Summary
Increasing data suggest that meditation impacts stress-related physiological processes relevant to health and disease. For example, our group recently reported that the practice of compassion meditation was associated with reduced innate immune (plasma interleukin [IL]-6) and subjective distress responses to a standardized laboratory psychosocial stressor (Trier Social Stress Test [TSST]). However, because we administered a TSST after, but not prior to, meditation training in our initial study, it remained possible that associations between practice time and TSST outcomes reflected the fact that participants with reduced stress responses prior to training were more able to practice compassion meditation, rather than that meditation practice reduced stress responses. To help resolve this ambiguity, we conducted the current study to evaluate whether innate immune, neuroendocrine and behavioral responses to a TSST conducted prior to compassion meditation training in an independent sample of 32 medically health young adults would predict subsequent amount of meditation practice time during a compassion meditation training protocol identical to the one used in our first study. No associations were found between responses to a TSSTadministered prior to compassion meditation training and subsequent amount of meditation practice, whether practice time was considered as a continuous variable or whether meditators were divided into high and low practice time groups based on a median split of mean number of practice sessions per week. These findings contrast strikingly with our original study, in which high and low practice time meditators demonstrated marked differences in IL-6 and distress responses to a TSST administered after meditation training. In addition to providing the first published data regarding stress responsivity as a potential predictor of subsequent ability/willingness to practice meditation, the current study strengthens findings from our initial work by supporting the conclusion that in individuals who actively engage in practicing the technique, compassion meditation may represent a viable strategy for reducing potentially deleterious physiological and behavioral responses to psychosocial stress.
Keywords: Meditation, Compassion, Mindfulness, Trier Social Stress Test, Cortisol, Interleukin-6
1. Introduction
Increasing evidence suggests that meditation may impact immune processes relevant to emotional and physical health. For example, our group recently reported that the practice of a Tibetan Buddhist-based compassion meditation technique was associated with reduced innate immune responses to a standardized laboratory psychosocial stressor (the Trier Social Stress Test [TSST]) administered after 6 weeks of meditation training (Pace et al., 2009). Specifically, although we found no effect of group assignment (compassion meditation vs. health discussion control group) on innate immune, neuroendocrine (plasma cortisol) or distress responses to the TSST, within the compassion meditation group total amount of practice time during the study was associated with reduced innate immune (plasma interleukin [IL]-6) and distress responses. These associations were apparent whether practice time was considered as a continuous variable or whether meditators were divided into high and low practice time groups by a post hoc median split of mean weekly practice time during the study.
While these results are consistent with the possibility that engagement with compassion meditation reduced inflammatory and distress responses to the TSST, the lack of a main effect of group assignment, combined with the fact that practice time cannot be randomized in advance, raises the specter of reverse causation. Thus, associations between practice time and TSST outcomes may have reflected the fact that participants with reduced stress responses were more able to practice compassion meditation during the study period, rather than that meditation practice reduced stress responses. This question is especially germane because we elected to administer a single TSST following training, rather than conducting pre- and post-training TSSTs, based on multiple studies reporting significant and highly variable rates of attenuation in response to repeated TSSTs (Kirschbaum et al., 1995; Schommer et al., 2003; von Kanel et al., 2006).
To further clarify this important causation issue, in the current study we recruited an independent sample of medically healthy young adults and examined whether innate immune, neuroendocrine and behavioral responses to a TSST conducted prior to compassion meditation training predicted subsequent amount of meditation practice time.
2. Methods
2.1. Participants and study procedures
The current study occurred during spring semester 2008. As in our initial compassion meditation study, all participants were recruited from an introductory health education class at Emory University. Inclusion/exclusion criteria were identical to our initial study and included being medically healthy, with no active psychiatric illness. Participants were also free of psychotropic or other medications that might affect TSST results and were free of acute infection at the time of TSST administration. All participants provided written informed consent, and all study procedures were a priori approved by the Emory University Institutional Review Board.
