Abstract
Suicide in late life is an enormous public health problem that will likely increase in severity as adults of the baby boom generation age. Data from psychological autopsy studies supplemented with recent studies of suicidal ideation and attempts point to a consistent set of risk factors for the spectrum of suicidal behaviors in late life (suicide ideation, attempts, and deaths). Clinicians should be vigilant for psychiatric illness (especially depression), physical illness, pain, functional impairment, and social disconnectedness. Recent advances in late-life suicide prevention have in common collaborative, multifaceted intervention designs. We suggest that one mechanism shared by all preventive interventions shown to reduce the incidence of late-life suicide is the promotion of connectedness. For the clinician working with older adults, our recommendation is to not only consider risk factors, such as depression, and implement appropriate treatments but to enhance social connectedness as well.
Keywords: Suicide, Suicidal ideation, Older adult, Aged, Elderly, Prevention
Introduction
Later life is characterized by greater well-being, greater meaning to life, and a better capacity to manage emotions [1]. However, in most countries around the world, suicide rates are higher for both men and women in later life than for younger age groups, and they peak in old age [2]. In the United States, older white men have dramatically elevated suicide rates compared with those of other segments of the population [3]. Thus, later life can be characterized both as a time of greater well-being and a time of greater risk of suicide. By conceptualizing a suicide death as the outcome of veering off the expected developmental trajectory due to the presence of several risk factors—and absence of protective factors—the body of research on late-life suicide can be brought together to explain this seeming paradox.
In this article, we employ a model of suicide as the end point of a developmental process [4] and integrate this model with recent theoretical and empirical advances in suicide research. We begin with a brief discussion on the epidemiology of suicide in later life, as well as a review of the most consistent and robust findings on risk factors. Next, we update the reader on recent scientific advances in the identification and elucidation of risk and protective factors for late-life suicide. Next, we describe a recently proposed theory of suicide that we posit can serve as a useful organizing framework. We then use this framework in conjunction with the notion of suicide as the result of a developmental trajectory to organize and synthesize the body of research on late-life suicide published during the past year. Finally, we conclude with our recommendations on one of the most promising targets for future prevention efforts: increasing social connectedness.
Epidemiologic Foundations
In the United States, when suicide rates are calculated as a function of age, gender, and race, the following picture emerges [3]. For both black and white women, rates steadily increase to a peak in midlife, and then steadily decrease thereafter. For black men, rates peak in both early adulthood and late life. Finally, throughout the life course, the highest rates are observed for white men; for this demographic group, rates rise with age and peak for the oldest age group (ie, ≥85 years old). Rates for a given year also should be considered in the context of the birth cohorts making up the population. The baby boom cohorts appear to have higher suicide rates compared with earlier or subsequent cohorts [5], suggesting that as baby boomers reach later life—the first in the cohort will reach 65 years of age in 2011—suicide rates in later life likely will increase. Thus, suicide in later life represents a significant public health problem that will likely grow in severity in the upcoming years. Older adults, especially older white men, are of high clinical concern compared with other demographic groups in the United States.
The presence or absence of risk and protective factors provides additional guidance for clinicians as to which patients are at elevated risk of suicide. Consistent findings have emerged from studies of older adults who have died by suicide (ie, psychological autopsy studies), indicating that psychiatric illness, especially depression; social isolation from family, friends, and the community; functional impairment; physical illness; and pain represent a constellation of risk factors that characterize older adults at greatest risk of suicide. Neurobiological factors such as serotonergic dysregulation [6]; cultural protective factors such as religious beliefs and spirituality [7]; personality, including low openness to experience [8]; and negative life events, such as family discord [9] also play a role in elevating risk and may do so by increasing the likelihood of one or more of the above-mentioned risk factors. In the following section, we review recent research findings on late-life suicide organized by these five key risk factors.
Recent Findings
Psychiatric Illness
Psychological autopsy studies indicate that psychiatric disorders are present in 85% to 90% of older adults who die by suicide [4]. Mood disorders, especially major depression, are the most common disorders among older adults who die by suicide and are present in 54% to 87% of cases [4]. Recent research has further clarified the role of psychiatric disorders in late-life suicidal behavior. One study indicated that older adults at risk of suicide immediately following an inpatient hospitalization are likely to have had a history of inpatient treatment for depressive disorders or a mood disorder diagnosis given at the last inpatient stay [10]. Recent research examining the structure of late-life depression suggests that depressive symptoms in the context of death and suicidal ideation may represent a specific subtype of late-life depression [11]. Another study examined correlates of the severity of suicidal intent among older adults who were admitted to an inpatient unit following a suicide attempt [12]. Results indicated two factors in the patients’ histories that were associated with higher levels of intent to die during the index attempt: current mood disorder diagnosis and a history of a prior suicide attempt.
