Abstract
Background
Medication nonadherence is a common problem among the elderly.
Objective
To conduct a systematic review of the published literature describing potential non-financial barriers to medication adherence among the elderly.
Methods
The PubMed and PsychINFO databases were searched for articles published in English between January 1998 and January 2010 that described “predictors,” “facilitators,” or “determinants” of medication adherence and those articles that examined the “relationship” between a specific barrier and adherence for elderly patients (ie, age ≥ 65 years) in the United States (U.S.). A manual search of the reference lists of identified articles and the authors’ files and recent review articles was conducted. The search included articles that (1) reviewed specific barriers to medication adherence and did not solely describe nonmodifiable predictors of adherence (eg, demographics, marital status); (2) were not interventions designed to address adherence; (3) defined adherence or compliance and specified its method of measurement; (4) involved U.S. participants only. Non-systematic reviews were excluded, as were studies that focused specifically on people who were homeless or substance abusers, or patients with psychotic disorders, tuberculosis, or Human Immunodeficiency Virus (HIV), because of the unique circumstances that surround medication adherence for each of these populations.
Results
Nine studies met inclusion criteria for this review. Four studies used pharmacy records/claims data to assess adherence, 2 studies used pill count/electronic monitoring, and 3 studies used other methods to assess adherence. Substantial heterogeneity existed among the populations studied as well as among the measures of adherence, barriers addressed, and significant findings. Some potential barriers (ie, factors associated with nonadherence) were identified from the studies, including patient-related factors such as disease-related knowledge, health literacy, and cognitive function, drug-related factors such as adverse effects and polypharmacy, and other factors including the patient-provider relationship and various logistical barriers to obtaining medications. None of the reviewed studies examined primary nonadherence or nonpersistence.
Conclusion
Medication nonadherence in the elderly is not well described in the literature, despite being a major cause of morbidity, and thus it is difficult to draw a systematic conclusion on potential barriers based on the current literature. Future research should focus on standardizing medication adherence measurements among the elderly in order to gain a better understanding of this important issue.
Keywords: medication adherence, elderly, barriers, systematic review
INTRODUCTION
Medications are frequently used in the elderly to improve quality of life, extend life-expectancy, and cure/mitigate disease. It is clear, however, that the elderly often fail to adhere to prescribed medications, leading to unwelcomed clinical and economic consequences.1-3
There are a variety of reasons why patients do not adhere to their prescribed medication regimens. One conceptual model of barriers to adherence describes patient, prescriber and health care system factors.4 Others have developed more detailed conceptual models specific to the elderly.2,3,5 Each model highlights the fact that the medication use process is affected by many factors in older adults, including drug- and patient-related factors such as patient representations of their illness, cognitive function, and medication side effects, as well as other factors (eg, patient-prescriber relationships). Furthermore, because older adults often suffer from multiple comorbid conditions and thus use more medications than their younger counterparts, medication nonadherence can have drastic deleterious health effects on the elderly.2 Therefore, finding potential areas for interventions to help improve this process should be a top priority of healthcare providers.
Most modifiable barriers that hinder an older adult from adequately adhering to their prescribed medications are not clearly described in the literature, with the exception of cost, which is well described.6-11 Prior reviews of medication adherence in the elderly cite inconsistencies across studies and draw few solid conclusions; additionally, these reviews contain many dated studies, and some include patients less than 65 years of age.1,2,12
Given this background and the objective to identify barriers to adherence specific to patients in the United States (U.S.), a systematic review of the published literature was conducted describing potential non-financial barriers to medication adherence among patients ≥ 65 years.
METHODS
Data Sources
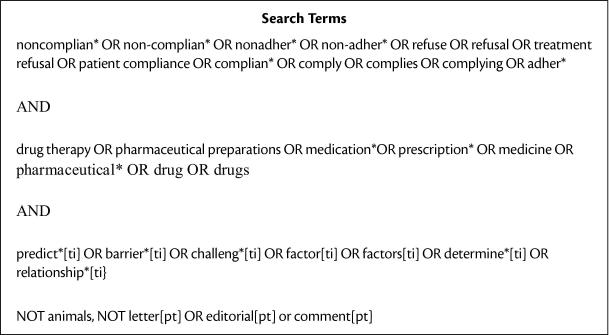
The PubMed and PsychINFO databases were searched, covering the time period from January 1998 to January 2010, limiting to English-language publications and omitting the publication types of “letters,” “editorials,” and “comments.” The year 1998 was used as the baseline year for the search because a previous review of medication adherence in the elderly was published using the years 1962 to 1997.1 The search strategy utilized both Medical Subject Headings (MeSH) and non-MeSH terms as outlined in Figure 1 below.
Figure 1.