At the start of the study, demographic and behavioral variables of potential relevance to TSST outcomes were assessed, including age, sex, body mass index (BMI), depressive symptom status and past history of meditation exposure (Pace et al., 2009). All subjects participated in a TSSTwithin 3 weeks of study enrollment. The TSST protocol for the current study was identical to the one employed in our initial study (Pace et al., 2009), except that subjects spent the night preceding the TSST in the Atlanta Clinical and Translational Science Institute (where all TSSTs were performed) to stabilize sleep wake times. Ninety minutes prior to the TSST stressor (public speaking followed by mental arithmetic) an indwelling intravenous catheter was placed in the antecubital vein of the non-dominant arm. As in our initial study, innate immune and neuroendocrine responses to the TSST were assessed by measuring plasma concentrations of IL-6 and cortisol, respectively. Plasma cortisol concentrations were assessed prior to initiation of the public speaking stressor (T0) and 15 min (T1), 30 min (T2), 45 min (T3), 60 min (T4), 75 min (T5) and 90 min (T6) after stressor initiation. Based on findings demonstrating a time-lag in IL-6 responses (Pace et al., 2009), plasma IL-6 concentrations were assessed at T0 and then 30 min (T2), 60 min (T4), 75 min (T5) and 90 min (T6) post-stressor. At each TSST assessment point, blood (7 ml) was collected into chilled EDTA-coated monovettes and centrifuged immediately. Plasma was stored at −80 °C until assay. Plasma IL-6 concentrations were measured by enzyme-linked immunosorbent assay (ELISA) (R&D Systems, Minneapolis, MN). Plasma cortisol concentrations were determined by radioimmunoassay (Diasorin, Stillwater, MN). Indications of assay variability were similar to coefficients of variation in our earlier study (Pace et al., 2009).
As in our initial study, the 30-item Profile of Mood States (POMS) was used to evaluate general distress levels prior to, and immediately following, the TSST. Following standard procedure, general distress was calculated by summing scores on the tension-anxiety, depression-dejection, anger-hostility, fatigue-inertia, and confusion-bewilderment sub-scales and subtracting scores on the vigor-activity subscale (McNair et al., 1992).
When the entire study group had completed the TSST, participants entered a 6-week compassion meditation training protocol identical to the one employed in our initial compassion meditation study, including use of the same teacher (study investigator L.T.N.) and same at-home practice CD. Subjects recorded at-home practice sessions within 48 h of their occurrence via a secure internet site. As in our initial study, meditation practice time was considered as the number of meditation sessions engaged in per week, calculated by adding all at-home sessions that exceeded 10 min in length to the total number of in-class meditation sessions attended and dividing this by the number of study weeks. Potential participants were informed that the purpose of the study was to examine health effects of meditation, but were not told that we would be testing relationships between responses to the TSST and subsequent practice time.
2.2. Statistical analysis
Baseline characteristics of the sample were correlated with amount of meditation practice using Pearson's product-moment coefficients or Spearman's rank coefficients as required. To evaluate the comparability of the present sample with subjects in our initial study, we used independent samples t-tests for continuous variables and Pearson's Chi-Square for categorical variables.
Changes in subjective distress and circulating levels of cortisol and IL-6 as a result of the TSST were examined with a one-way analysis of variance (ANOVA) for dependent measures. To examine whether responses to the TSST predicted subsequent amount of practice time, Pearson partial moment correlations controlling for time of TSST administration were employed. We calculated physiological and behavioral responses to the TSST in a manner identical to our initial study (Pace et al., 2009). Specifically, maximal responses to the TSST were considered to be IL-6 concentrations 90 min and cortisol concentrations 30 min after initiation of the TSST. IL-6 and cortisol responses to the TSSTwere also evaluated according to two area under the curve (AUC) methodologies, one of which calculated AUC from the initial value (AUCi), the other of which calculated AUC from the ground—or zero—value (AUCg) (Pruessner et al., 2003). To maintain consistency with data analytic strategies in our initial study, we also evaluated relationships between TSST responses and later compassion mediation practice by considering practice time as a categorical variable, based on a median split of average practice sessions per week during the study. Differences in the absolute values of each variable across the entire TSST procedure (i.e. from baseline to 90 min post-stressor) between high practice time and low practice time meditation groups were evaluated with a two-way ANOVA for mixed measures, employing Huynh-Feldt adjustments for unequal variance when required. Where indicated, post hoc comparisons of specific means of interest were conducted using the Bonferroni test.
