Abstract
Background:
The objectives of this review were to integrate the evidence of curative effects through aquatic exercise and assess the quality of studies based on a review of nonrandomized controlled trials (nRCTs).
Methods:
Study design was a systematic review of nonrandomized controlled trials. Trials were eligible if they were nonrandomized clinical trials. Studies included one treatment group in which aquatic exercise was applied. We searched the following databases from 2000 up to July 20, 2009: MEDLINE via PubMed, CINAHL, and Ichushi-Web.
Results:
Twenty-one trials met all inclusion criteria. Languages included were English (N = 9), Japanese (N = 11), and Korean (N = 1). Target diseases were knee and/or hip osteoarthritis, poliomyelitis, chronic kidney disease, discomforts of pregnancy, cardiovascular diseases, and rotator cuff tears. Many studies on nonspecific disease (healthy participants) were included. All studies reported significant effectiveness in at least one or more outcomes. However results of evaluations with the TREND and CLEAR-NPT checklists generally showed a remarkable lack of description in the studies. Furthermore, there was the problem of heterogeneity, and we were therefore not able to perform a meta-analysis.
Conclusion:
Because there was insufficient evidence on aquatic exercise due to poor methodological and reporting quality and heterogeneity of nRCTs, we were unable to offer any conclusions about the effects of this intervention. However, we were able to identify problems with current nRCTs of aquatic exercise, and propose a strategy of strengthening study quality, stressing the importance of study feasibility as a future research agenda objective.
Keywords: aquatic exercise, systematic review, nonrandomized controlled trials
Introduction
Over the years, aquatic exercise has been known as pool therapy, hydrotherapy, and sometimes in earlier literature, as balneotherapy.1 Exercise in warm water, usually termed hydrotherapy or aquatic therapy, is a popular treatment with a pain relief effect for many patients with painful neurologic or musculoskeletal conditions.2 The warmth and buoyancy of water may block nociception by acting on thermal receptors and mechanoreceptors, thus influencing spinal segmental mechanisms.3,4 In addition, the warmth may enhance blood flow, which is thought to help in dissipating algogenic chemicals, and it may facilitate muscle relaxation. The hydrostatic effect may also relieve pain by reducing peripheral edema5 and by dampening sympathetic nervous system activity.6
Recent reports have demonstrated the effectiveness of comprehensive health education, including lifestyle education and exercise in combination with spa bathing, for male white-collar workers,7 and middle-aged and elderly people.8,9
It is well known in research design that evidence grading is highest for a systematic review (SR) with meta-analysis of randomized controlled trials (RCTs). In “the recent review (summary)10 of the SRs of RCTs”, it was reported that there were three SRs1,2,11 that included meta-analyses of RCTs on aquatic exercise. Bartels et al1 reported that aquatic exercise had some beneficial short-term effects for patients with hip and/or knee osteoarthritis. Hall et al2 reported that aquatic exercise had a small post-treatment effect in relieving pain compared with no treatment for patients with neurologic and musculoskeletal diseases, but there were no differences in pain relieving effects between aquatic and land exercise. Pittler et al11 suggested that spa exercise may be effective for treating patients with chronic low back pain. However, we did not find any SRs of RCTs in which physical (eg, cardiovascular fitness) or psychological (eg, depression) effects were the primary outcome measurements.
An RCT is initially very difficult to execute and contains etiological issues, while the design of a non-RCT (nRCT) is easy to implement compared with an RCT. Although many studies have reported the curative effects of locomotrium diseases through aquatic exercise, there have been no systematic reviews of the evidence based on nRCTs. The objective of this study was to integrate the evidence from nRCTs on the curative effects through aquatic exercise for various diseases, and to assess the quality of those trials.
Methods
Criteria for considering studies included in this study
Studies were eligible if they were nRCTs and included one treatment group in which curative aquatic exercise was applied. Any type of aquatic exercise for cure and not for sports (eg, swimming) was permitted. The use of medication, alternative therapies, or lifestyle changes was described, and had to have been comparable in the group studies. There was no restriction on language.
Search methods for identification of studies
We searched the following databases from 2000 up to July 20, 2009: MEDLINE via PubMed, CINAHL, Web of Science, and Ichushi-Web (in Japanese). The International Committee of Medical Journal Editors (ICMJE) recommended uniform requirements for manuscripts submitted to biomedical journals in 1993. We selected articles published on and after 2000 because it appeared that the ICMJE recommendation had been adopted by the relevant researchers and had strengthened the quality of reports.
All searches were performed by two specific searchers (hospital librarians) who were qualif ied in medical information handling, and who were sophisticated in clinical trial research.
Search strategies
The search strategies contained the following elements and terms for all databases:
I: Search “aquatic exercise” or “water exercise”
II: Search “water gymnastic” or “water aerobics” or “pool exercise” or “pool therapy” or “aerobic aquatics” or aquatics
III: Search “exercise therapy”[MeSH] and “water”[MeSH]
IV: Search “water-based exercise”[All Fields] or “water-based training”[All Fields] or “aquatic therapy”[All Fields] or “aquatic physical therapy”[All Fields] or “water training”[All Fields] or “water-gymnastics”[All Fields]
V: Search I or II or III or IV Limits: Publication Date from January 1, 2000 to 2009
VI: Search I or II or III or IV Limits: Publication Date from January 1, 2000 to 2009, Randomized Controlled Trial
VII: Search V not VI.
Only keywords about intervention were used for the searches. First, titles and abstracts of identified published articles were reviewed to determine the relevance of the articles. Next, references in relevant studies and identified nRCTs were screened.
2000 is the year the CONSORT Statement became available on the Internet. The CONSORT Statement was created in the mid-1990s for improving the quality of RCTs. Because of the impact of the Internet, the quality of RCTs has improved since 2000.
Reference checking, hand-searching and others
We did not check the references of included studies, perform any hand-searching, or contact any institutions, societies, or specialists known to have expertise in aquatic exercise, or authors of included studies to identify any additional published or unpublished data.
Selection of trials
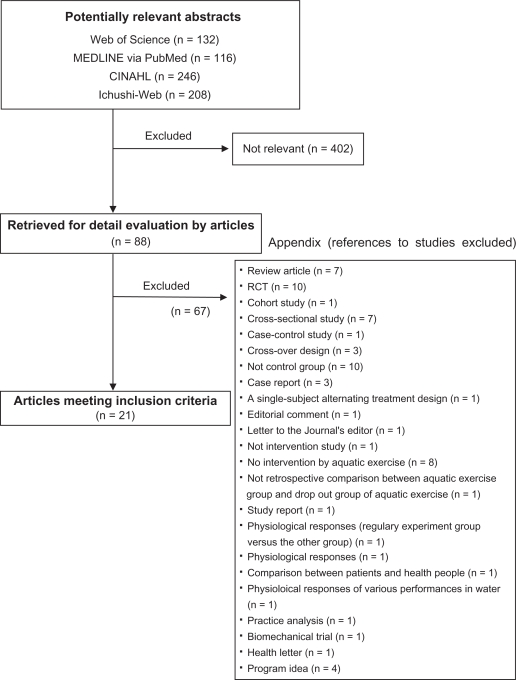
To make the final selection of studies for the review, all criteria were applied independently by two authors (JK and NS) to the full text of articles that had passed the first eligibility screening (Figure 1). Disagreements and uncertainties were resolved by discussion between the review authors.
Figure 1.
Flowchart of trial process.
Abbreviation: RCT, randomized controlled trial.
Studies were selected when 1) the design was an nRCT and 2) one of the interventions was a form of aquatic exercise. Curative effects were used as a primary outcome measure. Trials that were excluded are presented with reasons for exclusion (Appendix 1).
Quality assessment and summary of studies
To ensure that variation was not caused by systematic errors in the study design or execution, two review authors (MK and HK) independently assessed the quality of articles. A full quality appraisal of these papers was made using the TREND statement checklist12 and CLEAR-NPT checklist,13 developed to assess the methodological quality of nRCTs and nonpharmacological trials, respectively. Disagreements and uncertainties were resolved by discussion between the review authors.
For meta-analysis preparation, the target objects and main outcomes in each study were examined. We found that there were various kinds of target diseases in the studies reviewed: healthy young students, middle-aged or elderly people, or people with a certain disease. In addition, the studies were heterogeneous, and the main outcomes varied. Moreover, the quality of most studies was low according to the checklist results, and such low-quality studies were excluded from the analysis based on the Cochrane Review.1 We could not perform a meta-analysis since no variable was eligible.
One review author (HK) selected the summary from each of the structured abstracts.
Benefit, harm, and withdrawals
The GRADE Working Group14 reported that the balance between benefit and harm, quality of evidence, applicability, and the certainty of the baseline risk were all considered in judgments about the strength of recommendations. Adverse events, withdrawals, and the cost for intervention were especially important information for researchers and users of clinical practice guidelines, and we presented this information with the description of each article.
Results
Study characteristics
The literature searches included 402 potentially relevant articles (Figure 1). Abstracts from those articles were assessed and 88 papers were retrieved for further evaluation (checks for relevant literature). Sixty-seven publications were excluded because they did not meet the eligibility criteria (see Appendix 1). Twenty-one trials15–35 met all inclusion criteria (Table 1). The languages of the eligible publications were English (N = 9), Japanese (N = 11), and Korean (N = 1). Target diseases were knee and/or hip osteoarthritis,19,24,28 poliomyelitis,15 chronic kidney disease,21 discomforts of pregnancy,30 cardiovascular diseases,33 and rotator cuff tears.35 Many studies16–18,20–23,25–27,29,31,32,34 on nonspecific disease (healthy participants) were included (Table 2). All studies reported significant effectiveness in one or more outcomes. In particular, many studies reported that aquatic exercise had a significant effect on pain relief and outcome measurements for locomotor diseases.15,19,24,28,35 These intervention periods ranged from 2 weeks to 12 months. These reflected the difficulty of maintaining long-term participation in each intervention trial. Whatever the case, the long-term effects are not clear.