List of Search Terms
Eligibility Criteria
The search focused on articles that examined barriers to medication adherence among U.S. elderly (ie, age ≥ 65 years), including articles that described “predictors,” “facilitators,” or “determinants” of medication adherence and those articles that examined the “relationship” between a specific barrier and adherence. The articles must have been published in a peer-reviewed journal (thus excluding conference proceedings, dissertations, and book chapters). Articles were included that (1) reviewed specific barriers to medication adherence and did not solely describe nonmodifiable predictors of adherence (eg, demographics, race/ethnicity, marital status); (2) were not interventions designed to address adherence; (3) defined adherence or compliance and specified its method of measurement; (4) involved U.S. participants only. Only U.S.-based studies were included since the effect of any particular barrier on adherence is influenced heavily by other factors of the healthcare system. Adherence studies from non-U.S. based healthcare systems are inherently different from those in the U.S., in that patients in other countries often have very different arrangements for procuring, paying for, and monitoring medications. Non-systematic reviews were excluded, as were studies that focused specifically on people who were homeless or substance abusers, or patients with schizophrenia or other psychotic disorders, tuberculosis, or Human Immunodeficiency Virus (HIV), because of the unique circumstances that surround medication adherence for each of these populations.
Search Strategy
The authors began by searching the literature for systematic reviews of adherence to medical therapy (whether medication or other therapies) to identify topics recently reviewed and found a large body of literature on the relationship between medication regimen complexity in the general adult population (ie, dosage frequency, administration instructions, and the prescribed dosage forms) and medication adherence.13-16 Therefore, although these reviews were not limited to those over age 65, the authors excluded individual studies in the review that focused on this relationship between adherence and medication regimen complexity; this review does not discuss this barrier further because of its clear relationship with adherence in the literature. However, the authors did not exclude studies that focused on the association between adherence and the total number of medications prescribed (ie, polypharmacy). As discussed previously, the search excluded individual studies of cost-sharing as a barrier to nonadherence, since this important area is well-described in the literature.6-11
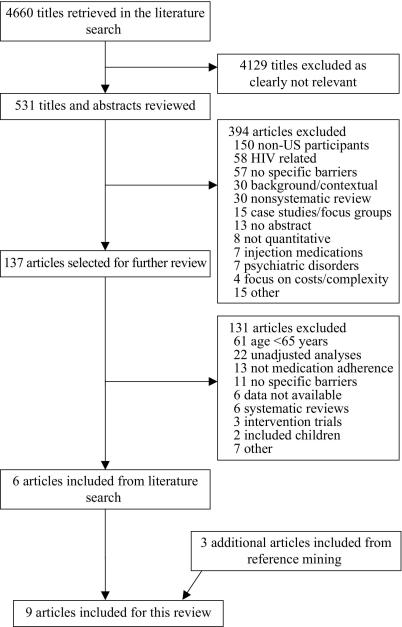
A flow-chart summary of the literature search is outlined in Figure 2. Briefly, of the 4,660 titles reviewed, 531 were deemed relevant to the analysis, and abstracts were pulled for review. Reviewers (W.G. and J. G.) then screened each of the abstracts independently for inclusion based on the criteria listed and resolved any disagreements by consensus, and 137 met criteria. Among the 137 articles reviewed, 61 included participants <65 years of age and thus were excluded. Additionally, 22 contained only unadjusted analyses without controlling for standard demographic factors and were excluded. Other reasons for article exclusion can be seen in Figure 2. The initial phase of the literature search resulted in 6 articles meeting the inclusion criteria. The authors conducted a manual search of the reference lists of the identified articles and the authors’ article files and recent reviews to identify additional publications, leading to the inclusion of 3 additional articles. A geriatric clinical pharmacist (Z.M.) reviewed potential articles for inclusion to ensure the articles addressed barriers relevant to the medication use process in older adults. Therefore, 9 total articles met final inclusion criteria and are the basis of this review.17-25
Figure 2.
Flow-Chart Summary of Literature Search
Data Items
Each article was coded on the following dimensions: (1) study design; (2) participant characteristics; (3) recruitment method; (4) sample size; (5) disease studied; (6) type of nonadherence (ie, nonpersistence, overadherence); (7) how adherence was assessed and measured (ie, self-report, pharmacy records/claims data, electronic monitoring, pill count, and exact scale or method used); (8) length of time over which adherence was measured, if specified; (9) specific barriers and predictors of adherence discussed, along with an indicator if a standard validated assessment of the barriers was included (eg, Beck Depression Inventory for depression). The individual barriers were assessed in each article using a standardized collection form that was created based on previously published conceptual frameworks addressing medication adherence among the elderly.2,5 Disagreements on articles to be included and on coding were resolved by consensus between the reviewers.
RESULTS
Nine articles that met inclusion criteria in this systematic review were included. Details from the studies in this review, including study sample, disease studied, method of assessing adherence, barriers discussed and findings, are summarized in Table 1. Four studies used pharmacy records/claims data to assess adherence, two studies used pill count/electronic monitoring, and three studies used other methods to assess adherence. The 9 articles included in this review varied in their methods of analysis, study population, and identification of exposure (barriers) and outcome variables (adherence). The result is tremendous heterogeneity among these studies; therefore, no attempt was made to combine the results into a meta-analysis. The following brief descriptions provide further information about the individual studies categorized by the method utilized to assess adherence.
Table 1.