Prior research demonstrated that two thirds or more of older adults who die by suicide are seen by primary care physicians within a month of their deaths, and up to one half within 1 week [13, 14]. Given that older adults most often present to busy primary care clinics, assessment tools that are quick and easy to administer are needed. Two recent studies examined the effectiveness of the Geriatric Depression Scale (GDS) in the detection of suicidal ideation, given that the GDS does not include an item specifically assessing suicidal or death ideation but is a frequently used screener for depression [15, 16•]. Taken together, results of these studies indicate that short forms of the GDS are as effective as the long form in detecting suicidal ideation, but the most effective detection strategy involves adding an item that specifically asks about the presence of suicidal thoughts. According to another research group, the five-item Brief Symptom Rating Scale, including indices of depression, anxiety, hostility, and interpersonal sensitivity, is an effective (and brief) index for determining risk of a nonlethal suicide attempt in later life [17]. The results of these three studies are relevant to the US Preventive Task Force’s current recommendations against universal screening for suicide risk in primary care [17] because the validation of screening measures represents a step toward meeting the Task Force’s criterion for effectiveness of screening [18].
Another recent report from Haw and colleagues [19] provided a review of the research on the association between dementia and suicidal behavior in later life [19]. The authors concluded that additional research is needed to clarify under which circumstances dementia diagnoses may confer risk of suicide. Specifically, evidence suggests that suicide risk may be increased soon after receiving a dementia diagnosis and that the degree of risk conferred may vary by dementia subtype.
Finally, recent research suggests that the prescription of sedative/hypnotic medications is associated with late-life suicide, independent of the psychiatric disorders for which the drugs may be prescribed [20]. These data suggest that care must be taken in the evaluation and monitoring of older adults prescribed these classes of medications.
Social Disconnectedness
A recent meta-analysis documented that the influence of social disconnectedness on risk of all-cause premature mortality is comparable to or greater than that associated with well-established risk factors such as smoking, obesity, and physical inactivity [21]. A body of literature also links several indices of social disconnectedness specifically to suicide deaths in later life, including living alone [22], loss of a spouse [23], loneliness [22], interpersonal discord [9], and low social support [24]. A recent qualitative analysis of interviews with individuals who knew an older adult who died by suicide suggested that before their deaths, these older adults were perceived as emotionally distant in their relationships [25], perhaps indicating social disconnectedness and suggesting that personality traits such as low openness to experience [8] may place older adults at risk of social disconnectedness and, consequently, suicide.
Many have documented that social disconnectedness is similarly associated with outcomes earlier in the pathway to suicide as well, including depression, suicidal ideation, and nonlethal attempts. This observation has important clinical implications because it suggests means by which to intervene earlier in the suicidal trajectory. Specifically, a recent study found that both being unmarried and living alone were associated with nonlethal suicide attempts among adults 70 years of age and older [26]. Another study found that depressed older adults with suicidal thoughts had lower levels of perceived social support and higher levels of chronic interpersonal problems compared with depressed older adults without suicidal ideation, indicating that social disconnectedness could not be attributed solely to depression and its sequelae [27]. Finally, among a sample of older adults in primary care, Golden and colleagues [28] found loneliness to be a significant contributor to depressive symptoms. Taken together, these data suggest that screening for social disconnectedness may create a point of intervention to prevent the development of the suicidal state.
Physical Illness and Pain
A body of literature has documented an association between physical illnesses and suicide risk. The risk of suicide conferred by individual illnesses in late life has been investigated for a diverse array of illnesses, including malignancies (other than skin cancer), HIV/AIDS, epilepsy, Huntington’s disease and multiple sclerosis, renal and peptic ulcer disease, heart and lung diseases, spinal cord injury, and systemic lupus erythematosus, and was found to be in the range of 1.5 to 4 times higher compared with those older adults without the illness under study [4]. Furthermore, research has shown that risk of suicide increases with the number of diagnosed illnesses [29]. A recent study extended this finding to risk of suicide attempts among depressed older adults [30]. The study found that the Cumulative Illness Rating Scale score was significantly higher among those older adults who had attempted suicide prior to admission compared with older adults admitted for other reasons. Respiratory and vascular problems were more common among those admitted for suicide attempts.
Although less research has examined the association between pain and suicide risk in older adults, available evidence suggests that pain may be a particularly important risk factor in later life, especially for men [29, 31]. In a recent study whose findings are consistent with past findings, Li and Conwell [32] found that among older adults receiving home care services, the presence of severe and uncontrolled pain elevated the risk of thoughts of self-harm in men, but not in women.
Another recent study found that cancer and central nervous system disorders, as well as proxy-reported health status (ie, as fair or poor) were significantly associated with suicide deaths [33]. However, when an index of functional impairments was added to the statistical model, health status was no longer a significant predictor, suggesting that physical illnesses may confer risk of suicide by eroding functional capacity, a topic to which we now turn.
Functional Impairment
Research is beginning to accumulate regarding the importance of considering functional capacity when assessing suicide risk. A study conducted in China found that compared with a sample of nonsuicidal older adults living in the community, older adults who had attempted or died by suicide were more functionally impaired [34]. In a study cited previously, Conwell and colleagues [33] found that deficits in instrumental activities of daily living significantly elevated risk of suicide above and beyond the risk conferred by psychiatric disorders. Furthermore, hospitalization for medical or surgical reasons as well as use of visiting nurse or home health aide services increased the risk of suicide. A recent psychological autopsy study of older adults who died by suicide suggested that functional impairments played a key role in the desire for suicide by creating perceptions of life as a burden and of the self as lacking autonomy and personal control [25, 35]. In addition, the individuals who died appeared to distrust medical providers due to fear of losing their autonomy. In contrast, the presence of perceived autonomy (as measured by an internal locus of control and self-efficacy) appears to protect against the development of suicidal ideation in the presence of functional impairments, as evidenced by results of a recent study conducted among nursing home residents [36]. Finally, another recent study suggested that functional decline may be delayed due to the presence of social connectedness [37], suggesting a role for social connectedness as a buffer against the effects of functional decline on suicide risk.
