Abstract
Objective:
The objective of this study was to see whether levels of alcohol consumption newly included as “moderate” in proposed changes to the 2010 Dietary Guidelines for Americans are associated with significant levels of alcohol-related harm.
Method:
Using longitudinal data from a nationally representative sample of U.S. adults (N = 26,438; 51.8% female), we compared relative risks and population attributable fractions for nine measures of concurrent and eight measures of prospective alcohol-related harm among three groups of drinkers: those whose consumption lay within the old 2005 Dietary Guidelines for Americans guidelines for moderate drinking, those in the “gray area” of consumption between the 2005 and proposed 2010 Dietary Guidelines for Americans, and those who exceeded the proposed 2010 Dietary Guidelines for Americans.
Results:
The gray area of consumption was associated with small but significantly increased risks of prevalent and incident alcohol dependence, incident alcohol-related interpersonal problems, and prevalent job loss. There were no associations with medical conditions or mental disorders. Although the harms associated with this level of consumption reflected low absolute and/or relative risks of harm, their impact was not negligible because of the large proportion of drinkers in the gray area of consumption (29.1%). The overwhelming majority of incident harm among baseline gray area drinkers was associated with consumption that had increased over the follow-up interval to exceed the proposed 2010 Dietary Guidelines for Americans.
Conclusions:
We recommend two alternative approaches to rewording the proposed changes to the 2010 Dietary Guidelines for Americans that would avoid suggesting that there are benefits associated with the gray area of alcohol consumption.
The united states has two major sets of drinking guidelines. The National Institute on Alcohol Abuse and Alcoholism (NIAAA) defines low-risk drinking as 14 or fewer drinks per week and 4 or fewer drinks on any day for men and 7 or fewer drinks per week and 3 or fewer drinks on any day for women (http://rethinkingdrink-ing.niaaa.nih.gov). The Dietary Guidelines for Americans (DGA), a joint effort of the Departments of Agriculture and Health and Human Services, contain recommended moderate (as opposed to low-risk) drinking levels that are currently undergoing revision. Whereas the 2005 DGA (http://www.cnpp.usda.gov/DGAs2005Guidelines.htm) defined moderate drinking as one drink per day for women and two drinks or less per day for men, not to be exceeded on any day, the proposed new 2010 DGA (http://www.cnpp.usda.gov/DGAs2010-DGACReport.htm) limit men to two drinks or less per day on average and four or fewer on any single day and limit women to one drink or less per day on average and three or fewer on any single day.
These proposed new limits, which differ from the NIAAA low-risk drinking guidelines only in whether average volume limits are expressed as drinks per week or average drinks per day, represent a significant shift in thinking. Whereas the former DGA restricted men to two drinks or less on any day, they now permit up to four drinks on some days, as long as the daily average does not exceed two drinks; likewise, whereas women were formerly restricted to no more than one drink on any day, they are now permitted up to three drinks on some days. (Like most drinking guidelines, both the 2005 and the proposed 2010 DGA note special population groups for which lower limits or total abstinence is recommended. These include individuals unable to control their alcohol intake; women who are or may become pregnant; lactating women; children and adolescents; individuals taking medications that may interact with alcohol; and those engaged in activities that require attention, skill, or coordination.)
Public responses to the proposed 2010 DGA have raised concerns about the public health ramifications of the revised definition of moderate drinking (http://www.cnpp.usda.gov/dietaryguidelines.htm), arguing that the proposed revision permits drinking patterns that should not be considered moderate. For example, whereas both the 2005 and the proposed 2010 DGA implicitly allowed men up to 14 drinks per week, the only way that limit could be reached under the 2005 DGA was by drinking 2 drinks per day every day. Under the proposed new DGA, men could consume four drinks per day three times a week and still be defined as moderate drinkers. Similarly, women could consume three drinks per day twice a week and lie within moderate drinking limits.
Is it appropriate to define drinking patterns such as these as “moderate drinking,” and will the revision of the moderate drinking guidelines result in an increased risk of adverse consequences associated with so-called moderate drinking? Using longitudinal data from a nationally representative sample of U.S. adults, we addressed these questions by comparing the risks of concurrent and prospective alcohol-related harm among three groups of drinkers: (a) those whose consumption lies within the 2005 DGA guidelines for moderate drinking, (b) those in what we will term the “gray area” of consumption between the 2005 and the proposed 2010 DGA, and (c) those who exceed the proposed 2010 DGA. The third group also represents those whose consumption exceeds the NIAAA low-risk drinking guidelines.