Studies Included in the Systematic Review
| Citation | Analyzed (Final) Sample Size |
Study Design |
Recruitment Site |
Sample Description |
How Adherence is Assessed |
Measure of Adherence |
Barriers Addressed | Findings |
|---|---|---|---|---|---|---|---|---|
| Balkrishnan et al (2003)17 |
775 | Observational cohort |
Health plan: Winston- Salem, NC |
Adults aged ≥ 65 years with type 2 diabetes |
Pharmacy records/ claims data |
Medication possession ratio |
Comorbidity*; Depression*; Alcohol use; Smoker; Physical activity; Self-reported health-status* |
Antidiabetic medication adherence was negatively associated with comorbidity severity (P<0.05). Adherence was not significantly associated with depression severity, alcohol consumption, smoking, physical activity, or perceived health status. |
| Balkrishnan et al (2006)18 |
275 | Observational cohort |
Health plan: southeastern USA |
Adults aged ≥ 65 years with overactive bladder |
Pharmacy records/ claims data |
Medication possession ratio |
Comorbidity*; Depression*; Alcohol use; Smoker; Physical activity; Self-reported health-status*; |
Adherence was positively associated with perceived health status (P<0.05) and negatively associated with comorbidity severity (P<0.01). Depression, alcohol consumption, smoking, and physical activity were not significantly associated with adherence. |
| Chapman et al (2008)19 |
4,052 | Observational cohort |
Protocare Sciences Managed Care Database |
Adults aged ≥ 65 years who initiated treatment with both AH and LL therapy within a 90- day period |
Pharmacy records/ claims data |
Medication possession ratio, Cutoff: 80.00 |
Time between start of AH and LL therapy; Depression; Dementia; # of prescription medications; # of outpatient physician visits |
Adherence rate was increased with AH/LL therapies being initiated closer together in time (AOR 1.13 for 0-30 days vs 61-90 days; 95% CI 1.00 to 1.29 P = 0.056) and with having more outpatient physician visits in the prior year (AOR 1.26 for 4-6 visits vs 0-1 visits; 95 % CI 1.08 to 1.47; P=0.003). Adherence rate was decreased with taking more medications (AOR 0.43 for ≥ 6 medications vs 0-1 medication; 95% CI 0.36 to 0.50; P<0.001). The relationship of depression and dementia and adherence was not significant. |
| Gazmararian et al (2006)20 |
1,549 | Observational cohort |
Health plans: Cleveland, OH; Houston, TX; South Florida; Tampa, FL |
Adults aged ≥ 65 years with coronary heart disease, diabetes, hyper- lipidemia, and/or HTN |
Pharmacy records/ claims data |
Cumulative medication gap less than 20% |
Health literacy*; # of oral prescription medications (≤ 3 vs >3); Cognitive function* |
Health literacy and number of prescription medications were both related to medication adherence in bivariate analyses (P>0.05). However, cognitive function was not associated with adherence in bivariate analyses (P=0.07). Unadjusted analysis showed that those with inadequate health literacy skills had increased odds (OR 1.37; 95% CI, 1.08 to 1.74) of low refill adherence vs those with adequate literacy skills; however, multivariate analysis did not support this relationship between inadequate health literacy skills and low refill adherence (AOR 1.23; 95% CI, 0.92 to 1.64). Multivariate analysis showed that those who took more medications had a lower odds of having nonadherence compared to those taking less medication (AOR 0.77; 95%, CI 0.73 to 0.95) after controlling for health literacy, age, race, sex, and education. |
| Gray et al (2001)21 |
147 | Observational cohort |
Home health agencies: Madison, WI |
Adults aged ≥ 65 years receiving home health care following hospitalization for medical illness |
Pill count | Underadherence: at least one medication < 70%; Overadherence: at least one medication > 120% |
# of comorbidities; Cognitive function*; Dependency in ADLs; Depression*; # of prescription medications; Taking a drug ≥3 times/day; Requiring help with administration of medications |
Multivariable analysis showed that underadherence was significantly associated with poor cognition (AOR 2.5, 95% CI 1.02 to 6.10) and greater medication use (AOR 1.16, 95% CI 1.03 to 1.31) after controlling for demographic, health-related and medication-related covariates. Multivariable analysis did not reveal any significant associations with any of the barriers and overadherence. |
| Insel et al (2006)22 |
95 | Observational cohort |
Community sample |
Adults aged ≥ 67 years living in the community who self- manage their medications |
Electronic monitoring (medication- monitoring cap system) |
Proportion of days with correct number of doses taken |
Cognitive function*; Memory and comprehension*; Depression*; Executive function* |
In unadjusted analyses, cognitive function (MMSE score), executive function and memory were significantly correlated with medication adherence. A composite score for executive working memory (β=0.44, P<0.05) was the only variable associated in multivariate analysis with better medication adherence, after adjusting for demographic characteristics, illness severity, mental health status, and financial status. |
| Ownby et al (2006)23 |
63 | Cross- sectional |
Single clinic: Miami Beach, FL |
Patients with memory disorders cared for at a memory disorders clinic |
Other | Caregivers’ reports of patients’ medication adherence by asking how often the patient took the medication on a five-point scale (‘Almost never’ to ‘Almost always’) |
Perceived disease outcome (without medication treatment); Perceived seriousness of disease; # of prescription medications; Presence of side effects; Depression*; Cognitive function*; Memory strategy used: rely on self |
