Abstract
Purpose
Koreans are recently at higher risk for coronary heart disease than are the Japanese. We aimed to evaluate levels of carotid intima-media thickness (IMT) and coronary risk factors in Korean and Japanese men in the post World War II birth cohort.
METHODS
We conducted a population-based study of 352 randomly-selected healthy men aged 40–49 years: 102 Koreans in Ansan City, Gyeonggi-do, Korea and 250 Japanese in Kusatsu City, Shiga, Japan. Imaging carotid IMT by ultrasound and other procedures were standardized. Analyzing blood samples and reading carotid IMT were performed at the University of Pittsburgh.
RESULTS
Despite more favorable or similar features in coronary risk factors as compared to the Japanese men, the Korean men had a higher crude IMT level than the Japanese men (mean ± s.e., .655 ± .008 mm versus .616 ± .005 mm, respectively, p<.0001). The difference in the levels of carotid IMT significantly remained after adjusting for metabolic and conventional risk factors (.654± .008 mm versus .616 ± .005 mm, respectively, p<.0001).
CONCLUSIONS
Among men aged 40–49, Koreans had significantly higher levels of carotid IMT than the Japanese. Factors that underlie the different susceptibility to subclinical atherosclerosis need to be explored.
Keywords: atherosclerosis, carotid artery, cohort studies, coronary disease, Japanese, Koreans
Among the Asian-Pacific region, Korea and Japan had relatively low coronary heart disease (CHD) mortality rates.[1] However, CHD mortality rate in Korea has been increasing since the 1980s as in many other Asian countries, whereas that in Japan has been decreasing since the 1970s.[1, 2] Among men in the post World War II (WWII) cohort, the CHD mortality rate in Korea has, in fact, exceeded that in Japan since the late 1980s.[3]
Compared to other Asian countries, Korea and Japan, closely located in East Asia, have relative similarity in socio-cultural and genetic background.[1, 4, 5] Furthermore, the post WWII birth cohorts of the two countries are more likely to have adopted a westernized lifestyle than the old cohorts. [3] Thus, a study on the comparison of CHD risk between Korean and Japanese populations in the post WWII birth cohorts may provide a powerful epidemiological tool for understanding the different trends in CHD mortality.
Carotid intima-media thickness (IMT) is a surrogate marker of general atherosclerosis. [6] Increased carotid IMT is positively associated with coronary risk factors [7, 8] and future cardiovascular events.[9] We have previously reported the difference in carotid IMT among men in the post WWII birth cohort between Japan and the U.S.[10] However, few studies have evaluated levels of carotid IMT in different ethnic cohorts of Asian populations. The purpose of the study is to determine whether there is a significant difference in levels of carotid IMT between Korean and Japanese men aged 40–49 years from population-based samples.
Methods
Subjects
Participants were population-based samples of 352 randomly-selected men aged 40–49: 102 Koreans in Ansan City, Gyeonggi-do, Korea and 250 Japanese in Kusatsu City, Shiga, Japan. Exclusion criteria were 1) clinical cardiovascular disease, 2) type I diabetes, 3) cancer except skin cancer in the past two years, 4) renal failure, and 5) genetic familial hyperlipidemias. All exclusion criteria were self-reported.
The 102 Koreans were randomly selected from the Korean Health and Genome Study (KHGS), an ongoing population-based prospective cohort study. [11] The target population was all non-institutionalized residents aged 40–69 of Ansan City, Gyeonggi-Do, Korea. By using the telephone directory of Ansan City, the KHGS randomly selected 5,020 participants, who had three consecutive cohorts (at the end of year 2002, 2004 and 2006). For this study, using the Ansan cohort in year 2004, we adopted a stratified random sampling by 2-year interval age groups (i.e. 40–41, 42–43, 44–45, 46–47, and 48–49), each including about 20 individuals. After extracting a list of 1,375 men aged 40–49, we contacted them at each age group by phone in randomly generated order. After 192 calls, 92 subjects took part in this study. The response rate was approximately 50%. Since the KHGS had an insufficient number of subjects aged 40–41 in 2004, we additionally enrolled 10 volunteers in the community.