Method
Sample
This study used data from two waves of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). The 2001–2002 Wave 1 nationally representative sample contained 43,093 U.S. adults 18 and older living in households and selected group quarters (response rate = 81.0%). The 2004–2005 Wave 2 follow-up sample contained 34,653 of the original respondents, 86.7% of those eligible for re-interview (cumulative response rate = 70.2%). Data were weighted to reflect design characteristics and oversam-pling of Blacks, Hispanics, and young adults; adjusted for nonresponse at the household and person levels; and further adjusted to match the sociodemographic distribution of the civilian population based on the 2000 Decennial Census (Grant et al., 2003a, 2007). Potential respondents were informed in writing about the nature of the survey, statistical uses of the survey data, voluntary aspect of their participation, and federal laws providing for the confidentiality of identifiable survey information; only those consenting to participate after receiving this information were interviewed. The research protocol, including informed consent procedures, received full ethical review and approval from the U.S. Census Bureau and the U.S. Office of Management and Budget.
This analysis is based on Wave 1 NESARC past-year drinkers with no missing data on consumption (N = 26,438; 51.8% female). To rule out increases in consumption in response to job loss, analyses of past-year job loss were restricted to individuals who had worked at some time during the year and who reported drinking at their current level/pattern for at least a year (n = 18,711). Analyses of prospective outcomes excluded individuals not re-interviewed at Wave 2 and individuals who had already experienced first incidence of a specific disorder at baseline or who were not at risk of marital disruption because of not being married/cohabiting at baseline (n = 11,962–21,886).
Measures
Consumption.
Three consumption exposure groups were created on the basis of (a) the largest quantity of drinks consumed in a single day in the past year for all types of alcoholic beverages combined and (b) average weekly drinks. The latter was derived by dividing annual volume of ethanol intake by 52 and converting to standard drinks of 0.6 oz. (14 g) ethanol. Annual volume was estimated for each of four individual beverage types and, using a separate series of questions, for all alcoholic beverages combined. If the largest quantity of drinks (Qlargest) was ≤5,
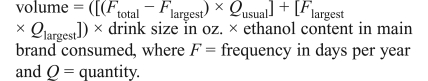 |
If Qlargest > 5,
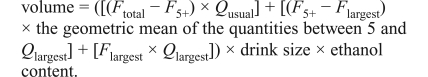 |
Annual volume was set to the larger of (a) the sum of the individual beverage volumes or (b) the volume for all alcoholic beverages combined.
The three exposure groups were defined as follows:
Individuals whose consumption lay within the old 2005 DGA moderate drinking guidelines comprised men who never drank more than two drinks on any day and women who never drank more than one drink on any day.
Individuals in the gray area of consumption comprised men who drank 14 or fewer drinks per week and 4 or fewer drinks on any day but who drank more than 2 drinks on at least one day and women who drank 7 or fewer drinks per week and 3 or fewer drinks on any day but who drank more than 1 drink on at least 1 day.
Individuals who exceeded the proposed new 2010 DGA comprised men who drank more than 14 drinks per week or more than 4 drinks on at least 1 day and women whodrank more than 7 drinks per week or more than 3 drink son at least 1 day.
Alcohol-related harm.
This analysis examined nine measures of past-year harm: alcohol dependence, alcohol-related interpersonal problems (fighting or problems with family and friends), mood and/or anxiety disorder, liver disease, hypertension, gastric disease, coronary heart disease, in-jury, and job loss. In addition, it examined eight measures of prospective harm: 3-year incident alcohol dependence, alcohol-related interpersonal problems, mood or anxiety disorder, liver disease, hypertension, gastric disease, coronary heart disease, and marital dissolution. Alcohol abuse per se was not considered because its most commonly endorsed symptoms reflect impaired driving, an outcome addressed by special exceptions to the drinking guidelines that recommend not drinking at all before driving. Measurement of alcohol dependence and mood and anxiety disorders conformed to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (American Psychiatric Association, 1994); their derivation and psychometric properties have been described in detail elsewhere (Grant et al., 2003b, 2004). Medical conditions required that the respondent report confirmation by a health professional. Incident disorders required first occurrence of the disorders between Wave 1 and Wave 2. Incidence of marital dissolution required the respondent to have been married or cohabiting at Wave 1 and divorced or separated/stopped living together between Wave 1 and Wave 2.
