Abstract
The treatment of infections caused by fungi and trypanosomatids is difficult due to the eukaryotic nature of these microbial cells, which are similar in several biochemical and genetic aspects to host cells. Aggravating this scenario, very few antifungal and anti-trypanosomatidal agents are in clinical use and, therefore, therapy is limited by drug safety considerations and their narrow spectrum of activity, efficacy and resistance. The search for new bioactive agents against fungi and trypanosomatids has been expanded because progress in biochemistry and molecular biology has led to a better understanding of important and essential pathways in these microorganisms including nutrition, growth, proliferation, signaling, differentiation and death. In this context, proteolytic enzymes produced by these eukaryotic microorganisms are appointed and, in some cases, proven to be excellent targets for searching novel natural and/or synthetic pharmacological compounds, in order to cure or prevent invasive fungal/trypanosomatid diseases. With this task in mind, our research group and others have focused on aspartic-type proteases, since the activity of this class of hydrolytic enzymes is directly implicated in several facets of basic biological processes of both fungal and trypanosomatid cells as well as due to the participation in numerous events of interaction between these microorganisms and host structures. In the present paper, a concise revision of the beneficial effects of aspartic protease inhibitors, with emphasis on the aspartic protease inhibitors used in the anti-human immunodeficiency virus therapy, will be presented and discussed using our experience with the following microbial models: the yeast Candida albicans, the filamentous fungus Fonsecaea pedrosoi and the protozoan trypanosomatid Leishmania amazonensis.
Keywords: Protease, Aspartic protease inhibitors, Trypanosomatids, Fungi, Cell biology, Virulence, Chemotherapy
INTRODUCTION AND EDUCATIONAL EXPERIENCE
Since I was young, I (Figure 1) have been interested in being a teacher, and that feeling grew and consolidated along with my professional journey. The scientific world was introduced to me during high school. From 1990 to 1994, I studied the Biotechnology course in a reputable Federal Institution from Rio de Janeiro State, Brazil, called Escola Técnica Federal de Química - ETFQ (currently CEFETEQ), an excellent technical school. Over those years, the disciplines related to the Microbiology area (Bacteriology, Mycology, Virology, Protozoology and Immunology) and the laboratory classes produced a great curiosity, motivation and stimulation of scientific thought, which ignited my desire to be a scientist. With this proposal in mind, in 1994, I started my bachelor degree in the Microbiology and Immunology course at the Federal University of Rio de Janeiro (UFRJ), being one of the 35 students approved to constitute the first class of that novel graduation course. In parallel, I worked as a Biotechnology technician at the Biochemistry Department of the State University of Rio de Janeiro (UERJ) under the supervision of Dr. Claudia Vitória de Moura Gallo, an exemplar professional and an excellent person, who contributed notably to turn my dream into reality. In early 1999, I finished the undergraduate program and started a Master’s degree at the Institute of Microbiology Prof. Paulo de Góes (IMPPG)-UFRJ. During the period from mid 2000 until early 2002, I developed my doctoral thesis at the IMPPG-UFRJ under the supervision of Dr. Rosangela Maria de Araújo Soares. Since August 2002, I have been Professor at the Department of General Microbiology of the IMPPG-UFRJ and, since then, I have been teaching lessons to several undergraduate courses including Microbiology and Immunology, Nursing, Biology and Pharmacy. Still, I effectively participate in two postgraduate courses at UFRJ: Microbiology from IMPPG and Biochemistry from Chemistry Institute.
Figure 1.
André Luis Souza dos Santos, Associate Professor, Laboratory of Multidisciplinary Studies on Microbial Biochemistry, Department of General Microbiology, Institute of Microbiology Prof. Paulo de Góes, Federal University of Rio de Janeiro, Rio de Janeiro, RJ 21941-902, Brazil.
Indubitably, my professional work has only been fully developed because I have a research group consisting of competent professionals, including technicians and undergraduate, masters, doctoral and postdoctoral students, who are extremely dedicated and committed to scientific thinking. I would like take this opportunity to express and reiterate my full admiration and gratitude to all my students. I would also like to thank to the several Brazilian researchers who have contributed immensely to my work, in particular Dr. Marta Helena Branquinha (IMPPG-UFRJ), Dr. Eliana Barreto-Bergter (IMPPG-UFRJ), Dr. Lucy Seldin (IMPPG-UFRJ), Dr. Celuta Sales Alviano (IMPPG-UFRJ), Dr. Claudia Masini d’Avila-Levy (Fundação Oswaldo Cruz-FIOCRUZ) and Dr. Lucimar Ferreira Kneipp (FIOCRUZ). My research has been supported by the Brazilian agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Conselho de Ensino para Graduados e Pesquisas (CEPG/UFRJ), Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ), Fundação Universitária José Bonifácio (FUJB) and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (CAPES). I have also been supported by a CNPq fellowship since 2005 and by a FAPERJ fellowship since 2007.
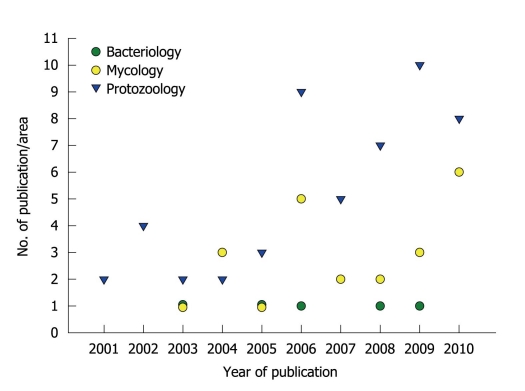
Over the past 10 years: (1) I supervised 16 monographs of graduate students, 10 master theses and 4 doctoral theses; (2) I published 79 papers in the field of Bacteriology (n = 5), Mycology (n = 22) and Protozoology (n = 52) (Figure 2); and (3) I was invited to participate as a speaker at national and international meetings. I am a peer reviewer for international scientific journals, as well as career and research grant committees. In addition, I have accepted invitations to write reviews and book chapters on the themes: (1) relevance of proteolytic enzymes produced by microorganisms; and (2) antimicrobial properties of protease inhibitors[1-11].
Figure 2.
Publication of scientific papers by the research group led by André Santos. The graphic summarizes the numbers and specific areas of Microbiology in relation to papers published during the past ten years.
ACADEMIC STRATEGIES AND GOALS
Our work group is distinguished by its multidisciplinary nature, with direct involvement of different research institutions from Brazil (other Departments and Institutes from UFRJ, UERJ, FIOCRUZ, Universidade Federal Fluminense (UFF), Universidade Federal do Estado do Rio de Janeiro (UNIRIO), Universidade do Estado de São Paulo (USP), Universidade Federal de São Paulo (UNIFESP), Universidade Federal do Espírito Santo (UFES)) and from other countries, generating productive and effective collaborations. Several publications in high-ranked journals, e.g. FEMS Microbiology Reviews, PLoS One, Archives of Biochemistry and Biophysics, Journal of Antimicrobial Chemotherapy, Journal of Clinical Microbiology, International Journal of Antimicrobial Agents, Microbes and Infection, International Journal for Parasitology, Protist, Parasitology and Medical Mycology, were produced in collaboration with these partners.
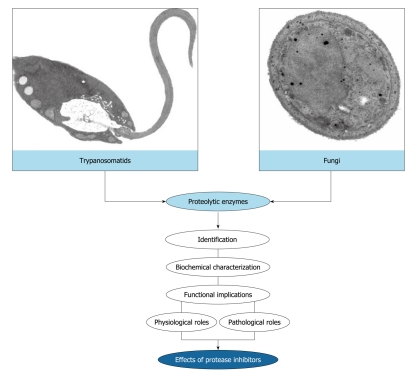
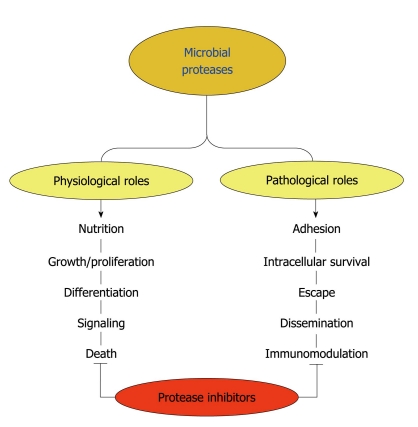
Over the last years, my group has focused on the identification, biochemical characterization and discovery of biological functions of proteases produced by microorganisms, with emphasis in trypanosomatids and fungi (Figure 3). More recently, we have started to study protease inhibitors in an attempt to use these bioactive compounds as a new therapeutic proposal against eukaryotic pathogenic microorganisms (Figure 3).