The 250 Japanese men who resided in Kusatsu City, Shiga, Japan, were randomly selected from the Basic Residents' Register during 2003 – 2004.[10] Each selected man was mailed an invitation to the study to determine his willingness to participation. The response rate was approximately 50%.
Informed consent was obtained from all participants. The study was approved by the Institutional Review Boards of Korea University (in Seoul, Korea), Shiga University of Medical Science (in Otsu, Japan), and the University of Pittsburgh (in Pittsburgh, Pennsylvania, U.S.).
Carotid IMT
A Titan (Sonosite) high-resolution ultrasound system with a 10.5 MHz linear array was used at the Korean site. A Toshiba 140A scanner equipped with a 7.5 MHz-linear-array imaging probe was used at the Japanese site. For the common carotid arteries, both near and far walls were examined approximately 1 cm proximal to the bulb; for the bulb and internal carotid arteries, only far walls were examined. The digitally stored scans were then analyzed by trained readers, at the Ultrasound Research Laboratory of the University of Pittsburgh, who were blind to the details of the study subjects. The IMT scores from each location in right and left sides were averaged to produce an overall score. The IMT scores were highly reproducible, demonstrating the estimate of correlations between scans performed by different readers (inter-reader reliability) was 0.99.[12]
In order to reduce an observer bias and to assure the scanning quality,[12] sonographers of both sites were given 3-day training sessions for carotid scanning by a sonographer at the Ultrasound Research Laboratory of the University of Pittsburgh and the quality of the scanning was continuously monitored.
Coronary risk factors
Physical examinations and questionnaires were standardized between the two research sites. Body mass index (BMI) was calculated using body weight and height (kg/m2). Waist circumference was measured at the level of the umbilicus while a participant was standing erect. Blood pressure was measured on the right arm in the seating position after a 5-minute rest with the bladder emptied, by using an automated sphygmomanometer (BP-8800, Colin Medical Technology, Komaki, Japan). An average of two measurements was used.
Venipuncture was performed early in a clinic visit after a 12-hour fast. All blood samples obtained at each research site were shipped on dry ice to the University of Pittsburgh after stored at −80 °C. Biochemical measurements of the blood samples were centralized at the Heinz Laboratory of the University of Pittsburgh. Serum lipids were determined with the standardized methods according to the Centers for Disease Control and Prevention, including total cholesterol (TC), low-density-lipoprotein cholesterol (LDL-C), high-density-lipoprotein cholesterol (HDL-C), and triglycerides.[13] Serum fasting glucose was determined by a hexokinasẽglucose-6-phosphate-dehydrogenase-enzymatic assay; serum fasting insulin by a radio-immuno assay (Linco Research Inc., St. Charles, Missouri).
Data for smoking were collected with categories of non-, past- and current smoker. Current smokers were defined as cigarette smokers over the last 30 days. Pack-years of smoking were calculated as years of smoking multiplied by number of cigarettes smoked per day divided by 20. Alcohol drinkers were defined as those who drank alcohol two days per week or more. Ethanol consumption (g/day) was estimated, assuming that concentrations of alcohol were 5% for beer, 12% for wine, 40% for liquor, 16% for soju (Korean rice wine), and 16% for sake (Japanese rice wine). Hypertension was defined as systolic blood pressure ≥ 140 mmHg, diastolic blood pressure ≥ 90 mmHg, or use of antihypertensive medications. Diabetes mellitus (type II) was defined as a serum fasting glucose level ≥ 126 mg/dL or use of diabetic medications. Education years were also collected. Prevalence of metabolic syndrome was assessed as having three or more components among the criteria proposed by the National Cholesterol Education Program (NCEP) Adult Treatment Panel III (ATP III).[14]
Statistical analyses
To compare coronary risk factors between the two populations, a t-test or Wilcoxon rank sum test for continuous variables and the chi-square test or Fisher’s exact test for dichotomous variables were used. To examine associations of carotid IMT with coronary risk factors within each population, Pearson (r) or Spearman (ρ) correlation coefficients for continuous variables and regression coefficients (β) of the linear regression for dichotomous or ordinal variables were obtained. Two dummy variables for smoking (past and current) were designed and a p-value for smoking was obtained by p-for-trend test.
