Abstract
Staging of rectal cancer is essential to help guide clinicians to decide upon the correct type of surgery and determine whether or not neoadjuvant therapy is indicated. Magnetic resonance imaging (MRI) is currently one of the most accurate modalities on which to base treatment decisions for patients with rectal cancer. MRI can accurately detect the mesorectal fascia, assess the invasion of the mesorectum or surrounding organs and predict the circumferential resection margin. Although nodal disease remains a difficult radiological diagnosis, new lymphographic agents and diffusion weighted imaging may allow identification of metastatic nodes by criteria other then size. In light of this, we have reviewed the literature on the accuracy of specific MRI findings for staging the local extent of primary rectal cancer. The aim of this review is to establish a correlation between MRI findings, prognosis, and available treatment options.
Keywords: Magnetic resonance imaging, Preoperative staging, Prognostic factors, Rectal cancer
INTRODUCTION
In 2010, an estimated 142 570 people were diagnosed with colorectal cancer in the United States, including 39 670 with rectal cancer[1]. In contrast to colon cancer, local recurrences in rectal cancer, which occur in up to 50% of patients with T3 or node positive lesions, have been a significant cause of morbidity[2]. In order to decrease rates of local recurrence, adjuvant treatment, such as radiotherapy with or without chemotherapy, is generally recommended for patients with T3 or higher and/or N+ rectal cancers[3]. Preoperative radiotherapy and chemo-radiotherapy are now preferred to postoperative because they are much better tolerated, thereby increasing treatment compliance. They also result in lower local recurrence rates[4]. However, even if given preoperatively, pelvic radiotherapy can result in deterioration of anal continence and sexual function as well as worsen the quality of life[5]. Importantly, according to data from recent chemoradiotherapy (CRT) trials, 18%-30% of enrolled patients are over-staged and therefore receive unnecessary and potentially harmful therapy[6]. Thus, accurate staging of this disease is essential to spare patients from potentially toxic over-treatment.
The most common pre-operative staging modalities for rectal cancer include endorectal ultrasonography (EUS), computed tomography (CT) and magnetic resonance imaging (MRI). In two large retrospective studies on rectal cancer patients, over a period of 10 years, the overall accuracy of T and N staging by EUS was shown to be only 69% and 68% respectively[7,8]. Compared to EUS, CT has an even lower accuracy for determining the depth of tumor invasion[9]. In contrast, high definition MRI with phased-array coils has been shown to be more reliable than EUS in staging advanced (stage ≥ II) rectal cancer[10]. In fact, MRI has been shown to provide important information about the depth of tumor infiltration within the bowel wall, the relationship between the tumor and mesorectal fascia, and the presence of lymph node and extramural vascular invasion. Information determined from MRI can help guide clinicians to decide upon the correct type of surgery, determine whether or not neoadjuvant therapy, such as chemo-radiation, is indicated, and predict patients’ prognosis. This information can be used to maximize the chance of complete oncological resection, improve survival and the quality of life, and minimize morbidity. The aim of this review is to establish a correlation between MRI findings, prognosis, and available treatment options.
MR IMAGING PROTOCOLS
The introduction of phased-array coils has been a major advance in imaging of rectal cancer allowing high spatial resolution, a large field of coverage[10], and visualization of structures 1-2 mm in diameter[11]. Ideally, for rectal MRI, the field of view should be small (i.e. less than 200 mm), the matrix (resolution in 2D) at least 256 × 256 pixels, and the slices 3 mm or less in thickness.
In the most current MRI protocol (Table 1), the tumor is first localized with low-resolution axial and sagittal images of the entire pelvis. The field of view is then restricted to the area of the cancer and high-resolution T2 weighted images are obtained perpendicular to the cranio-caudal axis of the rectum at the level of the tumor (Figure 1A). True axial (i.e. perpendicular) images of the tumor are critical because they reduce the overestimation of the tumor depth of invasion noted upon oblique imaging[12]. Coronal images (parallel to the anus) are important in identifying the relationship of low rectal tumors to the internal sphincter as well as the external sphincter/levators complex[13] (Figure 1B). T2-weighted sagittal images are often necessary to determine the relationship of the tumor to the peritoneal reflection (Figure 1C)[14]. In some cases, axial diffusion weighted imaging (DWI) may be performed to help in the localization of small tumors[15] (Figure 2).
Table 1.
Optimal rectal MRI protocol
| Sequence | Area | Plane | Purpose |
| 1-Low resolution T2 ± T1 | Whole pelvis | Axial | Overview of the pelvis and tumor localization |
| 2-High resolution T2 | Rectum | Sagittal | Determination of cranio-caudal extension of the tumor, peritoneal reflection and distance from the anal canal |
| 3-High resolution T2 | Whole mesorectum | Axial to the tumor | Assessment of the mesorectum and of the CRM |
| 4-High resolution T2 | Rectum | Coronal based on the anal canal plane | Assess relation to the sphincter-levator complex |
CRM: Circumferential resection margin.
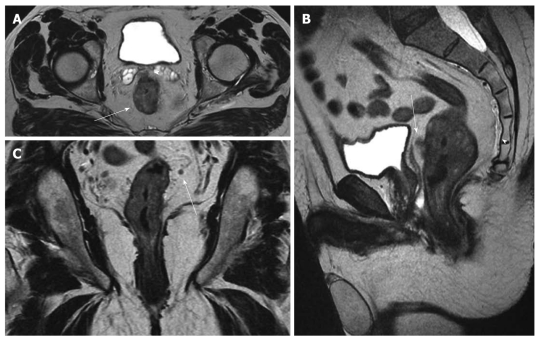
Figure 1.
Magnetic resonance imaging staging of rectal cancer before chemoradiation: T3, N+. Pathology result: T3, N1. A: Axial T2w image shows the circumferential tumor (arrow) and the extramural spread anteriorly (arrowhead) close to the seminal vesicles; B: In the sagittal T2w image, the anterior extramural spread (arrow) can be also recognized close to the mesorectal fascia (thin vertical hypointense line posterior to the bladder). The presacral fascia can also be appreciated (arrowhead) continuing inferiorly as the rectosacral fascia; C: In the coronal T2w image, a small mesorectal lymph node (arrow) is seen.
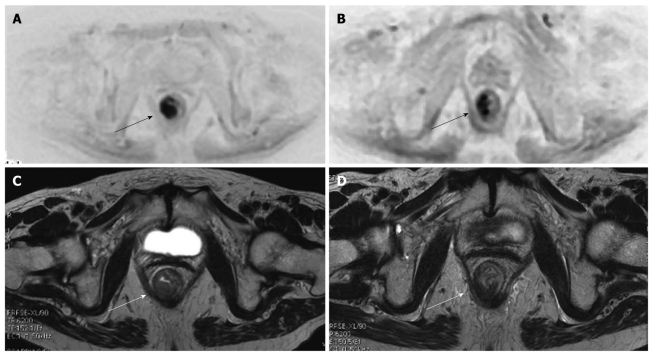
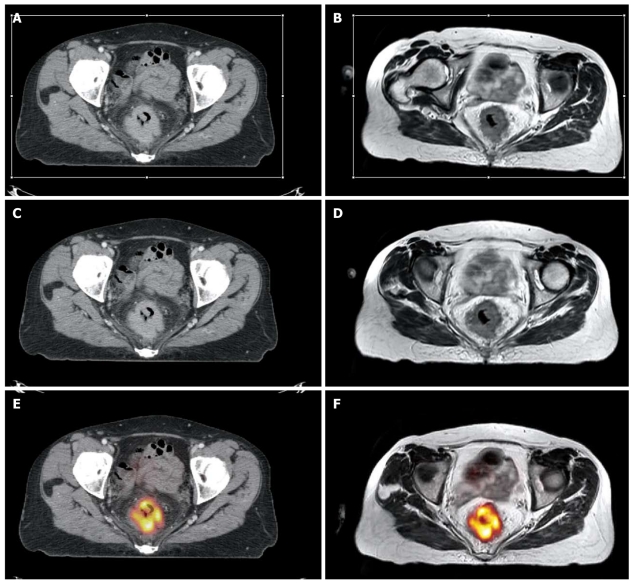
Figure 2.
Diffuse weighted imaging and cancer (arrows) of the lower rectum. At initial MR staging T3N1. After neoadjuvant therapy, MR restage was T3N0. At pathology: T3N1 (only one small metastatic mesorectal lymph node). Diffusion weighted imaging (DWI) (A) and axial T2w (B) images show the tumor (arrows) before chemoradiotherapy. The DWI image allows for better recognition of the lesion. DWI (C) and axial T2w (D) images after chemoradiotherapy show a reduction in the dimensions of the lesion (arrows).
The importance of the imaging protocol for assessment of advanced rectal tumors has recently been reported. Suzuki and associates demonstrated that by including the imaging parameters listed in sequence 2 and 3 (Table 1), the sensitivity and specificity of assessing invasion of anterior organs was 80% and 95% respectively, compared to only 50% and 33% with protocols that employed different imaging parameters[16].