Table 1.
Summary of articles based on structured abstracts
| Article | Year | Title | Aim/objective | Setting/place | Participants | Detail and period of intervention | Main and secondary outcomes | Main results | Conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Willén et al15 | 2001 | Dynamic water exercise in individuals with late poliomyelitis | To evaluate the specific effects of general dynamic water exercise on individuals with late effects of poliomyelitis | A university hospital department | Twenty-eight individuals with late effects of polio, 15 (7 men, 8 women) assigned to the TG and 13 (9 men, 6 women) to the CG. The mean age was 51 years (range, 22–65 years) for the TG and 49 years (range, 28–59 years) for the CG | A 40-minute general fitness training session in warm (33°C) water twice a week. The average training period was 5 months | Peak load, peak work load, peak oxygen uptake, peak HR, muscle function in knee extensors and flexors, and pain dimension of the NHP | The exercise did not influence the peak work load, peak oxygen uptake, or muscle function in knee extensors compared with the controls. However, a decreased HR at the same individual work load was seen, as well as significantly lower distress in the dimension pain of the NHP | A program of nonswimming dynamic exercises in heated water has a positive impact on individuals with late effects of polio, with a decreased HR at exercise, less pain, and a subjective positive experience. The program was well tolerated (no adverse effects were reported) and can be recommended for this group of individuals |
| Ebisu et al16 | 2001 | Effectiveness of serum lipids on spa-walking | To examine the effect of spa walking on serum lipids | A spa pool | Spa walking group consisted of five healthy female students who did not have an exercise regime (21.3 ± 0.7 years). Nonwalking group consisted of five females who did not have an exercise regime (22.1 ± 0.2 years) | Walking in a spa pool three times a week (30 minutes at a time) for 10 weeks | Serum lipids (TC, HDL-C, LDL-C, triglycerides) and energy intake | In the exercise group, a significant increase of HDL-C was seen. A group comparison was not conducted | Spa walking can improve HDL-C value, though the detailed mechanism for HDL-C increase is unclear |
| Aoba et al17 | 2001 | The effects of enforcement water exercise class on hypotensive elderly subjects | To examine the effect of 8 weeks of water exercise on blood pressure in 133 elderly subjects | A heated pool | One hundred elderly people (29 males and 71 females, aged 59.1 ± 10.0 years) who participated in the water exercise program and 30 elderly people (17 men and 13 women, aged 57.0 ± 12.5 years) who didn’t have fitness regimes | The exercise group trained for 8 weeks with two 90-minute programs per week. Each program consisted of stretches and cool down on land, and walking, stretching, resistance training, and aerobic exercise in water | Blood pressure | In elderly subjects, significant improvements of SBP or DBP and blood pressure were shown among the subjects in the elderly group. However, obese subjects showed no significant change | The present study suggested that blood pressure value would improve with water exercise and recognition of health for elderly subjects who participated in the water exercise program |
| Yamada et al18 | 2002 | Effects of water-based well-rounded exercise on vital age and physical fitness in older adults | To determine the effects of water-based exercise training on the VA of older adults | No description | Thirty-nine volunteers were randomly divided into an exercise group (8 males and 13 females aged 69 ± 4 years) and control group (5 males and 11 females aged 68 ± 4 years) | The exercise group participated in a 12-week water-based exercise program, 70 minutes/day, and 3 days/week; the control group continued their normal lives | VA based on age and various physical fitness tests | Significant lowering in VA was noted in the exercise group, and no significant changes were observed in the control group | Water-based exercise is an effective measure to lowering VA, thus improving the overall physical fitness in the elderly |
| Murai et al19 | 2002 | Exercise therapy for osteoarthritis of the knee – preliminarily study of water exercise | To compare the effects of aquatic exercise training and land exercise on patients with slight knee OA | No description | Aquatic exercise group consisted of 16 females aged 49.7 years on average. Land exercise group consisted of 6 females aged 53.5 years on average | Once per week for 10 weeks on average. Voluntary exercise was permitted. Aquatic exercise included walking in the water, balancing exercises and cool down. Land exercise included stretching, resistance training, balancing exercises, ergometer exercise and icing | Body fat, VAS, JOA knee score, and isometric knee extension force | There was no significant difference in weight and body fat. VAS, JOA score and COP sway were significantly decreased or improved by aquatic exercise. They improved by land exercise, although not significantly. Knee extension force was improved in both groups. Significance level was higher in aquatic exercise group | Knee pain, JOA, muscle force and COP were significantly improved in the aquatic exercise group. Only muscle force was improved in land exercise group. Aquatic exercise was more effective than land exercise in patients with slight OA |
| Igarashi et al20 | 2002 | Health effect of aquatic exercise therapy using a hot spring | To examine the health effect of aquatic exercise therapy with a hot spring for people who are not athletes | A city hot spring pool | The aquatic exercise group consisted of an aquatic exercise class for 13 females for 2 years (56–70 years). The nonaquatic exercise group consisted of 7 females who did not have an exercise regime (60–75 years) | Stretching and balance training was included. 45 minutes a week for 4 months | Physical characteristics (height, weight, body fat, blood pressure), muscle volume, VO2 max, physical flexibility were examined at the beginning and end of the intervention. | In the exercise group, significant reduction of weight and minimum blood pressure were seen. A group comparison was not conducted | The intervention period (4 months) and frequency (once a week) might not be enough to improve health |
| Pechter et al21 | 2003 | Beneficial effects of water-based exercise in patients with chronic kidney disease | To ascertain whether water-based, 12-week, regular, low-intensity aerobic exercise conditioning provides beneficial effects for individuals with moderate CRF and to compare the outcome with data from a sedentary control group | No description | Twenty-six patients with moderate CRF: an exercise group (7 male and 10 females aged 31–72 years) and a control group (6 men and 3 women aged 35–65 years) | The exercise group did low-intensity aerobic exercise in the pool over a period of 12 weeks, twice a week, with sessions lasting for 30 minutes; the control group remained sedentary | Cardiorespiratory parameters (VO2 max and peak ventilation), renal functional parameters (serum creatinine, Cys-C, GFR, and U-prot), SBP and DBP, and oxidative stress indices (products of lipid peroxidation and reduced GSH | Only in the exercise group, all cardiorespiratory functional parameters, SBP, and DBP were lowered significantly. U-prot and U-prot were diminished significantly and GFR was enhanced. LPO was reduced significantly, and GSH showed significant improvement | Regular water-based exercise has beneficial effects on the cardiorespiratory, renal functional parameters, and oxidative stress status in patients with moderate renal failure, and can be used in the complex rehabilitation of chronic renal failure patients, together with blood pressure control, dietary consultation, encouragement and education to prevent physical worsening and to postpone cardiovascular and renal atherosclerotic complications. |
| Douris et al22 | 2003 | The effect of land and aquatic exercise on balance scores in older adults | To determine if aquatic exercise was more effective than land-based exercise when training balance | Aquatic: Inground Custom Therapy Pool (Longmont, CO, USA). Land; assisted living recreation area | Subjects were healthy elderly aged 65 years and older who were independent walkers with or without an assistive device and independent in activities of daily living. Land group: 83.2 ± 8.14 (73–91) years (5 subjects). Aquatic group: 75.0 ± 3.63 (68–78) years (6 subjects) | Exercise was comparable for both land and water and was administered twice a week for 6 weeks. Walking activities (3 times each): 1) walking forward 11 feet, 2) marching forward 11 feet, 3) sidestepping without crossing legs 11 feet, and 4) tandem walking 11 feet. Exercise activities (one set of 15 repetitions): 1) marching in place, 2) hip flexion/extension, 3) hip abduction/adduction, 4) toe raises/heel raises, 5) shallow knee bends, 6a) sit to stand from chair in land group, 6b) sit to stand from pool shelf in aquatic group | BBS score | There was a significant main effect of time (P < 0.001) but not group on BBS scores. There was no significant interaction between group and time | The utilization of lower body exercise, whether in water or on land, was accompanied by improved balance |
| Liquori et al23 | 2003 | Effects of a 6-week prenatal water exercise program on physiological parameters and wellbeing in women with pregnancies in the 2nd–3rd trimesters: a pilot study | To evaluate an established prenatal water aerobics program for its impact on the physiological function and wellbeing of females with low risk pregnancy in the 2nd and early 3rd trimesters | A pool in a rehabilitation center | Seven healthy females with uncomplicated singleton pregnancies participated in the exercise group (mean age 32.8 years). Six women having the same characteristics participated in the control group (mean age 30.5 years) | Participating in the 1-hour water aerobic exercise class using a pool in a rehabilitation center, 2 or 3 times a week for 6 weeks | Cooper 6-minute walk test, muscle force in the quadriceps, shoulder abductors, biceps, and triceps, and the health promoting lifestyle profile II questionnaire | Post-test measures of strength in the quadriceps and biceps, as well as the subscale of physical activity within the HPLP II questionnaire were greater in the exercise group | This study outcome supported the effect of prenatal water aerobic exercise but further research with greater number of subjects is necessary to establish the most effective protocols |