To examine an independent association between ethnicity (Korean or Japanese) and carotid IMT, the linear regression model was conducted by adjustment for potential confounders in four steps of modeling (crude, model I, II, and III,) where adjusted-means of carotid IMT for the two populations were calculated. Ethnicity was entered to calculate the crude means of IMT in both populations. Traditional risk factors (age, BMI, DBP, LDL-C, TC/HDL-C ratio, log-transformed TG, glucose, insulin, and pack-years of smoking) were entered in Model I, followed by metabolic syndrome and ethanol consumption in model II, and by other risk factors (education years, hypertension, diabetes, and use of lipid lowering medications) in model III.
All p-values were two-tailed. A P-value of <.05 was considered as significant. STATA 9.0 (StataCorp LP, College Station, Texas, USA) was used for all statistical analyses.
Results
The Korean men had more favorable features than the Japanese men in TC, LDL-C, fasting glucose, smoking, and pack years of smoking; similar features in age, SBP, triglycerides, TC/HDL-C ratio, ethanol consumption, hypertension, diabetes, and use of lipid-lowering medications (Table 1). However, the Korean men had less favorable features in BMI, DBP, HDL-C, and fasting insulin.
Table 1.
Coronary risk factors between Korean and Japanese men
| Korean (n=102) | Japanese (n=250) | P-value | |
|---|---|---|---|
| Age (years) | 44.8±2.8 | 45.2±2.8 | .283 |
| BMI (kg/m2) | 24.6±2.5 | 23.8±3.1 | .001 |
| Waist circumference (cm) | 84.2±7.2 | 85.3±8.3 | .421 |
| SBP (mmHg) | 123.8±15.0 | 125.1±16.4 | .601 |
| DBP (mmHg) | 80.0±11.5 | 76.5±11.9 | .006 |
| TC (mg/dL) | 182.0±27.6 | 218.5±36.3 | <.001 |
| LDL-C (mg/dL) | 111.3±27.2 | 134.1±35.5 | <.001 |
| HDL-C (mg/dL) | 41.9±9.3 | 53.6±12.9 | <.001 |
| TG (mg/dL) | 122.5 (92–173) | 137.5 (104–181) | .124 |
| TC/HDL-C ratio | 4.5±1.1 | 4.3±1.3 | .117 |
| Fasting glucose (mg/dL) | 100.0±12.2 | 105.9±16.0 | <.001 |
| Fasting insulin (µIU/mL) | 11.5±4.8 | 10.4±4.5 | .026 |
| Education (years) | 13.3±.3 | 14.3±.1 | .001 |
| Metabolic syndrome, yes (%) | 14.7 | 12.8 | .633 |
| Smoking | .009 | ||
| Current, yes (%) | 33.3 | 49.2 | |
| Past, yes (%) | 34.0 | 38.2 | |
| Pack-years of smoking | 10.3 (0–23) | 18.9 (3–30) | .003 |
| Alcohol drinking, yes (%) | 38.0 | 66.8 | >.999 |
| Ethanol consumption (g/day) | 10.0 (1.8–71.4) | 14.3 (2.0–42.5) | .184 |
| Hypertension, yes (%) | 21.6 | 26.4 | .416 |
| Diabetes mellitus, yes (%) | 3.9 | 4.8 | >.999 |
| Lipid lowering medication, yes (%) | 2.0 | 3.2 | .730 |
Abbreviation: BMI, body-mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; HDL-C, high-density-lipoprotein cholesterol; LDL-C, low-density-lipoprotein cholesterol; TG, triglycerides
Values are expressed as mean and standard deviation (SD) or median and inter-quartile range for continuous variables.
Metabolic syndrome denotes > three risk factors defined by NCEP-ATP III
Alcohol drinking denotes > two times of alcohol drinking per week
For continuous variables, a t-test or Wilconxon rank sum test was performed; for dichotomous variables, the chi-square test or Fisher’s exact test
The Korean men had significantly positive associations of carotid IMT with age, TC, systolic and diastolic BP, and prevalence of metabolic syndrome. The Japanese men had significantly positive associations of the carotid IMT with age, BMI, systolic and diastolic BP, LDL-C, TC /HDL-C ratio, fasting glucose, prevalence of metabolic syndrome, hypertension and diabetes (Table 2).
Table 2.