Cognitive and Neurobiological Processes
While the constellation of risk factors described above represents five key factors that have received especially consistent and/or robust empirical support, other contextual factors play a role in risk of late-life suicide. In particular, neurobiological and cognitive processes that underlie the suicidal state and/or increase the likelihood of that state occurring represent an emerging area of research. Dombrovski and colleagues [38] found that older adult suicide attempters, but not ideators, demonstrated impairments in reward/punishment learning, an aspect of decision making. The authors provided evidence that this impairment is not equivalent to a deficit in executive functioning in general. They propose that this cognitive processing deficit may indicate that older adults who attempt suicide overemphasize present reward/punishment contingencies to the exclusion of past experiences, reflecting a “myopia for the past.” Furthermore, they reported that these deficits converge with findings from postmortem studies of late-life suicide that implicate ventral prefrontal cortical regions as neural substrates of processes involved in suicidal behavior.
Another cognitive process that has been shown to be associated with suicidal behavior in younger adults is problem solving. Gibbs and colleagues [39] examined problem solving with three groups of older adults: depressed suicide attempters, depressed nonattempters, and controls. They found that relative to both comparison conditions, depressed suicide attempters reported more negative problem-solving orientations (ie, negativistic attitude toward solving problems) and greater tendencies to engage in impulsive or careless problem-solving strategies. Thus, another cognitive process that may underlie late-life suicidal behavior is an impairment in problem solving, although future research needs to examine whether the deficits are perceived and therefore indicate a form of hopelessness, or reflect cognitive or behavioral deficits in the problem-solving process.
Finally, Hwang and colleagues [40] used voxel-based morphometry techniques to examine differences in cortical and subcortical structures among three groups of older Chinese adults: individuals with late-onset major depression with a history of suicidal behavior, those with late-onset major depression without a history of suicidal behavior, and community controls. They found that the group with a history of suicidal behaviors was characterized by decreased brain volume—including gray and white matter—across several brain regions, most notably the dorsal medial prefrontal cortex. The authors posit that their data suggest that decreased brain volume across the constellation of brain regions found in their study may be a biological substrate of suicidal behavior.
Personality and Cultural Factors
Research on risk factors such as psychiatric illness and neurobiological processes must be considered within the broader context of the individual’s overall functioning, including protective factors and the influence of culture. Marty and colleagues [41] investigated coping strategies associated with resiliency against the development of suicidal ideation. Using the COPE measure of coping styles, they found that both “problem-focused” and “emotion-focused” coping were protective against suicidal ideation, while “dysfunctional coping” elevated the risk of suicidal ideation. These data suggest that in addition to assessment of risk factors such as those outlined above, risk assessments should also include protective factors that may moderate the association between risk factors (eg, psychiatric illness) and negative outcomes (eg, suicidal behavior). One such protective factor that clinicians may wish to assess is reasons for living. Edelstein and colleagues [42] published an adapted version of the Reasons for Living Scale, which was originally created for use with middle-aged adults, for use with older adults. The scale assesses reasons patients endorse for staying alive when having thoughts of suicide.
Finally, clinicians also should be aware of cultural backgrounds and societal attitudes that may have impacted their patients. A recent study by Yur’yev and colleagues [43] found that greater positive societal attitudes toward older adults were associated with lower suicide rates, suggesting that individuals’ internalization of attitudes toward older adults can function as protective or risk factors depending on whether attitudes are positive or negative.
A Theoretical Framework for Scientific Advances
We suggest that integrating research on risk and protective factors with a theoretical foundation can provide clinicians with guidance for risk assessment and intervention. In this section, we introduce a recently proposed theory of suicide, the Interpersonal Theory of Suicide [44•], as an organizing framework for material reviewed above and material on prevention that follows. The theory proposes two proximal causes of the desire for suicide—thwarted belongingness and perceived burdensomeness. Thwarted belongingness is a painful mental state that results from an unmet need to belong—a need to feel connected to others in a positive and caring way. Perceived burdensomeness involves the mental calculation, “My death is worth more than my life to others” and involves the presence of interpersonal connections that are negatively valenced and thus do not meet the need to belong. Thus, as depicted in Fig. 1, these two constructs—thwarted belongingness and perceived burdensomeness—are referred to collectively as social disconnectedness. Regarding the effect of social disconnectedness, the theory also proposes that a particularly dangerous level of suicidal desire results from the simultaneous presence of both factors. Importantly, the theory also proposes that suicidal desire is necessary but not sufficient for lethal (or near-lethal) suicidal behavior to result because, simply put, dying by suicide is not an easy thing to do. The theory proposes that suicidal desire must be accompanied by an acquired capability for suicide, which is acquired through habituation to the pain and fear involved in suicidal behavior if lethal (or near-lethal) suicidal behaviors are to result.
