Abstract
Household survey data on age at first use of alcohol, tobacco, marijuana, and hard drugs can be biased due to sample selection and inaccurate recall. One potential concern is attrition, whereby individuals who get involved with substance use at an early age become increasingly less likely to be surveyed in successive years. A comparison of data from the National Household Survey on Drug Abuse (NHSDA) with data from a longitudinal study suggested that attrition might have caused substantially less bias than did “forward telescoping,” the inflating of age at first use over time. The evidence of forward telescoping was particularly pronounced with respect to age at first use of alcohol. This paper presents a procedure for correcting the distribution of age at first use for forward telescoping (but not attrition) by viewing a portion of the NHSDA data collected in successive years as constituting a cohort study. Results are presented from applying this procedure with NHSDA data collected from 1982 to 1995 for respondents born 1968–1973. The findings suggest that prevention programs need to be introduced at an earlier age than would be indicated by “uncorrected” retrospective data. Other implications are also highlighted.
Keywords: drug use, self-report, validity, forward telescoping, attrition
1. INTRODUCTION
In the last few decades, several trends in the advancement of data collection have greatly improved the quality of survey information available for research on substance use and abuse. Two important trends include the increasing collection of longitudinal data and the institution of several major cross-sectional surveys on an annual basis. Longitudinal panel studies have been broadly recognized as an important standard of quality for research on adolescent development (Elliott, 1992; Kandel, 1978; Tonry et al., 1991). In a longitudinal study, subjects are recruited at a young age and reinterviewed at regular intervals as they grow up. When carefully executed, this research design helps to avoid (but does not always eliminate) three of the greatest threats to a study's validity: inaccurate recall, nondisclosure, and sample selection bias. The accurate identification of when events occurred, the context of the event, and how the individual felt about them is greatly enhanced through the contemporaneous collection of information. The rate of self-disclosure is also potentially enhanced through researchers’ continued efforts to gain rapport with each individual over time. Perhaps most importantly, such studies have the potential for identifying the prevalence of various behaviors and the risks and protective factors for the behavior, to the extent that they start with representative samples and control for attrition.
For these reasons, the longitudinal design can be thought of as the “gold standard” for developmental research. However, just like gold, this approach to research is expensive, particularly when it comes to relocating and interviewing individuals over time. Due to the large follow-up costs, longitudinal studies are typically of limited size. This limitation generally restricts their utility for studying the etiology of behaviors like abuse of hard drugs that are relatively rare in the general population. Furthermore, the limited sample size most often precludes comparisons across location, birth year, or race/ethnicity, which hinders the generalizability of the findings. Lastly, there is the time element. As Tonry et al. (1991, p. 11) concisely noted, “Long-term longitudinal studies... take a long time to be carried out.”
The cohort approach, sometimes called a repeated cross-section analysis, provides an alternative method for studying adolescent development. In the repeated cross-section design, researchers interview a representative sample of individuals born in the same year or over a few consecutive years (referred to as a birth cohort) at a young age. Then, at regular intervals the researchers interview other representative samples in which the same birth cohort is included. Unlike in the more restrictive longitudinal design, however, these would not be the same individuals. Consequently, this repeated cross-section approach avoids the expense of tracking individuals over time. To the extent that each cross-sectional sample is truly representative, this approach can identify a birth cohort's experience over time. In particular, it can identify the incidence of initiation and prevalence of drug use behaviors prevailing at each age for the birth cohort studied.
The major limitation of a cohort analysis is that it does not identify those factors at one age that are associated with behaviors at a subsequent age. This limitation generally precludes the identification of risk and protective factors for drug abuse, unless individuals are asked to provide retrospective reports. This leads to a third approach to developmental research, the examination of life histories provided retrospectively.