Associations between carotid IMT and coronary risk factors within each population
| Korean (n=102) | Japanese (n=250) | |
|---|---|---|
| Age (years) | .34*** | .25*** |
| BMI (kg/m2) | .11 | .32*** |
| Waist circumference (cm) | .11 | .26*** |
| SBP (mmHg) | .24* | .19** |
| DBP (mmHg) | .29** | .17** |
| TC (mg/dL) | .24* | .12 |
| LDL-C (mg/dL) | .15 | .16* |
| HDL-C (mmol/L) | .03 | −.12 |
| TG (mmol/L) | .03 | .01 |
| TC/HDL-C ratio | .12 | .19** |
| Fasting glucose (mg/dL) | .14 | .19** |
| Fasting insulin (µIU/mL) | −.01 | .04 |
| Pack-years of smoking (years) | <−.001 | .05 |
| Ethanol consumption (g/day) | .05 | −.01 |
| Education (years) | −.05 | −.04 |
| Metabolic syndrome, yes | .07* | .03** |
| Smoking | ||
| Current, yes | −.02 | .01 |
| Past, yes | .02 | .01 |
| Alcohol drinking, yes | .01 | −.01 |
| Hypertension, yes | .04 | .02* |
| Diabetes mellitus, yes | −.01 | .05* |
| Lipid lowering medication, yes | .06 | <.01 |
p <.001,
p<.01,
p<.05
Pearson (r) or Spearman (rho) correlation coefficients for continuous variables; regression coefficients (β) for dichotomous or ordinal variables (two dummy variables for smoking were designed [current and past] and a p-value was obtained by using p-for-trend test)
Abbreviation as Table 1.
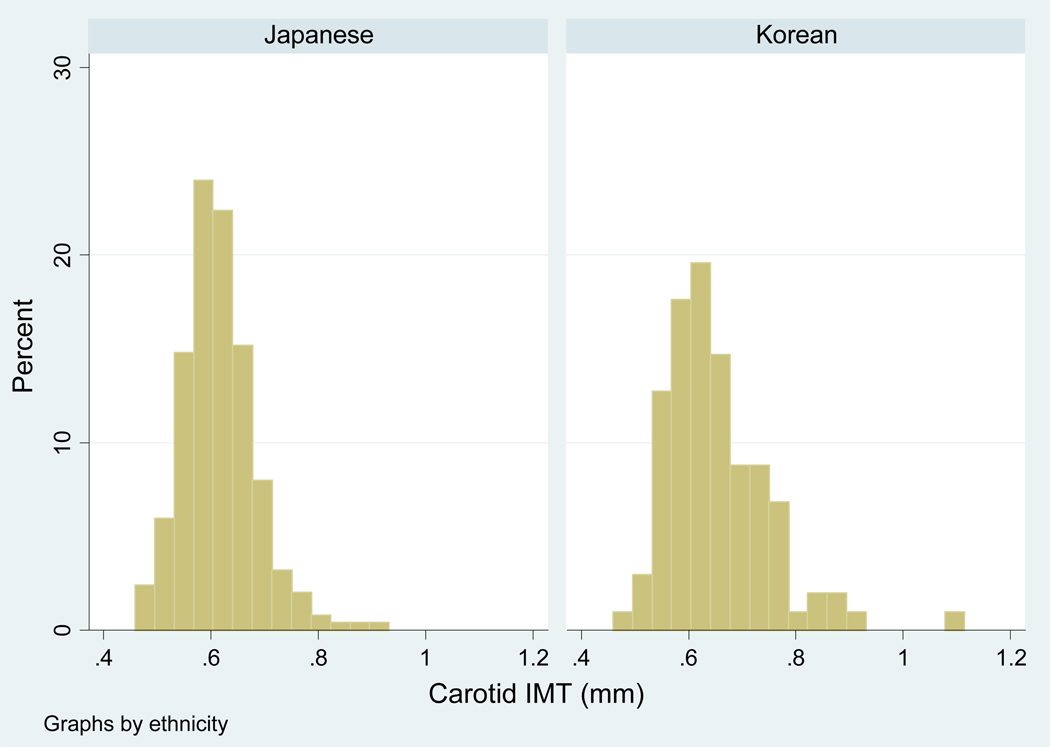
The distribution of carotid IMT was near-normal both in the Korean and Japanese men (Figure 1). The crude IMT was significantly greater in the Korean men than in the Japanese men (Table 3); the difference in the crude IMT was .039 mm. After adjusting for age, BMI, DBP, TC/HDL-C ratio, LDL-C, log-transformed TG, glucose, insulin, and pack-years of smoking (model I), the significant difference remained in the IMT. Further adjusting for metabolic syndrome and ethanol consumption (model II) and further adjusting for other factors (model III) did not alter the result.
