Abstract
Background
Prior studies have reached contradictory conclusions concerning whether binge eating disorder (BED) is associated with greater psychopathology in extremely obese patients who seek bariatric surgery. This study used the Structured Clinical Interview for DSM-IV Diagnoses (SCID) to compare rates of Axis I psychopathology in surgery candidates who were determined to have BED or to be currently free of eating disorders. The relationship of BED to other psychosocial functioning and weight loss goals also was examined.
Method
195 bariatric surgery patients completed the Weight and Lifestyle Inventory and the Beck Depression Inventory-II (BDI-II) and were later administered the Eating Disorder Examination. Of these 195, 44 who were diagnosed with BED, and 61 who were currently free of eating pathology, completed a telephone-administered SCID.
Results
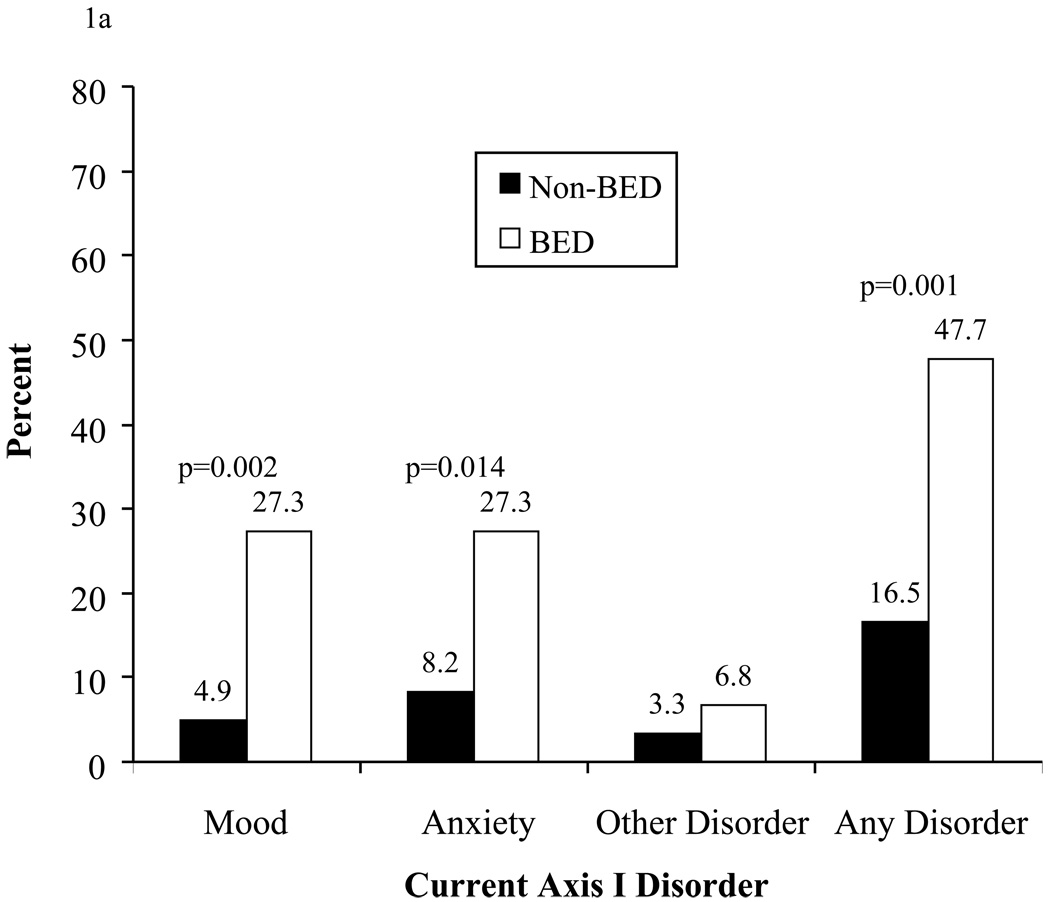
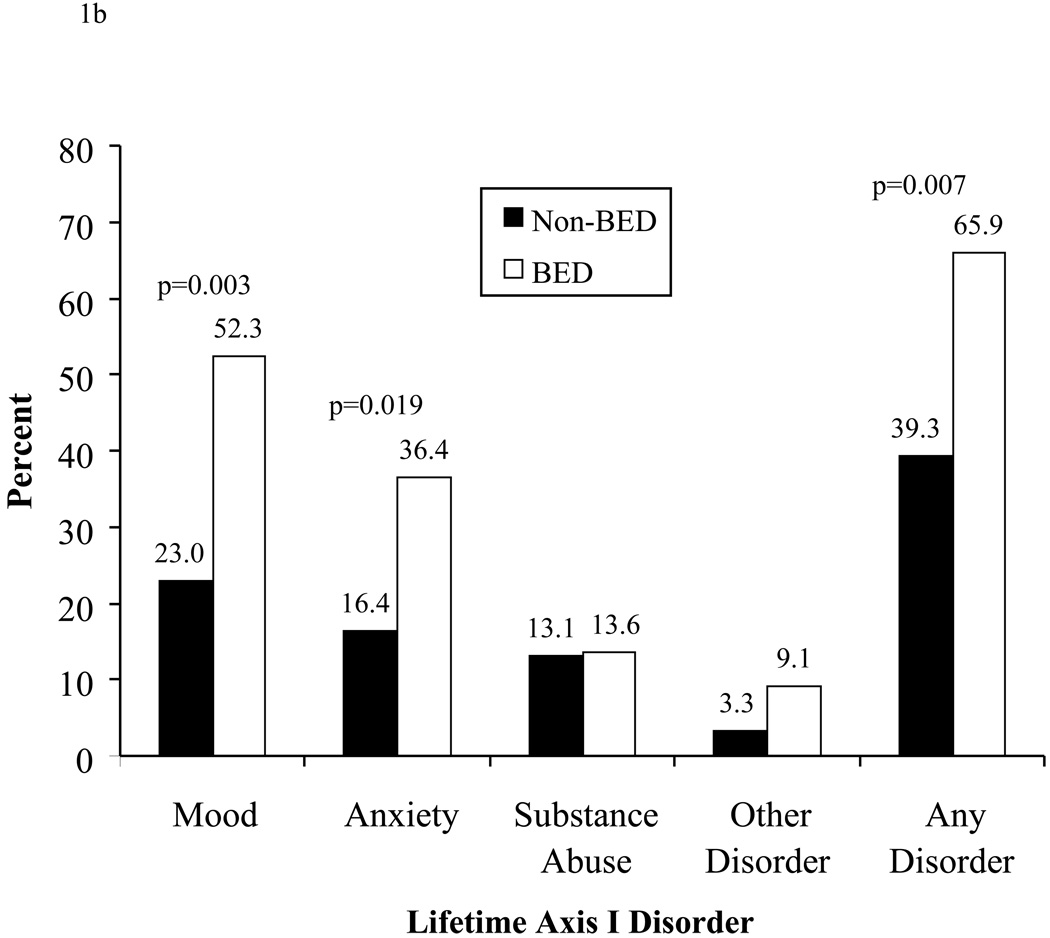
Significantly more BED than non-BED participants had a current mood disorder (27.3% vs 4.9%, p=0.002), as well as a lifetime history of this condition (52.3% vs 23.0%, p=0.003). More BED than non-BED participants also had a current anxiety disorder (27.3% vs. 8.2%, p=0.014) and lifetime anxiety disorder (36.4% vs 16.4%, p=0.019). BED also was associated with greater symptoms of depression, as measured by the BDI-II, as well as with lower self-esteem. BED and non-BED groups, however, did not differ in their desired weight loss goals following surgery.