Improving MR image quality can be facilitated with the use of rectal cleaning to limit misinterpretation due to stool residue. Distension of the rectum by air insufflation, gel enema, or intravenous administration of spasmolytic medication also improves evaluation of the rectal wall layers.
MRI FINDINGS IN RECTAL CANCER
In T2 weighted images, rectal cancers typically have a signal-intensity intermediate between that of the perirectal fat, which is bright, and the muscularis propria, which is pitch black. The signal intensity is increased if the tumors contain mucin, but a low signal intensity similar to that of the muscle layer usually indicates a marked desmoplastic reaction of the tumor[17].
The anatomy relevant to rectal cancer imaging is also well visualized in T2 weighted images (Figure 1). The mucosa has a hypointense signal, the submucosa a hyperintense signal, the muscularis propria a hypointense signal, and the mesorectal fat a highly hyperintense signal. The mesorectal fascia can be identified as a thin, low-signal intensity structure that envelopes the mesorectum. However, due to a diminishing thickness of mesorectal fat, the mesorectal fascia is typically better visualized in the upper and middle third as well as the posterior portions of the rectum than the lower third and anterior portions[9]. The presacral fascia is also a thin hypointense layer in T2 weighted images. It covers the pelvic walls and the sacrum and joins with the mesorectum at the level of S4/S5 to form the rectosacral fascia, also known as the Waldayer’s fascia (Figure 1B).
Non-enhanced T1 weighted images have limited value in distinguishing the tumor from the layers of the bowel wall[14]. However, after intravenous injection of paramagnetic contrast, the smooth muscle of the internal sphincter brightly enhances, which can sometimes be useful in studying the relationship of the tumor with the sphincter complex[18].
PROGNOSTIC FACTORS ASSESSED BY MRI
The prognostic factors of rectal cancer that significantly influence the management strategy, the type of resection, tumor resectability, and candidacy for neo-adjuvant therapy, depend on the information obtained from pre-operative MRI, including depth of tumor infiltration within the bowel wall, involvement of neighboring pelvic organs and/or the peritoneum (T stage), the circumferential resection margin (CRM), the presence of local lymph node metastases (N stage), extramural vascular invasion, and the extent of extramural tumor spread in mm.
T staging
The depth of invasion through the muscle wall is one important element seen on MRI that can help guide clinical decision making for patients with rectal cancer. Not only does the incidence of nodal involvement increase with increasing tumor penetration[19,20], but clinical studies have shown that patients with stage I (T1-2 N0) rectal cancer do not benefit from neo-adjuvant radiotherapy[21] and may be amenable to a less than radical surgical treatment[22]. Patients with clinically staged T3-4 tumors typically require preoperative CRT since it reduces the rates of local recurrence more effectively than either postoperative CRT or preoperative radiotherapy alone[23-25]. However, some problems remain with T stage determination on MR imaging. Overall, the agreement between MRI and histology for T staging has ranged from 66%-94%[18,26-28]. One of the main problems of T staging on MRI is the distinction between T2 and T3 tumors. In fact, investigators have shown that the negative predictive value for invasion beyond the muscularis propria varied from 93% (expert reading) to 76% (general radiologist reading)[26]. This difficulty is attributed to the presence of desmoplastic reactions around the tumor. This reaction makes it difficult to distinguish between spiculation in the perirectal fat caused by fibrosis alone from that caused by fibrous tissue that contains tumor cells[26]. In contrast, MRI has been shown to be more accurate in imaging the more advanced tumors (T4)[27,29]. According to a meta-analysis, MRI for T4 lesions has a specificity of 96%[30].
CRM
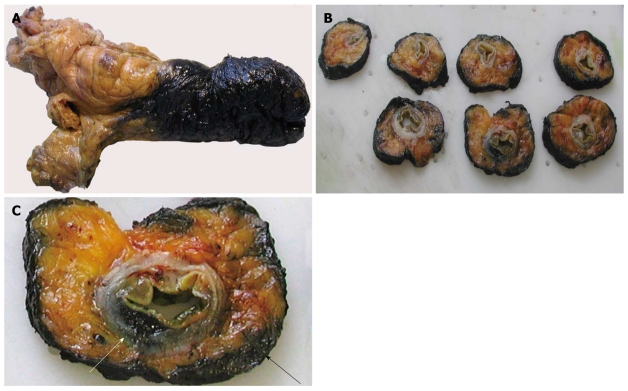
The CRM (lateral, radial) is defined as the surgical cut surface of the connective tissues (i.e. lymphovascular, fatty and neural tissue) that circumferentially encase the rectum. It equates to the mesorectal fascia that forms the plane of dissection in rectal cancer surgery. It is assessed by marking the outer surface (i.e. the CRM) with ink, taking serial cuts through the specimen and examining the macroscopic and microscopic relations between the tumor and the inked margin (Figure 3A-C). The CRM gives significant information not only about the quality of the performed operation but also prognosis of the disease. Indeed, in a recent study based on the data from a randomized clinical trial, Nagtegaal et al[31] demonstrated in a multivariate model that the CRM is more important than the T stage for the prognosis of rectal cancer. The definition of a positive CRM remains a matter of debate. A review of the literature in 2006 showed that the majority of studies that dealt with CRM status used the ≤ 1 mm definition for positive CRM (91.1%; 7373 of 8094 patients)[32].
Figure 3.
Pathological evaluation of the circumferential resection margin (CRM). A: The excised rectum is dipped in ink; B: Serial sections including the tumor are taken through the entire rectum; C: One of the sections shows the tumor’s leading edge (white arrow) and its relation with the CRM (black arrow).
Six distinct types of CRM involvement have been described; direct tumor spread which occurs in 18% to 29% of cases; discontinuous tumor spread in 14% to 67% of cases; lymph node metastases in 12% to 14% of cases; venous invasion in 14% to 57% of cases; lymphatic invasion in 9% of cases; and perineural tumor spread in 7% to 14% of cases[32]. In approximately 30% of patients, there is more than one type of margin involvement. In contrast to direct tumor spread, the involvement of the CRM by lymph node metastases is not associated with local recurrence[32].
MRI is highly accurate and reliable for prediction of the CRM[33,34]. In their most recent study of 98 rectal cancer patients, Brown et al[27] reported a 92% agreement between MRI images and histologic findings for prediction of CRM involvement. In another study assessing the tumor relationship to the mesorectal fascia, two observers independently scored the tumor stage and the distance to the mesorectal fascia on MRI and compared these observations with the final histological findings[26]. For twelve tumors with involved mesorectal fascia, and thus, a CRM of 0 mm, the accuracy in predicting the CRM was 100% for both readers. In 29 patients with a wide CRM (10 mm), the accuracy for predicting the negative margin was 97% (27 of 28) for one reader and 93% (26 of 28) for the other[26].
It is relevant to point out that 5 mm of mesorectal tissue surrounding the lateral tumor edge on MRI was shown to equal a CRM of 2 mm in the surgical specimen[26]. In the report by Nagtegaal et al[35], a linear regression curve showed that the crucial distance of at least 2 mm could be predicted with 97% confidence when the distance on MRI is at least 6 mm. Therefore, the safe rule to predict CRM involvement on MRI is considered to be an MRI measurement minus 4 mm due to shrinkage of the specimen with fixation[6]. Of note, the CRM becomes more difficult to identify in low, anterior tumors and in patients with a limited amount of perirectal fat[36].
In a recent study by Frasson et al[37], the 5-year local recurrence rates for patients with a preoperative CRM of < 2 mm on MRI or EUS who did not receive preoperative chemoradiation was 19.4% compared to 5.4% for patients with a non threatened margin. It is important to realize that a short course of preoperative radiotherapy has limited ability to control positive CRM. An analysis of more than 17 500 pathologic specimens by Nagtegaal et al[32] revealed that the chance of local recurrence was higher for patients with a positive CRM after neoadjuvant treatment (both radiotherapy and radiochemotherapy) than those with a positive CRM following immediate surgery (Hazard ratio 6.3 vs 2.0, respectively). Similar results have been reported following postoperative treatment[38]. In the MRC CR-07 trial, patients with positive radial margins who were selected to receive postoperative chemoradiation had a 21% local recurrence rate[39]. Thus, in cases where the tumors are close (< 2 mm) or through the mesorectal margin on preoperative MRI, a more aggressive treatment regimen is required with neoadjuvant CRT or an upfront regimen of chemotherapy before chemoradiation prior to operation. In contrast, patients with a free margin > 2 mm from mesorectal fascia may undergo surgery [total mesorectal excision (TME)] alone, avoiding preoperative chemoradiation.
Interestingly, MRI-based therapy for CRM positive tumors was able to reduce the frequency of neoadjuvant therapy for rectal carcinoma by 35% without the risk of worsening the oncological results[40]. However, omitting preoperative chemoradiation for all CRM-negative tumors on MRI needs to be further investigated in prospective clinical trials before it is adopted as standard therapy.
