enthusiastic than their administrative leaders. Staff members may perceive investigators as threatening observers of the care they provide, and intruders who will create more work for an already overburdened group of caregivers [27]. Since nursing home residents and families often have their most frequent contact with nursing staff members, the nursing staff perception and enthusiasm for any research project can affect consent rates and recruitment efforts. Therefore, incentives to encourage participation by nursing staff in nursing home studies are often an essential component, improve their perception of the study, and translate to more encouragement of residents and families to participate. Second, the high prevalence of dementia among nursing home residents requires surrogate consent to participate for the vast majority of eligible subjects [13, 17]. Surrogate consent procedures can be arduous in that consent forms must be mailed to designated proxies, follow up phone calls are required to answer any questions or concerns, and signed consent forms must be mailed back to investigators. Additionally, after obtaining proxy consent, direct verbal assent to participate from the subject is necessary prior to enrollment. This consent/assent procedure is more time consuming and requires more staff resources than in other research settings, but it is not insurmountable once a standard protocol is developed for an individual study. Consent rates in observational studies tend to be higher (85–95%) [13, 16–17], than for interventional studies (32–44%) in nursing homes [24–25], but the ranges are very similar to consent rates in community cohorts. Third, because of the frailty and high annual mortality rates of nursing home residents, drop-outs are common. Therefore, recruitment is often necessary not only at the beginning of the study in an individual home (i.e., “prevalent subject recruitment”), but at pre-defined intervals after the study begins to account for losses (i.e., “incident subject recruitment”) [25]. These additional “incident subjects” are typically new residents who enter the home after the study has begun, replacing previous residents who have died or transferred out of the home. These repeated waves of recruitment at each nursing home result in increased burden on study staff members, but they represent an extremely valuable strategy to achieve necessary sample sizes required for both observational and intervention studies.
Surveillance for Infectious Disease Outcomes
As for any cohort study, surveillance for clinical outcomes (e.g., to assess risk factors, prognosis, and functional status) is a critical task [28]. One distinct advantage for outcome surveillance among nursing home residents is their grouped residence within the home. This fosters a closed cohort with easy access to surveillance data without concerns of being lost to follow up as may happen in community cohorts. In addition, because these residents are in need of long-term care, prospective surveillance of outcomes over long periods of time is possible. This duration of follow-up is less feasible in the inpatient hospital setting where length of stay is diminishing. A second advantage for outcome surveillance is the mandatory requirement for a minimum data set (i.e., MDS), a Medicare standardized questionnaire that must be completed on all nursing home residents upon admission and on a quarterly basis, to improve the quality of care in the nursing home setting [15–16, 29–31]. Data from the MDS includes information about acute infectious disease events, as well as functional changes in residents, making it a rich source of data for prospective surveillance. Large administrative datasets, such as the MDS, Medicare claims data, and OSCAR (Online Survey, Certification and Reporting – inspection survey data maintained by CMS) have been validated and can provide a wealth of knowledge regarding the magnitude of infections in the long-term care setting [32]. However, for many studies, outcome surveillance requires additional data not recorded on the MDS, and mandates solicitation of information directly from nursing staff or additional medical records.
One recognized challenge to research in the nursing home settings is that annual turnover is high among nursing home staff, and it can range from 20–150% annually [26]. Many shifts, including nights and weekends are covered by part-time casual employees who may be less invested in improving the quality of overall care at the home. This affects the conduct of any study, as education and reeducation of nursing staff regarding study goals and procedures can be burdensome to the research team. Nonetheless, it has been our experience that engagement of staff through educational sessions, one-on-one feedback, and incentives (e.g., providing training certification, gift cards) can be highly successful in obtaining their participation in overall study objectives and procedures.