Conclusion
The present findings indicate that the presence of BED, in patients who seek bariatric surgery, is associated with an increased prevalence of Axis I psychopathology, beyond the already elevated rate observed with severe (i.e., class III) obesity.
Keywords: obesity, binge eating disorder, Axis I disorders, psychopathology
Patients who seek bariatric surgery have high prevalence rates of psychiatric disorders [1–6]. Kalarchian and colleagues [1], for example, assessed 288 surgical candidates, using a structured clinical interview, and determined that 15.6% and 24.0% of participants were experiencing mood and anxiety disorders, respectively, at the time of evaluation. A total of 45.5% and 37.5% had a lifetime history of mood and anxiety disorders, respectively.
Bariatric surgery candidates with binge eating disorder (BED) would appear to be at the greatest risk of co-morbid psychiatric conditions [7]. BED is characterized by the consumption of an objectively large amount of food in a discrete period of time (i.e., 2 hours), with an accompanying sense of loss of control over eating and subsequent distress [8,9]. Studies of both community [10,11] and clinical samples [12–14] have reported greater psychopathology - including depression, anxiety, and substance abuse – in persons with BED than in those without this condition. By contrast, this finding has not been consistently observed in studies of severely obese patients with BED, including those seeking bariatric surgery [3,15,16]. The contradictory studies, however, included 20 or fewer patients with BED, thus, limiting power to detect differences between patient groups.
The present study was designed to improve estimates of psychopathology in bariatric surgery patients with BED by examining a larger sample of these patients and by using structured clinical interviews to determine both the presence of binge eating and Axis I psychopathology. Previous studies frequently used self-report measures to assess one or both of these dimensions [3, 17–20]. Use of the Questionnaire on Eating and Weight Patterns (QEWP) [21], for example, appears to overestimate the prevalence of BED [22], while the use alone of instruments such as the Beck Depression Inventory (BDI-II) [23] is not sufficient to diagnose major depression [24]. In the present study, we first used the Eating Disorder Examination [25], a clinician-administered interview, to establish the presence or absence of BED. A Structured Clinical Interview for DSM-IV [8] Diagnoses (SCID) [26] was then conducted to assess Axis I disorders. In addition to having greater psychopathology, we predicted that patients with BED, compared to those without, would have higher rates of physical and sexual abuse [27], lower self-esteem, happiness and weight satisfaction [28], and more unrealistic weight loss goals [29].
Method
Participants
Participants were recruited from the bariatric surgery program at the Hospital of the University of Pennsylvania from September 2005 to December 2008. Bariatric surgery candidates must have a body mass index (BMI) of 40 kg/m2 (or 35 kg/m2 in the presence of co-morbid conditions) and complete several pre-operative evaluations, including a behavioral assessment. Participants complete the BDI-II [23] and the Weight and Lifestyle Inventory (WALI) [30], at the time of the behavioral assessment, which is conducted by mental health professionals (i.e., doctoral level psychologists and a master’s level psychiatric nurse) at the Center for Weight and Eating Disorders. The WALI assesses weight and dieting histories, eating and activity habits, and psychosocial status. This instrument includes the QEWP [21], which screens for BED and other eating disorders. This study was approved by the Institutional Review Board of the University of Pennsylvania and was conducted in accordance with the Declaration of Helsinki.
Procedures
After completing the behavioral assessment, mental health professionals (i.e., clinicians) summarized their clinical findings for the candidates, answered any questions posed, provided recommendations for adjunctive psychiatric care (as needed), and indicated that they would forward a letter to the referring surgeon, who reviewed the findings of the evaluation. This concluded the behavioral assessment, as it is conducted with all surgical candidates at the Center.
Following the assessment, clinicians informed select patients that the Center was conducting a research study to compare mood, eating habits, and other behaviors in persons with and without BED who sought bariatric surgery. This information was shared with surgery candidates who, based on their responses to the QEWP, appeared either to be free of binge eating or to potentially meet criteria for BED. Candidates were informed that they were under no obligation to participate in the study. However, those who wished to learn more about the investigation were encouraged to speak with a research coordinator. Clinicians did not inform research coordinators of candidates’ provisional binge eating status, as determined by the QEWP.
Research coordinators informed potential participants of the nature and requirements of the study, answered any questions, and obtained written informed consent from interested individuals. Participants who consented then completed the Eating Disorder Examination (EDE), which was administered by trained assessors who were masked to clinicians’ provisional BED diagnoses. The EDE uses a structured clinical interview to assess participants’ eating-related attitudes and behaviors and yields diagnoses for the major eating disorders. The EDE has excellent reliability when administered by trained examiners [31].