Figure 3.
Rationale of the research works developed in the André Santos’ laboratory. The main purpose of our study focuses on the identification and biochemical characterization of cellular and/or extracellular proteases produced by eukaryotic microorganisms, especially trypanosomatids and fungi. Subsequently, we have focused on the discovery of possible biological functions for these hydrolytic enzymes in both the social context of the microbial cell and the participation in interaction events with biotic and abiotic substrates. Finally, we have used the protease inhibitors in an attempt to block vital processes in microbial cells, thus preventing a successful infection.
RESEARCH ACHIEVEMENTS
Proteolytic enzymes and their inhibitors: an overview
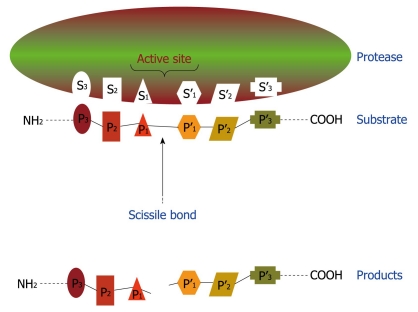
Proteolytic enzymes catalyze the cleavage of peptide bonds, which link amino acid residues in proteins and peptides. A redundant set of terms is used by the scientific community to refer to proteolytic enzymes, including: peptide hydrolase, peptidase and protease. All proteases bind their substrates in a groove or cleft, where peptide bond hydrolysis occurs (Figure 4). Amino acid side chains of substrates occupy proteolytic enzyme sub-sites in the groove, designated as S3, S2, S1, S1’, S2’, S3’, that bind to corresponding substrate/inhibitor residues P3, P2, P1, P1’, P2’, P3’ with respect to the cleavable peptide bond (Figure 4). After the proteinaceous substrate cleavage, at least two smaller peptides can be generated (Figure 4)[12-15].
Figure 4.
Schematic representation of binding region and catalytic site of a protease. This hypothetical protease possesses six subsites (S1-S3 and S1’-S3’) in its catalytic site and, consequently, is able to recognize and bind to a sequence of six amino acids (P1-P3 and P1’-P3’) in the proteinaceous substrate. After proteolysis, at least two smaller peptides are generated as the reaction products.
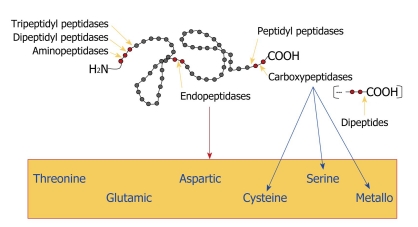
Proteases are subdivided into two major groups depending on their site of action: exopeptidases and endopeptidases. Exopeptidases cleave the peptide bond proximal to the amino (NH2) or carboxy (COOH) termini of the proteinaceous substrate, whereas endopeptidases cleave peptide bonds within a polypeptide chain. Based on their site of action at the NH2 terminal, the exopeptidases are classified as aminopeptidases, dipeptidyl peptidases or tripeptidyl peptidases that act at a free NH2 terminus of the polypeptide chain and liberate a single amino acid residue, a dipeptide or a tripeptide, respectively. Carboxypeptidases or peptidyl peptidases act at the COOH terminal of the polypeptide chain and liberate a single amino acid or a dipeptide (which can be hydrolyzed by the action of a dipeptidase). Carboxypeptidases can be further divided into three major groups: serine, metallo and cysteine carboxypeptidases, based on the functional group present at the active site of the enzymes. Similarly, endopeptidases are classified according to essential catalytic residues at their active sites in: serine, metallo, glutamic, threonine, cysteine and aspartic endopeptidases (Figure 5). Conversely, there are a few miscellaneous proteases that do not precisely fit into the standard classification[12-15].
Figure 5.
Classification of proteases. Gray circles represent amino acids and red circles indicate the amino acid sequence that is bound to the proteolytic enzyme. Yellow arrows point to the site of cleavage. The blue arrows indicate the classification of carboxypeptidases and the red arrow shows the box containing all the classes of endopeptidases, according to the chemical group present in their catalytic sites.
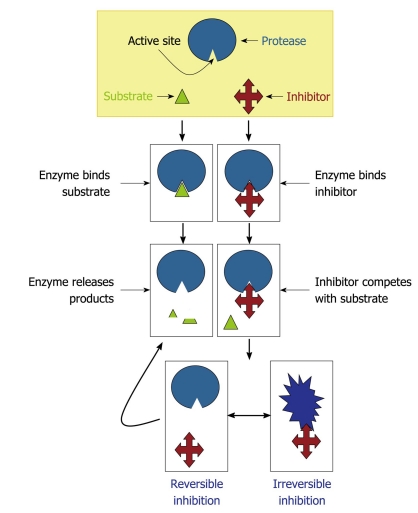
The class of a protease is characteristically determined according to the effects of proteolytic inhibitors on the enzymatic activity[16,17]. Protease inhibitors enter or block a protease active site to prevent substrate access. In competitive inhibition, the inhibitor binds to the active site, thus preventing enzyme-substrate interaction. In non-competitive inhibition, the inhibitor binds to an allosteric site, which alters the active site and makes it inaccessible to the substrate[16,17]. The proteolytic inhibitors can be divided into two functional classes on the basis of their interaction with the target protease: (1) irreversible trapping reactions and (2) reversible tight-binding reactions (Figure 6). Inhibitors which bind through a trapping mechanism change conformation after cleaving an internal peptide bond and “trap” the enzyme molecule covalently; neither the inhibitor nor protease can participate in further reactions. In tight-binding reactions, the inhibitor binds directly to the active site of the protease; these reactions are reversible and the inhibitor can dissociate from the proteolytic enzyme in either the virgin state, or after modification by the protease. Based on their structural dichotomy, proteolytic inhibitors can be generally classified into two large groups: low molecular mass peptidomimetic inhibitors and protein protease inhibitors composed of one or more peptide chains. Proteolytic inhibitors can be further classified into five groups (metallo, serine, threonine, cysteine and aspartic protease inhibitors) according to the mechanism employed at the active site of proteolytic enzymes they inhibit. Some proteolytic inhibitors interfere with more than one type of protease[16,17].
Figure 6.
Mechanisms of protease inhibition. The protease inhibitor competes with the substrate to bind to the active site of a protease and two distinct possibilities arise: (1) substrate binds to the catalytic site and then is cleaved by the protease, which releases the products or (2) inhibitor binds to the active site and by steric hindrance blocks the substrate attachment. In this last case, the inhibitor can promote an irreversible (the conformational structure of the protease is completely lost) or reversible inhibition (when the inhibitor disconnects from the enzyme, the substrate can bind to it).
Proteases produced by microorganisms: global functions
Proteases are essential for all life forms. They are involved in a multitude of physiological reactions from simple digestion of proteins for nutrition purposes to highly-regulated metabolic cascades (e.g. proliferation and growth, differentiation, signaling and death pathways), being essential factors for homeostatic control in both prokaryote and eukaryote cells (Figure 7)[12]. Proteases are also essential molecules in viruses, bacteria, fungi and protozoa for their colonization, invasion, dissemination and evasion of host immune responses, mediating and sustaining the infectious disease process (Figure 7). Collectively, proteases participate in different steps of the multifaceted interaction events between microorganism and host structures, being considered as virulent attributes. Consequently, the biochemical characterization of these proteolytic enzymes is of interest not only for understanding proteases in general but also for understanding their roles in microbial infections and thus their exploitation as targets for rational chemotherapy of microbial diseases[3,6,10,18-24].
Figure 7.
Possible functions played by microbial proteases. Surface and/or secreted proteases are able to cleave different host components such as serum proteins, antimicrobial peptides, surface molecules and structural proteinaceous compounds. The degradation of host proteins can help the microorganisms in several steps of their life cycle and pathogenesis including dissemination, adhesion, escape, nutrition and immunomodulation of the host immune response. These proteases can also contribute to maintaining basic metabolic processes in a microbial cell, which govern crucial events like proliferation, differentiation, signaling and death pathways. Proteolytic inhibitors are able to block one or several of these fundamental events.