Fig. 1.
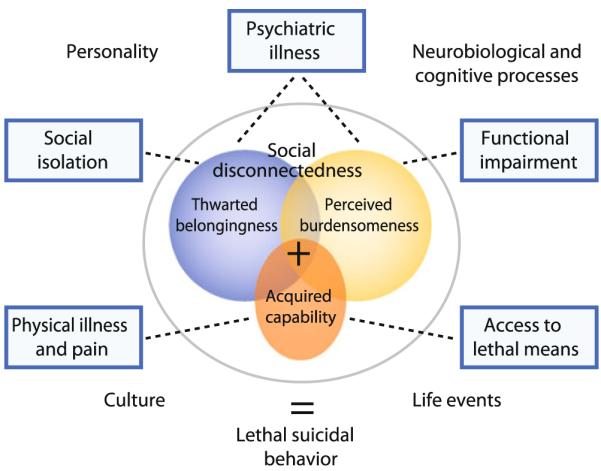
The Interpersonal Theory of Suicide applied to late life. Note that the three inner colored circles represent the three key constructs posited to cause suicide according to the Interpersonal Theory of Suicide. The five boxes represent key risk factors for late-life suicide derived from psychological autopsy studies. The dotted lines from these risk factors to one of the inner circles indicate hypothesized psychological mechanisms (derived from the Interpersonal Theory of Suicide) whereby risk factors elevate the risk of late-life suicide. All these factors and mechanisms are couched within the context of personality, neurobiology, life events, and culture
As depicted by the three inner circles in Fig. 1, the theory proposes that a relatively large number of individuals may experience thwarted belongingness or perceived burdensomeness, and a smaller number have acquired the capability for suicide. Crucially, the smaller area of overlap between thwarted belongingness and perceived burdensomeness indicates that fewer individuals will experience both states and thereby fewer will experience more severe levels of suicidal desire. Finally, the area of overlap between all three constructs is especially small, reflecting the fact that very few individuals will concurrently experience thwarted belongingness, perceived burdensomeness, and an acquired capability. Thus, according to the theory, only a very small number of people should die by suicide, although many more may have thoughts about suicide (ie, milder suicidal desire). In this way, the theory is consistent with the finding replicated worldwide and over time that only a small subset of those who think about suicide go on to attempt, and even fewer will die by suicide [45]. Research conducted on the theory thus far has been promising, especially with regard to the hypotheses regarding suicidal desire [46], although more research is needed that examines the key outcome of suicide deaths. For an in-depth discussion of the theory’s hypotheses and a review of studies testing the theory, see Van Orden et al. [44•].
A key hypothesis of the theory is depicted graphically in Fig. 1. The circle containing thwarted belongingness, perceived burdensomeness, and acquired capability represents the theory’s hypothesis that these three factors are the most proximal to the outcome of suicide. The five boxes outside the circle represent the risk factors for late-life suicide that have received consistent support from psychological autopsy studies—psychiatric illness, social isolation, functional impairment, physical illness and pain, and access to lethal means—and the diagram depicts them as causing thwarted belongingness, perceived burdensomeness, or acquired capability (ie, the dotted lines) because the theory proposes that risk factors elevate risk to the extent that they create one of these proximal causes of the suicidal state. As described above, culture, personality, neurobiological and cognitive processing, and life events may contribute to these factors; thus, those domains surround all other aspects. Figure 1 represents an application of the Interpersonal Theory of Suicide in late life. Specifically, the figure illustrates the hypotheses that psychiatric illness makes individuals vulnerable to thwarted belongingness and perceived burdensomeness (consistent with the fact that many with disorders such as major depression think about suicide but do not die by suicide). Social isolation indicates that the need to belong may be thwarted; functional impairment increases the risk of developing perceptions of burdensomeness; the experience of pain increases acquired capability (by engaging habituation to pain); and older adults’ greater planning and preparation for suicide and use of more lethal means indicate greater acquired capability for suicide.
Clinically, this hypothesis suggests that for interventions to be effective in preventing suicide in older adults, they must reduce existing levels (or prevent the incidence) of thwarted belongingness or perceived burdensomeness, or must block the expression of acquired capability (which is not posited to be amenable to intervention). Thus, the theory proposes that risk assessments need not involve assessments of all known risk factors for suicide in older adults, and interventions need not target all risk factors. Rather, effective risk assessments will involve assessment of key risk factors as well as the degree to which the risk factors create or magnify the theory’s constructs. For example, with an 85-year-old man diagnosed with depression who presents with increasing functional impairment, a clinician using the Interpersonal Theory of Suicide to inform risk assessment would inquire as to whether this man feels like a burden on others. Given that functional impairment is common in later life, whereas suicide is not, examining the psychological effect of risk factors such as functional impairment can elucidate the mechanisms whereby those risk factors may elevate risk, thereby providing a more nuanced assessment and potentially identifying a target for intervention.