In a patient characteristics model, perceived outcome of disease without medication treatment (β = 0.32; P<0.001) was associated with adherence, and reliance on self to remember (β = −0.44; P<0.001) was negatively associated with adherence. Depression and cognitive function were not associated with adherence. In a disease representation model, the occurrence of side effects was negatively associated with adherence (β = −0.21; P<0.001). |
| Turner et al (2009)24 |
202 | Cross- sectional |
Multiple clinics: Philadelphia, PA |
Adults aged ≥ 70 years with HTN |
Other | Self-reported not missing any medication in the past 3 months |
Antihypertensive regimen complexity (≥ 4 medications); Self-reported health status; Self-activation and social support; Personal medication taking habits; Not/somewhat unimportant to fill new prescriptions quickly; 8 logistical barriers to filling medications (remembering to take the medication, cost of medication, medication not covered by insurance, transportation to pharmacy, having to switch to generic, concerned about too many medications, having to get medication every month, having to deal with Internet); Doctor-patient relationship; Patient knowledge about conditions due to HTN and not due to HTN |
Adherence was significantly negatively associated (less likely) with the following: having ≥ 4 antihypertensive medications in regimen (AOR 0.23; 95% CI, 0.08 to 0.72); running out of medication (AOR 0.25; 95% CI, 0.09 to 0.66), having more logistical barriers to obtaining medication (AOR per each of 8 barriers 0.72; 95% CI, 0.57 to 0.91), lower priority given to discussing HTN with the doctor (AOR 0.32; 95% CI, 0.12 to 0.84), and less knowledge about disease not due to HTN (AOR 0.62; 95% CI, 0.43 to 0.89). |
| Stoehr et al (2008)25 |
343 | Cross- sectional |
Multiple clinics: SW Pennsylvania |
Adults aged ≥ 65 years cared for in 7 private office practices |
Other | Global judgment by research nurses (ie, dichotomous outcome, yes/no) after a home visit |
Cognitive function*; Verbal learning and memory*; # of prescription medications (≥ 5 vs < 5); Dosing frequency (≥4 vs <4 times/day) |
Adherence was negatively associated with a greater number of prescription medications (OR 0.45; 95% CI, 0.21 to 0.95; P=0.04), and adherence was positively associated with higher scores on the executive function test (OR 3.25; 95% CI, 1.13 to 9.33; P=0.03). |
ADL = activities of daily living; AH = antihypertensive; AOR = adjusted odds ratio; ER = emergency room; HMO = health maintenance organization; HTN = hypertension; LL = lipid lowering; OR = odds ratio; USA = United States of America
Validated assessments used to measure barrier
Pharmacy Record/Claims Data
A longitudinal cohort study assessed the relationship between self-reported health status (using Short Form-12 scores) and antidiabetic medication adherence among 775 patients aged ≥ years with type 2 diabetes enrolled continuously in one Medicare managed care plan.17 Adherence was measured using the standard definition of Medication Possession Ratio (MPR) (ie, the days of antidiabetic prescription supply dispensed divided by the number of days between the prescription refills), with correction for days hospitalized. Mean MPRs for antidiabetic medications ranged from 0.70 to 0.78 across 5 years of patient data. After controlling for demographic, clinical, and other health status-related covariates, an increase in comorbidity severity (measured using the Charlson Index) was associated with a significant decrease in MPR (P<0.05). Potentially modifiable barriers assessed (ie, depression severity, alcohol consumption, smoking, physical activity, and perceived health status) were not significantly associated with adherence.
Balkrishnan et al. used the same database to conduct another longitudinal cohort study of 275 patients with overactive bladder to examine the relationship between self-reported health status (using Short Form-12 scores) and antimuscarinic medication adherence.18 Adherence was measured again using standard definitions of the MPR. The average MPR for antimuscarinic medications was 0.42 across the 3 years of study. In multivariate analyses, an increase in comorbidity severity (Charlson Index) was associated with a decrease in MPR (P<0.01); conversely, self-reported health status was significantly associated with an increase in MPR (P<0.05). Various other modifiable barriers assessed (ie, depression, alcohol consumption, smoking, and physical activity) were not significantly associated with adherence.
The third pharmacy claims-based study was a retrospective cohort study of 4,052 Medicare managed care enrollees aged ≥ 65 years who initiated concomitant antihypertensive (AH) and lipid-lowering (LL) therapy.19 Adherence was measured as the proportion of days covered by any AH and/or LL medication for up to 36 months (mean follow-up 19.5 months). Patients were classified as adherent if they had ≥ 80% days covered by both AH and LL medication. The proportion of patients who were adherent to both agents was 40.5% at 3 months, 32.7% at 6 months, and 32.9% at 12 months. After adjusting for age, sex, baseline history of depression, dementia, and diabetes, adherence was better among those having more outpatient physician visits in the year prior (AOR 1.26 for 4-6 visits vs 0-1 visits; 95% CI 1.08 to 1.47; P=0.003). Initiating AH/LL therapies closer together in time did not have a statistically significant independent effect on adherence (adjusted odds ratio [AOR] 1.13 for 0-30 days vs 61-90 days; 95% CI 1.00 to 1.29; P=0.056) Adherence was decreased in those patients taking more medications (AOR 0.43 for ≥ 6 medications vs 0-1 medication; 95% CI 0.36 to 0.50; P<0.001).