| Lin et al24 | 2004 | Community rehabilitation for older adults with osteoarthritis of the lower limb: a controlled clinical trial | To examine the effectiveness of a 12-month community-based water exercise program on measures of self-reported health and physical function in people aged over 60 years with knee-hip OA | Public community swimming pool in Sheffield, UK | One hundred and six community-dwelling sedentary older people (aged >60 years), with conformed knee-hip OA, enrolled in an experimental controlled trial for 12 months. Sixty-six subjects in the exercise group were offered a water-exercise program. Forty age-matched, nonexercising, ‘control’ subjects received monthly education material and quarterly telephone calls | Participants in the exercise group were asked to attend two exercise sessions a week of 1 hour for 12 months led by specially trained swimming instructors | The disease-specific Western Ontario, McMaster University Osteoarthritis Index (WOMAC), a battery of performance-based physical function tests | After 1 year, participants in the exercise group experienced a significant improvement in physical function (4.0 ± 9.1 versus −0.4 ± 7.3 units; 95% CI 0.96–7.96, P < 0.05) and reduction in the perception of pain (1.3 ± 3.7 versus 0.2 ± 2.5 units; 95% CI −0.19–2.52, P < 0.05) compared with the control group, as measured by the WOMAC Osteoarthritis Index. In addition, the exercise group performed significantly better in the ascending and descending stairs tests (P < 0.05), had significantly greater improvements in knee range of movement (P < 0.01) and hip range of movement (P < 0.005). There were no significant differences in the two groups for quadriceps muscle strength and psychosocial wellbeing (Arthritis Impact Measurement Scales 2 questionnaire) | Older people with knee/hip OA gained modest improvements in measures of physical function, pain, general mobility, and flexibility after participating in 12 months of community-based water exercise |
| Akamine et al25 | 2005 | Effects of underwater exercise with hot spring bathing on middle aged people | To investigate the effects of underwater exercise with hot spring bathing on middle aged people | No description | Three males and 22 females (59.6 ± 8.9 years) without serious systemic complication | Group A: (1-day intervention): underwater exercise (70 minutes) and hot spring bathing (20 minutes). Group B: (1-day intervention): underwater exercise (70 minutes) and fresh water bathing (20 minutes) Group C: no exercise, no bathing | Blood pressure, total cholesterol, CD4, red blood cells, hematocrit, total protein, and POMS | Exercise with bathing significantly lowered values of DBP, TC, CD4, red blood cells, hematocrit, and total protein when compared with the before exercise with bathing group (P < 0.05). After exercise with bathing, significantly lower levels of depression-dejection, anger-hostility and confusion in POMS test were observed when compared with control group | Underwater exercise with hot spring bathing has good effects on the health of middle aged people |
| Takumi et al26 | 2005 | Participation in an aquatic exercise class twice a week for 12 weeks improved physical fitness for good walking, walking self-efficacy on winter roads, mental health and QOL in elderly women | This study investigated whether the level of good walking, walking SE on winter roads, mental health and QOL improved through participation in an aquatic exercise class (twice a week, for 12 weeks) in elderly women | A pool with water temperature 34°C | The subjects were 15 females who took part in the aquatic exercise class and 16 females in the control group (over 60 years) | The duration of each class was 60 minutes (twice a week, for 12 weeks) and was conducted under the guidance of a skilled instructor | Good walking tests (standing on one leg with eyes open, Bosu balance score), walking SE, MHP, and QOL | Good walking tests of the final class were improved compared with the first class (P < 0.05). Walking SE on winter roads did not change in either group, but the SE scores for general falling were significantly increased at the last class compared with the first class in the exercise group (P = 0.032). The stress scores of MHP did not increase in the exercise group, which indicates that participating in the aquatic exercise class was not stressful. In QOL measures, the scores of physical symptoms (P < 0.001) and the mean of QOL (P = 0.028) was significantly improved at the last class compared with the first class in the exercise group | Participation in an aquatic exercise class is suggested to be effective for promoting good walking, QOL, and an active lifestyle |
| Takumi and Moriya27 | 2005 | Participation in an aquatic exercise class for 12 weeks improved physical fitness for good walking, walking self-efficacy on winter roads, mental health and QOL in elderly women | This study investigated whether participation in an aquatic walking class (once a week, for 12 weeks) had an effect on middle-aged and elderly women, compared with no participation | A pool with water temperature 29°C | The subjects were 35 women (58.5 ± 8.3 years) who took part in the aquatic exercise class and 24 women (61.0 ± 7.4 years) in the control group | The duration of the exercise class was 50 minutes (once a week, for 12 weeks) under the guidance of a skilled instructor. Averages of % HRR during exercise were 24%–34%, so that the intensity of exercise was lower middle level | Mood Check List- Short Form 1, good walking tests (maximal one step distance, one leg squat, Bosu balance test, 10 m walk time), walking SE | Mood Check List-Short Form 1 for pleasantness and relaxation significantly increased post-exercise compared with pre-exercise every time (P < 0.001). Good walking tests in the 12th week improved compared with those from the first week. The scores of walking SE in strong wind and on an icy surface in the 12th week were increased compared with the scores from the first week. No changes were observed in the control women group | No changes were observed in the control group |
| Lee28 | 2006 | Comparison of effects among Tai Chi exercise, aquatic exercise, and a self- help program for patients with knee osteoarthritis | To compare the effects between Tai Chi exercise, aquatic exercise, and a self-help program for knee OA patients on symptoms of arthritis, muscle strength, balance, and difficulty of programming activities | Tai Chi exercise and self-help program: public health center. Aquatic exercise: a pool | Tai Chi exercise group (N = 18: 61.3 ± 9.5 years), aquatic exercise group (N = 16: 66.4 ± 6.7 years) and self-help program group (N = 16: 61.6 ± 7.6 years) were enrolled for this study. All subjects had knee OA and did not have an exercise regime during the past 6 months | Tai Chi exercise and aquatic exercise group exercised twice a week (1 hour) for 2 months. In the self-help program group, they exercised once a week (2 hours) for 2 months | Muscle strength, balance and difficulty of performing activities (K-WOMAC Index) | The Tai Chi group was significantly different from the self-help group for knee extensor peak torque, knee flexor, and stiffness. In addition, the Tai Chi group or aquatic group were significantly different from the self-help group for difficulty of performing activities | The Tai Chi group or aquatic group were significantly different from the self-help group. However, it seems that Tai Chi exercise may be more suitable than aquatic exercise in an OA exercise program |
| Lord et al29 | 2006 | The effects of water exercise on physical functioning in older people | To determine whether a 22-week water exercise program can improve physical functioning in older people | All participants in central and eastern Sydney. The exercises were undertaken in heated pools with water temperatures that ranged between 25°C and 29°C | Eighty-five persons (18 males and 67 females, mean age 71.8 years) participated in a water-exercise program, and 44 control subjects (7 males and 37 females, mean age 76.5 years) participated in the study | The exercisers participated in approximately 1-hour exercise sessions once a week for two 10-week periods (with 2-week inter-term break). The intervention comprised the ‘WAVES’ water exercise program specifically designed for older people | Leaning balance, quadriceps strength, reaction time and shoulder range of motion | The 48 exercise subjects who were available for retest showed significantly improved leaning balance (as measured by tests of maximal balance range and coordinated stability) and shoulder range of motion compared with the controls. The groups did not differ in tests of quadriceps strength and reaction time. However, 37 people dropped out from the program because of dislike of the pool environment (N = 7), move/vacation (N = 6), hospitalization (N = 5), illness (N = 11), caring for sick spouse (N = 2), requested no second interview (N = 2), deceased (N = 1), changed to another program (N = 1), and no reason (N = 2) | These findings show that water exercise can produce benefits with regard to improving balance and flexibility in older people |
| Smith and Michel30 | 2006 | A pilot study on the effects of aquatic exercises on discomforts of pregnancy | To estimate the impact of an aquatic exercise program on the perception of body image, participation in health-promoting behaviors, barriers to health-promoting participation, level of physical discomfort, and mobility | No description | Forty nonexercising pregnant women with more than 19 weeks gestation. Based on self-selection, participants were assigned to either aquatic exercise group (N = 20: 25.1 ± 4.9 years) or control group (N = 20: 24.8 ± 5.6 years) | The aquatic exercise group participated in a 60-minute, 6-week aquatic exercise program (three sessions per week). The control group was instructed to continue their normal activities of daily living | The Pregnancy Body Shape Questionnaire, the Health Promotion Lifestyle Profile, the Timed Get Up and Go Test, and the Discomfort Intensity Index | Women in the aquatic exercise group reported significantly less physical discomfort, improved mobility, and improved body image and health-promoting behaviors as compared with control subjects | Aquatic exercise during pregnancy may enhance physical functioning, decreasing maternal discomfort, improving maternal body image, and improving health-promoting behaviors |
