Abstract
Phosphodiesterase type-5 inhibitor (PDE5-i) drugs were first marketed in 1998 (sildenafil) for 'ondemand' treatment of male erectile dysfunction (ED) of any origin. They selectively inhibit intrapenile PDE5 isoenzyme which in turn increases intracellular cyclic guanosine monophosphate levels, thus resulting in prolonged relaxation of cavernosum smooth muscle cells and facilitating the erectile process. Since 2003, two new molecules (tadalafil and vardenafil) have been introduced, resulting in greater interest in these compounds and leading patients to ask for more prescriptions from their doctors. The vast use of PDE5-i in diabetic and cardiovascular ED patients led researchers to investigate their possible extra sexual effects. Several studies investigating their effects on endothelium, coronary and pulmonary circulation, inferior oesophageal sphincter and kidney functions have appeared and, finally, sildenafil was approved for the treatment of pulmonary arterial hypertension. Recent animal studies highlighted a possible interaction between chronic PDE5 inhibition and glucose homeostasis which occurs through a marked improvement of high fat diet induced insulin resistance. If this data is extended to humans, a new scenario will be opened for the chronic use of PDE5-i for sexual rehabilitation along with cardiovascular and metabolic benefits.
Keywords: Endothelium, Insulin, Cardio protection, Diabetes, Atherosclerosis, Erectile dysfunction
INTRODUCTION
Erectile dysfunction (ED) is the persistent inability to achieve and maintain an erection adequate for satisfactory sexual performance[1]. Its prevalence is underestimated because the patients treated (less than 20% out of total) are considered as only the ‘tip of the iceberg’[2]. The probability of ED increases with ageing and the presence of diabetes mellitus, hypertension, hypercholesterolemia, ischemic cardiac disease, depression and obesity. Although cigarette smoking is not a direct causative factor, it may increase the risk of presenting with peripheral vascular disease and hypertension. Drugs and alcohol abuse may also increase the risk of ED. Based on our data, as more than 70% of the male population affected by moderate to severe ED complain of concomitant diseases, we conclude that it is a symptom and not a disease itself[3]. The probability of manifested severe ED increases two-fold in the presence of the above mentioned diseases, thus suggesting that modification of associated risk factors may contribute to improve ED in internal medicine patients.
Phosphodiesterase type-5 inhibitors (PDE5-i) are currently used in the treatment of male ED. Sildenafil, vardenafil and tadalafil all inhibit PDE5 at the level of the corpus cavernosum[4] with different onset of action, bioavailability and pharmacokinetic profiles (Table 1)[5]. However, tadalafil is innovative due to its longer half-life (17.5 and proven efficacy rates after 36 h) and highest selectivity (Table 2). These molecules are contraindicated in the presence of class New York Heart Association III/IV cardiac disease and in all men consuming nitric oxide (NO)-derivatives in any pharmaceutical form. In the remaining cases, they can be used safely with an overall response rate of approximately 70%-80%; adverse events are dose-related, mild-moderate in intensity (mainly headache 15%-20%, gastric discomfort 10% and rhinitis 5%-10%) and tend to disappear over the time[6]. Since tadalafil has a longer half-life but similar onset of action when compared to sildenafil and vardenafil, we can assume that it can be considered the ideal drug for men who do not wish to be tied to pill consumption for sexual activity, thus contributing to the elimination of the state of performance-induced anxiety frequently encountered in almost all sexual dysfunctions.
Table 1.
Pharmacological profile of oral PDE5-i at therapeutic dosage for ED
| Parameter | Sildenafil 100 mg | Tadalafil 20 mg | Vardenafil 20 mg |
| Tmax (h) | 1.16 ± 0.99 | 2 | 0.66 (0.250-3.0) |
| T1/2 (h) | 3.82 ± 0.84 | 17.5 | 3.94 ± 1.31 |
| C (max ng/m) | 327 ± 236 | 378 | 20.9 ± 1.83 |
| AUC (ng × h/m) | 1963 ± 859 | 8066 | 74.5 ± 1.82 |
PDE5-i: Phosphodiesterase type-5 inhibitor; ED: Erectile dysfunction.
Table 2.