Retrospective life histories are subject to a variety of potential biases that are described in Section 1.1. Thus, these data are less valuable, case per case, than longitudinal panel data. On the other hand, massive amounts of retrospective data are collected annually. Perhaps with regard to the calculation of total usefulness, quantity can somehow substitute for quality. The National Household Survey on Drug Abuse (NHSDA) program alone currently collects about 30,000 cases per year. The public archive for these data is available online (www.icpsr.umich.edu) from the Inter-University Consortium for Political and Social Research (ICPSR) and includes over 150,000 drug use histories; all of them provide retrospective self-reports. These data provide much information about substance use and development and can be analyzed across locations, birth years, and interview years. This information is useful for evaluating recent substance use trends, and identifying the appropriate timing of prevention programs, among other public policy applications. The value of these data is greatly enhanced to the extent to which their biases are understood and analytic strategies for their correction developed.
This paper examines the use of retrospectively reported age at first use of various substances: alcohol, tobacco, marijuana and hard drugs. First, we present a comparison of the NHSDA data to data from a longitudinal sample. The findings are consistent with the idea that the most extensive bias in the reported age at first use is due to forward telescoping—individuals increasing their reported age at first use as they age. Next, we present a technique for controlling the impact of forward telescoping by viewing the NHSDA as a collection of cohort studies. This procedure does not correct for sampling bias or for nondisclosure. The procedure is used to obtain “corrected” distributions for the ages at first use of alcohol, tobacco, marijuana, and hard drugs for the 1968–1973 birth cohort.
The resulting distributions provide important basic information about substance use. The larger contribution of this work, however, is the extent to which it advances our understanding of the bias in retrospectively reported ages at first use and the presentation of a correction procedure when using NHSDA data to study developmental issues. The conclusion highlights the implications of these findings and suggests important directions for further research.
1.1. Biases in Household Survey Data
Survey biases are broadly classified as emanating either from the sampling procedure or from the quality of responses obtained (a.k.a., nonsampling errors). The NHSDA program uses an advanced statistical design involving random sampling within various strata in order to obtain a highly representative sample of household residents in the United States. The responses thus provide an indication of substance use within mainstream America. However, it is well established that the NHSDA tends to undersample hardcore drug abusers who are apt to be more transient, are often not living in stable households, and are more likely to not agree to respond to the survey (Wright et al., 1997). Thus, all statements based on findings from the NHSDA are relevant only to the selected sampling frame, household residents, a sample selection bias.
This bias not only affects the population to which findings can be generalized but also can seriously bias repeated cross-section analyses. The central assumption of the repeated cross-section design is that respondents are sampled from the same population over time as they age. However, as some individuals become more deviant with age, and more involved with substance use, they may also become less likely to live in a stable household. In this regard, some of the most deviant individuals may be increasingly less likely to be interviewed by the NHSDA over time. We refer to this phenomenon as attrition from the sampling frame.
Regarding the validity of self-report responses, a preliminary concern is whether individuals will even disclose use of a substance. Indeed, several studies suggest that individuals often inconsistently report whether they had used a substance (Bailey et al., 1992; Fendrich and Vaughn, 1994; Harrison, 1995; Johnston and O'Malley, 1997). Among those who do disclose, there are still a variety of psychological and communications factors that can potentially affect the accuracy of reported age at first use of a substance (Eisenhower et al., 1991). The clarity with which individuals remember their first use of a substance and their age at the time may simply fade as the years pass, resulting in increased unreliability with age. This unreliability may also result from the fact that personal memories rarely contain information about absolute (i.e., calendar) time (Brewer, 1988).
In addition to this general unreliability, numerous studies suggest that individuals tend to underestimate the time since the occurrence of an event, which can result in forward telescoping [see Eisenhower et al. (1991) for a summary of this literature]. Indeed, Johnson et al. (1997) found evidence of such possible forward telescoping in response to questions of age at first use of various substances in the NHSDA. Similar to forward telescoping, the reported age at first use can potentially increase with interview age as a result of a continuing redefinition of what an individual believes constitutes “first use,” even if the question is stated exactly the same. Younger children might count a sip or two of a parent's drink as their first use of alcohol, older individuals might remember the first time they bought liquor or got drunk with friends.