N staging
The presence of involved lymph nodes is an indicator for the likelihood of systemic disease and local recurrence[41]. Therefore node-positive disease is generally an indication for preoperative chemoradiation. However, radiological evaluation of lymph node metastatic involvement remains a challenge.
Results of anatomic studies show that over half of the metastatic nodes from rectal cancer are within 3 cm of the primary tumor and are smaller than 5 mm in size[42]. With a standard TME, the perirectal nodes are removed with the primary tumor, but the internal iliac and obturator nodes are left in place. Moriya et al[43] reported that as many as 28% of lymph node-positive distal rectal cancers have involvement of lateral nodes and in 6% of cases, these were the only nodes involved. This means that in 6% of patients, the disease was incorrectly staged post-operatively as node-negative at TME.
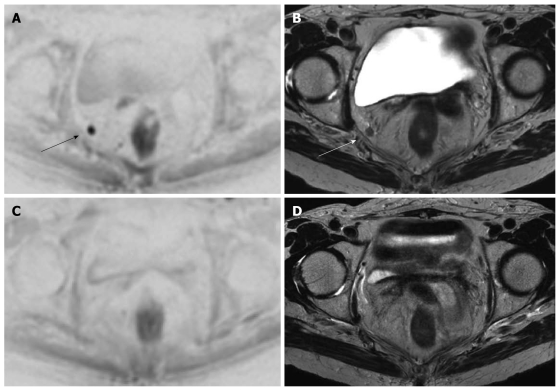
For pre-operative lymph node imaging, MRI at present is only moderately accurate, although this could change with advances in new MR techniques. Currently, the reported accuracy rate of MRI for nodal staging ranges from 71% to 91%[42]. On MRI, lymph nodes typically have lower signal intensity than the perirectal fat but higher signal intensity than arteries and veins (Figure 4). In patients with mucinous carcinoma, metastatic lymph nodes are visualized as hyperintense nodules alone or as hyperintense areas within hypointense nodules. A node is considered enlarged if the major axis length is more than 5 mm (mesorectal), 7 mm (internal iliac), 10 mm (external iliac), or 9 mm (common iliac)[44]. However, the morphological features or signal intensity of the nodes on MRI may more accurately determine metastatic involvement rather than measurement of size. Brown et al[45] demonstrated that an irregular border or mixed signal intensity of lymph nodes on MRI improved the specificity of predicting nodal status from 68% (based on size alone) to 97%.
Figure 4.
Same case as Figure 2. An enlarged right obturator lymph node is suspected in this patient with a lower third rectal cancer. Diffusion weighted imaging (DWI) (A) and axial T2w (B) images show the enlarged obturator lymph node nicely (arrows). DWI (C) and axial T2w (D) images following chemoradiotherapy show that the lymph node has disappeared
One of the more promising advances of MRI may be the use of new lymphographic agents that help assess tumor spread to lymph nodes. In a recent study, gadofosveset-enhanced MRI improved the specificity of nodal staging from 82% achieved with standard MRI to 97%[46]. Fusion of diffusion-weighted MR with T2-weighted images improves identification of pelvic lymph nodes compared with T2-weighted images alone. Using fusion images, 29% additional nodes were detected compared with T2-weighted images alone[47]. The improved nodal identification may aid in treatment planning.
Extramural vascular invasion
Venous invasion is defined as the presence of tumor tissue within an endothelium lined space, either surrounded by a rim of smooth muscle or containing red blood cells. Talbot et al[48] showed that extramural venous invasion was present in 52% of rectal cancer specimens examined. Of these, the specimens showing invasion in thick-walled veins were significantly associated with distant metastases and death from tumor recurrence.
On MRI, using contiguous 3-mm slices, the presence of tumor signal intensity within a vascular structure is highly suggestive of extramural vascular invasion[49]. Typically, on T2-weighted images, the tumor signal intensity is intermediate (gray) while the veins are serpiginous or tortuous linear structures beyond the muscle coat[49]. Larger vessels are typically in a consistent anatomic position and appear black owing to signal void. As tumor invades along the vessel lumen, the vessel expands and ultimately the tumor may disrupt the vessel border, making the vessel border appear irregular or nodular[49]. Brown et al[50] found that MRI correctly identified 15 of the 26 rectal cancer patients that had extramural venous invasion documented histologically. In the remaining cases, the subtle microscopic extramural venous invasion could not be resolved on MRI.
Using four criteria (tumor margin, tumor location relative to vessels, vessel size, and vessel border), a 5-point grading system for the MRI-based preoperative assessment of extramural vascular invasion has been proposed[51]. Initial data suggests it that has been shown to correlate with clinical outcome. On univariable analysis, relapse-free survival at 3 years was 35% for patients with an extramural vascular invasion score on MRI of 3 to 4, compared with 74% for those with a score of 0 to 2 (P < 0.001). Interesting, these scores are similar to relapse-free survival rates noted in patients with histologically positive and negative extramural vascular invasion, respectively (34% vs 73.7%, P < 0.001). Therefore, the stratification of patients into prognostic groups according to MRI extramural vascular invasion score appears to be clinically accurate for assessing the need for preoperative treatment of patients at high risk.
Extramural spread
Depth of extramural tumor spread is defined as the measured distance of the tumor beyond the outer longitudinal muscle coat. MRI provides valuable information regarding extramural tumor spread[12], except when the tumors are circumferential or have little peri-rectal fat[36].
Pathologists have long recognized that with increasing depth of spread there is an increasing incidence of nodal involvement and extramural vascular invasion[52,53]. Moreover, patients with T3 rectal cancers extending less than 5 mm into the perirectal fat have a significantly better 5-year cancer-related survival rate than do patients with pT3 tumors extending more than 5 mm beyond the rectal wall (85% vs 54%, respectively)[52-54]. Based on these observations, neo-adjuvant therapy has not been routinely recommended for patients with pT3 carcinomas invading minimally (< 5 mm) into the perirectal tissue; instead patients should undergo immediate surgery.
However, the use of < 5 mm as the determinant for the therapeutic decision is controversial and should be used with caution when determining treatment options for patients. Merkel et al[54] reported that tumors with less than 5 mm extramural spread may still have a 38%-43% rate of nodal metastasis. Moreover, if very advanced tumors and those with positive margins are excluded this prognostic factor no longer correlates with survival[55].
RE-STAGING AFTER CRT
Because of the increasing use of preoperative CRT, MRI is frequently repeated after treatment to re-stage the tumor, assess the response, determine whether it is operable, and establish the extent of surgical resection. However, early studies have questioned the accuracy of MRI in the post-CRT setting with a T-stage correlation of only 47%-54% and an N stage correlation of 64%-68%[46,56-59]. In the study by Kulkarni et al[60], MRI performed 6 wk post CRT overestimated the CRM involvement in 56% of cases, while T stages were over-staged in 38% and N stages in 4%. Over-staging was due to lack of discrimination between residual tumor and post-treatment changes, both appearing as a diffuse hypointense signal. Post-treatment changes are due to marked fibrosis of the bowel wall or to peritumoral infiltration of inflammatory cells and proliferating vessels as confirmed by other investigators[46,57].
Recently, improved accuracy of MRI in the post-CRT setting was achieved by lengthening the interval after CRT. In the study by Johnston et al[61], the radiological T-stage determined on MRI obtained 10-11 wk after CRT was the same as the pathological T-stage on the resected specimen in 14 out of 17 cases (88%) as compared to only a 59% agreement between the MRI and subsequent post-resection histopathology when the MRI was performed 6 wk after treatment. In this study, the pre-operative MRI showed ongoing response to CRT up to 12 wk after CRT, which has important clinical implications regarding the most appropriate time to operate.
Change in the surgical strategy may occur after CRT, especially for patients who seem to exhibit a complete tumor response. For this subset of patients, transanal excision or non-operative treatment in selected circumstances maybe considered with good prognosis[62]. However, predicting the nodal status for these patients using imaging techniques becomes crucial, since the nodes are not removed at local excision. Importantly, the assessment of tumor spread to lymph nodes may be improved with the use of a novel nanoparticle contrast medium (ultra-small superparamagnetic iron oxide; USPIO)[63,64]. In a recent prospective multicenter study, MRI performed after CRT for rectal cancer using USPIO was able to improve the negative predictive value of the nodal status to 95%[65]. Unfortunately, this product is not currently commercially available.