The fourth study using pharmacy claims was a prospective cohort study of 1,549 community-dwelling Medicare patients over age 65 newly enrolled in managed care plans who were taking medication for coronary heart disease, hypertension, diabetes, and/or hyperlipidemia.20 The study assessed the relationship between health literacy (measured using the Short Test of Functional Health Literacy in Adults) and medication adherence. Refill adherence (over one year) was determined separately for each medication using a cumulative medication gap (CMG) (ie, number of days in which the medication was not available between each fill divided by the number of days between the first and last fill), with correction for days hospitalized. Low adherence was defined as CMG ≥ 20%. Overall, 40% (620/1,549) of study participants had low refill adherence. Bivariate analyses showed that health literacy and the total number of scheduled oral medications (≤ 3 vs > 3 medications) were both related to medication adherence (P<0.05, both). In unadjusted analyses, respondents with inadequate health literacy had higher odds of nonadherence (OR 1.37, 95% CI 1.08 to 1.74). However, after controlling for sociodemographics, number of medications, and health status, health literacy was not an independent predictor of refill adherence (AOR 1.23; 95% CI, 0.92 to 1.64). On the other hand, those who took more medications (>3) were found to have significantly lower odds of having nonadherence compared to those taking less medications (≤ 3) (AOR 0.77; 95% CI, 0.73 to 0.95).
Pill Count/Electronic Monitoring
An observational cohort study assessed the prevalence of and risk factors associated with under- and overadherence with medications in a two-week period after hospital discharge in 147 patients age 65 and older receiving home health services.21 A home visit within five days of hospitalization and two weeks after baseline was conducted to interview the patients and assess medication use with pill count. Underadherence was defined as having at least one medication with less than 70% compliance, and overadherence was defined as having at least one medication with more than 120% compliance. The authors found that 44% (64/147) of the final sample was under- or overadherent; underadherence with at least one medication was more common than overadherence (30.6%; 45/147 vs. 11.6%; 17/147, respectively). After controlling for demographic, health-related and medication-related covariates, poor cognition (ie, Mini-Mental State Examination score <24) (AOR 2.5, 95% CI 1.02 to 6.10) and higher medication use (AOR 1.16, 95% CI 1.03 to 1.31) were significantly associated with underadherence. Specifically, the likelihood of nonadherence increased by 16% for each one-unit increase in medications that a person was taking (eg, 3 vs 2 medications). None of the barriers assessed were found to have a significant association with overadherence on multivariate analysis.
In another observational cohort study, researchers assessed the association between cognitive processes (ie, executive function, working memory, cued recall, and recognition memory) and medication adherence over an 8-week period among 95 community-dwelling adults age 67 and older .22 An initial 3-hour intake visit was conducted at which time the subject was asked to place one of their prescribed medications in a medication container with a medication-monitoring cap system (MEMS). Adherence was defined as the percentage of days that the correct number of doses was taken. The authors found that medications were taken as prescribed an average of 80.4% of days. There was no significant association between the type of medication and adherence, although that analysis was limited by small sample size. After controlling for various covariates, including demographics, cognitive and executive function, the only significant predictor variable was the executive-working memory score (β = 0.44, P<0.01). Of note, a memory composite score and depression were not significantly associated with adherence.
Other
A cross-sectional observational study assessed factors related to adherence in 63 patients (mean age 76 years) with dementia or mood illnesses seen at a memory disorders clinic. The study used a questionnaire to ask about patient beliefs about their illness, mnemonic strategies to assist patients in adherence, and other patient characteristics.23 Medication adherence was primarily measured using caregivers’ reports of patients’ medication adherence. Both patients and caregivers were asked how often the patient took their medication on a five-point scale (‘Almost never’ to ‘Almost always’). Patients and their caregivers were also asked questions assessing their beliefs about the seriousness of each condition for which a medication was prescribed and the likely outcome of that condition without treatment. Additional information was collected, including presence of side effects, total number of medications taken, and patients’ mood and cognitive status in addition to the methods used to remember to take their medication. Overall, patient perceived outcome of their condition without treatment was associated with reported adherence (β = 0.32, P<0.001), whereas the occurrence of side effects (β = −0.21) and reliance on self to remember (β = −0.44) were negatively related to adherence (P<0.001, both). Depression and cognitive function were not found to be significantly associated with adherence.
Turner et al reported on a cross-sectional telephone survey assessing antihypertensive medication adherence and potential barriers in a representative sample of 202 patients aged ≥ 70 years from four urban primary care practices.24 Antihypertensive adherence was measured using self-report (ie, ‘When was the last time you missed taking any of your blood pressure pills?’), and multiple other questions were asked regarding health issues, personal experience and social support, medication insurance, patient-physician interaction, hypertension knowledge, and barriers to filling and using antihypertensive medications (remembering to take the medication, cost of medication, medication not covered by insurance, transportation to pharmacy, having to switch to generic, concerned about too many medications, having to get medication every month, having to deal with Internet). Medication adherence was defined as not missing any medication in the past 3 months. Overall, 22% (44/202) of the subjects reported missing taking their blood pressure medication in the past 3 months. The final multivariate analysis found poorer adherence to be significantly associated with the following barriers: having ≥ 4 antihypertensive medications (AOR 0.23; 95% CI, 0.08 to 0.72); running out of medication (AOR 0.25; 95% CI, 0.09 to 0.66); having more logistical barriers to obtaining antihypertensive medication (AOR per each of 8 barriers assessed 0.72; 95% CI, 0.57 to 0.91); lower priority given to discussing hypertension with the doctor (AOR 0.32; 95% CI, 0.12 to 0.84); and less knowledge about disease not related to hypertension (AOR 0.62; 95% CI, 0.43 to 0.89) (P<0.05, all).