The declining precision of recall with age may also result in individuals commonly reporting a convenient age at first use around a pivotal time in their life, like age 18 or even 21. This type of a clumping phenomenon often presents itself to census takers working in less developed countries. In some of these countries, there are no central organizations that maintain accurate birth records. Moreover, many individuals in such countries do not keep track of their age. Thus when asked, they provide an approximate age. This approximation typically results in a disproportionate number of ages ending in the digits 0 and 5. The reported age at first use of alcohol and tobacco might further be influenced by the age at which their use is legal. Many individuals might not wish to disclose illegal activity despite the survey taker's assurances that their individual responses will remain confidential.
2. METHODS
This paper focuses on the accuracy of the distribution of alcohol, tobacco, marijuana, and hard drugs reported to the NHSDA. For this study, hard drug use was defined as the nonprescription use of cocaine powder, crack, and/or heroin, drugs with strong psychoactive properties that have been widely abused. The primary hypothesis that initially guided this work held that these data would be biased due to attrition from the sampling frame.
Hypothesis: Individuals who become involved with alcohol, tobacco, marijuana or hard drug use at an early age are more likely to move out of a household, perhaps not by choice. This process results in attrition of early substance users with age from the NHSDA sampling frame.
To investigate this attrition, we chose to explore variation over time in the distribution of age at first use (for each substance) as reported by members of a single birth cohort. It was expected that fewer of the older respondents would have reported early initiation of each substance. In this way, the extent of attrition from the sampling frame could be identified, assuming that the self-reports of age at first use were accurate. The possibility that the data were inaccurate led to the following alternative explanation for any decline in the proportion of early initiators with respondent age.
Alternative Hypothesis: Reports of early substance use initiation among older respondents are rare because of forward telescoping. As they age, early initiators become increasingly less likely to report having started early.
These two very different biases (attrition and forward telescoping) could potentially have caused similar distortions in the distribution of age at first use, fewer reports of early initiation among older respondents. To investigate the plausibility of each hypothesis, the repeated cross-section data from the NHSDA were compared to data from a longitudinal study, the Rutgers Health and Human Development Project (hereafter referred to as the Rutgers Project). The Rutgers Project interviewed exactly the same individuals on successive occasions. Thus, the reported distribution of age at first use might have been affected by forward telescoping but not by differential attrition.
A visual comparison of the distributions from the two datasets was performed. A more rigorous statistical analysis was precluded by the limited sample size of the Rutgers Project and the differences from the NHSDA in the population sampled. Although both surveys used representative household populations, the NHSDA data are representative of the United States and the Rutgers Project data are representative of most of New Jersey. Additionally, slightly different birth years were used in each data set. Thus, the distribution of age at first use of each substance was not expected to match precisely.
Overall, the Rutgers Project data were not expected to provide an accurate estimate of the bias in the NHSDA data but, rather, a general sense that could help guide subsequent corrections to the NHSDA data. To the extent that the decline in early initiators was not observed in the Rutgers Project data, support would be provided for the idea that the variation observed in the NHSDA might have been caused by attrition from the sampling frame. To the extent that the findings from the two datasets were similar, support would be provided for the idea that the variation observed in the NHSDA might have resulted from forward telescoping.
The remainder of this section presents: a procedure for obtaining a distribution for age at first use from the NHSDA that corrects for forward telescoping, a description of the NHSDA data, and a description of the Rutgers Project data.
2.1. A “Corrected” Distribution for Age at First Use
We had originally devised a procedure for correcting the distribution of reported age at first use in the NHSDA assuming that the decline in early initiators resulted from attrition and that forward telescoping was negligible. The procedure involved using data obtained from respondents at each age to calculate the hazard of initiation during the previous year. The use of hazard rates focused the estimation procedure on recent initiation which is likely to have been accurately reported and thus avoided the impact of attrition by early initiators. These hazard rates would have then been used to derive the distribution of age at initiation.
As it turned out, the analysis with the Rutgers Project data appeared more consistent with the idea that the observed decrease in early initiators with age at interview resulted from forward telescoping as opposed to attrition. In light of this finding, we decided that at this time a procedure to correct for forward telescoping was more relevant. The procedure presented does not correct for attrition from the sampling frame or for nondisclosure of substance use.