Analysis
All estimates were derived using SUDAAN 10 (Research Triangle Institute, 2008), a software package that uses Taylor series linearization to account for complex, multistage sample design characteristics. Adjusted odds ratios (AORs) were derived from logistic regression models controlling for age, sex, marital status, education, past-year smoking, and obesity. AORs were converted to relative risks as per Zhang and Yu (1998):
where P0 is the prevalence/incidence of the outcome among drinkers whose consumption lay within the old 2005 DGA daily limits. Population attributable fractions (PAFs) were derived using the formula for polytomous exposure variables recommended by Hanley (2001):
where PF1 and PF2 represent the proportions of drinkers in the gray area and exceeding the new DGA limits, and RR1 and RR2 are the relative risks of the outcome in those two groups. These fractions represent the proportion of alcohol-related harm that would not have occurred in the absence of the exposure variable (i.e., if all drinkers had levels of consumption that lay within the old 2005 DGA daily limits).
Results
Past-year drinkers were fairly evenly divided among those whose consumption lay within the old 2005 DGA limits (31.5%), those whose consumption lay within the gray area between the old and new DGA (29.1%), and those whose consumption exceeded the proposed new DGA (39.4%) (data not shown). As can be seen in Table 1, drinkers in the gray area of consumption experienced a significantly increased risk of two types of past-year alcohol-related harm. Their odds of alcohol dependence were slightly more than doubled (AOR = 2.28), but this corresponded to a prevalence of less than 1%, accounting for only a small proportion of the overall prevalence of alcohol dependence (PAF = .028). Although the proportionate increase in risk was smaller for job loss (AOR = 1.22), the prevalence of this outcome was higher (7.3%), as was the PAF (.051). In addition, gray area drinkers had a significantly reduced risk of injury (AOR = 0.87).
Table 1.
Prevalence/incidence rates (%), adjusted odds ratios (AORs), and population attributable fractions (PAFs) for selected past-year and 3-year incident outcomes, by whether exceeded 2005 and proposed 2010 Dietary Guidelines for Americans (DGA) drinking guidelines: U.S. drinkers 18 years of age and older
| Did not exceed proposed 2010 DGAa |
|||||||||
| Did not exceed 2005 DGAb |
Exceeded 2005 DGA:b gray area drinkers |
Exceeded proposed 2010 DGAa |
|||||||
| Variable | % (SE) | AOR [95% CI] | PAF | % (SE) | AOR [95% CI] | PAF | % (SE) | AOR [95% CI] | PAF |
| Past-year outcomes | |||||||||
| Alcohol dependence | 0.3 (0.1) | 1.00 [ref.] | N.A. | 0.7 (0.1) | 2.28 [1.22,4.25] | .028 | 13.9(0.5) | 33.27 [18.28, 60.56] | .895 |
| Alcohol-related interpersonal problems | 0.1 (0.0) | 1.00 [ref.] | N.A. | 0.3 (0.1) | 2.19 [0.92,5.23] | N.A. | 1.6(0.3) | 28.66 [14.45, 56.87] | .887 |
| Mood or anxiety disorder | 14.3 (0.5) | 1.00 [ref.] | N.A. | 17.9 (0.6) | 1.03 [0.93, 1.14] | N.A. | 21.0(0.5) | 1.21 [1.09,1.33] | .064 |
| Liver disease | 0.5 (0.1) | 1.00 [ref.] | N.A. | 0.5 (0.1) | 1.32 [0.76, 2.30] | N.A. | 0.7(0.1) | 1.69 [1.05, 2.73] | .198 |
| Hypertension | 20.7 (0.7) | 1.00 [ref.] | N.A. | 13.8 (0.4) | 0.92 [0.82, 1.02] | N.A. | 12.0(0.4) | 1.08 [0.97, 1.20] | N.A. |
| Gastric disease | 5.5 (0.3) | 1.00 [ref.] | N.A. | 5.0 (0.3) | 0.96 [0.79, 1.16] | N.A. | 4.5 (0.3) | 0.93 [0.77, 1.12] | N.A. |
| Coronary heart disease | 7.8 (0.4) | 1.00 [ref.] | N.A. | 5.5 (0.4) | 0.90 [0.76, 1.07] | N.A. | 4.7 (0.3) | 0.91 [0.77, 1.09] | N.A. |
| Any injury | 18.8(0.6) | 1.00 [ref.] | N.A. | 17.7 (0.5) | 0.87 [0.79,0.95] | N.A. | 20.4 (0.6) | 0.94 [0.85, 1.03] | N.A. |