A third observational cross-sectional survey assessed medication adherence and self-reported management of one’s own medication in 343 patients aged ≥ 65 years at 7 private office practices in southwest Pennsylvania.25 Medication adherence was measured using a global judgment of the level of prescription adherence by research nurses (ie, dichotomous outcome, yes/no) after a home visit in which the patient’s medication use process was assessed. Nonadherence was defined as those subjects who failed to keep up with any medication, took less than half of the doses as prescribed, or did not take ≥ 1 medication as directed even if adherent with the other medications. Overall, 89.8% (308/343) of the subjects were classified as adherent. After adjusting for multiple covariates, having better executive function (ie, higher scores on Part B of the Trail Making Test) was significantly associated with better adherence (AOR 3.25; 95% CI 1.13 to 9.33; P=0.03). In addition, having a higher total number of prescription drugs (≥5) was significantly negatively associated with adherence (AOR 0.45; 95% CI, 0.21 to 0.95; P=0.04).
DISCUSSION
There are no known prior systematic reviews of the non-financial barriers to medication adherence among the U.S. elderly (ie, age ≥ 65 years). The search found only 9 studies that met the inclusion criteria, and each one studied a different population and/or disease, or used a different assessment of medication adherence, making a clear synthesis of the literature extremely difficult. Studies of adherence have been burdened by heterogeneity for decades,26-28 and recent literature seems to be no different. This heterogeneity reflects the fact that medication adherence is an extremely complex behavior, and identifying a clear set of barriers that applies to all patients is not possible and probably not advised.
In light of the serious limitations of the current literature on medication adherence among the elderly, it is important to recognize what can be learned from published studies and to focus on ways to improve future research. Based on this review, several factors have been shown to be potential barriers to adherence and can be placed into 3 categories using a previously published approach2 – patient-related factors, drug-related factors, and other factors.
Common patient-related factors previously found to be associated with medication adherence include socio-demographics, psycho-social profile, comorbidities, cognitive ability, and health beliefs.2 Although most socio-demographic characteristics (eg, age, gender, race) and comorbidities are non-modifiable, other patient-related variables are potentially modifiable. This review found 1 study reporting that patients with hypertension having less knowledge about diseases not related to hypertension (eg, arthritis) were less likely to be adherent to their antihypertensive therapy.24 Educating patients, therefore, so that they understand the true potential risks of their disease state could possibly help minimize counterproductive health beliefs and promote motivation to adhere to treatment.
Another study reported that inadequate health literacy was associated with low adherence in unadjusted analysis but not in adjusted analyses.20 While it has been posited that an adequate level of functional health literacy is necessary to achieve successful medication adherence, this study used prescription refills records to measure adherence and it could be possible that health literacy skills are more important in taking medication correctly rather than refilling a prescription; correct medication administration would not be captured using administrative data.20 Future research on health literacy and adherence should use additional measures of adherence (eg, self-report, electronic monitoring) to better describe this complex relationship.
Cognitive function was significantly associated with underadherence in 1 study using a validated instrument (MMSE).21 Four other studies in this review measured cognitive function but did not find significant results.19,22,23,25 One of those studies, however, found that reliance on self to remember to take medications was negatively associated with adherence.23 Any research assessing the relationship between cognition and adherence should likely account for the degree of assistance with medication use received by the patient. Clearly, further research is needed to better understand the relationship between cognitive function and adherence among older adults.
Common drug-related factors previously identified as being associated with medication adherence include the number of drugs taken, adverse effects, and administration regimens.2 While the number of drugs may be expected to have a negative impact on adherence, this has not always proven to be the case.2 Similar to prior research showing mixed results for the effect of number of drugs on adherence, the current review found 4 studies19,21,24,25 that reported a negative association between taking more drugs and adherence (ie, greater number of drugs being associated with worse adherence) and 1 study20 that found a positive association between taking more drugs and adherence (ie, greater number of drugs being associated with better adherence). Not surprisingly, 1 study found that patients who experienced side effects from their medication were more likely to be nonadherent.23 Due to the uncertainty surrounding these drug-related barriers among older adults, perhaps the research focus in this area should shift towards understanding the effect of the appropriateness of drug regimen on adherence rather than the count of the total number of drugs. Although this review did not include studies focused solely on medication regimen complexity, prior literature is fairly clear on the association with more complex dosing regimens and poorer adherence.13-16
Some other factors potentially associated with medication adherence in previous reviews include the patient-prescriber relationship, access to medication, and social support.2 The current review found 1 study reporting that patients with hypertension who gave lower priority to discussing their hypertension with the physician were significantly more likely to be nonadherent to their blood pressure medication.24 This suggests that improving the patient-prescriber relationship is an area for future research to potentially improve patients’ adherence. Furthermore, this same study identified potential logistical barriers to successful adherence with the medication use process, including cost of medication, medication not being covered by insurance, transportation to a pharmacy, and having to switch to a generic medication, to name a few.24 Older adults face multiple logistical barriers throughout the medication use process, and identifying and addressing such barriers on an individual basis is critical to successful adherence.