Antimicrobial properties of proteolytic inhibitors
Current therapy for both fungal and trypanosomatid infections is suboptimal due to toxicity of the available therapeutic agents and the emergence of drug resistance[25-28]. Compounding these problems is the fact that many endemic countries and regions are economically poor. For that reason, the development of novel antifungal and/or anti-trypanosomatidal drugs is an imperative requirement. A number of new strategies to obstruct fungal/trypanosomatid biological processes have emerged; one of them is focused on protease inhibition. Currently, the main approach has been to obtain good inhibitors of the target protease, in the belief that inhibition of the activity will be therapeutic. In this context, our research group has published some works that corroborate this premise[1-6,10,29-39].
Aspartic protease inhibitors used in anti-human immunodeficiency virus therapy present anti-microbial properties
Lessons from the yeast Candida albicans (C. albicans), the filamentous fungus Fonsecaea pedrosoi (F. pedrosoi) and the protozoan Leishmania amazonensis (L. amazonensis) are illustrated as follows.
C. albicans: C. albicans is both a successful commensal and pathogen of humans that can infect a broad range of body sites[40]. The transition from commensalism to parasitism requires a susceptible host, which includes individuals with humoral and/or cellular deficiencies as well as persons submitted to different immunosuppressive procedures. Candidiasis is the most common fungal infection diagnosed in humans[41-43]. Due to the emergence of pathogens resistant to conventional antifungals and the toxicity of some antimycotics, intense efforts have been made to develop more effective antifungal agents for clinical use[44-48]. The pathogenesis of C. albicans is multifactorial and different virulence attributes are important during the various stages of infection[20,21,49-55]. Secreted aspartic proteases (Saps) play a role in several infection stages of C. albicans, being the most important virulence factors expressed by this opportunistic fungus. Actually, C. albicans possesses ten different SAP genes (SAP1 to SAP10), which are expressed according to distinct environments and host conditions[56-60]. Therefore, Saps are potential targets for the development of novel anti-C. albicans drugs[1,2,34,35]. In this context, several groups have demonstrated that aspartic protease inhibitors, including pepstatin A and the first generation of protease inhibitors used in anti-human immunodeficiency virus (HIV) therapy (nelfinavir, saquinavir, ritonavir and indinavir), are able to restrain Sap activity (especially Sap1, Sap2 and Sap3) as well as arrest crucial events of C. albicans yeast cells such as proliferation and adhesion to both abiotic (e.g. plastic and acrylic substrates) and biotic structures (e.g. surface of different epithelial cell lineages)[61-72]. Our results showed that amprenavir[72] (unpublished data) and lopinavir (unpublished data), two HIV aspartic protease inhibitors of the second generation, significantly inhibited the hydrolytic activity of Sap2 and also blocked the yeasts into mycelia transformation, an essential step during the candidiasis pathogenesis. In addition, scanning electron microscopy revealed prominent ultrastructural alterations of yeast cells, which corroborated the inhibition of cellular division by these protease inhibitors. Several surface and/or secreted molecules have had their expression/production significantly diminished including (1) mannose- and sialic acid-rich surface glycoconjugates, which are directly involved in adhesive properties and biofilm formation; (2) sterol content, which controls the membrane fluidity; (3) secretion of lipases (e.g. esterases and phospholipases), which are related to the host membrane disruption; and (4) catalase activity, which reduces the ability of yeasts to escape from oxidative stress generated by hydrogen peroxide, for example, released by host phagocytes[72] (unpublished data). However, it is also important to note that the inhibitory effects of HIV protease inhibitors both in in vitro and in vivo experimental models were observed at concentrations (μmol/L range) much higher than those needed for HIV protease inhibition (nmol/L range). This probably reflects a much lower affinity of these drugs for Sap than that for HIV protease[31,34]. Another explanation is that, in contrast to the very small and structurally simplified HIV protease, Saps are larger and more complex[60,73]. They possess a relatively large active site which might be responsible for the broader substrate specificity and also their susceptibilities to distinct aspartic protease inhibitors[60]. Nevertheless, the above concentrations may be achieved under current highly active antiretroviral therapy (HAART) regimens both in the blood[31], in human saliva (at least for indinavir)[74] and in lungs (at least for lopinavir)[75]. In this sense, our group has showed that lopinavir at 10 mg/kg promoted a therapeutic effect in an experimental murine model of disseminated candidiasis, with an efficacy comparable to that of fluconazole, a recognized anti-candidal drug (unpublished results).
F. pedrosoi: Fonsecaea is a genus containing pigmented filamentous fungus isolated from soil, rotten wood and decomposing plant material. F. pedrosoi is one of the major causative agents of chromoblastomycosis, a post-traumatic and chronic infection of subcutaneous tissues in humid tropical areas specially South America and Japan[8,76-79]. F. pedrosoi is a valuable model in cell biology, since its life cycle comprises different morphological states that include reproduction structures (conidia) and fungal forms usually found in the saprophytic (mycelia) and parasitic stage (sclerotic bodies)[8]. The first report on protease production by F. pedrosoi was described by our group[80], which demonstrated that the pattern of protease production and secretion by F. pedrosoi conidial cells was closely dependent on the culture medium composition: metalloproteases were induced after cultivation in complex culture medium, while aspartic proteases were detected under chemically defined growth conditions. Mycelia[81] and sclerotic cells (unpublished results) of F. pedrosoi were also able to secrete aspartic-type proteases. The aspartic proteases produced by conidia and mycelia were capable of degrading relevant host serum proteins (e.g. IgG and albumin) as well as extracellular matrix components (e.g. laminin, fibronectin and collagen)[80,81]. For that reason, the extracellular hydrolytic enzymes produced by F. pedrosoi cells, such as proteases and lipases[82], could support the initial development of this fungus inside the host, and the existence of two biochemically distinct secreted proteases makes it possible to cover a wide range of host conditions. The effect of saquinavir, ritonavir, indinavir and nelfinavir on the secreted proteases of F. pedrosoi was evaluated[81,83]. These compounds inhibited the extracellular aspartic proteolytic activity produced by both conidial and mycelial forms in a dose-dependent manner. Nelfinavir was the best inhibitor of the aspartic protease activity secreted by conidia and mycelia, restraining the hydrolytic activities around 80% at 50 μmol/L. Interestingly, recent isolated strains of F. pedrosoi produced higher levels of extracellular protease activity when compared with a laboratory-adapted strain[81,83], suggesting that the production of secreted aspartic-type proteases may be stimulated by interaction with the host. HIV aspartic protease inhibitors and pepstatin A also arrested the growth of conidial forms as well as transformation into mycelia[83], an essential step during the F. pedrosoi life cycle and virulence[8]. Pepstatin A showed a significant inhibition of conidial viability even at low concentration (0.1 μmol/L); however, the HIV protease inhibitors were toxic only at high concentrations (ranging from 50 to 200 μmol/L). The synergistic action on proliferation behavior between nelfinavir (25 μmol/L) and amphotericin B (3 μg/mL), when both were used at sub-inhibitory concentrations, was also observed[83]. Interestingly, HIV protease inhibitors-treated conidial cells presented irreversible ultrastructural alterations, as shown by transmission electron microscopy images such as invaginations in the cytoplasmic membrane and withdrawal of the cytoplasmic membrane from within the cell wall, disorder and detachment of the cell wall, rupture of internal organelles, detection of large and irregular cytoplasmic vacuoles, some of them containing small vesicles, abnormal cellular division and breakage of cell wall. Furthermore, the aspartic protease inhibitors drastically reduced the adhesion and endocytic indexes during the interaction between F. pedrosoi conidia and epithelial cells of the Chinese hamster ovary lineage, fibroblasts or macrophages. Aspartic protease inhibitors also promoted a significant increase in the susceptibility killing by macrophage cells, promoting a significant reduction in the number of viable intracellular conidia after the treatment of infected macrophage monolayers with indinavir, nelfinavir and ritonavir at 6.25 μmol/L for 24 h[83].