In the present study, we were interested principally in assessing the occurrence of objective binge eating episodes. Such episodes refer to eating a large amount of food (as judged by the examiner) during a discrete period of time (i.e., a 2-hour period), with the patients’ report of loss of control during the episode [8]. The EDE initially queries respondents about their eating behavior for the previous 28 days, which can be extended to the previous 3 to 6 months to obtain information needed to diagnose different disorders. Participants in this study were diagnosed with BED if they reported at least one objective binge eating episode per week for the past 3 months, met associated behavioral characteristics (including distress about their eating behavior), and were free of compensatory behaviors associated with bulimia nervosa (i.e., purging or eliminating). These frequency and duration requirements are consistent with the proposed DSM-5 criteria for the diagnosis of BED [32], and were adopted at the outset of the study based upon recommendations of an eating disorders expert (i.e., Dr. G. Terence Wilson). Studies generally have revealed no significant differences in psychopathology, treatment outcomes, and related variables in persons who engaged in binge eating only once a week versus two or more times weekly, leading experts to recommend that the frequency criterion of once or more per week be used to diagnose BED [33].
Participants in a non-BED comparison group were selected on the basis of their not reporting any objective binge eating episodes during the previous 3 months and being free of purging and other compensatory behaviors. In addition, these individuals did not report more than one objective overeating episode per week during the previous 3 months. Such episodes, as defined by Fairburn and Cooper [25], involve consuming an objectively large amount of food but without the experience of loss of control. (An example would be eating a whole pizza and reporting enjoyment of the eating, with no loss of control.) These individuals were considered to be free of a current eating disorder.
After completing the EDE, participants were scheduled for a telephone administration of the SCID to assess Axis I disorders, according to DSM-IV-TR [8] criteria. SCIDs were administered by telephone for the convenience of participants. Previous research has suggested that telephone administration of the SCID yields comparable results as face-to-face administration [34]. The SCID is designed to assess whether a particular psychiatric disorder is present currently (i.e., “current”), or has ever been present (i.e., “lifetime”). The SCID has excellent reliability and validity [35]. Assessors included a doctoral level psychologist and two bachelor’s level research assistants, all of whom were trained and supervised by a psychologist who had extensive experience in administering the SCID. Training included the review of prior video-taped administrations of the SCID, as well as the provision of on-going feedback on the results of the telephone-administered SCIDs.
Outcome Measures
Axis I disorders
The primary outcome was the prevalence of current and lifetime Axis I disorders, as determined by the SCID. Disorders in partial remission were considered current.
Symptoms of depression
In addition to assessing mood disorders with the SCID, participants completed the BDI-II, which is the most widely-used paper-and-pencil measure of depressive symptomatology [23]. Scores range from 0–63, with higher scores indicating greater symptoms of depression.
History of physical and sexual abuse
Participants responded (yes or no) to two items on the WALI that assessed whether they had ever experienced physical or sexual abuse, respectively. Test-retest agreement on these dichotomized variables was 100% [36].
Self-esteem and weight-related satisfaction
Self-esteem and satisfaction with weight and shape were assessed by items from the WALI. Self-esteem was measured by two items that assessed patients’ overall satisfaction with themselves and their perceived self-esteem compared with that of others. Items were rated on a 1-to-5 scale on which higher scores were more favorable. Three items (which employed 7-point scales) were used to assess participants’ satisfaction with their current weight, shape, and appearance. Items ranged from 1 (very dissatisfied) to 7 (very satisfied). Test-retest reliability for the five items from the WALI ranged from 0.69 to 0.83 [36].
Weight history and goals
Weight history and weight loss goals also were assessed by items from the WALI. Participants were asked to report their: 1) age of onset of overweight; 2) highest adult weight; 3) lowest adult weight (not due to illness); and 4) desired weight loss goal following surgery. The test-retest reliability of these items ranged from 0.85 to 0.95, as described previously [36,37].
Statistical Analyses
Differences between BED and non-BED groups in the occurrence of current and lifetime Axis I disorders were compared using chi square tests or Fisher’s exact test (as were differences in demographic variables, including gender and ethnicity). Analysis of variance was used to compare BED and non-BED participants on all continuously-distributed variables. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 16 [38].
Results
Participants’ Characteristics
A total of 195 surgery candidates, whom mental health professionals believed met study inclusion criteria (for BED or non-BED), were referred to the study’s research coordinators. Of these 195, 15 elected not to participate further, while the remaining 180 completed the EDE. Of these 180, 62 were determined to have BED, and 89 were determined to be free of a current eating disorder (qualifying them for the non-BED group). The remaining 29 fell in between BED and non-BED status. They either engaged in objective overeating more than once per week (thus excluding them from the “free of current eating disorders” group), or they met some but not all criteria for BED (thus excluding them from the BED group). These 29 participants were not included in the investigation. Of the 155 qualified patients, 44 with BED (67%) and 61 without BED (69%) completed the telephone-administered SCID. These 105 patients are the subject of the subsequent analyses. Table 1 presents demographic characteristics of these participants and shows that there were no significant differences between BED and non-BED participants in weight, BMI, gender, ethnicity, or level of education. There also were no significant differences on any of these variables between applicants who completed the SCID and those who did not. However, those who did not complete the SCID were significantly younger than those who completed the interview [40.1 ± 10.8 vs. 46.2 ± 10.1 yr, respectively (p< 0.01)].
Table 1.
Baseline demographic characteristics of participants with and without binge eating disorder (BED).
| Variable | Non-BED (N=61) |
BED (N=44) |
P value |
|---|---|---|---|
| Age | 44.7 ± 9.9 | 47.9 ± 10.0 | .11 |
| Weight (kg) | 140.7 ± 26.0 | 140.4 ± 23.2 | .96 |
| Height (in) | 65.7 ± 3.7 | 66.6 ± 3.2 | .19 |
| BMI (kg/m2) | 50.4 ± 7.2 | 49.1 ± 7.4 | .37 |
| Gender (Female) | 78.7% | 77.3% | .86 |
| Ethnicity | .25 | ||
| Caucasian | 72.1% | 81.8% | |
| African American | 23.0% | 18.2% | |
| Other | 4.9% | 0% | |
| Education | .67 | ||
| Some high school (HS) | 5.2% | 5.0% | |
| HS diploma | 24.1% | 35.0% | |
| Some college | 31.0% | 22.5% | |
| Bachelors | 29.3% | 27.5% | |
| Masters | 10.3% | 7.5% | |
| Doctorate | 0 | 2.5% |
Note: Values are means ± standard deviations or percentages.