Specific Challenges Unique to Randomized Trials
There are several challenges which are specific to the conduct of randomized clinical trials (RCTs) in the nursing home setting. First, sample size calculations require more than the outcome event rate, anticipated effect of an intervention, the alpha error, and the study power. Because of the high attrition rate of participants (i.e., due to death), more subjects must be recruited to generate the number of outcome events hypothesized for a study. Also, given that nursing home residents reside in grouped quarters that can be considered “clusters”, where their routine care and exposures make them less “independent” individuals than community dwellers, sample size calculations require an “inflation factor” to account for the clustering. Many RCTs in nursing homes utilize a cluster design (i.e., homes are randomized to intervention vs. no intervention rather than randomizing individual subjects). This type of design is often necessary, and preferred, to prevent “contamination” of control subjects, (i.e., preventing the intervention from being adopted by control residents or providers at a home if individual randomization occurs) [20, 33]. Second, clustered randomization designs of clinical trials raise the risk of imbalance of baseline home characteristics. That is, it is more likely that 10 randomized nursing homes are imbalanced at baseline (i.e., by staffing patterns, quality of routine care, annual outcome events) than 200 individually randomized subjects recruited from those homes. Therefore, stratification of homes before randomization (e.g., based on measures of quality of care available in publically available databases) is often needed to promote balance. For example, in an ongoing trial to test the effectiveness of enhanced oral care in preventing pneumonia in nursing home residents, the clustered randomization of homes was preceded by stratification based on number of minutes per day that nursing staff spend with individual residents (ClinicalTrials.gov identifier: NCT00975780). Third, cluster designs can create challenges in maintaining the blinding of study staff who are involved in the ongoing recruitment of subjects and assessment of clinical outcomes. Therefore, research staff in the field often require separation into distinct recruitment/assessment and intervention/education teams. Timing of home visits by the intervention/education team must be scheduled separately to prevent un-blinding of the recruitment/assessment team who are doing surveillance for outcome events. Finally, interruptions in the clinical trial protocol are possible during potential state audits, receivership of homes for financial issues, and infectious disease outbreaks (e.g., norovirus, C. difficile).
In summary, nursing home residents are a vastly understudied, vulnerable, and growing segment of our society that is particularly susceptible to infectious diseases. Given the aging of the population with growing functional disability, there is a public health need to investigate infectious diseases in this setting. Evolving options to provide long-term care (e.g., nursing homes, rehabilitation facilities, dementia units, assisted living) provide expanded avenues for investigation. Unique considerations given the goals of care, quality of life, functional outcomes, and life expectancy add to the scientific complexity and methodological challenges of designing an appropriate research protocol [28]. Although challenges exist, there are enormous opportunities for research. With careful attention to the unique needs of nursing home residents, and by maintaining positive relationships with nursing home leadership and surrogates, obstacles are surmountable and new knowledge can be created to improve an emerging major public health problem.
Acknowledgements
MJM is supported by NIH/NIA K23 AG028691, Claude D. Pepper Older Americans Independence Center (P30 AG21342), Atlantic Philanthropies, IDSA/NFID, John A. Hartford Foundation, Association of Specialty Professors, and CTSA Grant Number UL1 RR024139 from the National Center for Research Resources (NCRR). VJQ is supported by NIH/NIA R01 AG030575.
Footnotes
Potential Conflicts of Interest: V.Q. has served as an educational speaker for Pri-Med in partnership with the American College of Physicians, and is a consultant to the Center for Medical Excellence and Research Experts.