Figure 1.
Distribution of carotid IMT scores by ethnicity
IMT, intima media thickness
Table 3.
Multivariate-adjusted mean of carotid IMT between Korean and Japanese men
| Korean (n=102) |
Japanese (n=250) |
||||
|---|---|---|---|---|---|
| Mean (SE) | 95% CI | Mean (SE) | 95% CI | P-value | |
| Crude | .655(.008) | .640–.670 | .616 (.005) | .606–.625 | <.0001 |
| Model I | .654 (.008) | .638–.670 | .616 (.005) | .607–.626 | <.0001 |
| Model II | .654 (.008) | .638–.670 | .616 (.005) | .607–.626 | <.0001 |
| Model III | .654 (.008) | .638–.671 | .616 (.005) | .607–.626 | <.0001 |
Mean (SE), mean and standard error; IMT, intima-media thickness; CI, confidence interval
Model I: adjusted for age, BMI, DBP, TC/HDL ratio, LDL-C, logTG, glucose, insulin, and pack-years of smoking
Model II: further adjusted for metabolic syndrome and ethanol consumption
Model III: further adjusted for education years, hypertension, diabetes, and use of lipid lowering medications
To examine if light-to-moderate ethanol consumption explained the difference in IMT between the populations, we categorized the continuous variable of ethanol consumption into 0, >0–15, >15–30, and >30 g/day. We found no significant difference in IMT across the categories of ethanol consumption in either population; moreover, no change in the difference in IMT between populations when we placed the categorical ethanol consumption in the crude model.
Discussion
This report is the first to examine the difference in levels of carotid IMT between Koreans and the Japanese in a population-based study. We found that, among men aged 40–49 years, the levels of carotid IMT were significantly greater in the Korean men than in the Japanese men. This difference was independent of metabolic and conventional risk factors.
Since increased carotid IMT is associated with CHD incidence and recurrence,[9, 15] our results suggest that middle-aged Korean men may continue to be at more increased risk for CHD than the Japanese men at least over the near future. Increase carotid IMT is also associated with stroke incidence and mortality.[9] Our observation of significantly greater IMT levels in the Korean men than in the Japanese men may be in accordance with the fact from the vital statistics that Korean men have higher stroke mortality than the Japanese men.[16]
The Korean men had lower levels of TC, LDL-C, and HDL-C than the Japanese men. These observations were consistent to those in previous studies.[8, 17] Lower TC and LDL-C levels in Koreans may reflect relatively lower fat intake of total energy intake than those in the Japanese. Recent rapid economic growth has allowed Koreans to have an accelerating concurrent shift to westernized diet pattern, which has led to an increase in average total fat intake, from 14% of energy intake in 1986 to ≈20% in 2002[18]. The total fat intake, however, is still lower in Korea than that in Japan (23.7%).[19]
Although many coronary risk factors were associated with carotid IMT as expected in each population, some risk factors showed weaker associations with IMT in the Korean men than in the Japanese men, including SBP, BMI, LDL, fasting glucose, hypertension and diabetes. The weaker associations are likely to be due to the small sample size of the Koreans. In addition, the lack of the significant association of LDL-C with IMT in the Korean men may be due to a small variability of LDL-C level.
The significant difference in carotid IMT scores between the two populations remained after adjusting for metabolic and conventional risk factors. This finding indicates that metabolic and conventional risk factors hardly explained the higher IMT in the Korean men than in the Japanese men. Genetic factors may be unlikely to explain the difference in the carotid IMT since it has been well known that Koreans and the Japanese are genetically similar[4, 5]. It was also reported that Japanese Americans have higher IMT levels than the native Japanese or Caucasians.[20, 21] In this context, we may assume that higher carotid IMT in the Korean men than in the Japanese men may be explained by environmental factors other than factors examined in the present study.