SPECIAL CONSIDERATION
Adenocarcinoma of the lower rectum
The lower third of the rectum (less than 5 cm from the anal verge) lies below the level of the peritoneal reflection. The majority of published series have shown that tumors arising in this anatomic location have the worst outcome, with local recurrence rates as high as 30%. This is due, in part, to the fact that compared to the tumors of the upper rectum, the surgical dissection for these low rectal tumors is less straightforward and is associated with a higher rate of perforation through the correct oncologic plane compared to the tumors of the upper rectum. Anatomically, the mesorectum thins out towards the lower third of the rectum and disappears at the level of the internal sphincter. There is less space for the tumor to traverse before it reaches the surgical plane of resection. Consequently, the CRM is more often positive in the surgical specimen for tumors located in the lower rectum, than for those located in the middle and upper rectum[32].
To overcome this shortcoming, a new operation, the “cylindrical” abdominoperineal resection (APR), has been pioneered in Europe[66,67]. In this operation, instead of following the mesorectum all the way to the levator muscles, the surgeon stops when the coccyx is visualized. The remaining dissection is performed from the perineum and is facilitated by the prone position. In the standard APR the perineal operator enters the levators anteriorly to the coccyx and the amount of levator muscle and ischiorectal fat removed around the tumor is not standardized. Instead in the cylindrical APR once the levators and the coccyx are encountered the coccyx is excised and the levators are followed laterally to their origin from the lateral pelvic sidewalls where they are transected. In the case of anterior tumors, the posterior vaginal wall and part of the prostate are also removed en bloc[66]. One disadvantage of the technique is that it leaves a very large pelvic gap that can not be primarily closed and therefore a muscle flap reconstruction with the gracilis, the rectus abdominis or the gluteus maximus is often required[66]. Comparing 27 cylindrical to 99 conventional APRs, West et al[68] found a 70% increase in the amount of tissue removed around the tumor and no violation of the oncologic plane of dissection in the former group as well as a much lower rate of positive CRM 15% vs 40%, respectively. While many series advocate a wide perineal resection, and report low rates of local recurrence, these enhanced perineal resections have not become standard of care and prospective data are lacking[69]. Perineal wound infection, wound breakdown, and neurological dysfunctions are major problems for patients who receive radiation followed by abdominoperineal excision[69]. Primary closure with a flap overcomes some of these difficulties by bringing non-irradiated tissue into the perineal wound.
In a prospective study of 40 rectal tumors ≤ 5 cm from the dentate line from a single institution, MRI with intravenous contrast medium was universally successful in detecting invasion of the internal and external sphincters[70]. For low-lying rectal tumors that are restricted to the rectal wall or internal sphincter, spare the external sphincter and levator ani, and are not amenable to local excision as determined by preoperative MRI, there are several advantages to performing inter-sphincteric APR. While the standard APR removes the whole sphincter complex in this procedure the dissection is carried out in the inter-sphincteric plane, the external sphincter is left in place and the perineal defect is easily closed by approximating the external sphincter margins. This not only minimizes the problems with wound healing and postoperative pain but also reduces risk of damage to the erigentes nerves, hypogastric plexus, and the neurovascular bundles of Walsh (containing the cavernous nerves). Damage to these nerves causes both sexual and bladder dysfunction in men and women. Overall, this represents an anatomic and well-standardized dissection, which decreases the risk of rectal perforation and positive margins.
Among the sphincter-saving options, the inter-sphincteric TME, which removes only the upper half of the internal sphincter, has been recently found to be a valid option for selected tumors of the lower rectum[71]. The procedure is similar to a TME with a manual colo-anal anastomosis. In a TME with a manual colo-anal anstomosis the surgeon performs a mucosectomy above the dentate line leaving the internal sphincter intact. In the inter-sphincteric TME the surgeon cuts through the internal sphincter at the level of the dentate line, enters and dissects along the inter-sphinteric plane until establishing a connection with the abdominal operator. The proximal bowel is then manually anastomosed to the dentate line leaving the distal part of the internal sphincter intact. This allows one to achieve negative distal margins for tumors down to the ano-rectal junction while still providing good functional and oncologic results[71]. This procedure is indicated for T1-2 tumors that are well or moderately differentiated and for selected T3 tumors that have responded well to CRT.
For some tumors of the lower rectum, a trans-perineal approach overcomes the lack of exposure due to the angled pelvic anatomy and the rectum being surrounded by the levators[72]. In this approach the external sphincter and the perineal body is exposed through a transverse incision between the anus and the vagina or scrotum. This dissection allows the last 2-3 cm of rectum to be directly visualized.
These new procedures are not part of the standard surgical armamentarium and have to be planned in advance. MRI can offer the surgeon a road map to select the safest plane of dissection and plan the most appropriate procedure (Figure 5)[13].
Figure 5.
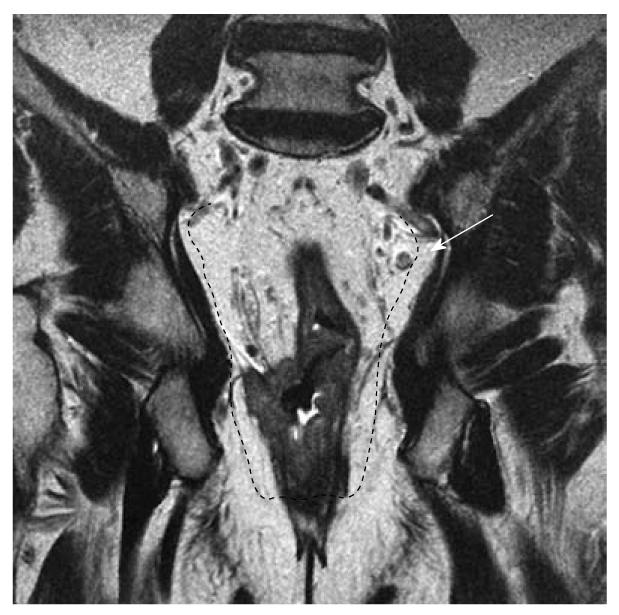
This case highlights the importance of the coronal plane in the assessment of the extension of the T4 lesion across the right levator complex into the right ischiorectal fossa, also shown (arrow) an enlarged and suspect lymph node. In this case, the surgeon may choose a modified APR resection (black dotted line).
Currently, the majority of tumors of the lower third of the rectum are irradiated preoperatively and MRI is not accurate for detecting residual microscopic sites of disease[57]. Thus, it is not advisable to make decisions about sphincter preservation based purely on MRI assessments of post-radiation tumor response. In this specific circumstance, EUS repeated after irradiation provided a 100% sensitivity but only a 53% positive predictive value for invasion of the sphincters[73].
Mucinous carcinomas
MRI in rectal carcinoma provides information on the mucinous status in addition to local tumor stage. The definition of mucinous carcinoma originates from histopathological examinations designating carcinomas with a mucin proportion of > 50% within the tumor volume[74]. Because of the high signal intensity in T2-weighted imaging, MRI can identify mucin pools in rectal carcinomas with a 97% accuracy and high inter-observer agreement[75]. Mucinous rectal tumors diagnosed at pre-therapeutic MRI have been associated with a noticeably worse response to chemoradiation as compared to that observed in non-mucinous carcinomas which allows an estimation of response before initiating neoadjuvant treatment[76,77].
NEW DEVELOPMENTS
There have been many advances in MRI techniques. The spatial resolution has improved, the speed of the examinations has been increased, DWI sequences have been used for body applications, and new contrast media have been developed. The newest 3 Tesla scanners provide excellent spatial resolution. High-resolution T2 sequences can be acquired in a shorter time[78] and isotropic (cubic) voxels can be acquired. In the near future, 3D T2 sequences with isotropic voxels will probably be available and the accurate positioning of imaging planes will no longer be an issue.
DWI is one of the most interesting developments of MR, allowing it to become an alternative to FDG-positron emission tomography (PET) in oncological imaging. DWI provides MR images with a signal intensity sensitized to the random motion of free water molecules[79,80]. In the rectum it is able to distinguish neoplastic from surrounding normal tissue (Figure 2). As such it may help in the detection of small tumors. However, the major challenge of MRI for rectal cancer is to reliably define the response to neoadjuvant therapy. Predicting a tumor’s response to treatment can be of considerable clinical benefit. Interestingly, preliminary results indicate that DWI might be effective in predicting treatment outcomes and for detecting the early tumor response[81-83]. In quantitative DWI, the magnetic resonance signal arises from both intracellular and extracellular compartments, and the result is given in terms of the apparent diffusion coefficient (ADC). Changes in the tumor ADC have been shown to correlate with the development of intra-tumoral fibrosis after chemoradiation[83], histologically proven apoptotic cell death[84] and regression in tumor size after chemotherapy and chemoradiation[81]. Other authors have supported the use of ADC values in combination with other MR imaging criteria in improving the discrimination between malignant and benign lymph nodes even after chemoradiation[46,63,85] (Figure 4). The main limitation to DWI imaging today is the variability in ADC values that are obtained with different magnets and imaging protocols. Further studies will be necessary to prove the possible value of DWI on predicting therapy outcome.