L. amazonensis: Leishmania are digenetic protozoan parasites that live as promastigotes in the digestive tract of sand flies and as amastigotes in the phagolysosomes of mammalian macrophages. They cause a wide spectrum of clinical manifestations (generically known as leishmaniasis), and its clinical manifestations are dependent on both parasite species and immune response of the host[84-89]. The increase in the incidence of the disease, associated with higher morbidity rates, the spread of some forms of leishmaniasis to new geographical areas and Leishmania-HIV co-infection, has become an important public health problem in the world[90-93]. However, the incidence of HIV-Leishmania co-infections has been decreasing since the introduction of HAART, in which aspartic-type protease inhibitors were included[94,95]. These findings instigated the research to confirm the possible connection between aspartic protease expression and basic molecular processes in Leishmania[96-103]. Our group showed that HIV protease inhibitors were able to impair in vitro proliferation of L. amazonensis promastigotes in a dose-dependent manner and in different extensions, in which nelfinavir (IC50 = 15.1 ± 1.1 μmol/L), lopinavir (IC50 = 16.5 ± 0.8 μmol/L) and amprenavir (IC50 = 62.0 ± 2.1 μmol/L) were the most potent compounds[103]. These three protease inhibitors (at the IC50 value) caused profound changes in the leishmania ultrastructure, including cytoplasm shrinking, increase in the number of lipid inclusions and some cells with the nucleus closely wrapped by endoplasmic reticulum, resembling an autophagic process, as well as chromatin condensation that is suggestive of apoptotic death. The treatment with HIV protease inhibitors of either the promastigote forms preceding the interaction with macrophage cells or the amastigote forms inside macrophages drastically reduced the association indexes (when inhibitors were used at 50 μmol/L) and the number of intracellular amastigotes (when inhibitors were used at 3.12 μmol/L)[103]. The hydrolysis of HIV protease substrate by L. amazonensis extract was fully inhibited by pepstatin A and HIV protease inhibitors at 10 μmol/L, suggesting that an aspartic protease may be the parasite target of the inhibitors. Despite all these beneficial effects, the HIV protease inhibitors induced an increase in the expression of cysteine protease b (cpb)[19] and the metalloprotease gp63[24], two well-known virulence factors expressed by Leishmania spp., probably in an attempt to compensate the parasite aspartic protease inhibition[103].
Proposals of the molecular mechanisms of the aspartic protease inhibitors on the aspartic protease produced by microorganisms
Direct actions - inhibition of aspartic proteases: The binding of the aspartic protease inhibitor to the active site of an aspartic protease blocks the binding of substrate to the enzyme. Therefore, the substrate remains intact and no peptides and/or amino acids are generated. Obviously aspartic protease inhibition will be more or less drastic depending on several parameters like the inhibitor affinity constant for the active site, its ability to reversibly or irreversibly bind to the enzyme, and the ratio of inhibitor in relation to the available substrate and enzyme. (1) The inhibition of secreted and/or surface aspartic proteases can result in an inability of the microorganism to obtain peptides and amino acids to its nutrition, leading to a reduction or a complete interruption in the proliferation rate. This phenomenon is clearly observed in C. albicans yeast cells when cultured under chemically defined medium containing large proteins (e.g. albumin and hemoglobin) as a unique nitrogenous source, but not when Candida cells are cultured in a medium containing an unlimited nitrogenous source[104-108]; (2) Some intracellular aspartic proteases produced by microorganisms also control the cleavage of important own proteins in order to promote protein activation and/or perfect functioning of a biosynthetic route; their inhibition can arrest signaling events and/or metabolic pathways, as a result inhibiting some crucial biological processes for microbial cells such as morphogenesis or expression of surface molecules responsible for adhesion or fungal protection. For example, some of these aspartic protease inhibitors alter the lipid biosynthesis, including ergosterol, resulting in altered membrane permeability[68,72,83]. These inhibitory actions will depend on the ability of the aspartic protease inhibitors to (a) enter in the microbial cells and (b) accumulate inside them; and (3) Some surface aspartic proteases participate in the assembly and organization of the microbial surface. For instance, in contrast to all other members of the Sap family, the proteases Sap9 and Sap10 are bound to the C. albicans cell surface by a glycosylphosphatidylinositol anchor motif. Sap9 seems to be predominantly located in the cell membrane, and Sap10 is located in the cell wall and membrane[109]. Recently, Schild et al[110] demonstrated that Sap9 and Sap10 cleave covalently linked cell wall proteins, including chitinase Cht2 and the glucan-cross-linking protein Pir1. Deletion of the SAP9 and SAP10 genes resulted in a reduction of cell-associated chitinase activity similar to that upon deletion of CHT2, suggesting a direct influence of Sap9 and Sap10 on Cht2 function. The treatment with amprenavir[72] and lopinavir (data not shown) promoted the removal of the amorphous layer that covers the entire surface of C. albicans, turning the rough surface into a smooth one. Moreover, surface aspartic proteases can promote microorganism adhesion (by functioning as an adhesive molecule or by destroying some receptors at the host surface, exposing and/or facilitating the adhesion event); therefore, their inhibition can diminish the ability of a microorganism to interact with host structures.
Indirect actions - binding to unrelated molecules: The possibility of aspartic protease inhibitors binding to or interfere with other molecules than aspartic proteases can not be excluded[35]. In this context, these compounds can generate irreversible toxic effects by perturbing the homeostasis of the microbial cells, culminating in death of microorganisms.
CONCLUSION
Microbial pathogenesis is a multifactorial process and different virulence factors are important during the various phases of infection. Some virulence attributes, such as the aspartic proteases, play a role in several infection stages and the inhibition of one of the many stages probably will contribute to the containment of the pathogen and thus should help in the treatment of disease. Therefore, aspartic proteases synthesized by pathogenic fungi and trypanosomatids are prospective targets for the development of new chemotherapeutic compounds. Both in vitro and in vivo studies demonstrated that the use of HIV protease inhibitors promoted a drastic reduction in the presence of both fungal and trypanosomatid opportunistic diseases as well as clearly revealing that these inhibitors are able to arrest vital events in microbial cells presenting eukaryotic architecture, including proliferation, differentiation and nutrition. These inhibitors also impair the development of infection in culture or animal models due to their capability of blocking adhesion, internalization, evasion and escape of host responses. Together, all these beneficial effects culminate in death of the microorganism and/or its inadequate ability to develop an efficient and successful infection. Future studies must investigate combination drug therapy, which may reduce the incidence of toxicity due to individual drugs and may also delay the emergence of drug resistance. In addition, the purification of aspartic proteases produced by fungi and trypanosomatids, the knowledge of its biochemical properties and the crystallization of the tertiary structure will contribute to better understanding of the functioning of these proteolytic enzymes as well as allowing the design of more specific inhibitors. At least for C. albicans, the crystal structure of Sap2 complexed with pepstatin A has been known since 1993[111], whereas the crystal structure of Sap3 and its complex with pepstatin A was first presented in 2007[112]. The secondary structures of Sap2 and Sap3 as well as Sap1 and Sap5 were recently described[113]. These data could help in the development of novel and more effective anti-C. albicans compounds.
I really hope that all these findings together arouse the curiosity and the enthusiasm of other researchers in order to look for novel compounds with the ability to inhibit aspartic proteases produced by fungi and trypanosomatids. These novel compounds must be more specific, powerful and with reduced side effects, in an attempt to increase our armamentarium to treat fungal and trypanosomatid diseases.
Acknowledgments
It is so difficult to put in words my scientific trajectory; firstly, because it is difficult to write about myself and, secondly, because some of the professional moments that I came through were intimately associated with my personal life, which has been difficult. But all of these difficult times were compensated by satisfactory and unforgettable moments. In this sense, I am grateful to the past and present members of my laboratory for their contributions to our studies. I also wish to express my gratitude to several colleagues and investigators for their collaborations, in especial Marta Helena Branquinha and Claudia Masini d’Avila-Levy, with whom I share all my scientific achievements and victories and to whom I dedicate this publication.