Axis I Disorders
Table 2 presents differences between BED and non-BED groups in current Axis I disorders. A significantly greater percentage of BED than non-BED participants met criteria for a current Axis I diagnosis (47.7% vs. 16.5%, p=0.001) (see Figure 1). Moreover, a significantly greater percentage of persons with BED, compared to those without this disorder, had a current mood disorder (27.3% vs. 4.9%, p=0.002), as well as a current anxiety disorder (36.4% vs. 16.4%, p=0.019).
Table 2.
Prevalence of current and lifetime Axis 1 disorders.
| Disorders | No BED (N=61) |
BED (N=44) |
P value Chi/Fisher |
|---|---|---|---|
| CURRENT DISORDERS | |||
| Any Axis I Disorder, N (%)* | 10 (16.5) | 21 (47.7) | .001 |
| Mood Disorders | |||
| Any mood disorder* | 3 (4.9) | 12 (27.3) | .002 |
| Major depressive disorder | 2 (3.3) | 12 (27.3) | |
| Dysthymia | 0 (0) | 1 (2.3) | |
| Bipolar disorder I | 1 (1.6) | 0 (0.0) | |
| Anxiety Disorders | |||
| Any anxiety disorder* | 5 (8.2) | 12 (27.3) | .014 |
| Panic disorder without agoraphobia | 2 (3.3) | 1 (2.3) | |
| Panic disorder with agoraphobia | 1 (1.6) | 1 (2.3) | |
| Generalized anxiety disorder | 0 (0) | 1 (2.3) | |
| Post-traumatic stress disorder | 0 (0) | 2 (4.5) | |
| Social phobia | 0 (0) | 3 (6.8) | |
| Specific phobia | 2 (3.3) | 3 (6.8) | |
| Obsessive compulsive disorder | 0 (0) | 0 (0) | |
| Anxiety disorder NOS | 0 (0) | 2 (4.5) | |
| Substance Use Disorders | |||
| Any substance use disorder* | 0 (0) | 1 (2.3) | .42 |
| Cannabis abuse | 0 (0) | 1 (2.3) | |
| Adjustment Disorders | |||
| Any adjustment disorder* | 0 (0) | 1 (2.3) | .42 |
| Adjustment disorder with mixed anxiety and depressed mood | 0 (0) | 1 (2.3) | |
| Other Conditions | 1.00 | ||
| Bereavement | 2 (3.3) | 1 (2.3) | |
| LIFETIME DISORDERS | |||
| Any Axis I Disorder, N (%)* | 24 (39.3) | 29 (65.9) | .01 |
| Mood Disorders | |||
| Any mood disorder* | 14 (23.0) | 23 (52.3) | .003 |
| Major depressive disorder | 12 (19.7) | 23 (52.3) | |
| Dysthymic disorder | 0 (0) | 1 (2.3) | |
| Bipolar I disorder | 1 (1.6) | 0 (0) | |
| Substance induced mood disorder | 1 (1.6) | 0 (0) | |
| Anxiety Disorders | |||
| Any anxiety disorder* | 10 (16.4) | 16 (36.4) | .019 |
| Panic disorder without agoraphobia | 5 (8.2) | 4 (9.1) | |
| Panic disorder with agoraphobia | 1 (1.6) | 1 (2.3) | |
| Generalized anxiety disorder | 0 (0) | 1 (2.3) | |
| Post-traumatic stress disorder | 1 (1.6) | 4 (9.1) | |
| Social phobia | 0 (0) | 3 (6.8) | |
| Specific phobia | 2 (3.3) | 3 (6.8) | |
| Obsessive compulsive disorder | 1 (1.6) | 2 (4.5) | |
| Anxiety disorder NOS | 0 (0) | 2 (4.5) | |
| Substance Use Disorders | |||
| Any substance use disorder* | 8 (13.1) | 6 (13.6) | .94 |
| Cannabis abuse | 2 (3.3) | 1 (2.3) | |
| Cannabis dependence | 1 (1.6) | 1 (2.3) | |
| Alcohol abuse | 5 (8.2) | 2 (4.5) | |
| Alcohol dependence | 2 (3.3) | 2 (4.5) | |
| Amphetamine dependence | 1 (1.6) | 1 (2.3) | |
| Cocaine dependence | 2 (3.3) | 0 (0) | |
| Stimulant dependence | 1 (1.6) | 0 (0) | |
| Sedative/anxiolytic/hypnotic abuse | 0 (0) | 1 (2.3) | |
| Eating Disorders | |||
| Any eating disorder* | 0 (0) | 1 (2.3) | .42 |
| Anorexia nervosa | 0 (0) | 1 (2.3) | |
| Impulse Control Disorders | |||
| Any impulse control disorder* | 0 (0) | 1 (2.3) | .42 |
| Trichotillomania | 0 (0) | 1 (2.3) | |
| Adjustment Disorders | |||
| Any adjustment disorders* | 0 (0) | 1 (2.3) | .42 |
| Adjustment disorder with mixed anxiety and depressed mood | 0 (0) | 1 (2.3) | |
| Other Conditions | 1.00 | ||
| Bereavement | 2 (3.3) | 1 (2.3) |
“Any disorder” refers to the number of participants who had any disorder of the type described. Participants were only counted once for “any disorder,” even if they met diagnoses for two or more disorders within a given class, such as “mood disorders.”
Figure 1.
Figure 1a. Prevalence of current Axis I disorders in bariatric surgery candidates with (N=44) and without (N=61) binge eating disorder (BED).
Figure 1b. Prevalence of lifetime Axis I disorders in bariatric surgery candidates with (N=44) and without (N=61) binge eating disorder (BED).
Similar to current diagnoses, a significantly greater percentage of BED than non-BED participants had a lifetime history of any Axis I disorder (65.9% vs. 39.3%, p=0.007). More participants with BED, compared to those without, had histories of mood (52.3% vs. 23.0%, p=0.003) and anxiety (36.4% vs. 16.4%, p=0.019) disorders (see Figure 2).