The estimation procedure viewed the NHSDA data for the 1968–1973 birth cohort from ages 12 through 25 as obtained from 1982 through 1995 as a repeated cross section. The first step was to use the data obtained from respondents at each age to estimate the cumulative distribution of initiation by 1 year prior to their age at interview. In choosing this statistic, the estimation procedure avoided an overreliance on the accuracy of any individual's reported age at first use. The age 1 year prior to the interview was used to avoid having to deal with partial years. (An individual who had not initiated use by the time of the interview might subsequently initiate use before a next birthday.) Subsequently, the “corrected” distribution for age at first use was obtained by taking the first differences of the cumulative percentages. In cases where the cumulative percentage reporting lifetime use at a given age is less than the percentage for the preceding age, the percentage initiating was estimated as zero.
2.2. The National Household Survey on Drug Abuse
In 1971, the Public Health Service of the U.S. Department of Health and Human Services established the NHSDA to measure the use of illicit drugs, alcohol, and tobacco within the general population of Americans aged 12 and above (SAMHSA, 1997). During the 1970s and 1980s, the sample was conducted at least once every 3 years. Starting with 1990, the survey has been conducted yearly and annual samples have included 20,000 to 30,000 interviews. Data collected through the NHSDA program are made publicly available through the Inter-University Consortium for Political and Social Research (ICPSR). At the time of this project, data were available from the 1982, 1985, 1988, and 1990–1995 collection years, which included 159,561 cases.
The NHSDA data collection procedures include personally visiting each residence, administering questionnaires, and providing self-administered answer sheets for sensitive information. The complex selection procedure includes unequal selection probabilities, stratification and clustering (SAMHSA, 1997, pp. 4–6). The sample has always included a proportionate number of females and has oversampled individuals who are either Black, Hispanic, or aged 12 to 17. To account for this nonproportional sampling, the NHSDA program constructs a sample weight for each respondent reflecting her or his probability of inclusion. An appropriately weighted average provides an estimate of the prevalence of any substance use behavior within the broader household population, which is not biased by the sample design.
This study examined the experiences of individuals born 1968–1973 who were included in the cross-sectional samples obtained by NHSDA from 1982 to 1995. These 6 consecutive birth years were selected because the NHSDA 1982–1995 data provide a fairly large sample of interviews at each age from 12 through 25 for this multiyear birth cohort. Table I indicates the actual number of cases from each birth year interviewed at each age. The combined subsample sizes by age ranges from 605 for 13 year olds up to 3504 for 21 year olds. Some cell counts are zero (or close to zero) because the NHSDA survey was not performed every year. For example, persons born in 1968 would have reached age 15 in 1983. However, the NHSDA was not conducted in 1983 and so there is no NHSDA data for persons born in 1968 at age 15.
Table I.
Sample Size by Age and Birth Year for the 1968–1973 Birth Cohort (NHSDA 1982–1995)
| Birth year |
SE (P = ) |
||||||||
|---|---|---|---|---|---|---|---|---|---|
| Age | 1968 | 1969 | 1970 | 1971 | 1972 | 1973 | Total | 50% | 10% |
| 12 | 2 | 252 | 4 | 137 | 213 | 608 | 2.0 | 1.2 | |
| 13 | 269 | 4 | 116 | 215 | 1 | 605 | 2.0 | 1.2 | |
| 14 | 265 | 160 | 291 | 5 | 721 | 1.9 | 1.1 | ||
| 15 | 140 | 237 | 4 | 4 | 551 | 936 | 1.6 | 1.0 | |
| 16 | 150 | 251 | 7 | 1 | 536 | 253 | 1198 | 1.4 | 0.9 |
| 17 | 239 | 2 | 5 | 579 | 234 | 1145 | 2204 | 1.1 | 0.6 |
| 18 | 1 | 240 | 182 | 931 | 735 | 2089 | 1.1 | 0.7 | |
| 19 | 1 | 202 | 175 | 887 | 722 | 725 | 2712 | 1.0 | 0.6 |
| 20 | 166 | 149 | 852 | 686 | 808 | 563 | 3224 | 0.9 | 0.5 |
| 21 | 139 | 786 | 739 | 751 | 574 | 515 | 3504 | 0.8 | 0.5 |
| 22 | 754 | 633 | 824 | 569 | 505 | 197 | 3482 | 0.8 | 0.5 |
| 23 | 686 | 809 | 625 | 539 | 211 | 2 | 2872 | 0.9 | 0.6 |
| 24 | 848 | 594 | 579 | 265 | 2286 | 1.0 | 0.6 | ||
| 25 | 644 | 569 | 245 | 1 | 1 | 1460 | 1.3 | 0.8 | |
| Total | 3894 | 4405 | 4944 | 4875 | 4883 | 4900 | 27901 | 0.3 | 0.2 |
All estimates for prevalence rates reported in this paper were calculated using the sample weights provided with the dataset. Thus, they are representative of the U.S. household population. The precise calculation for the standard error of any estimates is complicated and requires extensive information about the intercorrelatedness of responses among cases (information that is not readily identified from the public-use data files). For the analyses presented in this paper, the calculations were further complicated by the use of multiple years of data. In lieu of complicated estimates of the standard errors, the study used a lower-bound on the standard error, which for a prevalence rate P was calculated using the following conventional formula:
Use of this formula disregards the impact of clustering and assumes that each case was independently and randomly selected from the larger population of interest. It therefore provides a lower-bound on the standard error.