Footnotes
Supported by Grants from the Brazilian Agencies: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq), Coordenação de Aperfeiçoamento Pessoal de Nível Superior and Fundação Carlos Chagas Filho de Amparo à Pesquisa do Estado do Rio de Janeiro (FAPERJ); the author was supported by CNPq and FAPERJ fellowships
Peer reviewers: Chen-Yong Lin, PhD, Associate Professor, Biochemistry and Molecular Biology, University of MarylandSchool of Medicine, 655 w Baltimore Street, 10-027 BRB, Baltimore, MD 21201, United States; Michiaki Yamashita, PhD, Chief, Food Biotechnology Section, National Research Institute of Fisheries Science, 2-12-4 Fukuura, Yokohama 236-8648, Japan
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Santos ALS. Aspartic proteases of human pathogenic fungi are prospective targets for the generation of novel and effective antifungal inhibitors. Curr Enz Inhib. 2011:In press. [Google Scholar]
- 2.dos Santos ALS. HIV aspartyl protease inhibitors as promising compounds against Candida albicans. World J Biol Chem. 2010;1:21–30. doi: 10.4331/wjbc.v1.i2.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Vermelho AB, Branquinha MH, D’Ávila-Levy CM, dos Santos ALS, Paraguai de Souza Dias E, Nogueira de Melo AC. Biological roles of peptidases in trypanosomatids. Open Parasitol J. 2010;4:5–23. [Google Scholar]
- 4.Santos ALS, d’Avila-Levy CM, Branquinha MH. Calpain-like proteins in trypanosomatids: effects of calpain inhibitors on the parasites’ physiology and motivations for their possible application as chemotherapeutic agents. In: Cohen JB, Ryseck LP, editors. Cystatins: protease inhibitors, biomarkers and immunomodulators. New York: Nova Science Publishers; 2011: In press. [Google Scholar]
- 5.Santos ALS, d’Avila-Levy CM, Branquinha MH. Anti-trypanosomatid properties of cystatin superfamily: implications on parasite development and virulence. In: Cohen JB, Ryseck LP, editors. Cystatins: protease inhibitors, biomarkers and immunomodulators. New York: Nova Science Publishers; 2011: In press. [Google Scholar]
- 6.Santos ALS. Aspartic peptidase inhibitors as potential bioactive pharmacological compounds against human fungal pathogens. Chapter 13. In: Ahmad I, Owais M, Shahid M, Aqil F, editors. Combating fungal infections: problems and remedy. Berlin: Springer-Verlag; 2010. pp. 289–326. [Google Scholar]
- 7.Santos AL, Bittencourt VC, Pinto MR, Silva BA, Barreto-Bergter E. Biochemical characterization of potential virulence markers in the human fungal pathogen Pseudallescheria boydii. Med Mycol. 2009;47:375–386. doi: 10.1080/13693780802610305. [DOI] [PubMed] [Google Scholar]
- 8.Santos AL, Palmeira VF, Rozental S, Kneipp LF, Nimrichter L, Alviano DS, Rodrigues ML, Alviano CS. Biology and pathogenesis of Fonsecaea pedrosoi, the major etiologic agent of chromoblastomycosis. FEMS Microbiol Rev. 2007;31:570–591. doi: 10.1111/j.1574-6976.2007.00077.x. [DOI] [PubMed] [Google Scholar]
- 9.Santos AL, d'Avila-Levy CM, Elias CG, Vermelho AB, Branquinha MH. Phytomonas serpens: immunological similarities with the human trypanosomatid pathogens. Microbes Infect. 2007;9:915–921. doi: 10.1016/j.micinf.2007.03.018. [DOI] [PubMed] [Google Scholar]
- 10.Vermelho AB, Giovanni De Simone S, d'Avila-Levy CM, Santos ALS, Nogueira de Melo AC, Silva-Junior FP, Bom EP, Branquinha MH. Trypanosomatidae peptidases: a target for drugs development. Curr Enz Inhib. 2007;3:19–48. [Google Scholar]
- 11.Santos AL, Branquinha MH, D'Avila-Levy CM. The ubiquitous gp63-like metalloprotease from lower trypanosomatids: in the search for a function. An Acad Bras Cienc. 2006;78:687–714. doi: 10.1590/s0001-37652006000400006. [DOI] [PubMed] [Google Scholar]
- 12.Rao MB, Tanksale AM, Ghatge MS, Deshpande VV. Molecular and biotechnological aspects of microbial proteases. Microbiol Mol Biol Rev. 1998;62:597–635. doi: 10.1128/mmbr.62.3.597-635.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Barrett AJ, Rawlings ND, O'Brien EA. The MEROPS database as a protease information system. J Struct Biol. 2001;134:95–102. doi: 10.1006/jsbi.2000.4332. [DOI] [PubMed] [Google Scholar]
- 14.Barrett AJ, Tolle DP, Rawlings ND. Managing peptidases in the genomic era. Biol Chem. 2003;384:873–882. doi: 10.1515/BC.2003.098. [DOI] [PubMed] [Google Scholar]
- 15.Rawlings ND, Morton FR, Barrett AJ. MEROPS: the peptidase database. Nucleic Acids Res. 2006;34:D270–D272. doi: 10.1093/nar/gkj089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rawlings ND, Tolle DP, Barrett AJ. Evolutionary families of peptidase inhibitors. Biochem J. 2004;378:705–716. doi: 10.1042/BJ20031825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Bode W, Huber R. Structural basis of the endoproteinase-protein inhibitor interaction. Biochim Biophys Acta. 2000;1477:241–252. doi: 10.1016/s0167-4838(99)00276-9. [DOI] [PubMed] [Google Scholar]
- 18.McKerrow JH, Sun E, Rosenthal PJ, Bouvier J. The proteases and pathogenicity of parasitic protozoa. Annu Rev Microbiol. 1993;47:821–853. doi: 10.1146/annurev.mi.47.100193.004133. [DOI] [PubMed] [Google Scholar]
- 19.Mottram JC, Brooks DR, Coombs GH. Roles of cysteine proteinases of trypanosomes and Leishmania in host-parasite interactions. Curr Opin Microbiol. 1998;1:455–460. doi: 10.1016/s1369-5274(98)80065-9. [DOI] [PubMed] [Google Scholar]
- 20.Hube B. Extracellular proteinases of human pathogenic fungi. Contrib Microbiol. 2000;5:126–137. doi: 10.1159/000060350. [DOI] [PubMed] [Google Scholar]
- 21.Monod M, Capoccia S, Léchenne B, Zaugg C, Holdom M, Jousson O. Secreted proteases from pathogenic fungi. Int J Med Microbiol. 2002;292:405–419. doi: 10.1078/1438-4221-00223. [DOI] [PubMed] [Google Scholar]
- 22.Klemba M, Goldberg DE. Biological roles of proteases in parasitic protozoa. Annu Rev Biochem. 2002;71:275–305. doi: 10.1146/annurev.biochem.71.090501.145453. [DOI] [PubMed] [Google Scholar]
- 23.Atkinson HJ, Babbitt PC, Sajid M. The global cysteine peptidase landscape in parasites. Trends Parasitol. 2009;25:573–581. doi: 10.1016/j.pt.2009.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Yao C. Major surface protease of trypanosomatids: one size fits all. Infect Immun. 2010;78:22–31. doi: 10.1128/IAI.00776-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rodriques Coura J, de Castro SL. A critical review on Chagas disease chemotherapy. Mem Inst Oswaldo Cruz. 2002;97:3–24. doi: 10.1590/s0074-02762002000100001. [DOI] [PubMed] [Google Scholar]
- 26.Croft SL, Yardley V. Chemotherapy of leishmaniasis. Curr Pharm Des. 2002;8:319–342. doi: 10.2174/1381612023396258. [DOI] [PubMed] [Google Scholar]
- 27.Juang P. Update on new antifungal therapy. AACN Adv Crit Care. 2007;18:253–260; quiz 261-262. doi: 10.4037/15597768-2007-3004. [DOI] [PubMed] [Google Scholar]
- 28.Lai CC, Tan CK, Huang YT, Shao PL, Hsueh PR. Current challenges in the management of invasive fungal infections. J Infect Chemother. 2008;14:77–85. doi: 10.1007/s10156-007-0595-7. [DOI] [PubMed] [Google Scholar]
- 29.Leung D, Abbenante G, Fairlie DP. Protease inhibitors: current status and future prospects. J Med Chem. 2000;43:305–341. doi: 10.1021/jm990412m. [DOI] [PubMed] [Google Scholar]