References
- 1.(PHS) D, editor. US Department of Health and Human Services (DHHS) PHS, National Center for Health Statistics. Health United States 1985. Hyattsville, MD: 1985. pp. 86–1232. [Google Scholar]
- 2.Centers for Diseases Control and Prevention. Public Health and Aging: Trends in Aging -- United States and Worldwide. MMWR Morb Mortal Wkly Rep. 2003 February 14;52(6):101–106. 2003. [PubMed] [Google Scholar]
- 3.Notice to Readers: National Nursing Home Week -- May 8–14, 2005. MMWR Morb Mortal Wkly Rep. 2005 May 6;54(17):438. 2005. [Google Scholar]
- 4.The National Nursing Home Survey: 2004 Overview. [Accessed June 1, 2010]; Available at: http://www.cdc.gov/nchs/data/series/sr_13/sr13_167.pdf. [PubMed]
- 5.High K. Immunizations in older adults. Clin Geriatr Med. 2007 Aug;23(3):669–685. doi: 10.1016/j.cger.2007.03.007. viii–ix. [DOI] [PubMed] [Google Scholar]
- 6.van Duin D, Allore HG, Mohanty S, et al. Prevaccine determination of the expression of costimulatory B7 molecules in activated monocytes predicts influenza vaccine responses in young and older adults. J Infect Dis. 2007 Jun 1;195(11):1590–1597. doi: 10.1086/516788. [DOI] [PubMed] [Google Scholar]
- 7.van Duin D, Mohanty S, Thomas V, et al. Age-associated defect in human TLR-1/2 function. J Immunol. 2007 Jan 15;178(2):970–975. doi: 10.4049/jimmunol.178.2.970. [DOI] [PubMed] [Google Scholar]
- 8.Loeb MB, Craven S, McGeer AJ, et al. Risk factors for resistance to antimicrobial agents among nursing home residents. Am J Epidemiol. 2003 Jan 1;157(1):40–47. doi: 10.1093/aje/kwf173. [DOI] [PubMed] [Google Scholar]
- 9.High KP, Bradley SF, Gravenstein S, et al. Clinical practice guideline for the evaluation of fever and infection in older adult residents of long-term care facilities: 2008 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009 Jan 15;48(2):149–171. doi: 10.1086/595683. [DOI] [PubMed] [Google Scholar]
- 10.Curns AT, Holman RC, Sejvar JJ, Owings MF, Schonberger LB. Infectious disease hospitalizations among older adults in the United States from 1990 through 2002. Arch Intern Med. 2005 Nov 28;165(21):2514–2520. doi: 10.1001/archinte.165.21.2514. [DOI] [PubMed] [Google Scholar]
- 11.Jackson ML, Neuzil KM, Thompson WW, et al. The burden of community-acquired pneumonia in seniors: results of a population-based study. Clin Infect Dis. 2004 Dec 1;39(11):1642–1650. doi: 10.1086/425615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fry AM, Shay DK, Holman RC, Curns AT, Anderson LJ. Trends in hospitalizations for pneumonia among persons aged 65 years or older in the United States, 1988–2002. JAMA. 2005 Dec 7;294(21):2712–2719. doi: 10.1001/jama.294.21.2712. [DOI] [PubMed] [Google Scholar]
- 13.Quagliarello V, Ginter S, Han L, Van Ness P, Allore H, Tinetti M. Modifiable risk factors for nursing home-acquired pneumonia. Clin Infect Dis. 2005 Jan 1;40(1):1–6. doi: 10.1086/426023. [DOI] [PubMed] [Google Scholar]
- 14.Litwin MS, Saigal CS, Beerbohm EM. The burden of urologic diseases in America. J Urol. 2005 Apr;173(4):1065–1066. doi: 10.1097/01.ju.0000156555.89385.54. [DOI] [PubMed] [Google Scholar]
- 15.Rogers MA, Mody L, Chenoweth C, Kaufman SR, Saint S. Incidence of antibiotic-resistant infection in long-term residents of skilled nursing facilities. Am J Infect Control. 2008 Sep;36(7):472–475. doi: 10.1016/j.ajic.2007.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mody L, Kauffman CA, Donabedian S, Zervos M, Bradley SF. Epidemiology of Staphylococcus aureus colonization in nursing home residents. Clin Infect Dis. 2008 May 1;46(9):1368–1373. doi: 10.1086/586751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Juthani-Mehta M, Quagliarello V, Perrelli E, Towle V, Van Ness PH, Tinetti M. Clinical features to identify urinary tract infection in nursing home residents: a cohort study. J Am Geriatr Soc. 2009 Jun;57(6):963–970. doi: 10.1111/j.1532-5415.2009.02227.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Boscia JA, Kobasa WD, Abrutyn E, Levison ME, Kaplan AM, Kaye D. Lack of association between bacteriuria and symptoms in the elderly. Am J Med. 1986 Dec;81(6):979–982. doi: 10.1016/0002-9343(86)90391-8. [DOI] [PubMed] [Google Scholar]