Some epidemiological studies reported a J-shaped association between ethanol consumption and carotid atherosclerosis,[22] although conflicting results have been reported.[22–25] We did not observe a J-shaped association in either population. Furthermore, the significant difference in IMT remained after adjusting for ethanol consumption. Thus, we have no evidence that ethanol consumption is likely to explain the difference in IMT between the two populations.
Differences in fat intake quality (e.g. polyunsaturated fatty acids, omega-3 fatty acids) between two populations may contribute to the difference in carotid IMT. Koreans consume relatively less fish of 60g per day than the Japanese population who has been well known to uniquely have high fish consumption, 120g per day.[26, 27] Hino et al. reported that omega-3 fatty acids intakes (e.g. eicosapentaenoic acid [EPA] or docosahexaenoic acid [DHA]) in fish had an inverse association with carotid IMT.[28] Thus, high fish consumption, rich in EPA and DHA, may be protective against carotid atherosclerosis, which might in part explain the higher carotid IMT in Koreans than the Japanese.
The study has several limitations. First, the fact that the study population is confined to men aged 40 to 49 years may limit generalization to older individuals and women. Second, we had a relatively small sample size of Koreans (n=102) compared to the Japanese (n=250). However, the levels of coronary risk factors and carotid IMT level in Koreans were not different from those reported in other studies.[29] Third, we had limited data for socio-environmental and behavioral factors (i.e. income, lifestyle, physical activity) that may be potential confounders. The two urban cities, chosen in this study, locate within a closed geographic zone determined by longitude and latitude. However, they are fairly different by population and industry. Ansan (in Korea) located near in Seoul, is a planned urban city of over 700,000 populations with a large industrial complex; Kusatsu (in Japan), located near in Kyoto City, is a city of over 110,000 populations, developed with service industry (hotels, etc.). Finally, with regard to IMT measurement by different machines, the difference was no greater than the variation between sonographers when evaluating between-machine differences. In addition, the two machines were comparable in the image quality. Thus, we believe that the variation in measurement due to the machine is relatively small.
Our finding suggests that higher level of carotid IMT in Koreans in the post World War II birth cohort may reflect a more increase risk for CHD than the Japanese. Further research is required to explore factors explaining the variation in carotid IMT between the two populations.
Acknowledgements
This research was supported by grants from the National Heart Lung and Blood Institute (R01 HL68200), the Central Research Development at the University of Pittsburgh, the Japanese Ministry of Education, Culture, Sports, Science and Technology (B16790355 and A13307016), and the Korean Centers for Disease Control and Prevention (Government budget code 2004-347-6111-213).
List of Abbreviations
- CHD
Coronary heart disease
- IMT
Intima-media thickness
- TC
Total cholesterol
- HDL-C
High density lipoprotein cholesterol
- LDL-C
Low density lipoprotein cholesterol
- TG
Triglycerides
- BMI
Body mass index
- SBP
Systolic blood pressure
- DBP
Diastolic blood pressure
- KHGS
Korean Health and Genome Study
References
- 1.Khor GL. Cardiovascular epidemiology in the Asia-Pacific region. Asia Pac J Clin Nutr. 2001;10(2):76–80. doi: 10.1111/j.1440-6047.2001.00230.x. [DOI] [PubMed] [Google Scholar]
- 2.Ueshima H. Trends in Asia. In: Marmot M, Elliott P, editors. Coronary heart disease epidemiology from aetiology to public health. second ed. Oxford: Oxford university press; 2005. pp. 102–112. [Google Scholar]