| Job loss | 5.9 (0.4) | 1.00 [ref.] | N.A. | 7.3 (0.4) | 1.22 [1.01,1.47] | .051 | 10.6(0.4) | 1.36 [1.15,1.61] | .117 |
| 3-year incident outcomes | |||||||||
| Alcohol dependence | 1.8(0.2) | 1.00 [ref.] | N.A. | 3.1 (0.3) | 1.54 [1.15,2.06] | .092 | 8.5 (0.5) | 3.10 [2.33, 4.13] | .356 |
| Alcohol-related interpersonal problems | 0.5 (0.1) | 1.00 [ref.] | N.A. | 0.9 (0.1) | 1.77 [1.05,2.99] | .087 | 4.2 (0.3) | 5.38 [3.35, 8.65] | .544 |
| Mood or anxiety disorder | 8.8 (0.5) | 1.00 [ref.] | N.A. | 10.7 (0.5) | 0.97 [0.82, 1.15] | N.A. | 10.4(0.5) | 0.93 [0.78, 1.11] | N.A. |
| Liver disease | 0.4(0.1) | 1.00 [ref.] | N.A. | 0.4(0.1) | 1.06 [0.54,2.09] | N.A. | 0.9(0.1) | 2.31 [1.26, 4.21] | .330 |
| Hypertension | 10.1 (0.5) | 1.00 [ref.] | N.A. | 8.1 (0.4) | 0.98 [0.85, 1.13] | N.A. | 7.4 (0.3) | 0.97 [0.84, 1.13] | N.A. |
| Gastric disease | 4.5 (0.3) | 1.00 [ref.] | N.A. | 3.7 (0.3) | 0.85 [0.68, 1.06] | N.A. | 3.0 (0.2) | 0.77 [0.62, 0.95] | N.A. |
| Coronary heart disease | 6.2 (0.4) | 1.00 [ref.] | N.A. | 4.9 (0.3) | 0.98 [0.79, 1.20] | N.A. | 4.0 (0.3) | 0.97 [0.79, 1.18] | N.A. |
| Divorce/separation | 4.1 (0.3) | 1.00 [ref.] | N.A. | 5.0 (0.4) | 0.95 [0.74, 1.22] | N.A. | 7.6 (0.5) | 1.24 [0.98, 1.56] | N.A. |
Notes: Bolded figures represent statistically significant (p < .05) AOR. PAF were estimated only for statistically significant AOR. CI = confidence interval; ref. = reference; n.a. = not applicable. aFor men, no more than two drinks per day on average and no more than four drinks on any day; for women, no more than one drink per day on average and no more than three drinks on any day; bfor men, no more than two drinks on any day; for women, no more than one drink on any day.
p < .05.
Consumption in excess of the new proposed 2010 DGA accounted for 89.5% of the prevalence of alcohol dependence and 11.7% of the prevalence of job loss, reflecting both the larger size of this risk group and its higher levels of excess risk (AOR = 33.27 for alcohol dependence and 1.36 for job loss). Drinkers exceeding the new DGA also had significantly increased risks of alcohol-related interpersonal problems (AOR = 28.66), mood or anxiety disorders (AOR = 1.21), and liver disease (AOR = 1.69), accounting for 88.7%, 6.4%, and 19.8%, respectively, of the prevalence of these conditions.
In terms of prospective harm, the only significant increases in risk among gray area drinkers were in the incidence of alcohol dependence (AOR = 1.54) and alcohol-related interpersonal problems (AOR = 1.77); slightly less than 10% of the incidence of each of these types of harm was attributable to gray area consumption (PAF = .092 and .087, respectively). The excess risks of these outcomes were two to three times as great for consumption in excess of the new DGA (AOR = 3.10 for alcohol dependence and 5.38 for alcohol-related interpersonal problems), accounting for 35.6% and 54.4%, respectively, of the incidence of these outcomes. In addition, this highest-risk drinking pattern was associated with a more than twofold increase in the risk of incident liver disease (AOR = 2.31), accounting for one third of the incidence of this condition (PAF = .330).
Based on self-reported past-year drinking patterns, few of the drinkers in the gray area of consumption drank in what might be considered an immoderate fashion (data not shown). Among men, 5.8% drank four drinks on all their drinking occasions, including 2.7% who consumed this quantity weekly or more often. Another 2.8% drank four drinks weekly or more often but usually consumed smaller quantities. Among women, 9.3% drank three drinks on all of their drinking occasions, including 2.0% who did so at least once a week. Another 1.1% drank three drinks once a week or more but usually drank two drinks or less.