| Chishaki et al31 | 2006 | Comparison of usefulness between water exercise and gymnastic exercise, Jikyojutsu, in maintaining physical ability for the elderly | To compare physical ability and physical characteristics of elderly women between water exercise and gymnastic exercise | No description | The aquatic group consisted of 21 healthy females (60 ± 5.2 years). The land group consisted of 10 healthy females (60 ± 3.2 years) | Aquatic group: aquatic walking, swimming (twice or more [60 minutes at a time] a week for 1 year). Land group: gymnastic (shoulder raise/lower, arm raise/lower, push-up, lower back twist, straddle stretching, head shake, tumble, etc) (every day [20 minutes in the morning and the afternoon] of the week for 1 year) | Physical characteristics (body mass index, waist size, hip size, % fat), and physical fitness (10 m walking, 10 m maximal walking, 10 m obstacle walking, single-leg standing with eyes open, grip strength, sit up, side steps, sitting-toe-touch test, VO2 max) | The mean percentage of fat mass was reduced in the gymnastic exercise group without change of weight. The average estimated maximal oxygen uptake increased in the gymnastic exercise more than in the water exercise. Sitting trunk flexion was decreased in both groups after 1 year | The results of this study suggested that water exercise could be more beneficial by adding flexibility exercise in the gymnastic exercise, and could maintain and promote physical fitness in elderly people |
| Kawasaki et al32 | 2007 | The effect of aquatic exercise on preventing falls and lifestyle related disease among middle-aged and elderly people | To evaluate the effects of water exercise on blood pressure, carbohydrate and lipid metabolism, arterial sclerosis, and stability of center of mass in middle- and old-age | A swimming club in Kyushu Sangyou University | Eleven healthy males and 24 healthy females were assigned to the training group (N = 35, 61.5 ± 0.8 years) and control group (N = 22, 62.6 ± 0.9 years) | A 2-hour program consisted of stretching, bicycling, walking in warm (30.5°C) water stream, and swimming twice weekly. The training period was 6 months | Anthropometric variables, blood pressure, HR, work load, blood biochemical values, urine testing, blood pressure pulse wave, and stability of center of mass | Weight, body mass index, amount of body fat, blood pressure, and pulse wave velocity decreased and lipid and carbohydrate metabolism and index of arterial sclerosis significantly improved in the training group | Water exercise may be useful for controlling metabolic syndrome and preventing falls in the middle-aged and elderly |
| Nishikawa et al33 | 2008 | Effect of aquatic walking on the cardiovascular patients in our hospital and health-related QOL – in comparison with indoor exercise therapy | To compare the effectiveness of a program of aquatic exercise therapy and land exercise therapy in patients with heart disease | Rehabilitation pool | The aquatic group consisted of 11 males and 3 females 66 ± 7 years. The land group consisted of 8 males and 2 females 63 ± 9 years. Patient characteristic (aquatic/land); angina pectoris (7/5), myocardial infarction (4/5), valve replacement (2/0), dilatative cardiomyopathy (1/0) | Aquatic exercise therapy: stretching, aquatic walking, resistance training. Land exercise therapy: stretching, resistance training, aerobic exercise (ergometer). Each therapy was conducted two times (60 minutes at a time) a week for 3 months | ATVO2, VO2 max, and health-related QOL | ATVO2, VO2 max, and health-related QOL were significantly improved in both groups | The improvement of aerobic fitness was similar in both groups. The difference of improved effect in QOL was due to the fact that the content and the environment of each exercise were different |
| Rotstein et al34 | 2008 | The effect of a water exercise program on the bone density of postmenopausal women | To examine the effect of a 7-month program of water exercise on BMD in postmenopausal females | A heated pool | Thirty-five postmenopausal females aged 50–65 (20 in the experimental group and 10 in the control) | The exercise group trained for 7 months with three 1-hour sessions per week. Each session was divided into four different segments: warm-up, aerobic set, strengthening muscles, and loading the bones, and cool down and stretches | Bone density by DEXA (lunar) for vertebrae L2–L4 and femoral neck of the legs | DEXA test findings for femoral neck density indicated no significant differences between the groups pre- and post-treatment. However a significant interaction was found for BMC in the right leg indicating an increased trend in BMC in the experimental group and a trend towards decrease for the control group | It is possible to plan and execute a water exercise program that has a positive effect on bone status of postmenopausal women |
| Brady et al35 | 2008 | The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: a feasibility study | To determine the feasibility of implementing and investigating the effect of a combined aquatic and land-based rehabilitation program in the post-operative rehabilitation of rotator cuff tears | University of Sydney and Delmer Private Hospital | Eighteen subjects undergoing rotator cuff repair. Aquatic and land group (N = 12, 56.3 ± 9.1 years) and land group (N = 53.5 ± 16.0 years) | Twice per week for 12 weeks. Combined aquatic- and land-based program: standard protocol (passive ROM, active-assisted ROM, resistive phase). Standard land-based program: standard protocol, adding 10 days postoperatively three primary stages: buoyancy assisted ROM, buoyancy supported ROM, and resistive phase | Passive ROM (forward flexion, external rotation), WORC index, health-related QOL, and 11-point VAS | Both subjects improved passive ROM and WORC. Participation in aquatic therapy significantly improved passive flexion range of motion measured at 3 and 6 weeks. No significant differences in the attendance rate and patients perceptions of the programs | The implementation of a combined aquatic- and land-based physiotherapy program following surgical repair of the rotator cuff is feasible and presents a potentially viable alternative to conventional land-based exercise with comparable outcomes |
Note:
*Description of study design was omitted.
Abbreviations: ATVO2, anaerobic threshold oxygen consumption; BBS, Berg Balance Scale; BMC, bone mineral content; BMD, bone mineral density; CG, control group; CI, confidence interval; COP, center of pressure; CRF, chronic kidney disease; Cys-C, cystatin-c; DBP, diastolic blood pressure; GFR, glomerular filtration rate; GSH, glutathione; HDL-C, high density lipoprotein cholesterol; HR, heart rate; HRR, heart rate reserve; HPLP II, Health Promotion Lifestyle Profile II; JOA, Japanese Orthopedic Association; LDL-C, low density lipoprotein cholesterol; LPO, lactoperoxidase; MHP, mental health pattern; NHP, Nottingham Health Profile; OA, osteoarthritis; POMS, Profile of Mood States; QOL, quality of life; ROM, range of motion; SBP, systolic blood pressure; SE, self-efficacy; TC, total cholesterol; TG, training group; U-prot, protein/creatinine ratio; VA, vital age; VAS, visual analog scale; VO2 max, maximal oxygen consumption; WORC, Western Ontario Rotator Cuff.
Table 2.
Brief summary of 21 articles
| Article | Year of publication | Object disease | Effects noted | Withdrawals | Adverse event | Cost of intervention |
|---|---|---|---|---|---|---|
| Willén et al15 | 2001 | Poliomyelitis | Significant effect | No withdrawal | Nothing | No description |
| Ebisu et al16 | 2001 | No specific disease | Significant effecta | No description | No description | No description |
| Aoba et al17 | 2001 | No specific disease | Significant effect | No description | No description | No description |
| Yamada et al18 | 2002 | No specific disease | Significant effect | No description | No description | No description |
| Murai et al19 | 2002 | Knee OA | Significant effect | No description | Nothing | No description |
| Igarashi et al20 | 2002 | No specific disease | Significant effect a | No description | No description | No description |
| Pechter et al21 | 2003 | Moderate chronic kidney disease | Significant effect | No description | No description | Not description |
| Douris et al22 | 2003 | No specific disease | Significant effect | No description | No description | Not description |
| Liquori et al23 | 2003 | No specific disease | Significant effect | No description | No description | No description |
| Lin et al24 | 2004 | Knee-hip OA | Significant effect | N = 9; Reason was not described. | No description | No description |
| Akamine et al25 | 2005 | No specific disease | Significant effect | No description | No description | No description |
| Takumi et al26 | 2005 | No specific disease | Significant effect | No description | No description | No description |
| Takumi and Moriya27 | 2005 | No specific disease | Significant effect | No description | No description | No description |
| Lee28 | 2006 | Knee OA | Significant effect | N = 3; Slipping on poolside, having a cold, low height. | N = 1 Slipping on poolside. | No description |
| Lord et al29 | 2006 | No specific disease | Significant effect | N = 37; Reasons were shown in Table 1 in detail. | No description | No description |
| Smith and Michel30 | 2006 | Discomforts of pregnancy | Significant effect | No description | No description | After pretests were completed, each participant received a $10 grocery store gift certificate, and each one in the aquatic exercise group were given the bus tickets or parking passes to assist participants’ attendance. Other cost was not described |
| Chishaki et al31 | 2006 | No specific disease | Significant effect | No description | No description | No description |
| Kawasaki et al32 | 2007 | No specific disease | Significant effect | N = 8; Low compliance. | No description | No description |
| Nishikawa et al33 | 2008 | Cardiovascular disease | Significant effect | No withdrawal | No description | No description |
| Rotstein et al34 | 2008 | No specific disease | Significant effect | N = 5; Reason was not described. | No description | No description |
| Brady et al35 | 2008 | Rotator cuff tears | Significant effect | No description | Nothing | No description |
Note:
Group comparison was not conducted.
Abbreviation: OA, osteoarthritis.
Withdrawals and adverse events
Withdrawals (dropouts) were reported in five studies,24,28,29,32,34 and adverse events were reported in four studies (Table 2). There were three studies15,19,35 that reported ‘nothing’ on adverse events, and one study28 reported a slipping accident on the poolside (details of the injury were unclear). Other studies did not provide information on withdrawals or adverse events.
Intervention costs
A description of intervention costs was included in only one trial,30 but the summary of that trial did not describe the costs (Table 2).