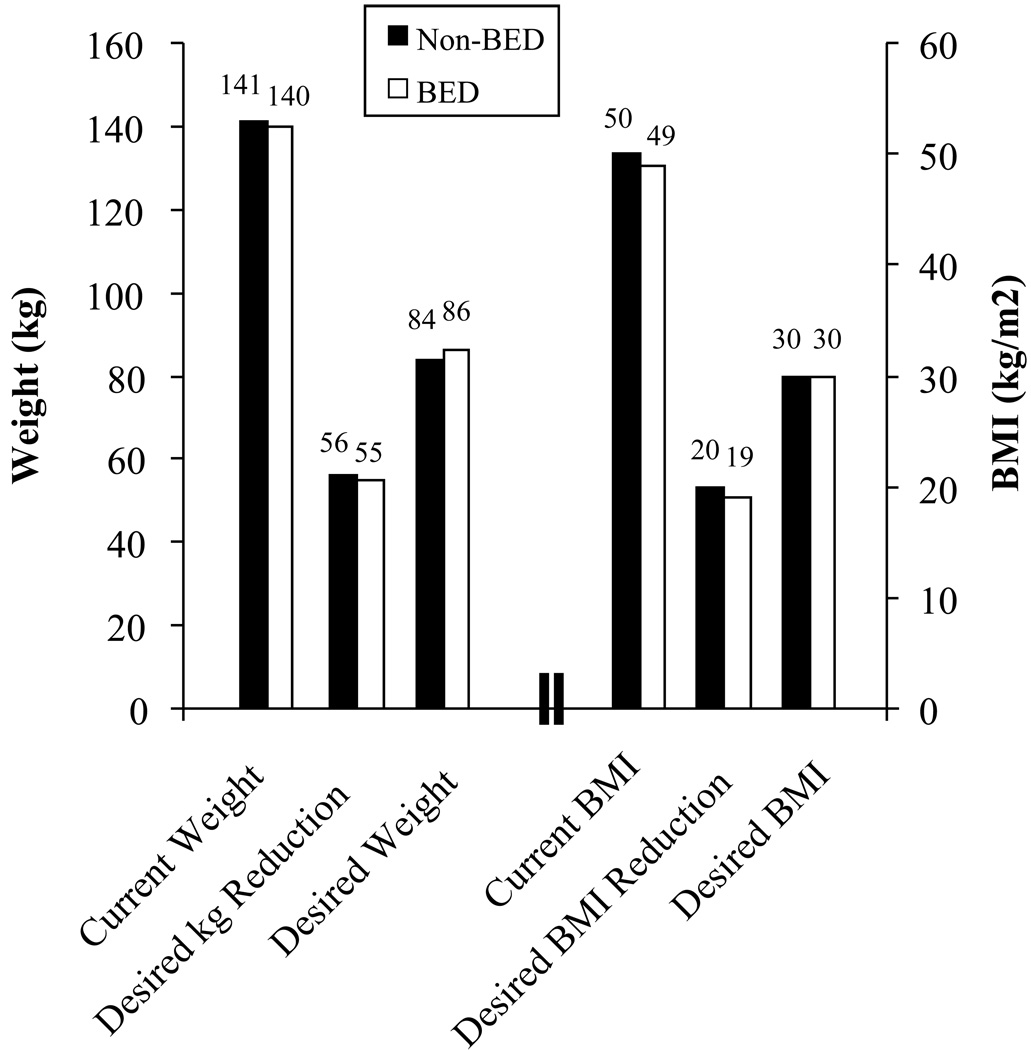
Figure 2.
Current weight/BMI, desired percent reduction, and desired weight/BMI in bariatric surgery candidates with (N=44) and without (N=61) binge eating disorder (BED). None of the comparisons between BED and non-BED participants was statistically significant (p>0.26).
In examining specific conditions, major depressive disorder and panic disorder without agoraphobia were the two most common current Axis I disorders, respectively, in both the BED and non-BED groups (see Table 2). These same disorders were also the most commonly identified lifetime Axis I disorders, respectively, followed by alcohol abuse disorder.
Depression and History of Sexual Abuse
Participants with BED reported greater symptoms of depression on the BDI-II than did their non-BED counterparts (12.7 ± 7.4 vs. 8.3 ± 6.5, p<0.001). The difference in reported sexual abuse between BED (22.2%) and non-BED (7.1%) approached significance (p=0.06). There were no significant differences between the two groups in reports of physical abuse (16.2% vs. 7.1%, p=0.19).
Self-Esteem and Weight-Related Satisfaction
As shown in Table 3, participants with BED reported lower overall happiness with themselves and lower self-esteem relative to others than did their non-BED counterparts (2.7 ± 1.3 vs. 3.5 ± 1.1 and 2.6 ± 1.0 vs. 3.6 ± 1.2, respectively; ps≤0.001). The two groups did not differ significantly (p>0.70) in their satisfaction with their current weight, shape, or overall appearance (see Table 3).
Table 3.
Patients’ responses to items that assess happiness/self-esteem and satisfaction with weight, shape, and appearance.
| Item | Non-BED N=61 |
BED N=44 |
|---|---|---|
| Happiness with self | 3.5 ± 1.1 | 2.7 ± 1.3* |
| Self-esteem compared with other people | 3.6 ± 1.2 | 2.6 ± 1.0* |
| Satisfaction with overall appearance | 1.8 ± 1.3 | 1.7 ± 1.3 |
| Satisfaction with current shape | 1.2 ± 0.7 | 1.3 ± 0.8 |
| Satisfaction with current weight | 1.1 ± 0.3 | 1.1 ± 0.4 |
Values shown are means ± standard deviations. Higher scores indicate greater happiness/self-esteem. Items 1–2 were measured on a 1 (lowest) to 5 (highest) scale, whereas items 3–5 were assessed on a 1(lowest) to 7 (highest) scale.
Groups are significantly different at p ≤ 0.001.