In vitro enzymatic inhibition activity of the marketed PDE5-i (IC50 nmol/L)
| PDE isoform | Sildenafil | Tadalafil | Vardenafil |
| PDE-1 | 60 | > 10 000 | 257 |
| PDE-2 | > 10 000 | > 10 000 | > 10 000 |
| PDE-3 | 2 600 | > 10 000 | 3 600 |
| PDE-4 | 1 800 | > 10 000 | 5 700 |
| PDE-5 | 3.8 | 1 | 0.7 |
| PDE-6 | 7.4 | 780 | 15.7 |
SYSTEMIC EFFECTS OF PDE5 INHIBITORS
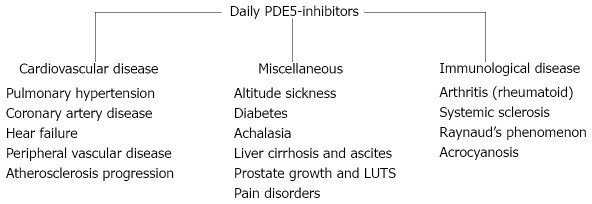
Since PDE5-i is highly efficacious and widely used in treating male ED, it is a timely hypothesis that it may exert important systemic effects at the endothelial level[7]. To further investigate this, several studies have investigated the effects of sildenafil on blood pressure variations mainly due to its vasodilatory effects and possible interactions with anti-hypertensive drugs[8]. Sildenafil did not decrease systemic arterial pressure because of its effect on renal PDE5 inactivation which elicits renin production, thus counterbalancing hypotensive effects[9]. Also, subsequent confirmatory studies carried out in men with liver cirrhosis and ascites suggested the activation of the renin-angiotensin-aldosterone pathway as a possible regulatory mechanism[10]. Further studies in an animal cirrhosis model clearly concluded that both acute and chronic sildenafil administration has a natriuretic effect, helping to prevent water retention associated with liver cirrhosis[11]. The recent approval of sildenafil for the treatment of pulmonary arterial hypertension (PAH) opens new applications for this class of drug (Figure 1), considering its efficacy in such a difficult-to-treat population usually refractory to conventional therapies[12]. Recently, new acquisition data revealed that tadalafil[13] and vardenafil[14] are equally safe and effective for the treatment of PAH. In a rat model of chronic NO deprivation where hypertension and aggravation of post-ischemic ventricular dysfunction are associated with loss of vascular endothelium-relaxant function, sildenafil provided significant cardiovascular protection, primarily by maintaining tissue cyclic guanosine monophosphate (cGMP) levels[15,16]. It is important to remember that sildenafil efficacy has been already demonstrated in idiopathic refractory achalasia[17] and Raynaud’s phenomenon[18]. Tadalafil has also been demonstrated to be effective in improving Raynaud’s attacks in men with systemic sclerosis[19]. However, because NO promotes upper airway congestion, muscle relaxation and pulmonary vasodilatation, it is remarkable that in patients with severe obstructive sleep apnoea, a single 50-mg dose of sildenafil at bedtime worsens respiratory and desaturation events[20].
Figure 1.
Potential applications of PDE5 inhibitors in internal medicine.