Quality assessment
We evaluated 21 items from the TREND checklist in more detail (Table 3). This assessment evaluated the quality of how the main findings of the study were summarized in the written report. A lack of description was noteworthy for the studies in general. The items for which the description rate was less than 30% were as follows: “information on how units were allocated to interventions (23.8%)”; “how sample size was determined and, when applicable, explanation of any interim analyses and stopping rules (23.8%)”; “method used to assign units to study conditions, including details of any restriction (19.0%)”; “inclusion of aspects employed to help minimize potential bias induced due to non-randomization (4.8%)”; “whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to study condition assignment; if so, statement regarding how the blinding was accomplished and how it was assessed (14.3%)”; “if the unit of analysis differs from the unit of assignment, the analytical method used to account for this (9.5%)”; “statistical methods used for additional analyses, such as subgroup analyses and adjusted analysis (9.5%)”; “methods for imputing missing data, if used (14.3%)”; “flow of participants through each stage of the study: enrollment, assignment, allocation and intervention exposure, follow-up, analysis (19.0%)”; “dates defining the periods of recruitment and follow-up (14.3%)”; “baseline comparisons of those lost to follow-up and those retained, overall and by study condition (9.5%)”; “comparison between study population at baseline and target population of interest (4.8%)”; “indication of whether the analysis strategy was ‘intention to treat’ or, if not, description of how noncompliers were treated in the analyses (9.5%)”; “for each primary and secondary outcome, a summary of results for each study condition, and the estimated effect (9.5%)”; “inclusion of results from testing prespecified causal pathways through which the intervention was intended to operate, if any (14.3%)”; “summary of other analyses performed, including subgroup or restricted analyses, indicating which are prespecified or exploratory (4.8%)”; and “summary of all important adverse events or unintended effects in each study condition (19.0%)”.
Table 3.
Evaluation of the quality of nonrandomized controlled trials by using the TREND checklist
| Paper section/topic | Item no. | Descriptor | N of yes | % |
|---|---|---|---|---|
| Title and abstract | 1 | • Information on how units were allocated to interventions | 5/21 | 23.8 |
| • Structured abstract recommended | 8/21 | 38.1 | ||
| • Information on target population or study sample | 12/21 | 57.1 | ||
| Introduction | ||||
| Background | 2 | • Scientific background and explanation of rationale | 18/21 | 85.7 |
| • Theories used in designing behavioral interventions | 8/21 | 38.1 | ||
| Methods | ||||
| Participants | 3 | • Eligibility criteria for participants, including criteria at different levels in recruitment/sampling plan (eg, cities, clinics, subjects) | 14/21 | 66.7 |
| • Method of recruitment (eg, referral, self-selection), including the sampling method if a systematic sampling plan was implemented | 10/21 | 47.6 | ||
| • Recruitment setting (settings and locations where the data were collected) | 7/21 | 33.3 | ||
| Interventions | 4 | • Details of the interventions intended for each study condition and how and when they were actually administered, specifically including: | 11/21 | 52.4 |
| • Content: what was given? | 19/21 | 90.5 | ||
| • Delivery method: how was the content given? | 19/21 | 90.5 | ||
| • Unit of delivery: how were subjects grouped during delivery? | 13/21 | 61.9 | ||
| • Deliverer: who delivered the intervention? | 10/21 | 47.6 | ||
| • Setting: where was the intervention delivered? | 16/21 | 76.2 | ||
| • Exposure quantity and duration: how many sessions or episodes or events were intended to be delivered? How long were they intended to last? | 20/21 | 95.2 | ||
| • Time span: how long was it intended to deliver the intervention to each unit? | 21/21 | 100.0 | ||
| • Activities to increase compliance or adherence (eg, incentives) | 7/21 | 33.3 | ||
| Objectives | 5 | • Specific objectives and hypotheses | 15/21 | 71.4 |
| Outcomes | 6 | • Clearly defined primary and secondary outcome measures | 17/21 | 81.0 |
| • Methods used to collect data and any methods used to enhance the quality of measurements | 17/21 | 81.0 | ||
| • Information validated instruments such as psychometric and biometric properties | 8/21 | 38.1 | ||
| Sample size | 7 | • How sample size was determined and, when applicable, explanation of any interim analyses and stopping rules | 5/21 | 23.8 |
| Assignment method | 8 | • Unit of assignment (the unit being assigned to study condition, eg, individual, group, community) | 16/21 | 76.2 |
| • Method used to assign units to study conditions, including details of any restriction (eg, blocking, stratification, minimization) | 4/21 | 19.0 | ||
| • Inclusion of aspects employed to help minimize potential bias induced due to nonrandomization (eg, matching) | 1/21 | 4.8 | ||
| Blinding (masking) | 9 | • Whether or not participants, those administering the interventions, and those assessing the outcomes were blinded to study condition assignment; if so, statement regarding how the blinding was accomplished and how it was assessed | 3/21 | 14.3 |
| Unit of analysis | 10 | • Description of the smallest unit that is being analyzed to assess intervention effects (eg, individual, group, or community) | 15/21 | 71.4 |
| • If the unit of analysis differs from the unit of assignment, the analytical method used to account for this (eg, adjusting the standard error estimates by the design effect or using multilevel analysis) | 2/21 | 9.5 | ||
| Statistical methods | 11 | • Statistical methods used to compare study groups for primary outcome(s), including complex methods for correlated data | 20/21 | 95.2 |
| • Statistical methods used for additional analyses, such as subgroup analyses and adjusted analysis | 2/21 | 9.5 | ||
| • Methods for imputing missing data, if used | 3/21 | 14.3 | ||
| • Statistical software or programs used | 10/21 | 47.6 | ||
| Results | ||||
| Participant flow | 12 | • Flow of participants through each stage of the study: enrollment, assignment, allocation and intervention exposure, follow-up, analysis (a diagram is strongly recommended) | 4/21 | 19.0 |
| • Enrollment: the numbers of participants screened for eligibility, found to be eligible or not eligible, declined to be enrolled, and enrolled in the study | 8/21 | 38.1 | ||
| • Assignment: the numbers of participants assigned to a study condition | 20/21 | 95.2 | ||
| • Allocation and intervention exposure: the number of participants assigned to each study condition and the number of participants who received each intervention | 21/21 | 100.0 | ||
| • Follow-up: the number of participants who completed the follow-up or did not complete the follow-up (ie, lost to follow up), by study condition | 10/21 | 47.6 | ||
| • Analysis: the number of participants included in or excluded from the analysis, by study condition | 13/21 | 61.9 | ||
| • Description of protocol deviations from study as planned, along with reasons | 9/21 | 42.9 | ||
| Recruitment | 13 | • Dates defining the periods of recruitment and follow-up | 3/21 | 14.3 |
| Baseline data | 14 | • Baseline demographic and clinical characteristics of participants in each study condition | 15/21 | 71.4 |
| • Baseline characteristics for each study condition relevant to specific disease prevention research | 7/21 | 33.3 | ||
| • Baseline comparisons of those lost to follow-up and those retained, overall and by study condition | 2/21 | 9.5 | ||
| • Comparison between study population at baseline and target population of interest | 1/21 | 4.8 | ||
| Baseline equivalence | 15 | • Data on study group equivalence at baseline and statistical methods used to control for baseline differences | 10/21 | 47.6 |
| Numbers analyzed | 16 | • Number of participants (denominator) included in each analysis for each study condition, particularly when the denominators change for different outcomes; statement of the results in absolute numbers when feasible | 18/21 | 85.7 |
| • Indication of whether the analysis strategy was “intention to treat” or, if not, description of how noncompliers were treated in the analyses | 2/21 | 9.5 | ||
| Outcomes and estimation | 17 | • For each primary and secondary outcome, a summary of results for each study condition, and the estimated effect size and a confidence interval to indicate the precision | 2/21 | 9.5 |
| • Inclusion of null and negative findings | 9/21 | 42.9 | ||
| • Inclusion of results from testing prespecified causal pathways through which the intervention was intended to operate, if any | 3/21 | 14.3 | ||
| Ancillary analyses | 18 | • Summary of other analyses performed, including subgroup or restricted analyses, indicating which are prespecified or exploratory | 1/21 | 4.8 |
| Adverse events | 19 | • Summary of all important adverse events or unintended effects in each study condition (including summary measures, effect size estimates, and confidence intervals) | 4/21 | 19.0 |
| Discussion | ||||
| Interpretation | 20 | • Interpretation of the results, taking into account study hypotheses, sources of potential bias, imprecision of measures, multiplicative analyses, and other limitations or weaknesses of the study | 10/21 | 47.6 |
| • Discussion of results taking into account the mechanism by which the intervention was intended to work (causal pathways) or alternative mechanisms or explanations | 15/21 | 71.4 | ||
| • Discussion of the success of and barriers to implementing the intervention, fidelity if implementation | 9/21 | 42.9 | ||
| • Discussion of research, programmatic, or policy implications | 9/21 | 42.9 | ||
| Generalizability | 21 | • Generalizability (external validity) of the trial findings, taking into account the study population, the characteristics of the intervention, length of follow-up, incentives, compliance rates, specific sites/settings involved in the study, and other contextual issues | 7/21 | 33.3 |
| Overall evidence | 22 | • General interpretation of the results in the context of evidence and current theory | 12/21 | 57.1 |
Table 4 presents an assessment of the evaluation of study quality by use of the CLEAR-NPT checklist. This tool mainly evaluated the quality of the study conduct. The description rate for the details of the intervention was high (81%), but the rate was low in other primary items. The primary items for which the executive rate was less than 30% were as follows: “Were participants adequately blinded? (4.8%)”; “Were care providers or persons adequately blinded? (4.8%)”; “Were outcome assessors adequately blinded to assess the primary outcomes? (9.5%)”; and “Were the main outcomes analyzed according to the intention-to-treat principle? (14.3%)”.
Table 4.