- 30.Abbenante G, Fairlie DP. Protease inhibitors in the clinic. Med Chem. 2005;1:71–104. doi: 10.2174/1573406053402569. [DOI] [PubMed] [Google Scholar]
- 31.Flexner C. HIV-protease inhibitors. N Engl J Med. 1998;338:1281–1292. doi: 10.1056/NEJM199804303381808. [DOI] [PubMed] [Google Scholar]
- 32.McKerrow JH, Engel JC, Caffrey CR. Cysteine protease inhibitors as chemotherapy for parasitic infections. Bioorg Med Chem. 1999;7:639–644. doi: 10.1016/s0968-0896(99)00008-5. [DOI] [PubMed] [Google Scholar]
- 33.Coombs GH, Goldberg DE, Klemba M, Berry C, Kay J, Mottram JC. Aspartic proteases of Plasmodium falciparum and other parasitic protozoa as drug targets. Trends Parasitol. 2001;17:532–537. doi: 10.1016/s1471-4922(01)02037-2. [DOI] [PubMed] [Google Scholar]
- 34.Stewart K, Abad-Zapatero C. Candida proteases and their inhibition: prospects for antifungal therapy. Curr Med Chem. 2001;8:941–948. doi: 10.2174/0929867013372698. [DOI] [PubMed] [Google Scholar]
- 35.Dash C, Kulkarni A, Dunn B, Rao M. Aspartic peptidase inhibitors: implications in drug development. Crit Rev Biochem Mol Biol. 2003;38:89–119. doi: 10.1080/713609213. [DOI] [PubMed] [Google Scholar]
- 36.Pozio E, Morales MA. The impact of HIV-protease inhibitors on opportunistic parasites. Trends Parasitol. 2005;21:58–63. doi: 10.1016/j.pt.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Mastrolorenzo A, Rusconi S, Scozzafava A, Barbaro G, Supuran CT. Inhibitors of HIV-1 protease: current state of the art 10 years after their introduction. From antiretroviral drugs to antifungal, antibacterial and antitumor agents based on aspartic protease inhibitors. Curr Med Chem. 2007;14:2734–2748. doi: 10.2174/092986707782360141. [DOI] [PubMed] [Google Scholar]
- 38.Nguyen JT, Hamada Y, Kimura T, Kiso Y. Design of potent aspartic protease inhibitors to treat various diseases. Arch Pharm (Weinheim) 2008;341:523–535. doi: 10.1002/ardp.200700267. [DOI] [PubMed] [Google Scholar]
- 39.McKerrow JH, Rosenthal PJ, Swenerton R, Doyle P. Development of protease inhibitors for protozoan infections. Curr Opin Infect Dis. 2008;21:668–672. doi: 10.1097/QCO.0b013e328315cca9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Calderone R, Odds FC, Boekhout T. Candida albicans: fundamental research on an opportunistic human pathogen. FEMS Yeast Res. 2009;9:971–972. doi: 10.1111/j.1567-1364.2009.00585.x. [DOI] [PubMed] [Google Scholar]
- 41.Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20:133–163. doi: 10.1128/CMR.00029-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.López-Martínez R. Candidosis, a new challenge. Clin Dermatol. 2010;28:178–184. doi: 10.1016/j.clindermatol.2009.12.014. [DOI] [PubMed] [Google Scholar]
- 43.van de Veerdonk FL, Kullberg BJ, Netea MG. Pathogenesis of invasive candidiasis. Curr Opin Crit Care. 2010;16:453–459. doi: 10.1097/MCC.0b013e32833e046e. [DOI] [PubMed] [Google Scholar]
- 44.Wilson LS, Reyes CM, Stolpman M, Speckman J, Allen K, Beney J. The direct cost and incidence of systemic fungal infections. Value Health. 2002;5:26–34. doi: 10.1046/j.1524-4733.2002.51108.x. [DOI] [PubMed] [Google Scholar]
- 45.Pfaller MA, Diekema DJ. Role of sentinel surveillance of candidemia: trends in species distribution and antifungal susceptibility. J Clin Microbiol. 2002;40:3551–3557. doi: 10.1128/JCM.40.10.3551-3557.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Montravers P, Jabbour K. Clinical consequences of resistant Candida infections in intensive care. Int J Antimicrob Agents. 2006;27:1–6. doi: 10.1016/j.ijantimicag.2005.11.002. [DOI] [PubMed] [Google Scholar]
- 47.Hsueh PR, Graybill JR, Playford EG, Watcharananan SP, Oh MD, Ja'alam K, Huang S, Nangia V, Kurup A, Padiglione AA. Consensus statement on the management of invasive candidiasis in Intensive Care Units in the Asia-Pacific Region. Int J Antimicrob Agents. 2009;34:205–209. doi: 10.1016/j.ijantimicag.2009.03.014. [DOI] [PubMed] [Google Scholar]
- 48.Niimi M, Firth NA, Cannon RD. Antifungal drug resistance of oral fungi. Odontology. 2010;98:15–25. doi: 10.1007/s10266-009-0118-3. [DOI] [PubMed] [Google Scholar]
- 49.Ghannoum MA. Potential role of phospholipases in virulence and fungal pathogenesis. Clin Microbiol Rev. 2000;13:122–143, table of contents. doi: 10.1128/cmr.13.1.122-143.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Calderone RA, Ronald LC. Host recognition. In: Calderone RA, Ronald LC, editors. Fungal pathogenesis: principles and clinical applications. New York: Marcel Dekker; 2002. pp. 1–24. [Google Scholar]
- 51.Yang YL. Virulence factors of Candida species. J Microbiol Immunol Infect. 2003;36:223–228. [PubMed] [Google Scholar]
- 52.Whiteway M, Oberholzer U. Candida morphogenesis and host-pathogen interactions. Curr Opin Microbiol. 2004;7:350–357. doi: 10.1016/j.mib.2004.06.005. [DOI] [PubMed] [Google Scholar]
- 53.Brown AJ, Odds FC, Gow NA. Infection-related gene expression in Candida albicans. Curr Opin Microbiol. 2007;10:307–313. doi: 10.1016/j.mib.2007.04.001. [DOI] [PubMed] [Google Scholar]
- 54.Seider K, Heyken A, Lüttich A, Miramón P, Hube B. Interaction of pathogenic yeasts with phagocytes: survival, persistence and escape. Curr Opin Microbiol. 2010;13:392–400. doi: 10.1016/j.mib.2010.05.001. [DOI] [PubMed] [Google Scholar]
- 55.Schaller M, Borelli C, Korting HC, Hube B. Hydrolytic enzymes as virulence factors of Candida albicans. Mycoses. 2005;48:365–377. doi: 10.1111/j.1439-0507.2005.01165.x. [DOI] [PubMed] [Google Scholar]
- 56.De Bernardis F, Sullivan PA, Cassone A. Aspartyl proteinases of Candida albicans and their role in pathogenicity. Med Mycol. 2001;39:303–313. doi: 10.1080/mmy.39.4.303.313. [DOI] [PubMed] [Google Scholar]
- 57.Hube B, Naglik J. Candida albicans proteinases: resolving the mystery of a gene family. Microbiology. 2001;147:1997–2005. doi: 10.1099/00221287-147-8-1997. [DOI] [PubMed] [Google Scholar]
- 58.Naglik JR, Challacombe SJ, Hube B. Candida albicans secreted aspartyl proteinases in virulence and pathogenesis. Microbiol Mol Biol Rev. 2003;67:400–428, table of contents. doi: 10.1128/MMBR.67.3.400-428.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Naglik J, Albrecht A, Bader O, Hube B. Candida albicans proteinases and host/pathogen interactions. Cell Microbiol. 2004;6:915–926. doi: 10.1111/j.1462-5822.2004.00439.x. [DOI] [PubMed] [Google Scholar]
- 60.Abad-Zapatero C, Goldman R, Muchmore SW, Hutchins C, Stewart K, Navaza J, Payne CD, Ray TL. Structure of a secreted aspartic protease from C. albicans complexed with a potent inhibitor: implications for the design of antifungal agents. Protein Sci. 1996;5:640–652. doi: 10.1002/pro.5560050408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Korting HC, Schaller M, Eder G, Hamm G, Böhmer U, Hube B. Effects of the human immunodeficiency virus (HIV) proteinase inhibitors saquinavir and indinavir on in vitro activities of secreted aspartyl proteinases of Candida albicans isolates from HIV-infected patients. Antimicrob Agents Chemother. 1999;43:2038–2042. doi: 10.1128/aac.43.8.2038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Cassone A, De Bernardis F, Torosantucci A, Tacconelli E, Tumbarello M, Cauda R. In vitro and in vivo anticandidal activity of human immunodeficiency virus protease inhibitors. J Infect Dis. 1999;180:448–453. doi: 10.1086/314871. [DOI] [PubMed] [Google Scholar]