Future research should strive to better describe the various types of nonadherence among older adults, including primary nonadherence (or nonfulfillment) and nonpersistence. Primary nonadherence occurs when the provider makes recommendations about a course of therapy that the patient ultimately does not initiate. 29 Nonpersistence occurs when the patient decides to stop taking the medication after starting it, without being advised by a health professional to do so. 30 None of the studies included in this review assessed primary nonadherence, and only one study measured overadherence.21 Future research in these understudied areas of the medication use process could provide greater understanding of modifiable barriers to adherence.
This review is subject to several limitations inherent in systematic reviews. First, because the search only included two databases and because of the selection of search terms, it is possible some studies were missed, despite reference mining. Second, studies with null effects might be unpublished disproportionally to those with significant results in the peer reviewed journals included in the search, potentially leading to publication bias. Finally, because the inclusion criteria were fairly strict, the generalizability of this review study is limited to the specific populations targeted (ie, U.S.-based studies assessing barriers other than cost and medication regimen complexity to medication adherence). Although this systematic review does not assess access/cost as barriers, it is clear that financial concerns do affect medication use in the elderly,7 and it is promising to note that the implementation of Medicare Part D may be improving medication adherence among older adults.31,32
CONCLUSION
This systematic review found a large amount of heterogeneity in the methods used to define, assess and measure medication adherence in the elderly; thus, it is not possible to make systematic conclusions. However, several potentially modifiable barriers to medication adherence were identified. The current state of the literature regarding modifiable barriers to medication adherence among older adults is limited and suggests a great need for well-designed studies and a consistently measured method to study adherence in this population. Furthermore, future research should assess clinical outcomes associated with adherence among older adults.
ACKNOWLEDGEMENTS
This study was supported by an Agency for Healthcare Research and Quality grant (T32 HS00046-14), a National Institute of Aging Grant (T32 AG021885), and Mehlman Vogel Castagnetti. Dr. Gellad is additionally supported by a VA HSR&D Career Development Award. The authors would like to thank Joseph T. Hanlon, PharmD, MS for his assistance with earlier drafts of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Balkrishnan R. Predictors of medication adherence in the elderly. Clin Ther. 1998;20:764–771. doi: 10.1016/s0149-2918(98)80139-2. [DOI] [PubMed] [Google Scholar]
- 2.Hughes CM. Medication non-adherence in the elderly: how big is the problem? Drugs Aging. 2004;21:793–811. doi: 10.2165/00002512-200421120-00004. [DOI] [PubMed] [Google Scholar]
- 3.Murray MD, Morrow DG, Weiner M, Clark DO, Tu W, Deer MM, Brater DC, Weinberger M. A conceptual framework to study medication adherence in older adults. Am J Geriatr Pharmacother. 2004;2:36–43. doi: 10.1016/s1543-5946(04)90005-0. [DOI] [PubMed] [Google Scholar]
- 4.Osterberg L, Blaschke T. Adherence to medication. N Engl J Med. 2005;353:487–497. doi: 10.1056/NEJMra050100. [DOI] [PubMed] [Google Scholar]
- 5.Park DC, Jones TR. Medication adherence and aging. In: Fisk AD, Rogers WA, editors. Handbook of Human Factors and the Older Adult. Academic Press; San Diego, Calif.: 1997. pp. 257–288. [Google Scholar]
- 6.Gibson TB, Ozminkowski RJ, Goetzel RZ. The effects of prescription drug cost sharing: a review of the evidence. Am J Manag Care. 2005;11:730–740. [PubMed] [Google Scholar]
- 7.Soumerai SB, Pierre-Jacques M, Zhang F, Ross-Degnan D, Adams AS, Gurwitz J, Adler G, Safran DG. Cost-related medication nonadherence among elderly and disabled medicare beneficiaries: a national survey 1 year before the medicare drug benefit. Arch Intern Med. 2006;166:1829–1835. doi: 10.1001/archinte.166.17.1829. [DOI] [PubMed] [Google Scholar]
- 8.Goldman DP, Joyce GF, Zheng Y. Prescription drug cost sharing: associations with medication and medical utilization and spending and health. JAMA. 2007;298:61–69. doi: 10.1001/jama.298.1.61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Briesacher BA, Gurwitz JH, Soumerai SB. Patients at-risk for cost-related medication nonadherence: a review of the literature. J Gen Intern Med. 2007;22:864–871. doi: 10.1007/s11606-007-0180-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gellad WF, Haas JS, Safran DG. Race/ethnicity and nonadherence to prescription medications among seniors: results of a national study. J Gen Intern Med. 2007;22:1572–1578. doi: 10.1007/s11606-007-0385-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Neuman P, Strollo MK, Guterman S, Rogers WH, Li A, Rodday AM, Safran DG. Medicare prescription drug benefit progress report: findings from a 2006 national survey of seniors. Health Aff (Millwood) 2007;26:w630–643. doi: 10.1377/hlthaff.26.5.w630. [DOI] [PubMed] [Google Scholar]