Evaluation of the quality of nonrandomized controlled trials by using the CLEAR-NPT checklist
| Item |
Practice; N (%) |
||
|---|---|---|---|
| Yes | No | Unclear | |
| 1. Was the generation of allocation sequences adequate?a | – | – | – |
| 2. Was the treatment allocation concealed?a | – | – | – |
| 3. Were details of the intervention administered to each group made available?b | 17 (81.0%) | 3 (14.3%) | 1 (4.7%) |
| 4. Were care providers’ experience or skillc in each arm appropriate?d | 7 (33.3%) | 4 (19.1%) | 10 (47.6%) |
| 5. Was participant (ie, patients) adherence assessed quantitatively?e | 6 (28.6%) | 13 (61.9%) | 2 (9.5%) |
| 6. Were participants adequately blinded? | 1 (4.8%) | 19 (90.6%) | 1 (4.8%) |
| 6.1. If participants were not adequately blinded | |||
| 6.1.1. Were all other treatments and care (ie, cointerventions) the same in each randomized group? | 5 (25.0%) | 12 (60.0%) | 3 (15.0%) |
| 6.1.2. Were withdrawals and lost to follow-up the same in each randomized group? | 14 (70.0%) | 6 (30.0%) | |
| 7. Were care providers or persons caring for the participants adequately blinded? | 2 (9.5%) | 18 (85.8%) | 1 (4.8%) |
| 7.1. If care providers were not adequately blinded | |||
| 7.1.1. Were all other treatments and care (ie, cointerventions) the same in each randomized group? | 4 (19.1%) | 10 (52.6%) | 5 (26.3%) |
| 7.1.2. Were withdrawals and lost to follow-up the same in each randomized group? | 0 | 11 (57.9%) | 8 (42.1%) |
| 8. Were outcome assessors adequately blinded to assess the primary outcomes? | 2 (9.5%) | 19 (90.5%) | 0 (0.0%) |
| 8.1. If outcome assessors were not adequately blinded, were specific methods used to avoid ascertainment bias (systematic differences in outcome assessment)?f | 0 | 19 (100%) | 0 (0%) |
| 9. Was the follow-up schedule the same in each group?g | 8 (38.1%) | 7 (33.3%) | 6 (28.6%) |
| 10. Were the main outcomes analyzed according to the intention-to-treat principle? | 3 (14.3%) | 18 (85.7%) | 0 (0.0%) |
Notes:
First and second items were not described in order to RCT design;
The answer should be “yes” for this item if these data were either described in the report or made available for each arm (reference to a preliminary report, online addendum etc);
Care provider experience or skill will be assessed only for therapist-dependent interventions (ie, interventions where the success of the treatment are directly linked to care provider’s technical skill). For other treatments, this item is not relevant and should be removed from the checklist or answered “unclear”;
Appropriate experience or skill should be determined according to published data, preliminary studies, guidelines, run-in period, or a group of experts and should be specified in the protocol for each study arm before the beginning of the survey;
Treatment adherence will be assessed only for treatments necessitating interventions (eg, physiotherapy that supposes several sessions, in contrast to a one-shot treatment such as surgery). For one-shot treatments, this item is not relevant and should be removed from the checklist or answered “unclear”;
The answer should be “yes” for this item, if the main outcome is objective or haed, or if outcomes were assessed by a blinded or at least an independent endpoint review committee, or if outcomes were assessed by an independent outcome assessor trained to perform the measurements in a standardized manner, or if the outcome assessor was blinded to the study purpose and hypothesis;
This item is not relevant for trials in which follow-up is part of the question. For example, this item is not relevant for a trial assessing frequent vs less frequent follow-up for cancer recurrence. In these situations, this item should be removed from the checklist or answered “unclear”.
Abbreviation: RCT, randomized controlled trial.
Discussion
Overall evidence and quality assessment
There were only 21 nRCTs about aquatic exercise published from 2000 to July 20, 2009, possibly due to the increase in studies with an RCT design. In previous SRs1–3 of RCTs, the authors actually collected many articles that were published in 2000. Pooling of the data from nRCTs was not performed because of the heterogeneity of the studies, multiple outcome measurements, and overall poor presentation. We used the TREND and CLEAR-NPT checklists as quality assessments. There were serious problems with the conduct and reporting of the target articles. Our summaries detected omissions of description and nonfulfillments, including detailed information on participants, sample size, assessors, care (health care) providers, blinding, and analysis methods. Furthermore, the description of adverse events and withdrawals were generally insufficient. In the Cochrane Review,1 there are strict eligibility criteria for a meta-analysis, and for each article, heterogeneity and low quality of reporting must first be excluded. Because there was insufficient evidence in studies of aquatic exercise, due to poor methodological and reporting quality and heterogeneity, we are unable to offer any conclusions about the effects of aquatic exercise based on an SR.
Characteristics of articles
The relevant articles represented several studies of locomotorium diseases (N = 4), compared with few studies of respiratory, circulatory, and psychiatric diseases. This characteristic was apparent in the review article10 of SRs of RCTs. In that review, there were many articles (N = 15) that targeted the health enhancement effect instead of a specific disease, the primary and/or secondary outcome measurements and target participants varied, and a consistent trend was not detected.
We were interested in comparing not only nonintervention as the control, but also land exercise. There were five reports that defined land exercise as the control group, knee osteoarthritis19,28 and rotater cuff tears35 as the target disease; the remaining reports22,31 were about healthy people. Two studies of knee osteoarthritis did not describe intervention effects. The recent meta-analysis2 of RCTs showed no differences between aquatic exercise and land exercise for the pain-relieving effects on neurologic or musculoskeletal disease (P = 0.56; weighted standardized mean difference (SMD), 0.11; 95% confidence interval [CI]: −0.27–0.50; N = 103). Presently, we can not suggest that aquatic exercise is more effective than land exercise for pain relief in locomotorium diseases.
Future research agenda
There were no studies to clarify the effects on serum lipids, body composition, or blood pressure as the main outcome for patients with metabolic syndrome (MS). A joint scientific statement36 about MS was issued recently, and many studies based on those criteria or outcomes should be started soon. Studies of aquatic exercise using prevention or cure as the outcome are also expected.
Table 5 shows the future research agenda for aquatic exercise. In advanced nations and areas, it appears that there is interest in studies about mental health as well as MS. Researchers should use the respective checklists for research design and intervention method, which would lead to improvement in the quality of the study, and contribute to the accumulation of evidence. Suitable comparisons are necessary to explain why aquatic exercise is better than other types of dynamic exercise. Aquatic exercise needs a valuable resource (hot water pool), which can not be overlooked in the study feasibility. A recent study37 suggested that public health is moving toward the goal of implementing evidence-based interventions, but the feasibility of possible interventions and determining whether comprehensive and multilevel evaluations should be justified to accomplish it.
Table 5.
Future research agenda on aquatic exercise intervention
| Item | Concrete agenda |
|---|---|
| Target diseasea or prevention | 1. The prevention and curative effect of metabolic syndrome |
| 2. The prevention and the curative effect of mental diseases such as depression | |
| Strengthening of quality | 1. Set of research protocol, practice, description based on each respective checklist |
| 2. Description of adverse event and withdrawal | |
| Feasibility and intrinsic characteristic | 1. Comparison with land exercise and/or other dynamic intervention |
| 2. Description of intervention cost |
Note:
The pain-relieving effect of chronic locomotorium diseases has already become clear from many randomized controlled trials.
Study limitations
This study was based on the PRISMA statement,38 except for the meta-analysis. However, there were several limitations to the study. Some selection criteria were common to the studies, as described above; however, bias remained due to differences in eligibility for participation in each study. Publication bias was also a limitation. Since we did not limit our search to English, we found 11 articles (52%) published in Japanese. Furthermore, we did not check the references of hand-searches and did not contact institutions, societies, specialists known to have expertise in aquatic exercise, and authors of included studies to identify any additional published or unpublished data.
In terms of quality assessment, disagreements and uncertainties were resolved by discussion between two authors; discussions with a third expert and contact with authors for the purpose of clarification were not allowed.
Conclusion
Because there was insufficient evidence on aquatic exercise due to poor methodological and reporting quality, and heterogeneity of nRCTs, we were unable to offer any conclusions about the effects of this type of intervention. However, we were able to identify the problems with current nRCTs of aquatic exercise, and propose a strategy of strengthening study quality and stressing the importance of study feasibility as a future research agenda objective.
Acknowledgments
This study was supported by the Health and Labour Sciences Research Grants (Research on Health Security Control: ID No. H20-007) from the Japanese Ministry of Health, Labour and Welfare in 2009. We would like to express our appreciation to Ms Rie Higashino, Ms Mari Makishi, and Ms Yukiko Yamada for their assistance in this study.