This formula reaches a maximum value when the prevalence of a trait P = 50%. Table I indicates the standard error for each age specific subsample. The largest value SE = 2% is associated with the ages having the smallest samples (ages 12 and 13). This suggests that the estimated prevalence rates will be typically within 2 percentage points of the true proportion for the population, when the prevalence is close to 50%. When the prevalence is closer to 10%, the standard error is only 1.2 percentage points, which is 60% of the error for P = 50%. The standard errors for the largest subsamples (ages 19 to 24) are half as large as the standard errors for the 12- and 13-year-old subsamples.
2.3. The Rutgers Health and Human Development Project
The Rutgers Health and Human Development Project recruited adolescents through a random sampling of telephone numbers covering all but the five counties of New Jersey most distant from the test site. Successive rounds of telephone calls were carried out to fill specific quotas of 200–225 males and females aged 12, 15, or 18. Only data obtained from 12 and 15 year olds were used in this paper. Respondents were predominantly white (89%); only a few were black (8%). Participants came to the research center for a full day of testing on four occasions spanning a 13-year period (for greater detail, see Horwitz and White, 1987).
This analysis compared reports of ages at first use of alcohol (beer, wine, or liquor), tobacco cigarettes, marijuana, and hard drugs provided on two separate occasions by the same individuals. From 1979 to 1981, the project recruited and interviewed an initial sample of 12 and 15 year olds. Nearly all of these individuals (97%) were reinterviewed 3 years later at ages 15 and 18, respectively. A total of 30 individuals (3%) dropped out after the first interview. A sample of 437 individuals who were age 12 at the initial interview (referred to hereafter as the younger cohort) and 455 individuals who were age 15 (referred to hereafter as the older cohort) provided information at both occasions.
At the initial interview, individuals were asked whether they had ever tried each substance. At reinterview, individuals were asked whether they had tried or used each substance “during the last 3 years.” Those who answered yes, at either occasion, were asked, “About how old were you the first time you ever tried...?” This sequence of questions did not fully anticipate the reliability analysis presented in this paper. Individuals who had not used a substance between interviews were not asked their age at first use. Thus, some of the earliest initiators who did not continue use were excluded from analysis.
3. RESULTS
We had originally hypothesized that attrition would result in a decline in early initiators among cohort members interviewed at later ages. Indeed, the distribution of age at first use of each substance as reported by members of the 1968–1973 birth cohort to the NHSDA at ages 12, 15, and 18 as reported in Table II indicate substantial declines in early initiators with interview age of alcohol and tobacco and even with marijuana and hard drugs which were generally initiated at older ages. This decline in the percentage of early alcohol initiators was especially noticeable for the age 10 column. When interviewed at age 12, 6.8% of the 1968–1973 birth cohort reported having initiated the use of alcohol at age 10. When interviewed at age 15, only 4.2% reported having initiated use at age 10 and by interview age 18, the rate had declined to a mere 2.1%. Based on a conventional two-sided z test, the difference in the percentages from interviews at age 12 to 15 was not statistically significant (α = 0.05 level), but the overall decline from age 12 to 18 was significant at the α = 0.01 level. This represented a decrease to less than one-third of the original rate that reported first alcohol use at age 10.