There are also alternative imaging techniques. CT has so far had a limited role in the local staging of rectal cancer. Today, perfusion imaging represents one of the most interesting fields of CT development. Perfusion imaging of large volumes is possible with multi-detector CT scanners. This technique has shown promise in predicting the response to neoadjuvant treatment[86]. CT perfusion data cannot currently be obtained with dynamic contrast-enhanced MR[87] and this represents a strong point in favor of CT.
PET and CT-PET scans are used mainly in the assessment of metastatic rectal cancer and local recurrence. Sequential determination of fluorodeoxyglucose uptake on PET/CT has proved useful in differentiating responsive from nonresponsive tumors during and at the end of neoadjuvant therapy[88]. However, radionuclide techniques have limitations, such as low spatial resolution and high cost. Large studies are needed to establish the most effective morphologic and functional imaging modalities for post-neoadjuvant therapy restaging of rectal cancer[86].
Over the last several years many strategies have been developed to overcome the limitations of radiotherapy planning using noncontrast-enhanced CT. Radiotherapy guided by MRI is possible using strategies that allow fusion and/or co-registration of MR images with those from other imaging techniques[88]. PET-CT, contrast enhanced CT, and non contrast enhanced CT and MR images can all be fused together to improve the assessment of rectal lesions and radiotherapy planning[89-91] (Figure 6). However, PET-guided radiotherapy has not yet provided a clear advantage. Better delineation of pelvic anatomy and pathology will become progressively more important as radiotherapy protocols are developed that include a boost on the gross tumor volume with documented improvement in patient outcome[92].
Figure 6.
Multimodal image registration can be performed to improve staging and radiotherapy planning of rectal cancer. Axial contrast enhanced computed tomography (CT) at the portal phase (A) and rigid registration of the axial T2w magnetic resonance (MR) image (B). Rigid registration reduces the misalignment between the anatomical structures in the two modalities. A, B: Volume selection (rectangular white thin line) for non-rigid registration is performed; C, D: Non-rigid registration compensates for the more complex deformations due to the different acquisition setting; E, F: Following non rigid registration, MR can be fused with the positron emission tomography (PET) image (F) and the result is super-imposable on the PET-CT image (E).
CONCLUSION
Rectal cancer is a global disease associated with poor outcomes if not properly staged and treated. The increased use of preoperative chemoradiation and refinement of surgical techniques have led to a greater proportion of patients being considered for curative resection. New surgical options exist for these patients in the form of sphincter saving resection or transanal excision in selected circumstances. For the vast majority of rectal carcinomas, MRI is currently the most accurate modality on which to base treatment decisions for patients with rectal cancer. Traditionally, the decision to apply preoperative treatment for rectal cancer patients has been based on the T- and N-stage. Lately, other MRI findings such as the radial distance of the tumor to the CRM and extramural vascular invasion score have been identified as important risk factors for local failure and survival. We strongly believe that every center that treats patients with rectal cancer should develop a multidisciplinary team featuring a description of the MRI findings and their implementation in the treatment strategy with the aim of increasing resectability, reducing the local recurrence and treatment morbidity, and improving the quality of life.
Footnotes
Peer reviewer: Chan Kyo Kim, MD, Assistant Professor, Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, 50 Ilwon-dong, Kangnam-gu, Seoul 135-710, South Korea
S- Editor Cheng JX L- Editor O’Neill M E- Editor Zheng XM
References
- 1.Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300. doi: 10.3322/caac.20073. [DOI] [PubMed] [Google Scholar]
- 2.Rich T, Gunderson LL, Lew R, Galdibini JJ, Cohen AM, Donaldson G. Patterns of recurrence of rectal cancer after potentially curative surgery. Cancer. 1983;52:1317–1329. doi: 10.1002/1097-0142(19831001)52:7<1317::aid-cncr2820520731>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 3.NCCN clinical practice guidelines in Oncology. accessed on October 13, 2010. Available from: http://www.nccn.org/professionals/physician_gls/f_guidelines.asp.
- 4.Valentini V, Aristei C, Glimelius B, Minsky BD, Beets-Tan R, Borras JM, Haustermans K, Maingon P, Overgaard J, Pahlman L, et al. Multidisciplinary Rectal Cancer Management: 2nd European Rectal Cancer Consensus Conference (EURECA-CC2) Radiother Oncol. 2009;92:148–163. doi: 10.1016/j.radonc.2009.06.027. [DOI] [PubMed] [Google Scholar]
- 5.Kosaras B, Kirschner DA. Radial component of CNS myelin: junctional subunit structure and supramolecular assembly. J Neurocytol. 1990;19:187–199. doi: 10.1007/BF01217297. [DOI] [PubMed] [Google Scholar]
- 6.Bosset JF. Adjuvant treatment of rectal cancer: improving patient selection. Gastrointest Cancer Res. 2008;2:37–38. [PMC free article] [PubMed] [Google Scholar]
- 7.Garcia-Aguilar J, Pollack J, Lee SH, Hernandez de Anda E, Mellgren A, Wong WD, Finne CO, Rothenberger DA, Madoff RD. Accuracy of endorectal ultrasonography in preoperative staging of rectal tumors. Dis Colon Rectum. 2002;45:10–15. doi: 10.1007/s10350-004-6106-3. [DOI] [PubMed] [Google Scholar]
- 8.Kauer WK, Prantl L, Dittler HJ, Siewert JR. The value of endosonographic rectal carcinoma staging in routine diagnostics: a 10-year analysis. Surg Endosc. 2004;18:1075–1078. doi: 10.1007/s00464-003-9088-7. [DOI] [PubMed] [Google Scholar]
- 9.Ju H, Xu D, Li D, Chen G, Shao G. Comparison between endoluminal ultrasonography and spiral computerized tomography for the preoperative local staging of rectal carcinoma. Biosci Trends. 2009;3:73–76. [PubMed] [Google Scholar]
- 10.Gagliardi G, Bayar S, Smith R, Salem RR. Preoperative staging of rectal cancer using magnetic resonance imaging with external phase-arrayed coils. Arch Surg. 2002;137:447–451. doi: 10.1001/archsurg.137.4.447. [DOI] [PubMed] [Google Scholar]
- 11.Ginsberg GG, Lewis JH, Gallagher JE, Fleischer DE, al-Kawas FH, Nguyen CC, Mundt DJ, Benjamin SB. Diazepam versus midazolam for colonoscopy: a prospective evaluation of predicted versus actual dosing requirements. Gastrointest Endosc. 1992;38:651–656. doi: 10.1016/s0016-5107(92)70559-8. [DOI] [PubMed] [Google Scholar]
- 12.Brown G, Richards CJ, Newcombe RG, Dallimore NS, Radcliffe AG, Carey DP, Bourne MW, Williams GT. Rectal carcinoma: thin-section MR imaging for staging in 28 patients. Radiology. 1999;211:215–222. doi: 10.1148/radiology.211.1.r99ap35215. [DOI] [PubMed] [Google Scholar]
- 13.Shihab OC, Heald RJ, Rullier E, Brown G, Holm T, Quirke P, Moran BJ. Defining the surgical planes on MRI improves surgery for cancer of the low rectum. Lancet Oncol. 2009;10:1207–1211. doi: 10.1016/S1470-2045(09)70084-1. [DOI] [PubMed] [Google Scholar]
- 14.Brown G, Daniels IR, Richardson C, Revell P, Peppercorn D, Bourne M. Techniques and trouble-shooting in high spatial resolution thin slice MRI for rectal cancer. Br J Radiol. 2005;78:245–251. doi: 10.1259/bjr/33540239. [DOI] [PubMed] [Google Scholar]