Prevention: Increasing Connectedness
We previously referred to the concept of developmental trajectories, which assumes that risk of developing the suicidal state—and dying by suicide—accumulates over time, and that risk is not static or explained in a linear fashion. Rather, more distal risk factors interact with the broader context of personality, neurobiology, culture, and life events to result in proximal causes of the suicidal state. Given the lethality of suicidal behavior in late life, we advocate for intervening early in the suicidal trajectory. However, intervening too early in the trajectory could result in misallocation of resources. Thus, we suggest that interventions will be most effective and efficiently used by preventing the development of the suicidal state through the prevention or reduction of those factors most proximal to the suicidal state. Within the framework of the Interpersonal Theory of Suicide, that would mean increasing social connectedness.
The two intervention trials that have demonstrated reductions in suicide deaths in older adults included as a component ways to increase social connectedness. The Telehelp/Telecheck intervention by De Leo et al. [47] provided telephone-based outreach, evaluation, and support services. Over 11 years of service delivery, significantly fewer suicides occurred among clients than would have been expected in the older adult population of that region. Oyama and colleagues [48] published a series of five reports (recently summarized in a meta-analysis) describing the effect on late-life suicide rates in rural Japan of a multifaceted intervention that included, in addition to screening and referral for care, efforts to engage older adults in health education, volunteer, and peer support activities. They found significantly lower suicide rates in the intervention areas relative to control regions. These interventions suggest that increasing social connectedness may be a key mechanism underlying effective suicide prevention interventions.
There have been many recent advances in late-life suicide prevention, many of which we suggest involve promoting social connectedness as one mechanism of their effectiveness. First, 24-month outcomes of the PROSPECT (Prevention of Suicide in Primary Care Elderly: Collaborative Trial) trial were recently reported [49•]. The PROSPECT intervention is a collaborative care model for older adults with major or minor depression that includes depression care managers, algorithm-guided medication recommendations, and an option for patients of interpersonal psychotherapy (if medications were declined, or as an adjunct). Results indicated that the PROSPECT intervention yielded greater declines in suicidal ideation over the 2-year period compared with usual care. We suggest that in addition to improved management of depressive symptoms, the collaborative care model may be effective in reducing or preventing suicidal ideation due to its collaborative nature, which may facilitate social connectedness of patients. For example, patients were connected to depression care managers, and interactions with their primary care physicians were likely improved as a result of a shared understanding of the goal of reducing depressive symptoms. Furthermore, some patients received interpersonal psychotherapy, a behavioral intervention designed to improve interpersonal functioning, which likely increases social connectedness.
Another recent advance involves an adaptation of interpersonal psychotherapy for suicidal older adults [50]. An uncontrolled pilot study of this intervention demonstrated the acceptability, tolerability, and safety of interpersonal psychotherapy on an outpatient basis for older adults with thoughts of suicide. The key feature of the intervention focused on linking unmet interpersonal needs and interpersonal problems with the occurrence of suicidal thoughts and behaviors, and addressing these interpersonal issues to resolve suicidal states. Thus, the intervention directly focused on helping patients meet their needs to belong through the promotion of social connectedness.
Results from a 2-year follow-up to a quasi-experimental study of a community-based depression collaborative care model for older adults at risk of suicide demonstrated reductions in suicide rates for a high-risk group (ie, previous suicide attempt) who received the intervention [51]. The intervention involved enhancing standard depression treatment procedures to include community-based care management for older adults who attempted suicide, as well as the introduction of community gatekeepers. Follow-up analyses indicated that service dropout rates were significantly lower for the group of high-risk older adults who improved, suggesting that improvements may have been due to higher levels of retention in the intervention that were facilitated by connectedness to care managers and gatekeepers—again suggesting a key role for social connectedness in reducing suicide risk.
Conclusions
Suicide in late life is an enormous public health problem that will likely increase in severity as adults of the baby boom generation age. Suicide among older adults presents unique challenges to clinicians because older adults are less likely to report depressive symptoms and suicidal thoughts, are more likely to use highly lethal means, and are more likely to die on a first attempt. However, research is accumulating that can provide the practicing clinician with tools to help older patients.
First, data from psychological autopsy studies supplemented with recent studies of suicidal ideation and attempts indicate a consistent set of risk factors for the spectrum of suicidal behaviors in late life (suicide ideation, attempts, and deaths). Clinicians should be vigilant for psychiatric illness (especially depression), physical illness, pain, functional impairment, and social disconnectedness.
Clinicians may wish to use the Interpersonal Theory of Suicide as a framework for organizing the literature on risk and protective factors [52]. Doing so involves evaluating the possible psychological effects of the presence of risk factors. For example, does the patient who recently lost her husband feel completely alone and as if no one cares about her (ie, thwarted belongingness)? Does the functionally impaired male patient believe his family would be better off without him (ie, perceived burdensomeness)? Does the combat veteran who talks to his family about dying with minimal fear in his voice own a gun he might use for suicide (ie, acquired capability for suicide)? Given the imprecision of individual risk factors in the determination of risk, considering the psychological mechanisms whereby risk for the suicide state is created can inform both the severity of risk as well as means of intervention.