Table II.
Comparison of Distribution of Age at First Use across Interviews at Ages 12, 15, and 18a
| Interview age | 0–5 | 6–8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | Total | SEb |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Percentage reporting age at first use of alcohol—NHSDA | ||||||||||||||
| 12 | 1.5 | 2.5 | 2.7 | 6.8 | 5.4 | 4.1 | 23.1 | 1.2 | ||||||
| 15 | 0.5 | 1.6 | 2.1 | 4.2 | 2.5 | 9.4 | 16.8 | 14.1 | 8.8 | 60.1 | 1.0 | |||
| 18 | 0.8 | 0.8 | 0.8 | 2.1 | 2.0 | 4.5 | 10.1 | 12.7 | 13.0 | 18.2 | 10.2 | 3.3 | 78.7 | 0.7 |
| Percentage reporting age at first use of alcohol—Rutgers Project | ||||||||||||||
| 12-Y | 6.5 | 15.4 | 6.9 | 8.1 | 4.3 | 0.9 | 42.1 | 1.4 | ||||||
| 15-Y | 6.7 | 12.3 | 5.1 | 12.1 | 6.0 | 9.4 | 9.6 | 3.8 | 1.8 | 66.9 | 1.4 | |||
| 15-O | 9.9 | 17.3 | 5.1 | 16.6 | 5.5 | 12.0 | 12.2 | 4.6 | 0.8 | 84.0 | 1.4 | |||
| 18-O | 4.0 | 16.2 | 2.9 | 13.3 | 3.6 | 12.2 | 10.5 | 10.5 | 8.4 | 4.8 | 1.7 | 0.4 | 88.6 | 1.4 |
| Percentage reporting age at first use of tobacco—NHSDA | ||||||||||||||
| 12 | 1.5 | 4.7 | 4.8 | 4.8 | 7.3 | 2.7 | 25.6 | 1.2 | ||||||
| 15 | 1.3 | 5.8 | 1.4 | 4.4 | 5.4 | 9.0 | 7.3 | 10.2 | 1.8 | 46.6 | 1.0 | |||
| 18 | 1.2 | 4.3 | 2.4 | 5.5 | 3.9 | 7.5 | 8.4 | 7.9 | 7.7 | 7.5 | 5.0 | 1.1 | 62.4 | 0.7 |
| Percentage reporting age at first use of tobacco—Rutgers Project | ||||||||||||||
| 12-Y | 2.5 | 2.7 | 4.3 | 3.6 | 0.7 | 13.6 | 1.4 | |||||||
| 15-Y | 0.2 | 4.5 | 1.8 | 3.1 | 4.0 | 10.1 | 10.1 | 6.0 | 1.6 | 41.4 | 1.4 | |||
| 15-O | 5.5 | 4.8 | 9.5 | 7.4 | 12.0 | 11.6 | 5.9 | 1.1 | 57.7 | 1.4 | ||||
| 18-O | 4.0 | 2.3 | 5.5 | 4.4 | 8.2 | 9.1 | 6.9 | 5.5 | 5.3 | 2.3 | 1.1 | 54.7 | 1.4 | |
| Percentage reporting age at first use of marijuana—NHSDA | ||||||||||||||
| 12 | 0.1 | 0.5 | 2.0 | 0.2 | 2.7 | 1.2 | ||||||||
| 15 | 0.4 | 0.6 | 0.2 | 0.8 | 1.4 | 2.9 | 5.7 | 7.4 | 4.9 | 24.4 | 1.0 | |||
| 18 | 0.4 | 1.0 | 0.9 | 0.7 | 1.8 | 5.2 | 4.7 | 7.1 | 6.7 | 6.6 | 2.6 | 37.7 | 0.7 | |
| Percentage reporting age at first use of marijuana—Rutgers Project | ||||||||||||||
| 12-Y | 0.2 | 0.7 | 0.9 | 0.9 | 2.7 | 1.4 | ||||||||
| 15-Y | 0.2 | 1.1 | 0.7 | 1.6 | 3.1 | 9.4 | 9.2 | 2.5 | 27.7 | 1.4 | ||||
| 15-O | 0.4 | 0.2 | 1.1 | 3.6 | 7.4 | 15.2 | 15.2 | 3.4 | 46.3 | 1.4 | ||||
| 18-O | 0.2 | 0.4 | 0.6 | 1.1 | 0.8 | 7.6 | 8.4 | 11.6 | 12.4 | 10.9 | 4.8 | 1.1 | 60.0 | 1.4 |
| Percentage reporting age at first use of hard drugs—NHSDA | ||||||||||||||
| 12 | 0.1 | 0.2 | 1.2 | |||||||||||
| 15 | 0.2 | 0.2 | 2.0 | 2.8 | 5.3 | 1.0 | ||||||||
| 18 | 0.1 | 0.8 | 0.7 | 1.3 | 2.2 | 2.3 | 1.0 | 8.4 | 0.7 | |||||
| Percentage reporting age at first use of hard drugs—Rutgers Project | ||||||||||||||
| 12-Y | 1.4 | |||||||||||||
| 15-Y | 0.2 | 0.4 | 0.9 | 0.9 | 2.5 | 1.4 | ||||||||
| 15-O | 0.2 | 0.2 | 0.4 | 1.3 | 0.8 | 2.9 | 1.4 | |||||||
| 18-O | 0.2 | 0.4 | 1.9 | 5.1 | 10.7 | 1.7 | 20.0 | 1.4 | ||||||