Appendix 1. References to studies excluded from this review
| No. | Author. Journal (Year) | Title | Reason for exclusion |
|---|---|---|---|
| E1 | Bar-Or. Phys Sport Med (2000) | Juvenile obesity, physical activity, and lifestyle changes | Review article |
| E2 | Biering-Sørensen et al. Spinal Cord (2000) | Bacterial contamination of bath-water from spinal cord lesioned patients with pressure ulcers exercising in the water | No intervention by aquatic exercise |
| E3 | Darby et al. J Sports Med Phys Fitness (2000) | Physiological responses during two types of exercise performed on land and in the water | Cross-over design |
| E4 | Hsieh. MAMM (2000) | Aquatic exercise makes a splash | Program idea |
| E5 | Jamison. Rehab Management (2000) | Long-term rehab. The healing properties of water | Review article |
| E6 | Sugano et al. J Physiol Anthropol Appl Hum Sci (2000) | Influence of water exercise and land stretching on salivary cortisol concentrations and anxiety in chronic low back pain patients | Cross-over design |
| E7 | Watanabe et al. Percept Mot Skills (2000) | Comparison of water- and land-based exercise in the reduction of state anxiety among older adults | RCT |
| E8 | Alzugaray. Midwifery Today (2001) | American AquaNatal: a midwifery-based holistic prenatal water exercise and educational program | Program idea |
| E9 | Hartmann et al. Geburtsh Frauenheilk (2001) | “Aqua-Fit” during pregnancy: Maternal and fetal hemodynamic responses during rest, immersion and exercise | No control group |
| E10 | Piso et al. Phys Med Rehabil Kuror (2001) | Analgesic effects of sauna in fibromyalgia | RCT |
| E11 | Postollec. Back on Track (2001) | Back on Track Aquatic therapy can help patients with back pain resume normal activity | Program idea |
| E12 | Shono et al. J Physiol Anthropol (2001) | Physiological responses to water-walking in middle aged women | Physiological responses (regulatory experiment group versus the other group) |
| E13 | Watanabe et al. Percept Mot Skills (2001) | Effects of increasing expenditure of energy during exercise on psychological well-being in older adults | No control group |
| E14 | Seki et al. Bul of Nurs College, Wakayama Med Univ (2001) | The effects of maintaining health by exercising in the water in middle to old-aged women | No control group |
| E15 | Belza et al. Nus Res (2002) | Does adherence make a difference | RCT |
| E16 | Huey et al. Best of Both Worlds (2002) | Combining aquatics with land exercise effectively reduces back pain | Program idea |
| E17 | V. Kendrick et al. J Aquatic Phys Ther (2002) | Effects of water exercise on improving muscular strength and endurance in suburban and inner city older adults | Cohort study |
| E18 | Warden et al. Sports Med (2002) | Aetiology of rib stress fractures in rowers | Review article |
| E19 | Weinsier et al. An J Clin Nutr (2002) | Free-living activity energy expenditure in women successful and unsuccessful at maintaining a normal body weight | No intervention by aquatic exercise |
| E20 | Winter et al. J Aquatic Phys Ther (2002) | Effects of aquatic lumbar stabilization and strengthening exercise protocol on chronic low back pain patients | No control group |
| E21 | Sudo et al. Ann reports Health Phys Educ Sports Sci (2002) | Effects of the underwater exercise on elderly with low-muscle strength | Cross-sectional study |
| E22 | Tsushita et al. J Aquatic Health Med (2002) | Effect of aquatic exercise on lifestyle-related diseases in middle-aged women | No control group |
| E23 | Campbell et al. Med Sci Sports Exer (2003) | Metabolic and cardiovascular response to shallow water exercise in young and older women | Physiological responses |
| E24 | Charitopoulos et al. J Human Mov Stud (2003) | Application of an aqua exercise programme in children with exercise induced asthma | No control group |
| E25 | Driver et al. J Cognit Rehabil (2003) | Effect of an aquatics program on psycho/social experiences of individuals with brain injuries: a pilot study | Case report |
| E26 | Gyurcsik et al. Arthritis Rheum (2003) | Exercise-related goals and self-efficacy as correlates of aquatic exercise in individuals with arthritis | Cross-sectional study |
| E27 | Mayo Clin. Health Lett (2003) | Water exercise for arthritis: low-impact fitness | Health letter |
| E28 | Suomi et al. Arch Phys Med Rehabil (2003) | Effects of arthritis exercise programs on functional fitness and perceived activities of daily living measures in older adults with arthritis | RCT |
| E29 | Weidner et al. Aktuelle Rheumatoligie (2003) | Rheumatism and Sports | Review article |
| E30 | Yurtkuran et al. Am J Phys Med Rehabil (2003) | Evaluation of hormonal response and ultrasonic changes in heel bone by aquatic exercise in sedentary postmenopausal women | RCT |
| E31 | Sugano et al. Bull Inst Health Sport Sci, Univ of Tsukuba (2003) | Prescription of water exercise for low back pain patients. Influence of water exercise and land stretching on salivary cortisol concentrations and anxiety in chronic low back pain patients | Study report |
| E32 | Matsumoto et al. Ann Reports Health Physl Educ Sports Sci (2003) | Blood chemical values in elderly persons performing habitual aquatic exercise | Cross-sectional study |
| E33 | Benelli et al. J Strength Cond Res (2004) | Physiological responses to fitness activities: a comparison between land-based and water aerobics exercise | Cross-over design |
| E34 | Booth. Activ Adapt Aging (2004) | Water exercise and its effect on balance and gait to reduce the risk of falling in older adults | Cross-sectional study |
| E35 | Preis et al. Fisioterapia em Movimento (2004) | Análise de um programa de execução de saltos múltiplos verticais no meio líquido e no solo | Biomechanical trial |
| E36 | Roebrs et al. J Neurol Phys Ther (2004) | Effects of an aquatics exercise program on quality of life measures for individuals with progressive multiple sclerosis | No control group |
| E37 | Aoba et al. Kokushikan Soc Sport Sci (2004) | The effect of continuation term on BP at water exercise | No retrospective comparison between aquatic exercise group and drop out group of aquatic exercise |
| E38 | Ashida et al. Ann Reports Misasa Med Center, Okayama Univ (2004) | Clinical study on reduction of costs of drugs for the treatment of asthma in relation to the administration method | Not intervention study |
| E39 | Katayama et al. Descente Sports Sci (2004) | Effects of weight reduction through dietary restriction and exercise training on blood fluidity in obese middle-aged women | No intervention by aquatic exercise |
| E40 | Higuma et al. J Oita Med Assoc (2004) | Rehabilitation after TKA in a hospital | Cross-sectional study |
| E41 | Barry Dale et al. Rehabil Management (2005) | Aquatic therapy offers benefits to a wide range of clinical populations | Review article |
| E42 | Cider et al. Clin Physiol Funct Imaging (2005) | Cardiorespiratory effects of warm water immersion in elderly patients with chronic heart failure | Comparison between patients on healthy people |
| E43 | Kelly et al. Development Med Child Neurol (2005) | Aquatic exercise for children with cerebral palsy | Review article |
| E44 | Kato et al. Research Reports Suzuka Univ Med Sci Technol (2005) | Influence of aquatic-exercise on arterial blood pressure and acceleration plethysmogram in middle-aged women | Case report |
| E45 | Matsubara et al. Ishikawa J Nurs (2005) | Case-control study on long-term effect of programmed movement practice course combined with bathing in hot spring | Case-control study |
| E46 | Gusi et al. Arthritis Rheum (2006) | Exercise in waist-high warm water decreases pain and improves health-related quality of life and strength in lower extremities in women with fibromyalgia | RCT |
| E47 | Katia et al. JAGS (2006) | Older people involved in physical activity benefit from water exercise, showing longer total sleep time | Letter to the journal’s editor |
| E48 | Goto et al. J Jpn Assoc Phys Med Balneol Climatol (2006) | The effect of Spa-aqua therapy on lifestyle-related diseases in collaboration with public spa facility | No control group |
| E49 | Kokubu et al. Hip Joint (2006) | Effect of underwater exercise for hip joint disease | Cross-sectional study |
| E50 | Yano et al. Jpn J Phys Fitness Sports Med (2006) | Effect of fluid in ingestion on physiological response before walking in a pool | No intervention by aquatic exercise |
| E51 | Brody. J Aquatic Phys Ther (2007) | Aquatic physical therapy practice analysis | Practice analysis |
| E52 | Goodwin. OT Practice (2007) | Exploring the effects of a swim program for clients with down syndrome | No control group |
| E53 | Kang et al. J Gerontol Nurs (2007) | Aquatic exercise in older Korean women with arthritis | No control group |
| E54 | Kron. Complementary Med (2007) | Water therapies | Review article |
| E55 | McManus B. Pedia Phys Ther (2007) | The effect of aquatic therapy on functional mobility of infants and toddlers in early intervention | RCT |
| E56 | Magkos et al. Clin J Sports Med (2007) | The bone response to nonweight-bearing exercise is sport-, site-, and sex-specific | Cross-sectional study |
| E57 | Schmid et al. Heart (2007) | Influence of water immersion, water gymnastics and swimming on cardiac output in patients with heart failure | Physiological responses of various performances in water |
| E58 | Alpert. Cardiology (2008) | A water-based exercise program for patients with coronary artery disease | Editorial comment |
| E59 | Hujibregts et al. Top Stroke Rehabil (2008) | Implementation, process, and preliminary outcome evaluation of two community programs for persons with stroke and their care partners | Not intervention by aquatic exercise |
| E60 | Kelley et al. Therapeutic Recreation J (2008) | Comparing the effects of aquatic and land-based exercise on the physiological stress response of women with fibromyalgia | A single-subject alternating treatment design |