Since endothelial dysfunction plays a key role in the pathogenesis of the atherosclerotic process, growing interest in the effects of PDE5-i in preventing atherosclerosis and the vascular endothelium damage has developed[21]. The event that triggers endothelial dysfunction is represented by the reduction of overall antioxidant pool with the consequent reduced response to oxidative stress and the activation of several pro-atherogenic processes[22] (Table 3): (1) reduction of NO bioavailability; (2) increased levels of circulating free fatty acids with subsequent sub-endothelial storage of lipid depots; and (3) increased smooth muscle cell proliferation of the media layer of the vascular wall[23]. Pro-inflammatory and infective processes may in turn contribute to activate and amplify the acute endothelial injury, thus perpetuating a vicious circle. In early atherogenic lesions, endothelial dysfunction causes adhesion and migration of monocytes and T-lymphocytes in the vascular inner layer in response to increased endothelial production of intercellular molecules, i.e. selectin, Vascular Cellular Adhesion Molecule-1 and Inter-Cellular Adhesion Molecule-1 (ICAM-1)[24]. Although data regarding the effects of PDE5-i on endothelial function are scarce, pilot studies using chronic administration of sildenafil have shown improvements both in endothelial[25] and cardiac functions[26]. Subsequent studies with an alternative dosing regimen of tadalafil (every other day) confirmed patients’ preference in the treatment of ED[27]. By using a once-a-day dosing in initially non-responders to on-demand treatment, tadalafil was able to restore potency in more than 30%[28]. In another study by Porst et al[29], daily tadalafil at low dosages (5 and 10 mg) was safe and effective with almost 50% of men and produced normalization of erectile function. These benefits were confirmed by our group in a recent study in men with ED of broad etiology[30]. In that study, it was demonstrated that the rehabilitative effects of chronic tadalafil on vascular function occurs via improvement of surrogate markers of endothelial function, i.e. C-reactive protein, endothelin-1 and ICAM-1. This led to marked improvement of flow-mediated-vasodilatation (FMD) at the level of the cavernous arteries as well as better inflow to the penis, as shown by ultrasound technique, when compared with on-demand regimes. Moreover, this study was the first one to report consistent improvements in morning erections as a possible mechanism for rehabilitative effects which persisted even after 15 d withdrawal. The same group confirmed those results in men without ED and increased cardiovascular risk[31]. Another possible explanation of increased endothelial function comes from pioneer studies suggesting a direct effect of PDE5-i on modulating the number of circulating endothelial progenitor cells (EPCs). In men with ED, this number is reduced compared with controls and studies have demonstrated that chronic tadalafil significantly increases EPCs[32], thus leading to improvements in brachial FMD. Overall, these data give the rationale for the chronic use of PDE5-i in men with ED and cardiovascular risk factors[33]. Attention has been given to the endocrine effects of PDE5-i administration. In a recent study[34], the effects of the administration of sildenafil and tadalafil on steroid hormones were assessed for three months in 80 patients with ED. Total and free testosterone rose significantly in subjects using tadalafil, probably due to a higher number of sexual intercourses per month allowed by the long-acting drug, speculated to cause an indirect and sustained activation of the hypothalamic-pituitary-testicular axis. However, our studies demonstrated that this rise is lost after 12 mo of continuous tadalafil consumption (3 pills per wk)[35]. Subsequent studies carried out in human adipocytes ex vivo suggest that, during acute exposure to tadalafil, an aromatase activation occurs that causes an increase in estradiol concentrations (data not published) that may be responsible for vascular beneficial effects of the drug. Thus, the hypothesis that tadalafil may modulate aromatase activity in humans during acute and chronic administration highlights potential implications for the treatment of prostate and breast cancer. Evidence-based medicine with off-label use of PDE5 inhibitors is scarce but pilot studies suggest that chronic PDE5-i use determines better endothelial function and may slow down progression of atherosclerosis, especially in men with organic ED and endothelial dysfunction at baseline. This latter effect may be a consequence of improvements in FMD (brachial and cavernous arteries), in biomarkers of endothelial function, in the number of EPCs and finally, in testosterone/estradiol ratio[36].
Table 3.
Causes and main interventions in endothelial dysfunction
| Factors associated with endothelial dysfunction | Interventions to correct endothelial dysfunction |
| Aging | L-arginine |
| Male sex | Estrogens |
| Cigarette smoking | Smoking cessation |
| History of CHD | Antioxidants |
| Low HDL- and high LDL-COL | Statins |
| Hypertension | ACE-i |
| Hyperomocysteinemia | Homocysteine lowering (folates) |
| Diabetes/obesity | Exercise |
| Erectile dysfunction | PDE5-i |
METABOLIC EFFECTS OF PDE5 INHIBITORS
Besides the above mentioned vascular systemic effects, emerging data suggest that PDE5-i may also impact on metabolic parameters. It is known that NO plays an important role in mediating insulin-induced effects, especially on glucose uptake at the muscular level[37]. Knock-out mice models for endothelial NO-synthase (eNOS) are insulin-resistant[38,39] and their treatment with drugs that inhibit NO formation produces inhibitory effects on insulin-mediated glucose uptake[40]. Also, in a diabetic human model where eNOS synthesis is reduced, insulin-resistance frequently occurs[41]. Given the important role of the NO-cGMP pathway in muscular metabolism, the effects of sildenafil on insulin function has been investigated in an animal model of insulin-resistance in vivo. Chronic sildenafil administration (12 wk) counteracted the detrimental effects of a high-fat diet on endothelial function and insulin resistance by improving energy balance and insulin function. This effect persisted even in the presence of NO donors, suggesting direct effects of sildenafil on metabolism other than eNOS activation[42]. In this regard, a pilot study in humans has been carried out using tadalafil and it demonstrated that in ED men who are not insulin resistant, a 30% increase of basal insulin secretion occurs[28]. However, in that study, insulin sensitivity was not assessed. Overall, these preliminary suggest a fascinating interplay between energy balance, insulin action and PDE5-i and may give new potential applications to this class of drugs (Figure 1).