- 19.Nicolle LE, Mubareka S, Simor A, et al. Variation in mortality rates among long-term care facilities for residents with lower respiratory tract infection. Infect Control Hosp Epidemiol. 2008 Aug;29(8):754–759. doi: 10.1086/590123. [DOI] [PubMed] [Google Scholar]
- 20.Loeb M, Carusone SC, Goeree R, et al. Effect of a clinical pathway to reduce hospitalizations in nursing home residents with pneumonia: a randomized controlled trial. JAMA. 2006 Jun 7;295(21):2503–2510. doi: 10.1001/jama.295.21.2503. [DOI] [PubMed] [Google Scholar]
- 21.Loeb M, Brazil K, Lohfeld L, et al. Effect of a multifaceted intervention on number of antimicrobial prescriptions for suspected urinary tract infections in residents of nursing homes: cluster randomised controlled trial. BMJ. 2005 Sep 24;331(7518):669. doi: 10.1136/bmj.38602.586343.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Nicolle LE, Mayhew WJ, Bryan L. Prospective randomized comparison of therapy and no therapy for asymptomatic bacteriuria in institutionalized elderly women. Am J Med. 1987 Jul;83(1):27–33. doi: 10.1016/0002-9343(87)90493-1. [DOI] [PubMed] [Google Scholar]
- 23.Loeb M, Hunt D, O'Halloran K, Carusone SC, Dafoe N, Walter SD. Stop orders to reduce inappropriate urinary catheterization in hospitalized patients: a randomized controlled trial. J Gen Intern Med. 2008 Jun;23(6):816–820. doi: 10.1007/s11606-008-0620-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Quagliarello V, Juthani-Mehta M, Ginter S, Towle V, Allore H, Tinetti M. Pilot testing of intervention protocols to prevent pneumonia in nursing home residents. J Am Geriatr Soc. 2009 Jul;57(7):1226–1231. doi: 10.1111/j.1532-5415.2009.02311.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kiel DP, Magaziner J, Zimmerman S, et al. Efficacy of a hip protector to prevent hip fracture in nursing home residents: the HIP PRO randomized controlled trial. Jama. 2007 Jul 25;298(4):413–422. doi: 10.1001/jama.298.4.413. [DOI] [PubMed] [Google Scholar]
- 26.Buckwalter KC, Grey M, Bowers B, et al. Intervention research in highly unstable environments. Res Nurs Health. 2009 Feb;32(1):110–121. doi: 10.1002/nur.20309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mody L, Miller DK, McGloin JM, et al. Recruitment and retention of older adults in aging research. J Am Geriatr Soc. 2008 Dec;56(12):2340–2348. doi: 10.1111/j.1532-5415.2008.02015.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.High KP, Bradley S, Loeb M, Palmer R, Quagliarello V, Yoshikawa T. A new paradigm for clinical investigation of infectious syndromes in older adults: assessment of functional status as a risk factor and outcome measure. Clin Infect Dis. 2005 Jan 1;40(1):114–122. doi: 10.1086/426082. [DOI] [PubMed] [Google Scholar]
- 29.Stevenson KB. Regional data set of infection rates for long-term care facilities: description of a valuable benchmarking tool. Am J Infect Control. 1999 Feb;27(1):20–26. doi: 10.1016/s0196-6553(99)70070-2. [DOI] [PubMed] [Google Scholar]
- 30.Stevenson KB, Moore J, Colwell H, Sleeper B. Standardized infection surveillance in long-term care: interfacility comparisons from a regional cohort of facilities. Infect Control Hosp Epidemiol. 2005 Mar;26(3):231–238. doi: 10.1086/502532. [DOI] [PubMed] [Google Scholar]
- 31.Stevenson KB, Moore JW, Sleeper B. Validity of the minimum data set in identifying urinary tract infections in residents of long-term care facilities. J Am Geriatr Soc. 2004 May;52(5):707–711. doi: 10.1111/j.1532-5415.2004.52206.x. [DOI] [PubMed] [Google Scholar]
- 32.Hawes C, Morris JN, Phillips CD, Mor V, Fries BE, Nonemaker S. Reliability estimates for the Minimum Data Set for nursing home resident assessment and care screening (MDS) Gerontologist. 1995 Apr;35(2):172–178. doi: 10.1093/geront/35.2.172. [DOI] [PubMed] [Google Scholar]
- 33.Loeb M, Brazil K, Lohfeld L, et al. Optimizing antibiotics in residents of nursing homes: protocol of a randomized trial. BMC Health Serv Res. 2002 Sep 3;2(1):17. doi: 10.1186/1472-6963-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]