- 3.Sekikawa A, Kuller LH, Ueshima H, Park JE, Suh I, Jee SH, et al. Coronary heart disease mortality trends in men in the post World War II birth cohorts aged 35–44 in Japan, South Korea and Taiwan compared with the United States. International journal of epidemiology. 1999 Dec;28(6):1044–1049. doi: 10.1093/ije/28.6.1044. [DOI] [PubMed] [Google Scholar]
- 4.Miller RD, Phillips MS, Jo I, Donaldson MA, Studebaker JF, Addleman N, et al. High-density single-nucleotide polymorphism maps of the human genome. Genomics. 2005 Aug;86(2):117–126. doi: 10.1016/j.ygeno.2005.04.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Akesaka T, Lee SG, Ohashi J, Bannai M, Tsuchiya N, Yoon Y, et al. Comparative study of the haplotype structure and linkage disequilibrium of chromosome 1p36.2 region in the Korean and Japanese populations. J Hum Genet. 2004;49(11):603–609. doi: 10.1007/s10038-004-0195-7. [DOI] [PubMed] [Google Scholar]
- 6.Grobbee DE, Bots ML. Carotid artery intima-media thickness as an indicator of generalized atherosclerosis. J Intern Med. 1994 Nov;236(5):567–573. doi: 10.1111/j.1365-2796.1994.tb00847.x. [DOI] [PubMed] [Google Scholar]
- 7.Tatsukawa M, Sawayama Y, Maeda N, Okada K, Furusyo N, Kashiwagi S, et al. Carotid atherosclerosis and cardiovascular risk factors: a comparison of residents of a rural area of Okinawa with residents of a typical suburban area of Fukuoka, Japan. Atherosclerosis. 2004 Feb;172(2):337–343. doi: 10.1016/j.atherosclerosis.2003.10.007. [DOI] [PubMed] [Google Scholar]
- 8.Kim CS, Kim HJ, Won YJ, Kim DJ, Kang ES, Ahn CW, et al. Normative values of carotid artery intima-media thickness in healthy Korean adults and estimation of macrovascular diseases relative risk using this data in type 2 diabetes patients. Diabetes research and clinical practice. 2006 May;72(2):183–189. doi: 10.1016/j.diabres.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 9.Lorenz MW, Markus HS, Bots ML, Rosvall M, Sitzer M. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007 Jan 30;115(4):459–467. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 10.Sekikawa A, Ueshima H, Kadowaki T, El-Saed A, Okamura T, Takamiya T, et al. Less subclinical atherosclerosis in Japanese men in Japan than in White men in the United States in the post-World War II birth cohort. American journal of epidemiology. 2007 Mar 15;165(6):617–624. doi: 10.1093/aje/kwk053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shin C, Abbott RD, Lee H, Kim J, Kimm K. Prevalence and correlates of orthostatic hypotension in middle-aged men and women in Korea: the Korean Health and Genome Study. J Hum Hypertens. 2004 Oct;18(10):717–723. doi: 10.1038/sj.jhh.1001732. [DOI] [PubMed] [Google Scholar]
- 12.Thompson T, Sutton-Tyrrell K, Wildman R. Continuous quality assessment programs can improve carotid duplex scan quality. Journal of Vascular Technology. 2001;25:33–39. [Google Scholar]
- 13.Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972;18:499–502. [PubMed] [Google Scholar]
- 14.National Cholesterol Education Program (NCEP) Expert Panel on Detection E, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III),. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation. 2002 Dec 17;106(25):3143–3421. [PubMed] [Google Scholar]
- 15.Wattanakit K, Folsom AR, Chambless LE, Nieto FJ. Risk factors for cardiovascular event recurrence in the Atherosclerosis Risk in Communities (ARIC) study. Am Heart J. 2005 Apr;149(4):606–612. doi: 10.1016/j.ahj.2004.07.019. [DOI] [PubMed] [Google Scholar]
- 16.The World Health Organization. [cited 2007];Table 1: Number of Registered Deaths. WHO Mortality Database 2007. Available from: http://www.who.int/whosis/database/mort/table1.cfm.