CONCLUSION
11 years after the sildenafil launch, ED is still an under diagnosed and under treated condition in the internal medicine setting, probably as it is perceived by the patient as a stress or age related condition. ED alters self-esteem and quality of life for patients and their partners and should be considered a symptom of an underlying condition, which can often lead to a diagnosis of organic disease. Each physician should consider the close relationship between internal medicine diseases and the pathophysiology of ED and each intervention should be intended to modify lifestyle and concomitant drugs with anti-erectile properties. Taking preliminary data into account, it can be postulated that PDE5-i may exert systemic other than penile rehabilitative effects, as well as important effects on pulmonary, gastrointestinal and metabolic systems. However, extra-sexual applications are not evidence-based and cost-effective at the moment. In the near future, the approval of new PDE5-i molecules will allow reduced costs related to investigational protocols targeted for a larger use of these drugs.
Footnotes
Peer reviewers: Mohammad Abdollahi, Professor, Faculty of Pharmacy, Tehran University of Medical Sciences, Tehran 1417614411, Iran; Cevdet Kaya, MD, Associate Professor, Haydarpasa Numune Training and Research Hospital, Department of Urology, Kadikoy, Istanbul, Turkey
S- Editor Zhang HN L- Editor Roemmele A E- Editor Liu N
References
- 1.NIH Consensus Conference. Impotence. NIH Consensus Development Panel on Impotence. JAMA. 1993;270:83–90. [PubMed] [Google Scholar]
- 2.Parazzini F, Menchini Fabris F, Bortolotti A, Calabrò A, Chatenoud L, Colli E, Landoni M, Lavezzari M, Turchi P, Sessa A, et al. Frequency and determinants of erectile dysfunction in Italy. Eur Urol. 2000;37:43–49. doi: 10.1159/000020098. [DOI] [PubMed] [Google Scholar]
- 3.Aversa A, Isidori AM, Gianfrilli D, Greco EA, Graziottin A, Zizzo G, Lenzi A, Fabbri A. Are subjects with erectile dysfunction aware of their condition? Results from a retrospective study based on an Italian free-call information service. J Endocrinol Invest. 2004;27:548–556. doi: 10.1007/BF03347477. [DOI] [PubMed] [Google Scholar]
- 4.Burnett AL, Lowenstein CJ, Bredt DS, Chang TS, Snyder SH. Nitric oxide: a physiologic mediator of penile erection. Science. 1992;257:401–403. doi: 10.1126/science.1378650. [DOI] [PubMed] [Google Scholar]
- 5.Aversa A, Bruzziches R, Pili M, Spera G. Phosphodiesterase 5 inhibitors in the treatment of erectile dysfunction. Curr Pharm Des. 2006;12:3467–3484. doi: 10.2174/138161206778343046. [DOI] [PubMed] [Google Scholar]
- 6.Aversa A, Pili M, Fabbri A, Spera E, Spera G. Erectile dysfunction: expectations beyond phosphodiesterase type 5 inhibition. J Endocrinol Invest. 2004;27:192–206. doi: 10.1007/BF03346268. [DOI] [PubMed] [Google Scholar]
- 7.Aversa A, Caprio M, Rosano GM, Spera G. Endothelial effects of drugs designed to treat erectile dysfunction. Curr Pharm Des. 2008;14:3768–3778. doi: 10.2174/138161208786898725. [DOI] [PubMed] [Google Scholar]
- 8.Caprio M, Mammi C, Jaffe IZ, Zennaro MC, Aversa A, Mendelsohn ME, Fabbri A, Rosano GM. The mineralocorticoid receptor in endothelial physiology and disease: novel concepts in the understanding of erectile dysfunction. Curr Pharm Des. 2008;14:3749–3757. doi: 10.2174/138161208786898743. [DOI] [PubMed] [Google Scholar]