- 15.Soyer P, Lagadec M, Sirol M, Dray X, Duchat F, Vignaud A, Fargeaudou Y, Placé V, Gault V, Hamzi L, et al. Free-breathing diffusion-weighted single-shot echo-planar MR imaging using parallel imaging (GRAPPA 2) and high b value for the detection of primary rectal adenocarcinoma. Cancer Imaging. 2010;10:32–39. doi: 10.1102/1470-7330.2010.0011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Suzuki C, Torkzad MR, Tanaka S, Palmer G, Lindholm J, Holm T, Blomqvist L. The importance of rectal cancer MRI protocols on interpretation accuracy. World J Surg Oncol. 2008;6:89. doi: 10.1186/1477-7819-6-89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akasu T, Iinuma G, Takawa M, Yamamoto S, Muramatsu Y, Moriyama N. Accuracy of high-resolution magnetic resonance imaging in preoperative staging of rectal cancer. Ann Surg Oncol. 2009;16:2787–2794. doi: 10.1245/s10434-009-0613-3. [DOI] [PubMed] [Google Scholar]
- 18.Hoeffel C, Marra MD, Azizi L, Tran Van K, Crema MD, Lewin M, Arrivé L, Tubiana JM. [External phased-array MR imaging preoperative assessment of rectal cancer] J Radiol. 2006;87:1821–1830. doi: 10.1016/s0221-0363(06)74162-2. [DOI] [PubMed] [Google Scholar]
- 19.Mellgren A, Sirivongs P, Rothenberger DA, Madoff RD, García-Aguilar J. Is local excision adequate therapy for early rectal cancer? Dis Colon Rectum. 2000;43:1064–1071; discussion 1071-1074. doi: 10.1007/BF02236551. [DOI] [PubMed] [Google Scholar]
- 20.Bueno CG, de Barros JJ, Terres JS, Pereira DS Júnior. [Mandibular osteoradionecrosis. Clinical study and presentation of two cases] Quintessencia. 1978;5:55–73. [PubMed] [Google Scholar]
- 21.Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med. 1997;336:980–987. doi: 10.1056/NEJM199704033361402. [DOI] [PubMed] [Google Scholar]
- 22.Bailey HR, Huval WV, Max E, Smith KW, Butts DR, Zamora LF. Local excision of carcinoma of the rectum for cure. Surgery. 1992;111:555–561. [PubMed] [Google Scholar]
- 23.Sauer R, Becker H, Hohenberger W, Rödel C, Wittekind C, Fietkau R, Martus P, Tschmelitsch J, Hager E, Hess CF, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med. 2004;351:1731–1740. doi: 10.1056/NEJMoa040694. [DOI] [PubMed] [Google Scholar]
- 24.Bosset JF, Collette L, Calais G, Mineur L, Maingon P, Radosevic-Jelic L, Daban A, Bardet E, Beny A, Ollier JC. Chemotherapy with preoperative radiotherapy in rectal cancer. N Engl J Med. 2006;355:1114–1123. doi: 10.1056/NEJMoa060829. [DOI] [PubMed] [Google Scholar]
- 25.Gérard JP, Conroy T, Bonnetain F, Bouché O, Chapet O, Closon-Dejardin MT, Untereiner M, Leduc B, Francois E, Maurel J, et al. Preoperative radiotherapy with or without concurrent fluorouracil and leucovorin in T3-4 rectal cancers: results of FFCD 9203. J Clin Oncol. 2006;24:4620–4625. doi: 10.1200/JCO.2006.06.7629. [DOI] [PubMed] [Google Scholar]
- 26.Beets-Tan RG, Beets GL, Vliegen RF, Kessels AG, Van Boven H, De Bruine A, von Meyenfeldt MF, Baeten CG, van Engelshoven JM. Accuracy of magnetic resonance imaging in prediction of tumour-free resection margin in rectal cancer surgery. Lancet. 2001;357:497–504. doi: 10.1016/s0140-6736(00)04040-x. [DOI] [PubMed] [Google Scholar]
- 27.Brown G, Radcliffe AG, Newcombe RG, Dallimore NS, Bourne MW, Williams GT. Preoperative assessment of prognostic factors in rectal cancer using high-resolution magnetic resonance imaging. Br J Surg. 2003;90:355–364. doi: 10.1002/bjs.4034. [DOI] [PubMed] [Google Scholar]
- 28.Videhult P, Smedh K, Lundin P, Kraaz W. Magnetic resonance imaging for preoperative staging of rectal cancer in clinical practice: high accuracy in predicting circumferential margin with clinical benefit. Colorectal Dis. 2007;9:412–419. doi: 10.1111/j.1463-1318.2006.01167.x. [DOI] [PubMed] [Google Scholar]
- 29.Sebag-Montefiore D. Treatment of T4 tumours: the role of radiotherapy. Colorectal Dis. 2003;5:432–435. doi: 10.1046/j.1463-1318.2003.00522.x. [DOI] [PubMed] [Google Scholar]
- 30.Bipat S, Glas AS, Slors FJ, Zwinderman AH, Bossuyt PM, Stoker J. Rectal cancer: local staging and assessment of lymph node involvement with endoluminal US, CT, and MR imaging--a meta-analysis. Radiology. 2004;232:773–783. doi: 10.1148/radiol.2323031368. [DOI] [PubMed] [Google Scholar]
- 31.Nagtegaal ID, Gosens MJ, Marijnen CA, Rutten HJ, van de Velde CJ, van Krieken JH. Combinations of tumor and treatment parameters are more discriminative for prognosis than the present TNM system in rectal cancer. J Clin Oncol. 2007;25:1647–1650. doi: 10.1200/JCO.2005.05.4825. [DOI] [PubMed] [Google Scholar]
- 32.Nagtegaal ID, Quirke P. What is the role for the circumferential margin in the modern treatment of rectal cancer? J Clin Oncol. 2008;26:303–312. doi: 10.1200/JCO.2007.12.7027. [DOI] [PubMed] [Google Scholar]
- 33.Mulla M, Deb R, Singh R. MRI in T staging of rectal cancer: How effective is it? Indian J Radiol Imaging. 2010;20:118–121. doi: 10.4103/0971-3026.63055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wieder HA, Rosenberg R, Lordick F, Geinitz H, Beer A, Becker K, Woertler K, Dobritz M, Siewert JR, Rummeny EJ, et al. Rectal cancer: MR imaging before neoadjuvant chemotherapy and radiation therapy for prediction of tumor-free circumferential resection margins and long-term survival. Radiology. 2007;243:744–751. doi: 10.1148/radiol.2433060421. [DOI] [PubMed] [Google Scholar]
- 35.Nagtegaal ID, Marijnen CA, Kranenbarg EK, van de Velde CJ, van Krieken JH. Circumferential margin involvement is still an important predictor of local recurrence in rectal carcinoma: not one millimeter but two millimeters is the limit. Am J Surg Pathol. 2002;26:350–357. doi: 10.1097/00000478-200203000-00009. [DOI] [PubMed] [Google Scholar]
- 36.Kim YW, Cha SW, Pyo J, Kim NK, Min BS, Kim MJ, Kim H. Factors related to preoperative assessment of the circumferential resection margin and the extent of mesorectal invasion by magnetic resonance imaging in rectal cancer: a prospective comparison study. World J Surg. 2009;33:1952–1960. doi: 10.1007/s00268-009-0126-z. [DOI] [PubMed] [Google Scholar]
- 37.Frasson M, Garcia-Granero E, Roda D, Flor-Lorente B, Roselló S, Esclapez P, Faus C, Navarro S, Campos S, Cervantes A. Preoperative chemoradiation may not always be needed for patients with T3 and T2N+ rectal cancer. Cancer. 2011:Epub ahead of print. doi: 10.1002/cncr.25866. [DOI] [PubMed] [Google Scholar]
- 38.Baik SH, Kim NK, Lee YC, Kim H, Lee KY, Sohn SK, Cho CH. Prognostic significance of circumferential resection margin following total mesorectal excision and adjuvant chemoradiotherapy in patients with rectal cancer. Ann Surg Oncol. 2007;14:462–469. doi: 10.1245/s10434-006-9171-0. [DOI] [PubMed] [Google Scholar]
- 39.Sebag-Montefiore D, Stephens RJ, Steele R, Monson J, Grieve R, Khanna S, Quirke P, Couture J, de Metz C, Myint AS, et al. Preoperative radiotherapy versus selective postoperative chemoradiotherapy in patients with rectal cancer (MRC CR07 and NCIC-CTG C016): a multicentre, randomised trial. Lancet. 2009;373:811–820. doi: 10.1016/S0140-6736(09)60484-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Strassburg J, Junginger T, Trinh T, Püttcher O, Oberholzer K, Heald RJ, Hermanek P. Magnetic resonance imaging (MRI)-based indication for neoadjuvant treatment of rectal carcinoma and the surrogate endpoint CRM status. Int J Colorectal Dis. 2008;23:1099–1107. doi: 10.1007/s00384-008-0531-z. [DOI] [PubMed] [Google Scholar]