Weight History and Goals
BED and non-BED participants reported similar ages of onset of obesity (12.8 ± 6.6 vs. 12.3 ± 7.2 yr), as well as similar highest weights (143.2 ± 25.5 vs. 140.2 ± 32.5 kg) and lowest weights as adults (84.6 ± 23.2 vs. 88.3 ± 21.3 kg, all ps>0.45). As shown in Figure 2, both groups reported wishing to lose approximately 55 kg with bariatric surgery, equal to about a 40% reduction in initial weight. This amount of weight loss would reduce their BMIs from approximately 50 to 30 kg/m2. There were no significant differences between groups on any of these measures.
Discussion
This study’s principal finding was that, among bariatric surgery candidates determined to have BED, over 40% also were diagnosed with a current mood or anxiety disorder. The rates of these disorders were significantly higher in BED than non-BED participants. The most common current condition was major depressive disorder, diagnosed in 27% of patients with BED. BED participants also were significantly more likely than individuals without BED to have a lifetime history of mood and anxiety disorders. Major depression was again the most common mood disorder, whereas the most frequent anxiety disorders were panic disorder (without agoraphobia), post-traumatic stress disorder, social phobia, and specific phobia.
The present findings of increased psychopathology in the presence of BED, obtained using criteria for BED proposed for DSM-5, are consistent with studies of volunteers in community samples [10,11], as well as of overweight and obese individuals assessed in clinical settings [12–14]. Our findings also agree with those of Rosenberger et al [7], who evaluated Axis I disorders in 174 consecutive bariatric surgery candidates. In the 24 patients (13.8%) diagnosed with an eating disorder, 66.7% met criteria for a current Axis I diagnosis, compared with only 26.7% of those who were free of an eating disorder. Our results suggest that prior studies that failed to observe greater depression and anxiety in severely obese individuals with BED were either underpowered (potentially because of small sample sizes) or used suboptimal methods (e.g., self-report questionnaires) to diagnose BED and other psychopathology [3,15,16]. Severe obesity (i.e., class III) clearly is associated with a greater risk of major depression and other psychopathology than are lesser degrees of adiposity [39]. The presence of BED, however, appears to be associated with a further increase in this elevated risk.
The present findings do not address the question of whether BED is associated with suboptimal short- or long-term weight loss following bariatric surgery [40,41] or whether surgery candidates should receive treatment (e.g., cognitive behavioral therapy) prior to surgery to reduce problem eating [42,43]. These are critical issues that require further study. Our results, however, confirm that BED is a marker of depression, anxiety, and other psychosocial problems [27,44]. The pre-surgical psychosocial assessment provides mental health professionals an opportunity to identify and facilitate the treatment of psychiatric conditions in bariatric surgery candidates [45]. The amelioration of patient suffering - from depression, anxiety, and other conditions - is a critical objective in itself, regardless of whether the preoperative amelioration of psychopathology improves the outcome of bariatric surgery [46].
We had expected surgical candidates with BED, compared to those without, to report greater dissatisfaction with their weight, shape, and overall appearance. However, the two groups did not differ significantly on these measures, potentially because of a floor effect. Both groups reported the greatest possible dissatisfaction with their weight and shape, with average scores of 1.1 and 1.3, measured on a scale of 1 to 7, on which 1 represents very dissatisfied. This finding suggests that all surgery candidates who have a BMI of approximately 50 kg/m2 are likely to be very dissatisfied with their weight, regardless of their overall psychological functioning. There also were no significant differences between BED and non-BED groups in the amount of weight they desired to lose with surgery. Both groups wished to lose about 55 kg from a starting weight of 140 kg, equal to about a 40% reduction in initial weight. A weight loss of this magnitude only modestly exceeds the 35% mean loss that is produced by Roux-en-Y gastric bypass 18 to 24 months postoperatively [47, 48]. Both BED and non-BED participants also appeared to realize that they would remain obese after surgery. If they obtained their desired post-surgical losses, both groups were calculated to have a BMI of 30 kg/m2. These data suggest that extremely obese patients who seek gastric bypass surgery have generally reasonable weight loss goals. These goals, however, must be tempered in individuals who seek laparoscopic adjustable banding, which produces a mean loss of approximately 20% of initial weight at 2 years post-surgery [48,49].
This study’s strengths included its use of rigorous measures to identify groups of patients with and without BED, who then completed a SCID. Limitations included the inability to determine whether participants who were diagnosed with BED, but failed to complete the SCID, differed in psychopathology from those who completed the interview. In addition, the investigation may have been vulnerable to participants’ selectively underreporting some aspects of their psychiatric status because they were aware that their psychosocial fitness for bariatric surgery was being evaluated. Thus, for example, few participants reported a current substance use disorder. Fabricatore et al have described the potential for such “impression management” in bariatric surgery candidates [50]. The study also would have been strengthened by examining Axis II disorders.
In summary, this study underscores the benefit of assessing BED in patients with extreme obesity who seek bariatric surgery. This disorder can be evaluated in a non-threatening, conversational manner while inquiring about patients’ eating habits. The presence of BED would appear to signal the need for more thorough assessment of psychiatric status and the likelihood of a clinically significant mood or anxiety disorder that could be ameliorated with psychiatric care. Weight reduction alone cannot be expected to fully alleviate the suffering associated with mental health disorders.
Acknowledgments
Preparation of this manuscript was supported, in part, by National Institutes of Health grants R01-DK069652 and K24-DK065018.