- 9.Chiu YJ, Reid IA. Effect of sildenafil on renin secretion in human subjects. Exp Biol Med (Maywood) 2002;227:620–625. doi: 10.1177/153537020222700810. [DOI] [PubMed] [Google Scholar]
- 10.Thiesson HC, Jensen BL, Jespersen B, Schaffalitzky de Muckadell OB, Bistrup C, Walter S, Ottosen PD, Veje A, Skøtt O. Inhibition of cGMP-specific phosphodiesterase type 5 reduces sodium excretion and arterial blood pressure in patients with NaCl retention and ascites. Am J Physiol Renal Physiol. 2005;288:F1044–F1052. doi: 10.1152/ajprenal.00142.2004. [DOI] [PubMed] [Google Scholar]
- 11.Ghali-Ghoul R, Tahseldar-Roumieh R, Sabra R. Effect of chronic administration of sildenafil on sodium retention and on the hemodynamic complications associated with liver cirrhosis in the rat. Eur J Pharmacol. 2007;572:49–56. doi: 10.1016/j.ejphar.2007.05.068. [DOI] [PubMed] [Google Scholar]
- 12.Karatza AA, Narang I, Rosenthal M, Bush A, Magee AG. Treatment of primary pulmonary hypertension with oral sildenafil. Respiration. 2004;71:192–194. doi: 10.1159/000076684. [DOI] [PubMed] [Google Scholar]
- 13.Galiè N, Brundage BH, Ghofrani HA, Oudiz RJ, Simonneau G, Safdar Z, Shapiro S, White RJ, Chan M, Beardsworth A, et al. Tadalafil therapy for pulmonary arterial hypertension. Circulation. 2009;119:2894–2903. doi: 10.1161/CIRCULATIONAHA.108.839274. [DOI] [PubMed] [Google Scholar]
- 14.Jing ZC, Jiang X, Wu BX, Xu XQ, Wu Y, Ma CR, Wang Y, Yang YJ, Pu JL, Gao W. Vardenafil treatment for patients with pulmonary arterial hypertension: a multicentre, open-label study. Heart. 2009;95:1531–1536. doi: 10.1136/hrt.2009.169417. [DOI] [PubMed] [Google Scholar]
- 15.Rossoni G, Manfredi B, De Gennaro Colonna V, Berti M, Guazzi M, Berti F. Sildenafil reduces L-NAME-induced severe hypertension and worsening of myocardial ischaemia-reperfusion damage in the rat. Br J Pharmacol. 2007;150:567–576. doi: 10.1038/sj.bjp.0707131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zahra GR, Elham DF, Atousa A, Hadi E, Azadeh M, Seyed NO, Mohammad A. Protection by cAMP and cGMP phosphodiesterase inhibitors of diazinon-induced hyperglycemia and oxidative/nitrosative stress in rat Langerhans islets cells: Molecular evidence for involvement of non-cholinergic mechanisms. Pestic Biochem Physiol. 2007;87:261–270. [Google Scholar]
- 17.Bortolotti M, Mari C, Lopilato C, Porrazzo G, Miglioli M. Effects of sildenafil on esophageal motility of patients with idiopathic achalasia. Gastroenterology. 2000;118:253–257. doi: 10.1016/s0016-5085(00)70206-x. [DOI] [PubMed] [Google Scholar]
- 18.Fries R, Shariat K, von Wilmowsky H, Böhm M. Sildenafil in the treatment of Raynaud's phenomenon resistant to vasodilatory therapy. Circulation. 2005;112:2980–2985. doi: 10.1161/CIRCULATIONAHA.104.523324. [DOI] [PubMed] [Google Scholar]
- 19.Rosato E, Letizia C, Proietti M, Aversa A, Menghi G, Rossi C, Torella E, Cotesta D, Petramala L, Bruzziches R, et al. Plasma adrenomedullin and endothelin-1 levels are reduced and Raynaud's phenomenon improved by daily tadalafil administration in male patients with systemic sclerosis. J Biol Regul Homeost Agents. 2009;23:23–29. [PubMed] [Google Scholar]