- 63.Borg-von Zepelin M, Meyer I, Thomssen R, Würzner R, Sanglard D, Telenti A, Monod M. HIV-Protease inhibitors reduce cell adherence of Candida albicans strains by inhibition of yeast secreted aspartic proteases. J Invest Dermatol. 1999;113:747–751. doi: 10.1046/j.1523-1747.1999.00747.x. [DOI] [PubMed] [Google Scholar]
- 64.Gruber A, Speth C, Lukasser-Vogl E, Zangerle R, Borg-von Zepelin M, Dierich MP, Würzner R. Human immunodeficiency virus type 1 protease inhibitor attenuates Candida albicans virulence properties in vitro. Immunopharmacology. 1999;41:227–234. doi: 10.1016/s0162-3109(99)00035-1. [DOI] [PubMed] [Google Scholar]
- 65.Gruber A, Berlit J, Speth C, Lass-Flörl C, Kofler G, Nagl M, Borg-von Zepelin M, Dierich MP, Würzner R. Dissimilar attenuation of Candida albicans virulence properties by human immunodeficiency virus type 1 protease inhibitors. Immunobiology. 1999;201:133–144. doi: 10.1016/S0171-2985(99)80052-7. [DOI] [PubMed] [Google Scholar]
- 66.Bektić J, Lell CP, Fuchs A, Stoiber H, Speth C, Lass-Flörl C, Borg-von Zepelin M, Dierich MP, Würzner R. HIV protease inhibitors attenuate adherence of Candida albicans to epithelial cells in vitro. FEMS Immunol Med Microbiol. 2001;31:65–71. doi: 10.1111/j.1574-695X.2001.tb01588.x. [DOI] [PubMed] [Google Scholar]
- 67.Schaller M, Krnjaic N, Niewerth M, Hamm G, Hube B, Korting HC. Effect of antimycotic agents on the activity of aspartyl proteinases secreted by Candida albicans. J Med Microbiol. 2003;52:247–249. doi: 10.1099/jmm.0.05048-0. [DOI] [PubMed] [Google Scholar]
- 68.Casolari C, Rossi T, Baggio G, Coppi A, Zandomeneghi G, Ruberto AI, Farina C, Fabio G, Zanca A, Castelli M. Interaction between saquinavir and antimycotic drugs on C. albicans and C. neoformans strains. Pharmacol Res. 2004;50:605–610. doi: 10.1016/j.phrs.2004.06.008. [DOI] [PubMed] [Google Scholar]
- 69.Falkensammer B, Pilz G, Bektić J, Imwidthaya P, Jöhrer K, Speth C, Lass-Flörl C, Dierich MP, Würzner R. Absent reduction by HIV protease inhibitors of Candida albicans adhesion to endothelial cells. Mycoses. 2007;50:172–177. doi: 10.1111/j.1439-0507.2006.01353.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cenci E, Francisci D, Belfiori B, Pierucci S, Baldelli F, Bistoni F, Vecchiarelli A. Tipranavir exhibits different effects on opportunistic pathogenic fungi. J Infect. 2008;56:58–64. doi: 10.1016/j.jinf.2007.08.004. [DOI] [PubMed] [Google Scholar]
- 71.Tsang CS, Hong I. HIV protease inhibitors differentially inhibit adhesion of Candida albicans to acrylic surfaces. Mycoses. 2010;53:488–494. doi: 10.1111/j.1439-0507.2009.01743.x. [DOI] [PubMed] [Google Scholar]
- 72.Braga-Silva LA, Mogami SS, Valle RS, Silva-Neto ID, Santos AL. Multiple effects of amprenavir against Candida albicans. FEMS Yeast Res. 2010;10:221–224. doi: 10.1111/j.1567-1364.2009.00595.x. [DOI] [PubMed] [Google Scholar]
- 73.Katoh I, Yasunaga T, Ikawa Y, Yoshinaka Y. Inhibition of retroviral protease activity by an aspartyl proteinase inhibitor. Nature. 1987;329:654–656. doi: 10.1038/329654a0. [DOI] [PubMed] [Google Scholar]
- 74.Hugen PW, Burger DM, de Graaff M, ter Hofstede HJ, Hoetelmans RM, Brinkman K, Meenhorst PL, Mulder JW, Koopmans PP, Hekster YA. Saliva as a specimen for monitoring compliance but not for predicting plasma concentrations in patients with HIV treated with indinavir. Ther Drug Monit. 2000;22:437–445. doi: 10.1097/00007691-200008000-00013. [DOI] [PubMed] [Google Scholar]
- 75.Atzori C, Villani P, Regazzi M, Maruzzi M, Cargnel A. Detection of intrapulmonary concentration of lopinavir in an HIV-infected patient. AIDS. 2003;17:1710–1711. doi: 10.1097/00002030-200307250-00022. [DOI] [PubMed] [Google Scholar]
- 76.Bonifaz A, Carrasco-Gerard E, Saúl A. Chromoblastomycosis: clinical and mycologic experience of 51 cases. Mycoses. 2001;44:1–7. doi: 10.1046/j.1439-0507.2001.00613.x. [DOI] [PubMed] [Google Scholar]
- 77.Esterre P, Queiroz-Telles F. Management of chromoblastomycosis: novel perspectives. Curr Opin Infect Dis. 2006;19:148–152. doi: 10.1097/01.qco.0000216625.28692.67. [DOI] [PubMed] [Google Scholar]
- 78.López Martínez R, Méndez Tovar LJ. Chromoblastomycosis. Clin Dermatol. 2007;25:188–194. doi: 10.1016/j.clindermatol.2006.05.007. [DOI] [PubMed] [Google Scholar]
- 79.Ameen M. Chromoblastomycosis: clinical presentation and management. Clin Exp Dermatol. 2009;34:849–854. doi: 10.1111/j.1365-2230.2009.03415.x. [DOI] [PubMed] [Google Scholar]
- 80.Palmeira VF, Kneipp LF, Alviano CS, dos Santos AL. The major chromoblastomycosis fungal pathogen, Fonsecaea pedrosoi, extracellularly releases proteolytic enzymes whose expression is modulated by culture medium composition: implications on the fungal development and cleavage of key's host structures. FEMS Immunol Med Microbiol. 2006;46:21–29. doi: 10.1111/j.1574-695X.2005.00003.x. [DOI] [PubMed] [Google Scholar]
- 81.Palmeira VF, Kneipp LF, Alviano CS, dos Santos AL. Secretory aspartyl peptidase activity from mycelia of the human fungal pathogen Fonsecaea pedrosoi: effect of HIV aspartyl proteolytic inhibitors. Res Microbiol. 2006;157:819–826. doi: 10.1016/j.resmic.2006.07.003. [DOI] [PubMed] [Google Scholar]
- 82.Palmeira VF, Kneipp LF, Alviano CS, dos Santos AL. Phospholipase and esterase production by clinical strains of Fonsecaea pedrosoi and their interactions with epithelial cells. Mycopathologia. 2010;170:31–37. doi: 10.1007/s11046-010-9293-6. [DOI] [PubMed] [Google Scholar]
- 83.Palmeira VF, Kneipp LF, Rozental S, Alviano CS, Santos AL. Beneficial effects of HIV peptidase inhibitors on Fonsecaea pedrosoi: promising compounds to arrest key fungal biological processes and virulence. PLoS One. 2008;3:e3382. doi: 10.1371/journal.pone.0003382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Matlashewski G. Leishmania infection and virulence. Med Microbiol Immunol. 2001;190:37–42. doi: 10.1007/s004300100076. [DOI] [PubMed] [Google Scholar]
- 85.De Souza W. From the cell biology to the development of new chemotherapeutic approaches against trypanosomatids: dreams and reality. Kinetoplastid Biol Dis. 2002;1:3. doi: 10.1186/1475-9292-1-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Castillo E, Dea-Ayuela MA, Bolás-Fernández F, Rangel M, González-Rosende ME. The kinetoplastid chemotherapy revisited: current drugs, recent advances and future perspectives. Curr Med Chem. 2010;17:4027–4051. doi: 10.2174/092986710793205345. [DOI] [PubMed] [Google Scholar]
- 87.Bates PA, Rogers ME. New insights into the developmental biology and transmission mechanisms of Leishmania. Curr Mol Med. 2004;4:601–609. doi: 10.2174/1566524043360285. [DOI] [PubMed] [Google Scholar]
- 88.Bañuls AL, Hide M, Prugnolle F. Leishmania and the leishmaniases: a parasite genetic update and advances in taxonomy, epidemiology and pathogenicity in humans. Adv Parasitol. 2007;64:1–109. doi: 10.1016/S0065-308X(06)64001-3. [DOI] [PubMed] [Google Scholar]