Discussion
The gray area of consumption between the old and proposed new DGA was associated with small but significantly increased risks of prevalent and incident alcohol dependence, incident alcohol-related interpersonal problems, and prevalent job loss. Although the harm associated with this level of consumption reflected either a low absolute risk of harm (a prevalence of less than 1% for past-year dependence) or a low level of relative risk (odds less than doubled for any of the other significant associations), the large numbers of gray area drinkers resulted in increased levels of harm that were not negligible. For past-year alcohol dependence, which affected a total of nearly 7.7 million U.S. adults, the PAF of .028 reflected approximately 215,000 cases of alcohol dependence attributable to gray area consumption. Likewise, gray area consumption accounted for approximately 408,000 cases of job loss, 465,000 cases of incident alcohol dependence, and 199,000 cases of incident alcohol-related interpersonal problems.
However, the cross-sectional findings do not establish causality and should be interpreted with caution, especially given the lack of adjustment for outcome-specific potential confounders (e.g., occupation, industry, part-time/full-time status, and seniority for the analysis of job loss). Moreover, of the gray area drinkers who experienced incident alcohol dependence and interpersonal problems, 89% of the former and 94% of the latter had moved out of the gray area and into the highest-risk consumption group over the course of the follow-up interval (data not shown). That is, the overwhelming majority of their harm was associated with increased consumption and would not necessarily have occurred if gray area consumption patterns had been maintained. Moreover, gray area consumption was not associated with any significantly increased risk of prevalent or incident psychiatric disorders or medical conditions, the latter being the basis for most drinking guidelines.
What do the results of this study mean, both for the proposed 2010 DGA and, more broadly, for drinking guidelines in general and our understanding of the relationship between consumption and harm? The relatively minor levels of risk associated with gray area consumption support its being labeled a low-risk (or lower-risk) drinking pattern, but is it moderate? Whereas low-risk drinking limits imply a threshold below which the risk of alcohol-related harm is fairly minimal, they do not imply any benefit of drinking at these levels. In contrast, moderate drinking guidelines may connote recommended or implicitly beneficial drinking levels, especially when embedded in broad dietary guidelines that include recommended levels of consumption for many types of valuable nutrients. How, then, can the DGA avoid seeming to recommend levels of drinking that are not without risk?
One approach (applicable to future revisions of drinking guidelines even if the fate of the 2010 DGA is already decided by this printing) would be to state that one to two drinks per day for men and one drink per day for women represent levels of alcohol intake that can be consumed on even a daily basis with little risk of harm. In contrast, four drinks for men and three drinks for women could be described as daily limits above which the risks of alcohol-related harm are significantly increased, even if consumed only occasionally. This nuanced approach avoids giving the false impression of a single cut-point that divides safe and risky consumption, when in fact a continuum of risk exists. Such an approach was used in the recently revised Australian drinking guidelines, which provided one limit (two standard drinks) that could safely be consumed every day and still result in a lifetime risk of alcohol-related mortality of less than 1% and a second, higher limit (four standard drinks) for reducing the risk of injury on any single drinking occasion (http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/ds10-alcohol.pdf). Notably, and reflecting an ongoing area of controversy, the Australian limits were gender-neutral, as are those of a number of countries (http://www.icap.org/PolicyIs-sues/DrinkingGuidelines). Because of their smaller standard drink size (10 g ethanol vs. 14 g for the United States), the Australian limits reflect levels of ethanol intake that lie between the male and female U.S. limits in the proposed 2010 DGA.
Alternatively, the DGA could simply eschew the term “moderate drinking guidelines” and more accurately re-label the proposed limits as “low-risk drinking guidelines,” a term widely used in the guidelines for other countries, including those with relatively low absolute limits (http://www.icap.org/PolicyIssues/DrinkingGuidelines). At a time when researchers are increasingly questioning both the purported heart health benefits of moderate drinking (Chikritzhs et al., 2009; Fillmore et al., 2007; Friesma et al., 2008; Fuchs and Chambless, 2007) and whether these should be netted out from negative effects of moderate drinking on other types of alcohol-related harm (Rehm et al., 2008; http://www.nhmrc.gov.au/_files_nhmrc/file/publications/synopses/ds10-alcohol.pdf), this may be the most appealing option.