- 12.Vik SA, Maxwell CJ, Hogan DB. Measurement, correlates, and health outcomes of medication adherence among seniors. Ann Pharmacother. 2004;38:303–312. doi: 10.1345/aph.1D252. [DOI] [PubMed] [Google Scholar]
- 13.Claxton AJ, Cramer J, Pierce C. A systematic review of the associations between dose regimens and medication compliance. Clin Ther August. 2001;23:1296–1310. doi: 10.1016/s0149-2918(01)80109-0. [DOI] [PubMed] [Google Scholar]
- 14.Iskedjian M, Einarson TR, MacKeigan LD, Shear N, Addis A, Mittmann N, Ilersich AL. Relationship between daily dose frequency and adherence to antihypertensive pharmacotherapy: evidence from a meta-analysis. Clin Ther. 2002;24:302–316. doi: 10.1016/s0149-2918(02)85026-3. [DOI] [PubMed] [Google Scholar]
- 15.Ingersoll KS, Cohen J. The impact of medication regimen factors on adherence to chronic treatment: a review of literature. J Behav Med. 2008;31:213–224. doi: 10.1007/s10865-007-9147-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Saini SD, Schoenfeld P, Kaulback K, Dubinsky MC. Effect of medication dosing frequency on adherence in chronic diseases. Am J Manag Care. 2009;15:e22–33. [PubMed] [Google Scholar]
- 17.Balkrishnan R, Rajagopalan R, Camacho FT, Huston SA, Murray FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with type 2 diabetes mellitus: a longitudinal cohort study. Clin Ther. 2003;25:2958–2971. doi: 10.1016/s0149-2918(03)80347-8. [DOI] [PubMed] [Google Scholar]
- 18.Balkrishnan R, Bhosle MJ, Camacho FT, Anderson RT. Predictors of medication adherence and associated health care costs in an older population with overactive bladder syndrome: a longitudinal cohort study. J Urol. 2006;175:1067–1071. doi: 10.1016/S0022-5347(05)00352-6. [DOI] [PubMed] [Google Scholar]
- 19.Chapman RH, Petrilla AA, Benner JS, Schwartz JS, Tang SS. Predictors of adherence to concomitant antihypertensive and lipid-lowering medications in older adults: a retrospective, cohort study. Drugs Aging. 2008;25:885–892. doi: 10.2165/00002512-200825100-00008. [DOI] [PubMed] [Google Scholar]
- 20.Gazmararian JA, Kripalani S, Miller MJ, Echt KV, Ren J, Rask K. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006;21:1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gray SL, Mahoney JE, Blough DK. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 2001;35:539–545. doi: 10.1345/aph.10295. [DOI] [PubMed] [Google Scholar]
- 22.Insel K, Morrow D, Brewer B, Figueredo A. Executive function, working memory, and medication adherence among older adults. J Gerontol B Psychol Sci Social Sci. 2006;61:P102–P107. doi: 10.1093/geronb/61.2.p102. [DOI] [PubMed] [Google Scholar]
- 23.Ownby RL, Hertzog C, Crocco E, Duara R. Factors related to medication adherence in memory disorder clinic patients. Aging Ment Health. 2006;10:378–385. doi: 10.1080/13607860500410011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Turner BJ, Hollenbeak C, Weiner MG, Ten Have T, Roberts C. Barriers to adherence and hypertension control in a racially diverse representative sample of elderly primary care patients. Pharmacepidemiol Drug Saf. 2009;18:672–681. doi: 10.1002/pds.1766. [DOI] [PubMed] [Google Scholar]
- 25.Stoehr GP, Lu SY, Lavery L, Bilt JV, Saxton JA, Chang CC, Ganguli M. Factors associated with adherence to medication regimens in older primary care patients: the Steel Valley Seniors Survey. Am J Geriatr Pharmacother. 2008;6:255–263. doi: 10.1016/j.amjopharm.2008.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW. Patient adherence and medical treatment outcomes: a meta-analysis. Med Care. 2002;40:794–811. doi: 10.1097/00005650-200209000-00009. [DOI] [PubMed] [Google Scholar]
- 27.DiMatteo MR. Variations in patients’ adherence to medical recommendations: a quantitative review of 50 years of research. Med Care. 2004;42:200–209. doi: 10.1097/01.mlr.0000114908.90348.f9. [DOI] [PubMed] [Google Scholar]
- 28.Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database Syst Rev. 2008;2:CD000011. doi: 10.1002/14651858.CD000011.pub3. [DOI] [PubMed] [Google Scholar]
- 29.Fischer MA, Stedman MR, Lii J, et al. Primary medication non-adherence: analysis of 195,930 electronic prescriptions. J Gen Intern Med. 2010;25:284–290. doi: 10.1007/s11606-010-1253-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cramer JA, Roy A, Burrell A, et al. Medication compliance and persistence: terminology and definitions. Value Health. 2008;11:44–47. doi: 10.1111/j.1524-4733.2007.00213.x. [DOI] [PubMed] [Google Scholar]
- 31.Madden JM, Graves AJ, Zhang F, Adams AS, Briesacher BA, Ross-Degnan D, Gurwitz JH, Pierre-Jacques M, Safran DG, Adler GS, Soumerai SB. Cost-related medication nonadherence and spending on basic needs following implementation of Medicare Part D. JAMA. 2008;299:1922–1928. doi: 10.1001/jama.299.16.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhang Y, Lave JR, Donohue JM, Fischer MA, Chernew ME, Newhouse JP. The impact of Medicare Part D on medication adherence among older adults enrolled in Medicare-Advantage products. Med Care. 2010;48:409–417. doi: 10.1097/MLR.0b013e3181d68978. [DOI] [PubMed] [Google Scholar]