Recent advances in late-life suicide prevention have in common collaborative, multifaceted intervention designs. Future research is needed to dismantle these interventions and determine the key effective elements so that these elements can be disseminated and applied across diverse settings. We suggest that one mechanism shared by all preventive interventions shown to reduce late-life suicide is the promotion of connectedness. Collaborative care models, community case management, peer support, and telephone outreach all have a common thread—they connect at-risk individuals to clinicians, peers, counselors, and others who care about these individuals’ well-being. For the clinician working with older adults, our recommendation is to attend to risk factors such as depression, implement appropriate treatments, and to consider that the latest scientific advances suggest that social connections are health promoting and life saving as well.
Acknowledgment
This work was supported in part by grant no. T32MH20061 from the National Institute of Mental Health.
Footnotes
Disclosure No potential conflicts of interest relevant to this article were reported.
Contributor Information
Kimberly Van Orden, Department of Psychiatry, University of Rochester Medical Center, 300 Crittenden Boulevard, Rochester, NY 14642, USA kimberly_vanorden@urmc.rochester.edu.
Yeates Conwell, University of Rochester Medical Center, 300 Crittenden Boulevard, Rochester, NY 14642, USA.
References
Papers of particular interest, published recently, have been highlighted as:
• Of importance
- 1.Charles ST, Carstensen LL. Social and emotional aging. Annu Rev Psychol. 2010;61:383–409. doi: 10.1146/annurev.psych.093008.100448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization [Accessed February 2006];Suicide rates (per 100,000), by country, year, and gender. 2003 Available at http://www.who.int/mental_health/prevention/suicide/suiciderates/en/
- 3.Heron MP, Hoyert DL, Murphy SL, Jiaquan X, Kochanek KD, Tejada-Vera B. Deaths: final data for 2006. Natl Vital Stat Rep. 2009;57:1–135. [PubMed] [Google Scholar]
- 4.Conwell Y, Van Orden K, Caine E. Suicide in older adults. Psychiatr Clin North Am. 2011;34(2) doi: 10.1016/j.psc.2011.02.002. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Phillips JA, Robin AV, Nugent CN, Idler EL. Understanding recent changes in suicide rates among the middle-aged: period or cohort effects? Public Health Rep. 2010;125:680–8. doi: 10.1177/003335491012500510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mann JJ, Oquendo M, Underwood MD, Arango V. The neurobiology of suicide risk: a review for the clinician. J Clin Psychiatry. 1999;60(Suppl 2):7–11. [PubMed] [Google Scholar]
- 7.Nock MK, Borges G, Bromet EJ, Cha CB, Kessler RC, Lee S. Suicide and suicidal behavior. Epidemiol Rev. 2008;30:133–54. doi: 10.1093/epirev/mxn002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duberstein PR, Conwell Y, Caine ED. Age differences in the personality characteristics of suicide completers: preliminary findings from a psychological autopsy study. Psychiatr Interpers Biol Process. 1994;57:213–24. [PubMed] [Google Scholar]
- 9.Rubenowitz E, Waern M, Wilhelmson K, Allebeck P. Life events and psychosocial factors in elderly suicides–a case-control study. Psychol Med. 2001;31:1193–202. doi: 10.1017/s0033291701004457. [DOI] [PubMed] [Google Scholar]
- 10.Karvonen K, Hakko H, Koponen H, Meyer-Rochow VB, Rasanen P. Suicides among older persons in Finland and time since hospitalization discharge. Psychiatr Serv. 2009;60:390–3. doi: 10.1176/ps.2009.60.3.390. [DOI] [PubMed] [Google Scholar]
- 11.Holland JM, Schutte KK, Brennan PL, Moos RH. The structure of late-life depressive symptoms across a 20-year span: a taxometric investigation. Psychol Aging. 2010;25:142–56. doi: 10.1037/a0018514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miret M, Nuevo R, Morant C, et al. Differences between younger and older adults in the structure of suicidal intent and its correlates. Am J Geriatr Psychiatry. 2010;18(9):837–47. doi: 10.1097/JGP.0b013e3181d145b0. [DOI] [PubMed] [Google Scholar]
- 13.Luoma JB, Martin CE, Pearson JL. Contact with mental health and primary care providers before suicide: a review of the evidence. Am J Psychiatry. 2002;159:909–16. doi: 10.1176/appi.ajp.159.6.909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Conwell Y, Lyness JM, Duberstein P, et al. Completed suicide among older patients in primary care practices: a controlled study. J Am Geriatr Soc. 2000;48:23–9. doi: 10.1111/j.1532-5415.2000.tb03024.x. [DOI] [PubMed] [Google Scholar]
- 15.Cheng S-TPD, Yu, Lee, et al. The Geriatric Depression Scale as a screening tool for depression and suicide ideation: a replication and extension. Am J Geriatr Psychiatry. 2010;18:256–65. doi: 10.1097/JGP.0b013e3181bf9edd. [DOI] [PubMed] [Google Scholar]
- 16 •.Heisel MJ, Duberstein PR, Lyness JM, Feldman MD. Screening for suicide ideation among older primary care patients. J Am Board Fam Med. 2010;23:260–9. doi: 10.3122/jabfm.2010.02.080163. This article describes the accuracy of the GDS in detecting the presence of suicidal ideation among older adults in primary care. Given that most older adults who die by suicide are seen in primary care, yet universal screening is not recommended by the US Preventive Task Force due to insufficient data on the efficacy of screening tools (see Liu et al. [17]), this article addresses a topic of great importance for late-life suicide prevention.