Unlike most of the studies informing drinking guidelines, which have examined health outcomes obtained through registry or death record information, this study is based on self-report of both outcomes and consumption. Any general tendency to withhold or disclose sensitive information may have increased levels of association relative to other study designs. The absolute levels of consumption are undoubtedly understated, as coverage rates for survey-based consumption estimates typically lie in the range of 40%-60%, even for surveys using consumption questions as extensive as those used in the NESARC (Kerr and Greenfield, 2007). These limitations imply that levels of risk associated with any given level of self-reported consumption reflect risks associated with a higher true level of intake. Thus, it is unlikely that this study would have underestimated the effects of gray area consumption.
A final limitation of this study was the relatively brief 3-year follow-up interval, which may have been too short to yield associations with medical conditions. Notably, the outcomes positively associated with gray area consumption in this study were related to alcohol use disorders and social problems, consequences largely ignored in the rationale for most drinking guidelines. In future revisions, consideration should be given to including a broader array of harms, including mental health outcomes, social harms, and harm to others. These reflect legitimate consequences of alcohol use that may be increased at levels of consumption lower than those associated with physical health outcomes. In addition, guidelines would benefit from including information on how to minimize the impact of drinking by pacing drinks, drinking with meals, and so forth.
Footnotes
The study on which this article is based, the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), is sponsored by the National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institutes of Health, U.S. Department of Health and Human Services, with supplemental support from the National Institute on Drug Abuse. This research was supported, in part, by the Intramural Program of the National Institutes of Health, NIAAA. The views and opinions expressed in this article are those of the authors and should not be construed to represent the views of any of the sponsoring organizations, agencies, or the U.S. government.
References
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: Author; 1994. [Google Scholar]
- Chikritzhs T, Fillmore K, Stockwell T. A healthy dose of scepticism: Four good reasons to think again about protective effects of alcohol on coronary heart disease. Drug and Alcohol Review. 2009;28:441–444. doi: 10.1111/j.1465-3362.2009.00052.x. [DOI] [PubMed] [Google Scholar]
- Fillmore KM, Stockwell T, Chikritzhs T, Bostrom A, Kerr W. Moderate alcohol use and reduced mortality risk: Systematic error in prospective studies and new hypotheses. Annals of Epidemiology. 2007;17:S16–S23. doi: 10.1016/j.annepidem.2007.01.005. [DOI] [PubMed] [Google Scholar]
- Friesema IHM, Zwietering PJ, Veenstra MY, Knottnerus JA, Gar-retsen HF, Kester ADM, Lemmens PHH. The effect of alcohol intake on cardiovascular disease and mortality disappeared after taking lifetime drinking and covariates into account. Alcoholism: Clinical and Experimental Research. 2008;32:645–651. doi: 10.1111/j.1530-0277.2007.00612.x. [DOI] [PubMed] [Google Scholar]
- Fuchs FD, Chambless LE. Is the cardioprotective effect of alcohol real? Alcohol. 2007;41:399–402. doi: 10.1016/j.alcohol.2007.05.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering RP. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): Reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003b;71:7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Grant BF, Kaplan K, Shepard J, Moore T. Source and accuracy statement for wave 1 of the 2001—2002 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003a. [Google Scholar]
- Grant BF, Kaplan K, Stinson FS. Source and accuracy statement: The 2004—2005 wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2007. [Google Scholar]
- Hanley JA. A heuristic approach to the formulas for population attributable fraction. Journal of Epidemiology and Community Health. 2001;55:508–514. doi: 10.1136/jech.55.7.508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kerr WC, Greenfield TK. Distribution of alcohol con-sumption and expenditures and the impact of improved measure-ment on coverage of alcohol sales in the 2000 National Alcohol Survey. Alcoholism: Clinical and Experimental Research. 2007;31:1714–1722. doi: 10.1111/j.1530-0277.2007.00467.x. [DOI] [PubMed] [Google Scholar]
- Rehm J, Room R, Taylor B. Method for moderation: Measuring lifetime risk of alcohol-attributable mortality as a basis for drinking guidelines. International Journal ofMethods in Psychiatric Research. 2008;17:141–151. doi: 10.1002/mpr.259. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Research Triangle Institute. SUDAAN Language Manual. Release 10.0. Research Triangle Park, NC: Research Triangle Institute; 2008. [Google Scholar]
- Zhang J, Yu KF. What's the relative risk? A method of correct-ing the odds ratio in cohort studies of common outcomes. Journal of the American Medical Association. 1998;280:1690–1691. doi: 10.1001/jama.280.19.1690. [DOI] [PubMed] [Google Scholar]