For all analyses except AUCg, IL-6 concentrations were log transformed to improve normality. Tests of significance were two-sided with an alpha level set at p < 0.05. All analyses were performed using SPSS 17 for Macintosh. ANOVAs were run with SPSS GLM Univariate.
3. Results
Thirty-two individuals (14 women/18 men) signed consent and were enrolled in the study, and 30 completed the TSST. Two women were excluded from the TSST because of elevated depressive symptoms. Out of the 30 participants who underwent the TSST, all completed the entire 6-week meditation training program. No differences were found between participants in the current study and subjects randomized to compassion meditation in our initial study in terms of age, sex, BMI, baseline IDS-SR scores or amount of weekly meditation practice during the study. Similarly, no significant correlations were found between sex, BMI or IDS-SR score and meditation practice time in current study participants. A positive correlation was found between age and practice time (rs = 0.46, p = 0.01), but including age as a covariate had no effect on associations between TSST results and subsequent practice time. No one in the current study sample had past meditation experience. This variable was not assessed in our initial study.
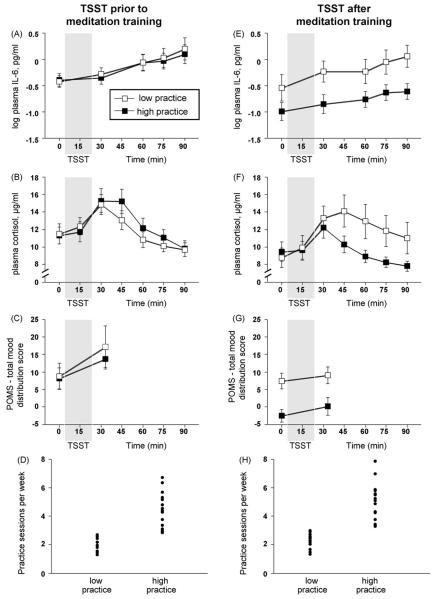
One-way ANOVA of TSST data revealed a significant effect of time for plasma cortisol (F[2.40,69.40] = 16.84, p < 0.001), plasma IL-6 (F[1.59,46.23] = 21.01, p < 0.001) and subjective distress (F[1.0,29.0] = 4.02, p = 0.054) confirming that the TSST successfully induced stress responses. No associations were observed between maximal cortisol, IL-6, or distress responses to the TSST and subsequent average meditation practice sessions per week (p value > 0.05 for all correlations). Similarly, no associations were found between AUCi or AUCg for cortisol or IL-6 and subsequent amount of practice. A similar lack of association was observed when responses to the TSST were compared between participants in high and low practice time groups. Specifically, investigation of IL-6, cortisol, and POMS responses to the TSST with separate two-way ANOVA for mixed measures demonstrated main effects of time (F[1.64,46.01] = 20.47, p < 0.001; F[2.47,69.17] = 16.88, p < 0.001; F[1,28] = 3.90, p = 0.058, respectively), but no main effects of group (F[1,28] = 0.04, p = 0.85; F[1,28] = 0.24, p = 0.63; F[1,28] = 0.22, p = 0.65, respectively) and no group × time interactions (F[1.64,46.01] = 0.26, p = 0.73; F[2.47,69.17] = 1.07, p = 0.36; F[1,28] = 0.15, p = 0.70, respectively) (Fig. 1A–C).
Figure 1.