- 89.Sereno D, Cordeiro da Silva A, Mathieu-Daude F, Ouaissi A. Advances and perspectives in Leishmania cell based drug-screening procedures. Parasitol Int. 2007;56:3–7. doi: 10.1016/j.parint.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 90.Desjeux P, Alvar J. Leishmania/HIV co-infections: epidemiology in Europe. Ann Trop Med Parasitol. 2003;97 Suppl 1:3–15. doi: 10.1179/000349803225002499. [DOI] [PubMed] [Google Scholar]
- 91.Rabello A, Orsini M, Disch J. Leishmania/HIV co-infection in Brazil: an appraisal. Ann Trop Med Parasitol. 2003;97 Suppl 1:17–28. doi: 10.1179/000349803225002507. [DOI] [PubMed] [Google Scholar]
- 92.Alvar J, Aparicio P, Aseffa A, Den Boer M, Cañavate C, Dedet JP, Gradoni L, Ter Horst R, López-Vélez R, Moreno J. The relationship between leishmaniasis and AIDS: the second 10 years. Clin Microbiol Rev. 2008;21:334–359, table of contents. doi: 10.1128/CMR.00061-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Ezra N, Ochoa MT, Craft N. Human immunodeficiency virus and leishmaniasis. J Glob Infect Dis. 2010;2:248–257. doi: 10.4103/0974-777X.68528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.del Giudice P, Mary-Krause M, Pradier C, Grabar S, Dellamonica P, Marty P, Gastaut JA, Costagliola D, Rosenthal E. Impact of highly active antiretroviral therapy on the incidence of visceral leishmaniasis in a French cohort of patients infected with human immunodeficiency virus. J Infect Dis. 2002;186:1366–1370. doi: 10.1086/344325. [DOI] [PubMed] [Google Scholar]
- 95.de La Rosa R, Pineda JA, Delgado J, Macías J, Morillas F, Mira JA, Sánchez-Quijano A, Leal M, Lissen E. Incidence of and risk factors for symptomatic visceral leishmaniasis among human immunodeficiency virus type 1-infected patients from Spain in the era of highly active antiretroviral therapy. J Clin Microbiol. 2002;40:762–767. doi: 10.1128/JCM.40.3.762-767.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Alves CR, Corte-Real S, Bourguignon SC, Chaves CS, Saraiva EM. Leishmania amazonensis: early proteinase activities during promastigote-amastigote differentiation in vitro. Exp Parasitol. 2005;109:38–48. doi: 10.1016/j.exppara.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 97.Valdivieso E, Dagger F, Rascón A. Leishmania mexicana: identification and characterization of an aspartyl proteinase activity. Exp Parasitol. 2007;116:77–82. doi: 10.1016/j.exppara.2006.10.006. [DOI] [PubMed] [Google Scholar]
- 98.Zhang T, Maekawa Y, Yasutomo K, Ishikawa H, Fawzy Nashed B, Dainichi T, Hisaeda H, Sakai T, Kasai M, Mizuochi T, et al. Pepstatin A-sensitive aspartic proteases in lysosome are involved in degradation of the invariant chain and antigen-processing in antigen presenting cells of mice infected with Leishmania major. Biochem Biophys Res Commun. 2000;276:693–701. doi: 10.1006/bbrc.2000.3538. [DOI] [PubMed] [Google Scholar]
- 99.Savoia D, Allice T, Tovo PA. Antileishmanial activity of HIV protease inhibitors. Int J Antimicrob Agents. 2005;26:92–94. doi: 10.1016/j.ijantimicag.2005.04.003. [DOI] [PubMed] [Google Scholar]
- 100.Trudel N, Garg R, Messier N, Sundar S, Ouellette M, Tremblay MJ. Intracellular survival of Leishmania species that cause visceral leishmaniasis is significantly reduced by HIV-1 protease inhibitors. J Infect Dis. 2008;198:1292–1299. doi: 10.1086/592280. [DOI] [PubMed] [Google Scholar]
- 101.Kumar P, Lodge R, Trudel N, Ouellet M, Ouellette M, Tremblay MJ. Nelfinavir, an HIV-1 protease inhibitor, induces oxidative stress-mediated, caspase-independent apoptosis in Leishmania amastigotes. PLoS Negl Trop Dis. 2010;4:e642. doi: 10.1371/journal.pntd.0000642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Valdivieso E, Rangel A, Moreno J, Saugar JM, Cañavate C, Alvar J, Dagger F. Effects of HIV aspartyl-proteinase inhibitors on Leishmania sp. Exp Parasitol. 2010;126:557–563. doi: 10.1016/j.exppara.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 103.Santos LO, Marinho FA, Altoé EF, Vitório BS, Alves CR, Britto C, Motta MC, Branquinha MH, Santos AL, d'Avila-Levy CM. HIV aspartyl peptidase inhibitors interfere with cellular proliferation, ultrastructure and macrophage infection of Leishmania amazonensis. PLoS One. 2009;4:e4918. doi: 10.1371/journal.pone.0004918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.White TC, Miyasaki SH, Agabian N. Three distinct secreted aspartyl proteinases in Candida albicans. J Bacteriol. 1993;175:6126–6133. doi: 10.1128/jb.175.19.6126-6133.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.de Brito Costa EM, dos Santos AL, Cardoso AS, Portela MB, Abreu CM, Alviano CS, Hagler AN, de Araújo Soares RM. Heterogeneity of metallo and serine extracellular proteinases in oral clinical isolates of Candida albicans in HIV-positive and healthy children from Rio de Janeiro, Brazil. FEMS Immunol Med Microbiol. 2003;38:173–180. doi: 10.1016/S0928-8244(03)00145-7. [DOI] [PubMed] [Google Scholar]
- 106.dos Santos AL, de Carvalho IM, da Silva BA, Portela MB, Alviano CS, de Araújo Soares RM. Secretion of serine peptidase by a clinical strain of Candida albicans: influence of growth conditions and cleavage of human serum proteins and extracellular matrix components. FEMS Immunol Med Microbiol. 2006;46:209–220. doi: 10.1111/j.1574-695X.2005.00023.x. [DOI] [PubMed] [Google Scholar]
- 107.Braga-Silva LA, Mesquita DG, Ribeiro MD, Carvalho SM, Fracalanzza SE, Santos AL. Trailing end-point phenotype antibiotic-sensitive strains of Candida albicans produce different amounts of aspartyl peptidases. Braz J Med Biol Res. 2009;42:765–770. doi: 10.1590/s0100-879x2009000800013. [DOI] [PubMed] [Google Scholar]
- 108.Dos Santos AL, Soares RM. Candida guilliermondii isolated from HIV-infected human secretes a 50 kDa serine proteinase that cleaves a broad spectrum of proteinaceous substrates. FEMS Immunol Med Microbiol. 2005;43:13–20. doi: 10.1016/j.femsim.2004.06.022. [DOI] [PubMed] [Google Scholar]
- 109.Albrecht A, Felk A, Pichova I, Naglik JR, Schaller M, de Groot P, Maccallum D, Odds FC, Schäfer W, Klis F, et al. Glycosylphosphatidylinositol-anchored proteases of Candida albicans target proteins necessary for both cellular processes and host-pathogen interactions. J Biol Chem. 2006;281:688–694. doi: 10.1074/jbc.M509297200. [DOI] [PubMed] [Google Scholar]
- 110.Schild L, Heyken A, de Groot PW, Hiller E, Mock M, de Koster C, Horn U, Rupp S, Hube B. Proteolytic cleavage of covalently linked cell wall proteins by Candida albicans Sap9 and Sap10. Eukaryot Cell. 2011;10:98–109. doi: 10.1128/EC.00210-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Cutfield S, Marshall C, Moody P, Sullivan P, Cutfield J. Crystallization of inhibited aspartic proteinase from Candida albicans. J Mol Biol. 1993;234:1266–1269. doi: 10.1006/jmbi.1993.1679. [DOI] [PubMed] [Google Scholar]
- 112.Borelli C, Ruge E, Schaller M, Monod M, Korting HC, Huber R, Maskos K. The crystal structure of the secreted aspartic proteinase 3 from Candida albicans and its complex with pepstatin A. Proteins. 2007;68:738–748. doi: 10.1002/prot.21425. [DOI] [PubMed] [Google Scholar]
- 113.Borelli C, Ruge E, Lee JH, Schaller M, Vogelsang A, Monod M, Korting HC, Huber R, Maskos K. X-ray structures of Sap1 and Sap5: structural comparison of the secreted aspartic proteinases from Candida albicans. Proteins. 2008;72:1308–1319. doi: 10.1002/prot.22021. [DOI] [PubMed] [Google Scholar]