| E61 | Tokmakidis et al. Cardiology (2008) | Training, detraining and retraining effects after a water-based exercise program in patients with coronary artery disease | RCT |
| E62 | Colado et al. Eur J Appl Physiol (2009) | Effects of aquatic resistance training on health and fitness in postmenopausal women | RCT |
| E63 | Fragala-Pinkham et al. Pedia Phys Ther (2009) | An aquatic physical therapy program at a pediatric rehabilitation hospital: a case series | Case report |
| E64 | Laurent et al. Euro Soc Cardiol (2009) | Training-induced increase in nitric oxide metabolites in chronic heart failure and coronary artery disease: an extra benefit of water-based exercises? | RCT |
| E65 | Schmid et al. Heart (2009) | Influence of water immersion, water gymnastics and swimming on cardiac output in patients with heart failure | No intervention by aquatic exercise |
| E66 | Souza Vale et al. Arch Gerontol Geriatrics (2009) | Effects of muscle strength and aerobic training on basal serum levels of IGF-1 and cortisol in elderly women | No intervention by aquatic exercise |
| E67 | Tolomio et al. Clin Ter (2009) | Effects of a combined weight- and non weight-bearing (water) exercise program on bone mass and quality in postmenopausal women with low bone mineral density | No intervention by aquatic exercise |
Abbreviations: IGF-1, insulin-like growth factor-1; RCT, randomized controlled trial.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bartels EM, Lund H, Hagen KB, Dagfinrud H, Christensen R, Danneskiold-Samsoe B. Aquatic exercise for the treatment of knee and hip osteoarthritis. Cochrane Database Syst Rev. 2007;4:CD005523. doi: 10.1002/14651858.CD005523.pub2. [DOI] [PubMed] [Google Scholar]
- 2.Hall J, Swinkels A, Briddon J, McCabe CS. Does aquatic exercise relieve pain in adults with neurologic or musculoskeletal disease? A systematic review and meta-analysis of randomized controlled trials. Arch Phys Med Rehabil. 2008;89:873–883. doi: 10.1016/j.apmr.2007.09.054. [DOI] [PubMed] [Google Scholar]
- 3.Bender T, Karaglle Z, Balint GP, Gutenbrunner C, Balint PV, Sukenik S. Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int. 2005;25:220–224. doi: 10.1007/s00296-004-0487-4. [DOI] [PubMed] [Google Scholar]
- 4.Yamazaki F, Endo Y, Torii S, Sagawa S, Shiraki K. Continuous monitoring of change in hemodilution during water immersion in humans: effect of water temperature. Aviat Space Environ Med. 2000;71:632–639. [PubMed] [Google Scholar]
- 5.Gabrielsen A, Videbaek R, Johansen LB, et al. Forearm vascular and neuroendocrine responses to graded water immersion in humans. Acta Physio Scand. 2000;169:87–94. doi: 10.1046/j.1365-201x.2000.00680.x. [DOI] [PubMed] [Google Scholar]
- 6.Fam AG. Spa treatment in arthritis: a rheumarologist’s view. J Rheumatol. 1991;18:1775–1777. [PubMed] [Google Scholar]
- 7.Kamioka H, Nakamura Y, Okada S, et al. Effectiveness of comprehensive health education combining lifestyle education and hot spa bathing for male white-collar employees: a randomized controlled trial with 1-year follow-up. J Epidemiol. 2009;19:219–230. doi: 10.2188/jea.JE20081020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kamioka H, Nakamura Y, Yazaki T, et al. Effectiveness of comprehensive health education combining hot spa bathing and lifestyle education in middle-aged and elderly women: one-year follow-up on randomized controlled trial of three- and six-month interventions. J Epidemiol. 2006;16:35–44. doi: 10.2188/jea.16.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kamioka H, Ohshiro H, Mutoh Y, et al. Effect of long-term comprehensive health education on the elderly in a Japanese village: Unnan cohort study. Int J Sports Health Sci. 2008;6:60–65. [Google Scholar]
- 10.Kamioka H, Tsutani K, Okuizumi H, et al. Effectiveness of aquatic exercise and balneotherapy: a summary of systematic reviews based on randomized controlled trials of water immersion therapies. J Epidemiol. 2010;20:2–12. doi: 10.2188/jea.JE20090030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pittler MH, Karagülle MZ, Karagülle M, Ernst E. Spa therapy and balneotherapy for treating low back pain: meta-analysis of randomized trials. Rheumatol. 2006;45:880–884. doi: 10.1093/rheumatology/kel018. [DOI] [PubMed] [Google Scholar]
- 12.Jarlais DC, Lyles C, Crepaz N, for the TREND group Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions. Am J Public Health. 2004;94:361–366. doi: 10.2105/ajph.94.3.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Boutron I, Moher D, Tugwell P, et al. A checklist to evaluate a report of a nonpharmacological trial (CLEAR NPT) was developed using consensus. J Clin Epidemiol. 2005;58:1233–1240. doi: 10.1016/j.jclinepi.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490–1497. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Willén C, Sunnerhagen KS, Grimby G. Dynamic water exercise in individuals with late poliomyelitis. Arch Phys Med Rehabil. 2001;82:66–72. doi: 10.1053/apmr.2001.9626. [DOI] [PubMed] [Google Scholar]
- 16.Ebisu T, Kobayashi M, Katsuki T, Yanagimoto Y. Effectiveness of serum lipids on spa-walking [in Japanese] Health Care. 2001;43:981–984. [Google Scholar]
- 17.Aoba T, Matsumoto T, Sugano A, Nomura T. The effects of enforcement water exercise class on hypotensive to blood pressure at elderly subjects [in Japanese with English abstract] Ann Reports Health Phys Educ Sports Sci. 2001;20:99–104. [Google Scholar]
- 18.Yamada T, Watanabe E, Okada A, Takeshima N. Effects of water-based well-rounded exercise on vital age and physical fitness in older adults [in Japanese with English abstract] Jpn Soc Phys Anthropol. 2002;7:87–93. [Google Scholar]
- 19.Murai E, Takeda Y, Imaya T, Uchiyama E, Nakazono K, Nakajima H. Exercise therapy for osteoarthritis of the knee -preliminarily study of water exercise [in Japanese with English abstract] J Jpn Soc Clin Sports Med. 2002;10:54–60. [Google Scholar]
- 20.Igarashi Y, Kondo T, Yamaoka K, et al. Health effect of aquatic exercise therapy using a hot spring [in Japanese] Sick Body Phys. 2002;36:11–14. [Google Scholar]
- 21.Pechter Ü, Ots M, Mesikepp S, et al. Beneficial effects of water-based exercise in patients with chronic kidney disease. Int J Rehabil Res. 2003;26:153–156. doi: 10.1097/00004356-200306000-00013. [DOI] [PubMed] [Google Scholar]
- 22.Douris P, Southard V, Varga C, Schauss W, Gennaro C, Reiss A. The effect of land and aquatic exercise on balance scores in older adules. J Geriatr Phys Ther. 2003;26:3–6. [Google Scholar]
- 23.Liquori A, Widener G, Clark L. Effects of a 6-week prenatal water exercise program on physiological parameters and well-being in women with pregnancies in the 2nd–3rd trimesters: a pilot study. J Section Women’s Health. 2003;27:11–19. [Google Scholar]
- 24.Lin SY-C, Davey RC, Cochrane T. Community rehabilitation for older adults with osteoarthritis of the lower limb: a controlled clinical trial. Clin Rehabil. 2004;18:92–101. doi: 10.1191/0269215504cr706oa. [DOI] [PubMed] [Google Scholar]
- 25.Akamine T, Yamanaka T, Taguchi N, et al. Effects of underwater exercise with hot spring bathing on middle aged people [in Japanese with English abstract] Kyushu Yamaguchi Sports Sci J. 2005;17:7–12. [Google Scholar]
- 26.Takumi Y, Moriya K, Oda S, Adikari MO, Fukuoka E. Participation in an aquatic exercise class twice a week for 12 weeks improved physical fitness for good walking, walking self-efficacy on winter roads, mental health and QOL in elderly women [in Japanese with English abstract] Jpn J Biometeor. 2005;42:17–27. [Google Scholar]
- 27.Takumi Y, Moriya K. Participation in an aquatic walking class for 12 weeks improved physical fitness for good walking, emotion and walking self-efficacy on winter roads in middle-aged and elderly women [in Japanese with English abstract] Jpn J Biometeor. 2005;42:5–15. [Google Scholar]
- 28.Lee HY. Comparison of effects among Tai-chi exercise, aquatic exercise, and a self-help program for patients with knee osteoarthritis [in Korean with English abstract] J Korean Acad Nurs. 2006;36:571–580. doi: 10.4040/jkan.2006.36.3.571. [DOI] [PubMed] [Google Scholar]
- 29.Lord SR, Matters B, George RS, Thomas M, Bindon J, Chan DK-Y. The effects of water exercise on physical functioning in older people. Australasian J Ageing. 2006;25:36–41. [Google Scholar]
- 30.Smith SA, Michel Y. A pilot study on the effects of aquatic exercises on discomforts of pregnancy. J Obstet Gynecol Neonatal Nurs. 2006;35:315–323. doi: 10.1111/j.1552-6909.2006.00045.x. [DOI] [PubMed] [Google Scholar]
- 31.Chishaki A, Makaya M, Nagahiro C, et al. Comparison of usefulness between water exercise and gymnastic exercise, Jikyojyutsu, in maintaining physical ability for the elderly [in Japanese with English abstract] Memoirs Dep Health Sci Sch Med Kyushu Univ. 2006;7:23–32. [Google Scholar]
- 32.Kawasaki T, Muratani H, Ozoe N, Higaki H, Kawasaki J. The effect of aquatic exercise on preventing falls and life-style related disease among middle-aged and elderly people [in Japanese] Jpn J Clin Exper Med. 2007;84:402–411. [Google Scholar]
- 33.Nishikawa A, Ueda Y, Wakayama K, Hayashi Y. Effect of aquatic walking on the cardiovascular patients in our hospital and health-related QOL- in comparison with indoor exercise therapy [in Japanese] JJCR. 2008;13:135–138. [Google Scholar]
- 34.Rotstein A, Harush M, Vaisman N. The effect of a water exercise program on bone density of postmenopausal women. J Sports Med Phys Fitness. 2008;48:352–359. [PubMed] [Google Scholar]
- 35.Brady B, Redfern J, Macdougal G, Williams J. The addition of aquatic therapy to rehabilitation following surgical rotator cuff repair: a feasibility study. Physiother Res Int. 2008;13:153–161. doi: 10.1002/pri.403. [DOI] [PubMed] [Google Scholar]
- 36.Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation TaskForce on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 37.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med. 2009;36:452–457. doi: 10.1016/j.amepre.2009.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–W94. doi: 10.7326/0003-4819-151-4-200908180-00136. [DOI] [PubMed] [Google Scholar]