- 20.Roizenblatt S, Guilleminault C, Poyares D, Cintra F, Kauati A, Tufik S. A double-blind, placebo-controlled, crossover study of sildenafil in obstructive sleep apnea. Arch Intern Med. 2006;166:1763–1767. doi: 10.1001/archinte.166.16.1763. [DOI] [PubMed] [Google Scholar]
- 21.Aversa A. Drugs targeted to improve endothelial function: clinical correlates between sexual and internal medicine. Curr Pharm Des. 2008;14:3698–3699. doi: 10.2174/138161208786898734. [DOI] [PubMed] [Google Scholar]
- 22.Khoshakhlagh P, Bahrololoumi-Shapourabadi M, Mohammadirad A, Ashtaral-Nakhai L, Minaie B and Abdollahi M. Beneficial effect of phosphodiesterase-5 inhibitor in experimental inflammatory bowel disease; molecular evidence for involvement of oxidative stress. Toxicol Mech Meth. 2007;17:281–288. doi: 10.1080/15376510601003769. [DOI] [PubMed] [Google Scholar]
- 23.Ross R. Atherosclerosis-an inflammatory disease. N Engl J Med. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 24.O'Brien KD, Allen MD, McDonald TO, Chait A, Harlan JM, Fishbein D, McCarty J, Ferguson M, Hudkins K, Benjamin CD. Vascular cell adhesion molecule-1 is expressed in human coronary atherosclerotic plaques. Implications for the mode of progression of advanced coronary atherosclerosis. J Clin Invest. 1993;92:945–951. doi: 10.1172/JCI116670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Desouza C, Parulkar A, Lumpkin D, Akers D, Fonseca VA. Acute and prolonged effects of sildenafil on brachial artery flow-mediated dilatation in type 2 diabetes. Diabetes Care. 2002;25:1336–1339. doi: 10.2337/diacare.25.8.1336. [DOI] [PubMed] [Google Scholar]
- 26.Gori T, Sicuro S, Dragoni S, Donati G, Forconi S, Parker JD. Sildenafil prevents endothelial dysfunction induced by ischemia and reperfusion via opening of adenosine triphosphate-sensitive potassium channels: a human in vivo study. Circulation. 2005;111:742–746. doi: 10.1161/01.CIR.0000155252.23933.2D. [DOI] [PubMed] [Google Scholar]
- 27.Mirone V, Costa P, Damber JE, Holmes S, Moncada I, Van Ahlen H, Wespes E, Cordell WH, Chan M, Lembo D, et al. An evaluation of an alternative dosing regimen with tadalafil, 3 times/week, for men with erectile dysfunction: SURE study in 14 European countries. Eur Urol. 2005;47:846–854; discussion 854. doi: 10.1016/j.eururo.2005.02.019. [DOI] [PubMed] [Google Scholar]
- 28.McMahon C. Efficacy and safety of daily tadalafil in men with erectile dysfunction previously unresponsive to on-demand tadalafil. J Sex Med. 2004;1:292–300. doi: 10.1111/j.1743-6109.04042.x. [DOI] [PubMed] [Google Scholar]
- 29.Porst H, Giuliano F, Glina S, Ralph D, Casabé AR, Elion-Mboussa A, Shen W, Whitaker JS. Evaluation of the efficacy and safety of once-a-day dosing of tadalafil 5mg and 10mg in the treatment of erectile dysfunction: results of a multicenter, randomized, double-blind, placebo-controlled trial. Eur Urol. 2006;50:351–359. doi: 10.1016/j.eururo.2006.02.052. [DOI] [PubMed] [Google Scholar]
- 30.Aversa A, Greco E, Bruzziches R, Pili M, Rosano G, Spera G. Relationship between chronic tadalafil administration and improvement of endothelial function in men with erectile dysfunction: a pilot study. Int J Impot Res. 2007;19:200–207. doi: 10.1038/sj.ijir.3901513. [DOI] [PubMed] [Google Scholar]