- 17.Liu IC, Chiu CH. Case-control study of suicide attempts in the elderly. Int Psychogeriatr. 2009;21:896–902. doi: 10.1017/S1041610209990056. [DOI] [PubMed] [Google Scholar]
- 18.US Preventive Services Task Force [cited Retrieved August 30, 2010];Screening for Suicide Risk: Recommendation and Rationale. 2004 May; Available at http://www.uspreventiveservicestaskforce.org/3rduspstf/suicide/suiciderr.htm.
- 19.Haw C, Harwood D, Hawton K. Dementia and suicidal behavior: a review of the literature. Int Psychogeriatr. 2009;21:440–53. doi: 10.1017/S1041610209009065. [DOI] [PubMed] [Google Scholar]
- 20.Carlsten A, Waern M. Are sedatives and hypnotics associated with increased suicide risk of suicide in the elderly? BMC Geriatr. 2009;9:20. doi: 10.1186/1471-2318-9-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Holt-Lunstad J, Smith TB, Layton JB. Social relationships and mortality risk: a meta-analytic review. PLoS Med. 2010;7:e1000316. doi: 10.1371/journal.pmed.1000316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Waern M, Runeson BS, Allebeck P, et al. Mental disorder in elderly suicides: a case-control study. Am J Psychiatry. 2002;159:450–5. doi: 10.1176/appi.ajp.159.3.450. [DOI] [PubMed] [Google Scholar]
- 23.Conwell Y, Rotenberg M, Caine ED. Completed suicide at age 50 and over. J Am Geriatr Soc. 1990;38:640–4. doi: 10.1111/j.1532-5415.1990.tb01422.x. [DOI] [PubMed] [Google Scholar]
- 24.Turvey CL, Conwell Y, Jones MP, et al. Risk factors for late-life suicide: a prospective community-based study. Am J Geriatr Psychiatry Special Issue: Suicidal behaviors in older adults. 2002;10:398–406. [PubMed] [Google Scholar]
- 25.Kjolseth I, Ekeberg O, Steihaug S. “Why do they become vulnerable when faced with the challenges of old age?” Elderly people who committed suicide, described by those who knew them. Int Psychogeriatr. 2009;21:903–12. doi: 10.1017/S1041610209990342. [DOI] [PubMed] [Google Scholar]
- 26.Wiktorsson S, Runeson B, Skoog I, Ostling S, Waern M. Attempted suicide in the elderly: characteristics of suicide attempters 70 years and older and a general population comparison group. Am J Geriatr Psychiatry. 2010;18:57–67. doi: 10.1097/JGP.0b013e3181bd1c13. [DOI] [PubMed] [Google Scholar]
- 27.Harrison KE, Dombrovski AY, Morse JQ, et al. Alone? Perceived social support and chronic interpersonal difficulties in suicidal elders. Int Psychogeriatr. 2010;22(3):445–54. doi: 10.1017/S1041610209991463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Golden J, Conroy RM, Bruce I, et al. Loneliness, social support networks, mood and wellbeing in community-dwelling elderly. Int J Geriatr Psychiatry. 2009;24:694–700. doi: 10.1002/gps.2181. [DOI] [PubMed] [Google Scholar]
- 29.Juurlink DN, Herrmann N, Szalai JP, Kopp A, Redelmeier DA. Medical illness and the risk of suicide in the elderly. Arch Intern Med. 2004;164:1179–84. doi: 10.1001/archinte.164.11.1179. [DOI] [PubMed] [Google Scholar]
- 30.Levy T Bergman, Barak Y, Sigler M, Aizenberg D. Suicide attempts and burden of physical illness among depressed elderly inpatients. Arch Gerontol Geriatr. 2010;52:115–7. doi: 10.1016/j.archger.2010.02.012. [DOI] [PubMed] [Google Scholar]
- 31.Sirey JA, Bruce ML, Carpenter M, et al. Depressive symptoms and suicidal ideation among older adults receiving home delivered meals. Int J Geriatr Psychiatry. 2008;23:1306–11. doi: 10.1002/gps.2070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Li LW, Conwell Y. Pain and self-injury ideation in elderly men and women receiving home care. J Am Geriatr Soc. 2010;58:2160–5. doi: 10.1111/j.1532-5415.2010.03151.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Conwell Y, Duberstein PR, Hirsch JK, Conner KR, Eberly S, Caine ED. Health status and suicide in the second half of life. Int J Geriatr Psychiatry. 2010;25(4):371–9. doi: 10.1002/gps.2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Tsoh J, Chiu HF, Duberstein PR, et al. Attempted suicide in elderly Chinese persons: a multi-group, controlled study. Am J Geriatr Psychiatry. 2005;13:562–71. doi: 10.1176/appi.ajgp.13.7.562. [DOI] [PubMed] [Google Scholar]
- 35.Kjolseth I, Ekeberg O, Steihaug S. Why suicide? Elderly people who committed suicide and their experience of life in the period before their death. Int Psychogeriatr. 2010;22:209–18. doi: 10.1017/S1041610209990949. [DOI] [PubMed] [Google Scholar]