References
- 1.Kalarchian MA, Marcus MD, Levine MD, et al. Psychiatric disorders among bariatric surgery candidates: Relationship to obesity and functional health status. Am J Psychiatry. 2007;164:328–334. doi: 10.1176/ajp.2007.164.2.328. [DOI] [PubMed] [Google Scholar]
- 2.Mauri M, Rucci P, Calderone A, et al. Axis I and II disorders and quality of life in bariatric surgery candidates. J Clin Psychiatry. 2008;69:295–301. doi: 10.4088/jcp.v69n0216. [DOI] [PubMed] [Google Scholar]
- 3.de Zwaan M, Mitchell JE, Howell LM, et al. Characteristics of morbidly obese patients before gastric bypass surgery. Compr Psychiatry. 2003;44:428–434. doi: 10.1016/S0010-440X(03)00092-0. [DOI] [PubMed] [Google Scholar]
- 4.Wadden TA, Sarwer DB, Fabricatore AN, et al. Psychosocial and behavioral status of patients undergoing bariatric surgery: what to expect before and after surgery. Med Clin North Am. 2007;9:451–469. doi: 10.1016/j.mcna.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 5.Sarwer DB, Wadden TA, Fabricatore AN. Psychosocial and behavioral aspects of bariatric surgery. Obes Res. 2005;13:639–648. doi: 10.1038/oby.2005.71. [DOI] [PubMed] [Google Scholar]
- 6.Zimmerman M, Francione-Witt C, Chelminski I, et al. Presurgical psychiatric evaluations of candidates for bariatric surgery, part 1: reliability and reasons for and frequency of exclusion. J Clin Psychiatry. 2007;68:1557–1562. doi: 10.4088/jcp.v68n1014. [DOI] [PubMed] [Google Scholar]
- 7.Rosenberger PH, Henderson KE, Grilo CM. Psychiatric disorder comorbidity and association with eating disorders in bariatric surgery patients: A cross-sectional study using structured interview-based diagnosis. J Clin Psychiatry. 2006;67:1080–1085. doi: 10.4088/jcp.v67n0710. [DOI] [PubMed] [Google Scholar]
- 8.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. TR. Washington, DC: 2000. [Google Scholar]
- 9.Allison KC, Wadden TA, Sarwer DB, et al. Night eating syndrome and binge eating disorder among persons seeking bariatric surgery: prevalence and related features. Obesity. 2006;14 Suppl 2:77S–82S. doi: 10.1038/oby.2006.286. [DOI] [PubMed] [Google Scholar]
- 10.Javaras KN, Pope HG, Lalonde JK. Co-occurrence of binge eating disorder with psychiatric and medical disorders. J Clin Psychiatry. 2008;69:266–273. doi: 10.4088/jcp.v69n0213. [DOI] [PubMed] [Google Scholar]
- 11.Grucza RA, Przybeck TR, Cloninger CR. Prevalence and correlates of binge eating disorder in a community sample. Compr Psychiatry. 2007;48:124–131. doi: 10.1016/j.comppsych.2006.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yanovski SZ, Nelson JE, Dubbert BK, et al. Association of binge eating disorder and psychiatric comorbidity in obese subjects. Am J Psychiatry. 1993;150:1472–1479. doi: 10.1176/ajp.150.10.1472. [DOI] [PubMed] [Google Scholar]
- 13.Specker S, de Zwaan M, Raymond N, et al. Psychopathology in subgroups of obese women with and without binge eating disorder. Compr Psychiatry. 1994;35:185–190. doi: 10.1016/0010-440x(94)90190-2. [DOI] [PubMed] [Google Scholar]
- 14.Telch CF, Stice E. Psychiatric comorbidity in women with binge eating disorder: prevalence rates from a non-treatment-seeking sample. J Consult Clin Psychol. 1998;66:768–776. doi: 10.1037//0022-006x.66.5.768. [DOI] [PubMed] [Google Scholar]
- 15.Hsu LK, Mulliken B, McDonagh B, et al. Binge eating disorder in extreme obesity. Int J Obes Relat Metab Disord. 2002;26:1398–1403. doi: 10.1038/sj.ijo.0802081. [DOI] [PubMed] [Google Scholar]
- 16.Riener R, Schindler K, Ludvik B. Psychosocial variables, eating behavior, depression, and binge eating in morbidly obese subjects. Eat Behav. 2006;7:309–314. doi: 10.1016/j.eatbeh.2005.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Sansone RA, Schumacher D, Wiederman MW, et al. The prevalence of binge eating disorder and borderline personality symptomatology among gastric surgery patients. Eat Behav. 2008;9:197–202. doi: 10.1016/j.eatbeh.2007.08.002. [DOI] [PubMed] [Google Scholar]
- 18.Saunders R. Binge eating in gastric bypass patients before surgery. Obes Surg. 1999;9:72–76. doi: 10.1381/096089299765553845. [DOI] [PubMed] [Google Scholar]
- 19.Stout AL, Applegate KL, Friedman KE, et al. Psychological correlates of obese patients seeking surgical or residential behavioral weight loss treatment. Surg Obes Relat Dis. 2007;3:369–375. doi: 10.1016/j.soard.2007.03.003. [DOI] [PubMed] [Google Scholar]
- 20.de Man Lapidoth J, Ghaderi A, Norring C. A comparison of eating disorders among patients receiving surgical vs non-surgical weight loss treatment. Obes Surg. 2008;18:715–720. doi: 10.1007/s11695-007-9250-8. [DOI] [PubMed] [Google Scholar]
- 21.Spitzer RL, Devlin M, Walsh TB, et al. Binge eating disorder: A multisite field trial of the diagnostic criteria. Int J Eat Disord. 1992;11:191–203. [Google Scholar]
- 22.Gladis MM, Wadden TA, Foster GD, et al. A comparison of two approaches to the assessment of binge eating in obesity. Int J Eat Disord. 1998;23:17–26. doi: 10.1002/(sici)1098-108x(199801)23:1<17::aid-eat3>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 23.Beck AT, Steer RA, Brown GK. Beck Depression Inventory II (BDI-II) Manual. San Antonio, TX: Harcourt Brace & Company; 1993. [Google Scholar]
- 24.Kendall PC, Hollon SD, Beck AT, et al. Issues and recommendations regarding use of the Beck Depression Inventory. Cognit Ther Res. 1987;11:288–299. [Google Scholar]
- 25.Fairburn CG, Cooper Z. The eating disorder examination. In: Fairburn CG, Wilson GT, editors. Binge Eating: Nature, Assessment, and Treatment, 12th ed. New York: Guilford Press; 1993. pp. 317–360. [Google Scholar]
- 26.First MB, Spitzer RL, Gibbon M, et al. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID) New York, NY: Biometrics Research, New York State Psychiatric Institute; 1995. [Google Scholar]
- 27.Gustafson TB, Gibbons LM, Sarwer DB, et al. History of sexual abuse among bariatric surgery candidates. Surg Obes Relat Dis. 2006;2:369–376. doi: 10.1016/j.soard.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 28.Grilo CM, Masheb RM. Correlates of body image dissatisfaction in treatment-seeking men and women with binge eating disorder. Int J Eat Disord. 2005;38:162–166. doi: 10.1002/eat.20162. [DOI] [PubMed] [Google Scholar]
- 29.Wadden TA, Womble LG, Sarwer DB, et al. Great expectations: "I'm losing 25% of my weight no matter what you say". J Consult Clin Psychol. 2003;71:1084–1089. doi: 10.1037/0022-006X.71.6.1084. [DOI] [PubMed] [Google Scholar]
- 30.Wadden TA, Foster GD. Weight and Lifestyle Inventory. Obesity. 2006;14 Suppl 2:99S–118S. doi: 10.1038/oby.2006.289. [DOI] [PubMed] [Google Scholar]
- 31.Cooper Z, Cooper P, Fairburn CG. The validity of the Eating Disorder Examination and its subscales. Brit J Psychiatry. 1989;154:807–812. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 32.American Psychiatric Association. DSM-5 Proposed Diagnostic Criteria for Binge Eating Disorder. [Accessed April 22, 2010]; http://www.dsm5.org/ProposedRevisions/Pages/proposedrevision.aspx?rid=372.