Trier Social Stress Test (TSST)-induced plasma interleukin (IL)-6, plasma cortisol, and subjective distress responses in high practice and low practice participants challenged with the TSST prior to or after compassion meditation training. High practice and low practice meditation groups in the current study (Panels A–D) and from our earlier investigation (Panels E–H) were formed based on a median split of mean number of practice sessions per week. Regardless of meditation training, challenge with the stressor increased plasma IL-6 (Panels A and E), plasma cortisol (Panels B and F), and distress as measured by the Profile of Mood States (POMS) total score (Panels C and G) in both the current and earlier study. In participants who underwent TSSTchallenge prior to meditation training (current study population), IL-6 (Panel A), cortisol (Panel B), and Profile of Mood States (POMS) total score (Panel C) responses to the TSST did not differ between high and low practice groups. In contrast, in participants who underwent TSST challenge after meditation training (prior study population), IL-6 (Panel E) and POMS total score (Panel G) responses across the TSST procedure were reduced in high practice participants compared to low practice participants. Of note, high and low practice participants in the current study showed comparable amounts of overall practice time compared to high and low practice participants in our earlier study (Panels D and H).
By way of comparison, in our first study cohort (with TSSTs administered after meditation training), an effect of group was observed for IL-6 and POMS scores, with subjects in the high practice group showing lower levels of both variables across the TSST procedure (IL-6: F[1,31] = 4.87, p = 0.035; POMS: F[1,31] = 10.96, p = 0.002) (Fig. 1E and G). As in the current study, no effect of practice time was noted for cortisol responses to the TSST. Finally, high and low practice time groups in the current study did not differ from their equivalent groups in the first study in terms of mean number of weekly meditation sessions during the study (Fig. 1D and H).
4. Discussion
The current study demonstrates that physiological and behavioral responses to a standardized laboratory psychosocial stressor (TSST) did not predict subsequent degree of engagement with a compassion meditation training protocol. In addition to providing the first published data regarding stress responsivity as a potential predictor of subsequent ability/willingness to practice meditation, these results are important because they strengthen the hypothesis that the association observed in our initial study between practice time and TSST responses after meditation training reflects an ability of compassion meditation to downregulate innate immune and distress responses to psychosocial stress. These findings may thus point to important potential health applications for compassion meditation, given the well established role of physiological stress responses in the development of many modern medical and psychiatric diseases (Cohen et al., 2007).
Current findings are especially relevant given that our first study did not find an overall effect of group assignment (compassion meditation vs. health discussion group control) on either IL-6 or distress responses to a TSST conducted after completion of these interventions. This absence of a group effect made observed correlations between practice time and TSST responses especially difficult to interpret, because practice time per se is not a variable upon which individuals can be randomized a priori. Thus while it was certainly possible that the practice of compassion meditation reduced IL-6 and distress responses, it was also not unreasonable to speculate that individuals with reduced inflammatory and emotional stress responsivity prior to training might have been more inclined/able to practice meditation. By disproving this possibility, the current study also increases the likelihood that the lack of a main effect of group assignment in our first study resulted from the fact that many participants randomized to compassion meditation did not practice a sufficient amount to benefit from the training.
Taken together, findings from our two study cohorts may also suggest that the health relevant effects of compassion meditation derive specifically from the practice itself, rather than from potentially therapeutic ancillary factors common to most forms of meditation training, including expectancy bias, group support and psychoeducation. Moreover, unlike many recent meditative interventions that deliberately incorporate other therapeutic modalities such as psychotherapy, yoga and journaling (Kabat-Zinn, 1982), the protocol used in both the current study and our initial investigation focused exclusively on techniques related to compassion meditation. This exclusive focus on meditative techniques further strengthens the argument that these techniques themselves, rather than other non-specific factors, may have affected mental functioning in ways that led to diminished innate immune and behavioral responses to psychosocial stress.
Strengths of the current study include use of the same recruiting environment, which enabled us to enroll a study population that closely matched our original study sample in terms of factors known to contribute to TSST outcomes such as sex and BMI and depressive symptom status (Pace et al., 2009). Although ages differed between our first and second sample, the numeric difference was slight (18.5 vs. 18.2) and unlikely to be of physiological relevance. The compassion meditation program in the current study was taught by the same teacher who taught all meditation classes in our initial study, utilizing a training protocol identical in content and delivery schedule, which likely contributed to the fact that overall practice times did not differ between our first and second study. Moreover, we conducted TSSTs in the same research unit, using the same protocol, including the same “committee chairmen” (the only TSST panel member who interacts with participants during the stressor) as in our original study.