- 36.Malfent D, Wondrak T, Kapusta ND, Sonneck G. Suicidal ideation and its correlates among elderly in residential care homes. Int J Geriatr Psychiatry. 2010;25:843–9. doi: 10.1002/gps.2426. [DOI] [PubMed] [Google Scholar]
- 37.Lund R, Nilsson CJ, Avlund K. Can the higher risk of disability onset among older people who live alone be alleviated by strong social relations? A longitudinal study of non-disabled men and women. Age Ageing. 2010;39:319–26. doi: 10.1093/ageing/afq020. [DOI] [PubMed] [Google Scholar]
- 38.Dombrovski AY, Clark L, Siegle GJ, et al. Reward/punishment reversal learning in older suicide attempters. Am J Psychiatry. 2010;167:699–707. doi: 10.1176/appi.ajp.2009.09030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009;24:1396–404. doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hwang JP, Lee TW, Tsai SJ, et al. Cortical and subcortical abnormalities in late-onset depression with history of suicide attempts investigated with MRI and voxel-based morphometry. J Geriatr Psychiatry Neurol. 2010;23:171–84. doi: 10.1177/0891988710363713. [DOI] [PubMed] [Google Scholar]
- 41.Marty MA, Segal DL, Coolidge FL. Relationships among dispositional coping strategies, suicidal ideation, and protective factors against suicide in older adults. Aging Ment Health. 2010;14:1015–23. doi: 10.1080/13607863.2010.501068. [DOI] [PubMed] [Google Scholar]
- 42.Edelstein BA, Heisel MJ, McKee DR, et al. Development and psychometric evaluation of the reasons for living–older adults scale: a suicide risk assessment inventory. Gerontologist. 2009;49:736–45. doi: 10.1093/geront/gnp052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yur’yev A, Leppik L, Tooding LM, et al. Social inclusion affects elderly suicide mortality. Int Psychogeriatr. 2010;22:1337–43. doi: 10.1017/S1041610210001614. [DOI] [PubMed] [Google Scholar]
- 44 •.Van Orden KA, Witte TK, Cukrowicz KC, Braithwaite SR, Selby EA, Joiner TE., Jr The Interpersonal Theory of Suicide. Psychol Rev. 2010;117:575–600. doi: 10.1037/a0018697. This theoretical paper describes the Interpersonal Theory of Suicide in detail, including rationale for its hypotheses and empiric studies investigating these hypotheses.
- 45.World Health Organization . Primary prevention of mental, neurological and psychosocial disorders. World Health Organization; Geneva: 1998. [Google Scholar]
- 46.Van Orden KA, Witte TK, Gordon KH, Bender TW, Joiner TE. Suicidal desire and the capability for suicide: tests of the interpersonal-psychological theory of suicidal behavior among adults. J Consult Clin Psychol. 2008;76:72–83. doi: 10.1037/0022-006X.76.1.72. [DOI] [PubMed] [Google Scholar]
- 47.De Leo D, Buono M Dello, Dwyer J. Suicide among the elderly: the long-term impact of a telephone support and assessment intervention in northern Italy. Br J Psychiatry. 2002;181:226–9. doi: 10.1192/bjp.181.3.226. [DOI] [PubMed] [Google Scholar]
- 48.Oyama H, Sakashita T, Ono Y, Goto M, Fujita M, Koida J. Effect of community-based intervention using depression screening on elderly suicide risk: a meta-analysis of the evidence from Japan. Community Ment Health J. 2008;44:311–20. doi: 10.1007/s10597-008-9132-0. [DOI] [PubMed] [Google Scholar]
- 49 •.Alexopoulos GS, Reynolds CF, III, Bruce ML, et al. Reducing suicidal ideation and depression in older primary care patients: 24-month outcomes of the PROSPECT study. Am J Psychiatry. 2009 doi: 10.1176/appi.ajp.2009.08121779. doi:10.1176/appi.ajp.2009.08121779. This article describes 2-year outcomes of a collaborative care model designed to reduce suicidal ideation among older adults and represents one of the largest and most well-designed clinical trials for the prevention of late-life suicidality.
- 50.Heisel MJ, Duberstein P, Talbot NL, King DK, Tu X. Adapting interpersonal psychotherapy for older adults at risk for suicide: preliminary findings. Prof Psychol Res Pract. 2009;40:156–64. doi: 10.1037/a0014731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Chan SS, Leung VP, Tsoh J, et al. Outcomes of a two-tiered multifaceted elderly suicide prevention program in a Hong Kong Chinese community. Am J Geriatr Psychiatry. 2011;19(2):185–96. doi: 10.1097/JGP.0b013e3181e56d0f. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Joiner TE, Van Orden KA, Witte TK, Rudd MD. The Interpersonal Theory of Suicide: guidance for working with suicidal clients. American Psychological Association; Washington: 2009. [DOI] [PubMed] [Google Scholar]