Y indicates the younger cohort, O indicates the older cohort in the Rutgers Project.
Standard error for a typical prevalence rate P = 10%.
On the other hand, a visual comparison of the types of declines in early initiators with data from the Rutgers Project provided support for the alternative hypothesis, that the apparent “attrition” may have actually been the result of forward telescoping. In addition to the NHSDA data, Table II presents the distributions for reported age at first use of each substance for the Rutgers Project. Overall, a visual inspection suggested that the declines in the percentages of each sample reporting first use at an early age were similar. (Section 3.1 describes such a comparison.) Based on these findings, it was difficult to ascertain with much precision the extent to which the observed decline in early alcohol use across interview years for the 1968–1973 NHSDA birth cohort resulted from forward telescoping. However, this limited comparison supported the idea that most of the observed decline could have resulted from forward telescoping (rather than attrition).
3.1. Comparison of NHSDA and Rutgers Project Data
For individuals from the Rutgers Project who reported having used alcohol at both interviews, extensive forward telescoping occurred in their responses. For the younger cohort, the mean difference in age at first use reported from age 12 to 15 was 1.2 years. For the older cohort, the difference from age 15 to 18 was 1.4 years. Adding these together suggests that from age 12 to 18 on average, the early initiators increased their age at first use by an average of 2.6 years. There was somewhat less telescoping in reported age at first use of tobacco and marijuana. Too few of the Rutgers interviewees reported having used hard drugs for an accurate comparison.
This forward telescoping in age at first use of alcohol was associated with a substantial decline in the percentage of early initiators. A much larger percentage of the Rutgers Project sample (42.1%) than the NHSDA sample (23.1%) reported having used alcohol when interviewed at age 12. This difference was most probably due to differences in the birth year and location of recruitment between the samples. A comparison of the distributions for age at first use of alcohol identified a decline in the percentage of early alcohol users with interview age for the Rutgers Project. This decline was especially noticeable for the age 9 column. Among the 12 year olds in the younger cohort, 6.9% reported having initiated alcohol use at age 9. This rate declined moderately to 5.1% when reinterviewed at age 15. Based on a standard z test, this difference was not statistically significant (α = 0.05 level), not because it was not substantial but because there were too few cases in the Rutgers Project data to detect whether a difference of this size was significant.