- 33.Wilson GT, Sysko R. Frequency of binge eating episodes in bulimia nervosa and binge eating disorder: Diagnostic considerations. Int J Eating Disord. 2009;42:603–610. doi: 10.1002/eat.20726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Simon GE, Revicki D, VonKorff M. Telephone assessment of depression severity. J Psychiatr Res. 1993;27:247–252. doi: 10.1016/0022-3956(93)90035-z. [DOI] [PubMed] [Google Scholar]
- 35.Lobbestael J, Leurgans M, Arntz A. Inter-rater reliability of the Structured Clinical Interview for DSM-IV Axis I Disorders (SCID I) and Axis II Disorders (SCID II) Clin Psychol Psychother. 2010 Mar 21; doi: 10.1002/cpp.693. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 36.Wadden TA, Butryn ML, Sarwer DB, et al. Comparison of psychosocial status in treatment-seeking women with class III vs. class I-II obesity. Obesity. 2006;14 Suppl 2:90S–98S. doi: 10.1038/oby.2006.288. [DOI] [PubMed] [Google Scholar]
- 37.Crerand CE, Wadden TA, Sarwer DB, et al. A comparison of weight histories in women with class III versus class I-II obesity. Obesity. 2006;14 Suppl 2:63S–69S. doi: 10.1038/oby.2006.284. [DOI] [PubMed] [Google Scholar]
- 38.SPSS for Windows, release 11.5. Chicago: SPSS Inc.; 2002. [Google Scholar]
- 39.Onyike CU, Crum RM, Lee HB, et al. Is obesity associated with major depression? Results from the Third National Health and Nutrition Examination Survey. Am J Epidemiol. 2003;158:1139–1147. doi: 10.1093/aje/kwg275. [DOI] [PubMed] [Google Scholar]
- 40.Alger-Mayer S, Rosati C, Polimeni JM, et al. Preoperative binge eating status and gastric bypass surgery: a long-term outcome study. Obes Surg. 2009;19:139–145. doi: 10.1007/s11695-008-9540-9. [DOI] [PubMed] [Google Scholar]
- 41.de Zwaan M, Hilbert A, Swan-Kremeier L. Comprehensive interview assessment of eating behavior 18–35 months after gastric bypass surgery for morbid obesity. Surg Obes Relat Dis. 2010;6:79–85. doi: 10.1016/j.soard.2009.08.011. [DOI] [PubMed] [Google Scholar]
- 42.Fabricatore AN, Crerand CE, Wadden TA, et al. How do mental health professionals evaluate candidates for bariatric surgery? Survey results. Obes Surg. 2006;16:567–573. doi: 10.1381/096089206776944986. [DOI] [PubMed] [Google Scholar]
- 43.Ashton K, Drerup M, Windover A, et al. Brief, four-session group CBT reduces binge eating behaviors among bariatric surgery candidates. Surg Obes Relat Dis. 2009;5:257–262. doi: 10.1016/j.soard.2009.01.005. [DOI] [PubMed] [Google Scholar]
- 44.Stunkard AJ, Allison KC. Binge eating disorder: disorder or marker? Int J Eat Disord. 2003;34 Suppl:S107–S116. doi: 10.1002/eat.10210. [DOI] [PubMed] [Google Scholar]
- 45.Mechanick JI, Kushner RF, Sugerman HJ, et al. American Association of Clinical Endocrinologists, The Obesity Society, and American Society for Metabolic & Bariatric Surgery medical guidelines for clinical practice for the perioperative nutritional, metabolic, and nonsurgical support of the bariatric surgery patient. Obesity. 2009;17 Suppl 1:S1–S70. doi: 10.1038/oby.2009.28. [DOI] [PubMed] [Google Scholar]
- 46.Wadden TA, Sarwer DB. Behavioral assessment of candidates for bariatric surgery: a patient-oriented approach. Obesity. 2006;14 Suppl 2:53S–62S. doi: 10.1038/oby.2006.283. [DOI] [PubMed] [Google Scholar]
- 47.Sjöström L, Narbro K, Sjöström CD, et al. Effects of bariatric surgery on mortality in Swedish obese subjects. N Engl J Med. 2007;357:741–752. doi: 10.1056/NEJMoa066254. [DOI] [PubMed] [Google Scholar]
- 48.Buchwald H, Avidor Y, Braunwald E, et al. Bariatric surgery: a systematic review and meta-analysis. JAMA. 2004;292:1724–1737. doi: 10.1001/jama.292.14.1724. [DOI] [PubMed] [Google Scholar]
- 49.O’Brien PE, Dixon JB, Laurie C, et al. Treatment of mild to moderate obesity with laparoscopic adjustable gastric banding or an intensive medical program: a randomized trial. Ann Intern Med. 2006;144:625–633. doi: 10.7326/0003-4819-144-9-200605020-00005. [DOI] [PubMed] [Google Scholar]
- 50.Fabricatore AN, Sarwer DB, Wadden TA, et al. Impression management or real change? Reports of depressive symptoms before and after the preoperative psychological evaluation for bariatric surgery. Obes Surg. 2007;17:1213–1219. doi: 10.1007/s11695-007-9204-1. [DOI] [PubMed] [Google Scholar]