- 41.Kapiteijn E, Marijnen CA, Nagtegaal ID, Putter H, Steup WH, Wiggers T, Rutten HJ, Pahlman L, Glimelius B, van Krieken JH, et al. Preoperative radiotherapy combined with total mesorectal excision for resectable rectal cancer. N Engl J Med. 2001;345:638–646. doi: 10.1056/NEJMoa010580. [DOI] [PubMed] [Google Scholar]
- 42.Beets-Tan RG, Beets GL. Rectal cancer: review with emphasis on MR imaging. Radiology. 2004;232:335–346. doi: 10.1148/radiol.2322021326. [DOI] [PubMed] [Google Scholar]
- 43.Moriya Y, Sugihara K, Akasu T, Fujita S. Importance of extended lymphadenectomy with lateral node dissection for advanced lower rectal cancer. World J Surg. 1997;21:728–732. doi: 10.1007/s002689900298. [DOI] [PubMed] [Google Scholar]
- 44.Grubnic S, Vinnicombe SJ, Norman AR, Husband JE. MR evaluation of normal retroperitoneal and pelvic lymph nodes. Clin Radiol. 2002;57:193–200; discussion 201-204. doi: 10.1053/crad.2001.0893. [DOI] [PubMed] [Google Scholar]
- 45.Brown G, Richards CJ, Bourne MW, Newcombe RG, Radcliffe AG, Dallimore NS, Williams GT. Morphologic predictors of lymph node status in rectal cancer with use of high-spatial-resolution MR imaging with histopathologic comparison. Radiology. 2003;227:371–377. doi: 10.1148/radiol.2272011747. [DOI] [PubMed] [Google Scholar]
- 46.Lambregts DM, Beets GL, Maas M, Kessels AG, Bakers FC, Cappendijk VC, Engelen SM, Lahaye MJ, de Bruïne AP, Lammering G, et al. Accuracy of gadofosveset-enhanced MRI for nodal staging and restaging in rectal cancer. Ann Surg. 2011;253:539–545. doi: 10.1097/SLA.0b013e31820b01f1. [DOI] [PubMed] [Google Scholar]
- 47.Mir N, Sohaib SA, Collins D, Koh DM. Fusion of high b-value diffusion-weighted and T2-weighted MR images improves identification of lymph nodes in the pelvis. J Med Imaging Radiat Oncol. 2010;54:358–364. doi: 10.1111/j.1754-9485.2010.02182.x. [DOI] [PubMed] [Google Scholar]
- 48.Talbot IC, Ritchie S, Leighton MH, Hughes AO, Bussey HJ, Morson BC. The clinical significance of invasion of veins by rectal cancer. Br J Surg. 1980;67:439–442. doi: 10.1002/bjs.1800670619. [DOI] [PubMed] [Google Scholar]
- 49.Smith NJ, Shihab O, Arnaout A, Swift RI, Brown G. MRI for detection of extramural vascular invasion in rectal cancer. AJR Am J Roentgenol. 2008;191:1517–1522. doi: 10.2214/AJR.08.1298. [DOI] [PubMed] [Google Scholar]
- 50.Brown G, Daniels IR. Preoperative staging of rectal cancer: the MERCURY research project. Recent Results Cancer Res. 2005;165:58–74. doi: 10.1007/3-540-27449-9_8. [DOI] [PubMed] [Google Scholar]
- 51.Smith NJ, Barbachano Y, Norman AR, Swift RI, Abulafi AM, Brown G. Prognostic significance of magnetic resonance imaging-detected extramural vascular invasion in rectal cancer. Br J Surg. 2008;95:229–236. doi: 10.1002/bjs.5917. [DOI] [PubMed] [Google Scholar]
- 52.Dukes CE, Bussey HJ. The spread of rectal cancer and its effect on prognosis. Br J Cancer. 1958;12:309–320. doi: 10.1038/bjc.1958.37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cawthorn SJ, Parums DV, Gibbs NM, A'Hern RP, Caffarey SM, Broughton CI, Marks CG. Extent of mesorectal spread and involvement of lateral resection margin as prognostic factors after surgery for rectal cancer. Lancet. 1990;335:1055–1059. doi: 10.1016/0140-6736(90)92631-q. [DOI] [PubMed] [Google Scholar]
- 54.Merkel S, Mansmann U, Papadopoulos T, Wittekind C, Hohenberger W, Hermanek P. The prognostic inhomogeneity of colorectal carcinomas Stage III: a proposal for subdivision of Stage III. Cancer. 2001;92:2754–2759. [PubMed] [Google Scholar]
- 55.Picon AI, Moore HG, Sternberg SS, Minsky BD, Paty PB, Blumberg D, Quan SH, Wong WD, Cohen AM, Guillem JG. Prognostic significance of depth of gross or microscopic perirectal fat invasion in T3 N0 M0 rectal cancers following sharp mesorectal excision and no adjuvant therapy. Int J Colorectal Dis. 2003;18:487–492. doi: 10.1007/s00384-003-0504-1. [DOI] [PubMed] [Google Scholar]
- 56.Kim DJ, Kim JH, Lim JS, Yu JS, Chung JJ, Kim MJ, Kim KW. Restaging of Rectal Cancer with MR Imaging after Concurrent Chemotherapy and Radiation Therapy. Radiographics. 2010;30:503–516. doi: 10.1148/rg.302095046. [DOI] [PubMed] [Google Scholar]
- 57.Kuo LJ, Chern MC, Tsou MH, Liu MC, Jian JJ, Chen CM, Chung YL, Fang WT. Interpretation of magnetic resonance imaging for locally advanced rectal carcinoma after preoperative chemoradiation therapy. Dis Colon Rectum. 2005;48:23–28. doi: 10.1007/s10350-004-0787-5. [DOI] [PubMed] [Google Scholar]
- 58.Allen SD, Padhani AR, Dzik-Jurasz AS, Glynne-Jones R. Rectal carcinoma: MRI with histologic correlation before and after chemoradiation therapy. AJR Am J Roentgenol. 2007;188:442–451. doi: 10.2214/AJR.05.1967. [DOI] [PubMed] [Google Scholar]
- 59.Vliegen RF, Beets GL, Lammering G, Dresen RC, Rutten HJ, Kessels AG, Oei TK, de Bruïne AP, van Engelshoven JM, Beets-Tan RG. Mesorectal fascia invasion after neoadjuvant chemotherapy and radiation therapy for locally advanced rectal cancer: accuracy of MR imaging for prediction. Radiology. 2008;246:454–462. doi: 10.1148/radiol.2462070042. [DOI] [PubMed] [Google Scholar]
- 60.Kulkarni T, Gollins S, Maw A, Hobson P, Byrne R, Widdowson D. Magnetic resonance imaging in rectal cancer downstaged using neoadjuvant chemoradiation: accuracy of prediction of tumour stage and circumferential resection margin status. Colorectal Dis. 2008;10:479–489. doi: 10.1111/j.1463-1318.2007.01451.x. [DOI] [PubMed] [Google Scholar]
- 61.Johnston DF, Lawrence KM, Sizer BF, Arulampalam TH, Motson RW, Dove E, Lacey N. Locally advanced rectal cancer: histopathological correlation and predictive accuracy of serial MRI after neoadjuvant chemotherapy. Br J Radiol. 2009;82:332–336. doi: 10.1259/bjr/61056525. [DOI] [PubMed] [Google Scholar]
- 62.Borschitz T, Wachtlin D, Möhler M, Schmidberger H, Junginger T. Neoadjuvant chemoradiation and local excision for T2-3 rectal cancer. Ann Surg Oncol. 2008;15:712–720. doi: 10.1245/s10434-007-9732-x. [DOI] [PubMed] [Google Scholar]
- 63.Lahaye MJ, Beets GL, Engelen SM, Kessels AG, de Bruïne AP, Kwee HW, van Engelshoven JM, van de Velde CJ, Beets-Tan RG. Locally advanced rectal cancer: MR imaging for restaging after neoadjuvant radiation therapy with concomitant chemotherapy. Part II. What are the criteria to predict involved lymph nodes? Radiology. 2009;252:81–91. doi: 10.1148/radiol.2521081364. [DOI] [PubMed] [Google Scholar]
- 64.Engelen SM, Beets-Tan RG, Lahaye MJ, Kessels AG, Beets GL. Location of involved mesorectal and extramesorectal lymph nodes in patients with primary rectal cancer: preoperative assessment with MR imaging. Eur J Surg Oncol. 2008;34:776–781. doi: 10.1016/j.ejso.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 65.Engelen SM, Beets-Tan RG, Lahaye MJ, Lammering G, Jansen RL, van Dam RM, Konsten J, Leijtens JW, van de Velde CJ, Beets GL. MRI after chemoradiotherapy of rectal cancer: a useful tool to select patients for local excision. Dis Colon Rectum. 2010;53:979–986. doi: 10.1007/DCR.0b013e3181dc64dc. [DOI] [PubMed] [Google Scholar]
- 66.Marr R, Birbeck K, Garvican J, Macklin CP, Tiffin NJ, Parsons WJ, Dixon MF, Mapstone NP, Sebag-Montefiore D, Scott N, et al. The modern abdominoperineal excision: the next challenge after total mesorectal excision. Ann Surg. 2005;242:74–82. doi: 10.1097/01.sla.0000167926.60908.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Holm T, Ljung A, Häggmark T, Jurell G, Lagergren J. Extended abdominoperineal resection with gluteus maximus flap reconstruction of the pelvic floor for rectal cancer. Br J Surg. 2007;94:232–238. doi: 10.1002/bjs.5489. [DOI] [PubMed] [Google Scholar]