Nonetheless, although we have shown in separate populations that compassion meditation practice is associated with innate immune and behavioral responses to a TSST administered after, but not prior to, meditation training we have not conclusively demonstrated that meditation practice caused a reduction in physiological and behavioral responses to a stressor. To more firmly establish causal efficacy for compassion meditation training a longitudinal design in which the TSSTwas administered both prior to, and upon completion of, meditation training in the same individuals would be required.
Acknowledgements
For their indispensable help, the authors would like to thank Andrew H. Miller, Robert Paul, Laurie Patton, Bobbi Patterson, Carol Newsome, Thomas R. Ziegler, Joyce M. Oglesby, the nursing staff of the Emory GCRC and the many members of Drepung Loseling Institute who gave so freely of their time.
Role of funding source
This study was supported by the Emory College Seed Fund and Emory Strategic Initiative funding to the Emory Collaborative for Contemplative Studies. The study was also supported in part by PHS Grant UL1 RR025008 from the Clinical and Translational Science Award program and PHS Grant M01 RR0039 from the General Clinical Research Center program, National Institutes of Health, National Center for Research Resources. These funding sources had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Conflicts of interest
Dr. Raison has been on speaker's bureaus for Wyeth and Lilly in the previous 12 months. He has served on advisory boards for Wyeth, Lilly, Schering Plough and Centocor, and is Chief Scientific Advisor and owns equity in Contemplativehealth.com.
References
- Cohen S, Janicki-Deverts D, Miller GE. Psychological stress and disease. JAMA. 2007;298:1685–1687. doi: 10.1001/jama.298.14.1685. [DOI] [PubMed] [Google Scholar]
- Kabat-Zinn J. An outpatient program in behavioral medicine for chronic pain patients based on the practice of mindfulness meditation: theoretical considerations and preliminary results. Gen. Hosp. Psychiatry. 1982;4:33–47. doi: 10.1016/0163-8343(82)90026-3. [DOI] [PubMed] [Google Scholar]
- Kirschbaum C, Prussner JC, Stone AA, Federenko I, Gaab J, Lintz D, Schommer N, Hellhammer DH. Persistent high cortisol responses to repeated psychological stress in a subpopulation of healthy men. Psychosom. Med. 1995;57:468–474. doi: 10.1097/00006842-199509000-00009. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of Mood States, Revised Edition. Educational and Industrial Testing Service; San Diego, CA: 1992. [Google Scholar]
- Pace TW, Negi LT, Adame DD, Cole SP, Sivilli TI, Brown TD, Issa MJ, Raison CL. Effect of compassion meditation on neuroendocrine, innate immune and behavioral responses to psychosocial stress. Psychoneuroendocrinology. 2009;34:87–98. doi: 10.1016/j.psyneuen.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pruessner JC, Kirschbaum C, Meinlschmid G, Hellhammer DH. Two formulas for computation of the area under the curve represent measures of total hormone concentration versus time-dependent change. Psychoneuroendocrinology. 2003;28:916–931. doi: 10.1016/s0306-4530(02)00108-7. [DOI] [PubMed] [Google Scholar]
- Schommer NC, Hellhammer DH, Kirschbaum C. Dissociation between reactivity of the hypothalamus–pituitary–adrenal axis and the sympathetic–adrenal–medullary system to repeated psychosocial stress. Psychosom. Med. 2003;65:450–460. doi: 10.1097/01.psy.0000035721.12441.17. [DOI] [PubMed] [Google Scholar]
- von Kanel R, Kudielka BM, Preckel D, Hanebuth D, Fischer JE. Delayed response and lack of habituation in plasma interleukin-6 to acute mental stress in men [see comment] Brain Behav. Immun. 2006;20:40–48. doi: 10.1016/j.bbi.2005.03.013. [DOI] [PubMed] [Google Scholar]