- 17.Shiwaku K, Hashimoto M, Kitajima K, Nogi A, Anuurad E, Enkhmaa B, et al. Triglyceride levels are ethnic-specifically associated with an index of stearoyl-CoA desaturase activity and n-3 PUFA levels in Asians. J Lipid Res. 2004 May;45(5):914–922. doi: 10.1194/jlr.M300483-JLR200. [DOI] [PubMed] [Google Scholar]
- 18.Suh I, Oh KW, Lee KH, Psaty BM, Nam CM, Kim SI, et al. Moderate dietary fat consumption as a risk factor for ischemic heart disease in a population with a low fat intake: a case-control study in Korean men. Am J Clin Nutr. 2001 Apr;73(4):722–727. doi: 10.1093/ajcn/73.4.722. [DOI] [PubMed] [Google Scholar]
- 19.Zhou BF, Stamler J, Dennis B, Moag-Stahlberg A, Okuda N, Robertson C, et al. Nutrient intakes of middle-aged men and women in China, Japan, United Kingdom, and United States in the late 1990s: the INTERMAP study. J Hum Hypertens. 2003 Sep;17(9):623–630. doi: 10.1038/sj.jhh.1001605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Watanabe H, Yamane K, Fujikawa R, Okubo M, Egusa G, Kohno N. Westernization of lifestyle markedly increases carotid intima-media wall thickness (IMT) in Japanese people. Atherosclerosis. 2003 Jan;166(1):67–72. doi: 10.1016/s0021-9150(02)00304-0. [DOI] [PubMed] [Google Scholar]
- 21.Chambless LE, Heiss G, Folsom AR, Rosamond W, Szklo M, Sharrett AR, et al. Association of coronary heart disease incidence with carotid arterial wall thickness and major risk factors: the Atherosclerosis Risk in Communities (ARIC) Study, 1987–1993. American journal of epidemiology. 1997 Sep 15;146(6):483–494. doi: 10.1093/oxfordjournals.aje.a009302. [DOI] [PubMed] [Google Scholar]
- 22.Jerrard-Dunne P, Sitzer M, Risley P, Steckel DA, Buehler A, von Kegler S, et al. Interleukin-6 promoter polymorphism modulates the effects of heavy alcohol consumption on early carotid artery atherosclerosis: the Carotid Atherosclerosis Progression Study (CAPS) Stroke; a journal of cerebral circulation. 2003 Feb;34(2):402–407. doi: 10.1161/01.str.0000053849.09308.b2. [DOI] [PubMed] [Google Scholar]
- 23.Mukamal K, Kronmal R, Mittleman M, O'Leary D, Polak J, Cushman M, et al. Alcohol consumption and carotid atherosclerosis in older adults: The Cardiovascular Health Study. Arteriosclerosis, thrombosis, and vascular biology. 2003;23:2252–2259. doi: 10.1161/01.ATV.0000101183.58453.39. [DOI] [PubMed] [Google Scholar]
- 24.Schminke U, Luedemann J, Berger K, Alte D, Mitusch R, Wood WG, et al. Association between alcohol consumption and subclinical carotid atherosclerosis: the Study of Health in Pomerania. Stroke; a journal of cerebral circulation. 2005 Aug;36(8):1746–1752. doi: 10.1161/01.STR.0000173159.65228.68. [DOI] [PubMed] [Google Scholar]
- 25.Zureik M, Gariepy J, Courbon D, Dartigues JF, Ritchie K, Tzourio C, et al. Alcohol consumption and carotid artery structure in older French adults: the Three-City Study. Stroke; a journal of cerebral circulation. 2004 Dec;35(12):2770–2775. doi: 10.1161/01.STR.0000147968.48379.c3. [DOI] [PubMed] [Google Scholar]
- 26.Ministry of Health and Welfare. National Nutrition Survey 1998. Tokyo: Daiichi Shuppan Publisher; 2000. [Google Scholar]
- 27.Ministry of Health and Welfare. In-Depth Report on 2001 National Health and Nutrition Survey – Nutrition Survey (II) Seoul: Ministry of Health and Welfare, Republic of Korea; 2003. [Google Scholar]
- 28.Hino A, Adachi H, Toyomasu K, Yoshida N, Enomoto M, Hiratsuka A, et al. Very long chain N-3 fatty acids intake and carotid atherosclerosis: an epidemiological study evaluated by ultrasonography. Atherosclerosis. 2004 Sep;176(1):145–149. doi: 10.1016/j.atherosclerosis.2004.04.020. [DOI] [PubMed] [Google Scholar]
- 29.Jeong G, Chang J, Kim S, Lee C, Kim D, Kim Y. Correlations of Atherosclerotic Risk Factors and Carotid Artery Intima-media Thickness in Healthy Subjects. Journal of Korean Society of Vascular Surgery. 2004;20(2):200–207. [Google Scholar]