- 68.West NP, Finan PJ, Anderin C, Lindholm J, Holm T, Quirke P. Evidence of the oncologic superiority of cylindrical abdominoperineal excision for low rectal cancer. J Clin Oncol. 2008;26:3517–3522. doi: 10.1200/JCO.2007.14.5961. [DOI] [PubMed] [Google Scholar]
- 69.Guillem JG, Minsky BD. Extended perineal resection of distal rectal cancers: surgical advance, increased utilization of neoadjuvant therapies, proper patient selection or all of the above? J Clin Oncol. 2008;26:3481–3482. doi: 10.1200/JCO.2007.15.6646. [DOI] [PubMed] [Google Scholar]
- 70.Holzer B, Urban M, Hölbling N, Feil W, Novi G, Hruby W, Rosen HR, Schiessel R. Magnetic resonance imaging predicts sphincter invasion of low rectal cancer and influences selection of operation. Surgery. 2003;133:656–661. doi: 10.1067/msy.2003.150. [DOI] [PubMed] [Google Scholar]
- 71.Rullier E, Laurent C, Bretagnol F, Rullier A, Vendrely V, Zerbib F. Sphincter-saving resection for all rectal carcinomas: the end of the 2-cm distal rule. Ann Surg. 2005;241:465–469. doi: 10.1097/01.sla.0000154551.06768.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Williams NS, Murphy J, Knowles CH. Anterior Perineal PlanE for Ultra-low Anterior Resection of the Rectum (the APPEAR technique): a prospective clinical trial of a new procedure. Ann Surg. 2008;247:750–758. doi: 10.1097/SLA.0b013e31816b2ee3. [DOI] [PubMed] [Google Scholar]
- 73.Assenat E, Thézenas S, Samalin E, Bibeau F, Portales F, Azria D, Quenet F, Rouanet P, Saint Aubert B, Senesse P. The value of endoscopic rectal ultrasound in predicting the lateral clearance and outcome in patients with lower-third rectal adenocarcinoma. Endoscopy. 2007;39:309–313. doi: 10.1055/s-2007-966211. [DOI] [PubMed] [Google Scholar]
- 74.Hamilton SR, Aaltonen LA. World Health Organization Classification of Tumours. Pathology and Genetics of Tumours of the Digestive System. Lyon: IARC Press; 2000. pp. 105–120. [Google Scholar]
- 75.Kim MJ, Park JS, Park SI, Kim NK, Kim JH, Moon HJ, Park YN, Kim WH. Accuracy in differentiation of mucinous and nonmucinous rectal carcinoma on MR imaging. J Comput Assist Tomogr. 2003;27:48–55. doi: 10.1097/00004728-200301000-00010. [DOI] [PubMed] [Google Scholar]
- 76.Grillo-Ruggieri F, Mantello G, Berardi R, Cardinali M, Fenu F, Iovini G, Montisci M, Fabbietti L, Marmorale C, Guerrieri M, et al. Mucinous rectal adenocarcinoma can be associated to tumor downstaging after preoperative chemoradiotherapy. Dis Colon Rectum. 2007;50:1594–1603. doi: 10.1007/s10350-007-9026-1. [DOI] [PubMed] [Google Scholar]
- 77.Oberholzer K, Menig M, Kreft A, Schneider A, Junginger T, Heintz A, Kreitner KF, Hötker AM, Hansen T, Düber C, et al. Rectal Cancer: Mucinous Carcinoma on Magnetic Resonance Imaging Indicates Poor Response to Neoadjuvant Chemoradiation. Int J Radiat Oncol Biol Phys. 2011:Epub ahead of print. doi: 10.1016/j.ijrobp.2010.08.057. [DOI] [PubMed] [Google Scholar]
- 78.Kim H, Lim JS, Choi JY, Park J, Chung YE, Kim MJ, Choi E, Kim NK, Kim KW. Rectal cancer: comparison of accuracy of local-regional staging with two- and three-dimensional preoperative 3-T MR imaging. Radiology. 2010;254:485–492. doi: 10.1148/radiol.09090587. [DOI] [PubMed] [Google Scholar]
- 79.Torricelli P, Pecchi A, Luppi G, Romagnoli R. Gadolinium-enhanced MRI with dynamic evaluation in diagnosing the local recurrence of rectal cancer. Abdom Imaging. 2003;28:19–27. doi: 10.1007/s00261-001-0127-3. [DOI] [PubMed] [Google Scholar]
- 80.Kremser C, Judmaier W, Hein P, Griebel J, Lukas P, de Vries A. Preliminary results on the influence of chemoradiation on apparent diffusion coefficients of primary rectal carcinoma measured by magnetic resonance imaging. Strahlenther Onkol. 2003;179:641–649. doi: 10.1007/s00066-003-1045-9. [DOI] [PubMed] [Google Scholar]
- 81.Dzik-Jurasz A, Domenig C, George M, Wolber J, Padhani A, Brown G, Doran S. Diffusion MRI for prediction of response of rectal cancer to chemoradiation. Lancet. 2002;360:307–308. doi: 10.1016/S0140-6736(02)09520-X. [DOI] [PubMed] [Google Scholar]
- 82.Barbaro B, Vitale R, Leccisotti L, Vecchio FM, Santoro L, Valentini V, Coco C, Pacelli F, Crucitti A, Persiani R, et al. Restaging locally advanced rectal cancer with MR imaging after chemoradiation therapy. Radiographics. 2010;30:699–716. doi: 10.1148/rg.303095085. [DOI] [PubMed] [Google Scholar]
- 83.Hein PA, Kremser C, Judmaier W, Griebel J, Pfeiffer KP, Kreczy A, Hug EB, Lukas P, DeVries AF. Diffusion-weighted magnetic resonance imaging for monitoring diffusion changes in rectal carcinoma during combined, preoperative chemoradiation: preliminary results of a prospective study. Eur J Radiol. 2003;45:214–222. doi: 10.1016/s0720-048x(02)00231-0. [DOI] [PubMed] [Google Scholar]
- 84.Chinnaiyan AM, Prasad U, Shankar S, Hamstra DA, Shanaiah M, Chenevert TL, Ross BD, Rehemtulla A. Combined effect of tumor necrosis factor-related apoptosis-inducing ligand and ionizing radiation in breast cancer therapy. Proc Natl Acad Sci USA. 2000;97:1754–1759. doi: 10.1073/pnas.030545097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Ono K, Ochiai R, Yoshida T, Kitagawa M, Omagari J, Kobayashi H, Yamashita Y. Comparison of diffusion-weighted MRI and 2-[fluorine-18]-fluoro-2-deoxy-D-glucose positron emission tomography (FDG-PET) for detecting primary colorectal cancer and regional lymph node metastases. J Magn Reson Imaging. 2009;29:336–340. doi: 10.1002/jmri.21638. [DOI] [PubMed] [Google Scholar]
- 86.Bellomi M, Travaini LL. Imaging as a surveillance tool in rectal cancer. Expert Rev Med Devices. 2010;7:99–112. doi: 10.1586/erd.09.63. [DOI] [PubMed] [Google Scholar]
- 87.Kierkels RG, Backes WH, Janssen MH, Buijsen J, Beets-Tan RG, Lambin P, Lammering G, Oellers MC, Aerts HJ. Comparison between perfusion computed tomography and dynamic contrast-enhanced magnetic resonance imaging in rectal cancer. Int J Radiat Oncol Biol Phys. 2010;77:400–408. doi: 10.1016/j.ijrobp.2009.05.015. [DOI] [PubMed] [Google Scholar]
- 88.Schiepers C, Haustermans K, Geboes K, Filez L, Bormans G, Penninckx F. The effect of preoperative radiation therapy on glucose utilization and cell kinetics in patients with primary rectal carcinoma. Cancer. 1999;85:803–811. doi: 10.1002/(sici)1097-0142(19990215)85:4<803::aid-cncr7>3.0.co;2-t. [DOI] [PubMed] [Google Scholar]
- 89.Anderson H, Singh N, Miles K. Tumour response evaluation with fluorodeoxyglucose positron emission tomography: research technique or clinical tool? Cancer Imaging. 2010;10 Spec no A:S68–S72. doi: 10.1102/1470-7330.2010.9088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bassi MC, Turri L, Sacchetti G, Loi G, Cannillo B, La Mattina P, Brambilla M, Inglese E, Krengli M. FDG-PET/CT imaging for staging and target volume delineation in preoperative conformal radiotherapy of rectal cancer. Int J Radiat Oncol Biol Phys. 2008;70:1423–1426. doi: 10.1016/j.ijrobp.2007.08.043. [DOI] [PubMed] [Google Scholar]
- 91.Garlaschi A, Bacigalupo LE, Biscaldi E, Chiusano G, Basso C, Rollandi GA. Multi-modal non-rigid image registration of MR and PET-CT for staging and therapy of rectal adenocarcinoma. Presented as a Scientific Poster at the Radiological Society of North America November 29 - December 4, 2009; Chicago, IL. Abstract Book, 921 [Google Scholar]
- 92.Roels S, Slagmolen P, Nuyts J, Lee JA, Loeckx D, Maes F, Vandecaveye V, Stroobants S, Ectors N, Penninckx F, et al. Biological image-guided radiotherapy in rectal cancer: challenges and pitfalls. Int J Radiat Oncol Biol Phys. 2009;75:782–790. doi: 10.1016/j.ijrobp.2008.11.031. [DOI] [PubMed] [Google Scholar]