- 31.Rosano GM, Aversa A, Vitale C, Fabbri A, Fini M, Spera G. Chronic treatment with tadalafil improves endothelial function in men with increased cardiovascular risk. Eur Urol. 2005;47:214–220; discussion 220-222. doi: 10.1016/j.eururo.2004.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Foresta C, Ferlin A, De Toni L, Lana A, Vinanzi C, Galan A, Caretta N. Circulating endothelial progenitor cells and endothelial function after chronic Tadalafil treatment in subjects with erectile dysfunction. Int J Impot Res. 2006;18:484–488. doi: 10.1038/sj.ijir.3901465. [DOI] [PubMed] [Google Scholar]
- 33.Kukreja RC. Cardiovascular protection with sildenafil following chronic inhibition of nitric oxide synthase. Br J Pharmacol. 2007;150:538–540. doi: 10.1038/sj.bjp.0707132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Carosa E, Martini P, Brandetti F, Di Stasi SM, Lombardo F, Lenzi A, Jannini EA. Type V phosphodiesterase inhibitor treatments for erectile dysfunction increase testosterone levels. Clin Endocrinol (Oxf) 2004;61:382–386. doi: 10.1111/j.1365-2265.2004.02108.x. [DOI] [PubMed] [Google Scholar]
- 35.Greco EA, Pili M, Bruzziches R, Corona G, Spera G, Aversa A. Testosterone:estradiol ratio changes associated with long-term tadalafil administration: a pilot study. J Sex Med. 2006;3:716–722. doi: 10.1111/j.1743-6109.2006.00264.x. [DOI] [PubMed] [Google Scholar]
- 36.Aversa A. Strategies to Improve Endothelial Function and its Clinical Relevance to Erectile Dysfunction. Eur Urol Suppl. 2009;8:71–79. [Google Scholar]
- 37.Duplain H, Burcelin R, Sartori C, Cook S, Egli M, Lepori M, Vollenweider P, Pedrazzini T, Nicod P, Thorens B, et al. Insulin resistance, hyperlipidemia, and hypertension in mice lacking endothelial nitric oxide synthase. Circulation. 2001;104:342–345. doi: 10.1161/01.cir.104.3.342. [DOI] [PubMed] [Google Scholar]
- 38.Shankar RR, Wu Y, Shen HQ, Zhu JS, Baron AD. Mice with gene disruption of both endothelial and neuronal nitric oxide synthase exhibit insulin resistance. Diabetes. 2000;49:684–687. doi: 10.2337/diabetes.49.5.684. [DOI] [PubMed] [Google Scholar]
- 39.Milani E, Nikfar S, Khorasani R, Zamani MJ, Abdollahi M. Reduction of diabetes-induced oxidative stress by phosphodiesterase inhibitors in rats. Comp Biochem Physiol C Toxicol Pharmacol. 2005;140:251–255. doi: 10.1016/j.cca.2005.02.010. [DOI] [PubMed] [Google Scholar]
- 40.Baron AD, Zhu JS, Marshall S, Irsula O, Brechtel G, Keech C. Insulin resistance after hypertension induced by the nitric oxide synthesis inhibitor L-NMMA in rats. Am J Physiol. 1995;269:E709–E715. doi: 10.1152/ajpendo.1995.269.4.E709. [DOI] [PubMed] [Google Scholar]
- 41.Kashyap SR, Roman LJ, Lamont J, Masters BS, Bajaj M, Suraamornkul S, Belfort R, Berria R, Kellogg DL Jr, Liu Y, et al. Insulin resistance is associated with impaired nitric oxide synthase activity in skeletal muscle of type 2 diabetic subjects. J Clin Endocrinol Metab. 2005;90:1100–1105. doi: 10.1210/jc.2004-0745. [DOI] [PubMed] [Google Scholar]
- 42.Ayala JE, Bracy DP, Julien BM, Rottman JN, Fueger PT, Wasserman DH. Chronic treatment with sildenafil improves energy balance and insulin action in high fat-fed conscious mice. Diabetes. 2007;56:1025–1033. doi: 10.2337/db06-0883. [DOI] [PubMed] [Google Scholar]