The older cohort in the Rutgers Project reported a higher rate of early alcohol use. At age 15, 84.0% of the older cohort reported having initiated alcohol use as compared to 66.9% of the younger cohort (at age 15). For the older cohort, the same percentage 5.1% reported having initiated use at age 9 when interviewed at age 15. At the time of their reinterview at age 18, only 2.9% reported having initiated use at age 9. Again, this difference was not statistically significant (α = 0.05 level). However, the difference between the 6.9% for the younger cohort at age 12 and the 2.9% for the older cohort at age 18 was statistically significant at the α = 0.01 level.
The reported rates of early tobacco use also declined substantially with increases in interview age, although the decrease was slightly less pronounced than it was for alcohol. It was particularly noticeable in the age 11 column (Table II). When interviewed at age 12, 7.3% of the 1968–1973 NHSDA cohort reported having initiated use of tobacco by age 11. This percentage declined to 5.4% at age 15 and then 3.9% at age 18. The difference from interview ages of 12 to 15 was not statistically significant (α = 0.05 level), but the overall decline from age 12 to 18 was significant at the α = 0.01 level.
Similar declines prevailed in the age 10 column for the data from the Rutgers Project. From age 12 to 15, the percentage reporting having started tobacco use at age 10 declined by a quarter from 4.3 to 3.1% (not statistically significant, α = 0.05 level). From age 15 to age 18, the percentage was almost half, a decline from 9.5 to 5.5% (statistically significant, α = 0.05 level).
The percentage of NHSDA respondents at age 18 who reported ever using marijuana (37.7%) and hard drugs (8.4%) was much lower than the reported rates for alcohol (78.7%) and tobacco (62.4%). Consistent with prior research, extremely few individuals reported having initiated use of marijuana or hard drugs before the midteens. Some declines in the percentage reporting marijuana initiation at ages 12 and 14 occurred between the interviews at age 15 and age 18. The decline in the age 12 column was not statistically significant, the decline from 7.4 to 4.7% in the age 14 column was significant at the α = 0.01 level. Some declines in the percentage reporting first use of hard drugs at ages 14 and 15 occurred between the interviews at age 15 and age 18, but they were not statistically significant.
3.2. Distributions of Age at First Use Corrected for Forward Telescoping
Tables IIIa through IIId present the distribution of age at first use of alcohol, tobacco, marijuana, and hard drugs, respectively, as reported by the 1968–1973 NHSDA birth cohort at ages 12 through 25. The second-to-last row of numbers in each table presents the cumulative distribution of age at first use derived from the 1982–1995 interview years. The last row of numbers, the “corrected” distribution, was estimated by taking the difference between successive entries in the cumulative distribution. The two rightmost columns present average ages at first use for different interview ages. For these calculations, all reports of age at first use of less than 11 were rounded up to 11. The second column from the right (“Rep”) presents the average age at first use retrospectively reported in the NHSDA survey (not corrected). The rightmost column (“Cor”) presents the corresponding average age based upon the “corrected” distribution of responses. The changes in the “corrected” average age (the rightmost column) essentially controls for the influence of forward telescoping. Thus, the difference between the two rightmost columns indicates the impact of forward telescoping on the average age at first use for each age at interview.
Table IIIa.
The Distribution of Age at First Use of Alcohol by Interview Year Compared with a Multiyear “Corrected” Distribution (NHSDA 1982–1995, 1968–1973 Birth Cohort)
| Interview age | Retrospective report of age at first use of alcohol |
Avg. age |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 12a | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | Rep. | Corr. | |
| 12 | 18.9 | 11.0 | 11.0 | |||||||||||||
| 13 | 20.7 | 12.9 | 11.4 | 11.4 | ||||||||||||
| 14 | 18.1 | 10.1 | 17.0 | 12.0 | 11.8 | |||||||||||
| 15 | 11.0 | 9.4 | 16.8 | 14.1 | 12.7 | 12.1 | ||||||||||
| 16 | 7.7 | 7.7 | 10.5 | 18.5 | 17.3 | 13.5 | 12.6 | |||||||||
| 17 | 8.1 | 5.8 | 8.0 | 13.7 | 19.2 | 15.9 | 14.1 | 13.0 | ||||||||
| 18 | 6.7 | 4.5 | 10.1 | 12.7 | 13.0 | 18.2 | 10.2 | 14.5 | 13.3 | |||||||
| 19 | 6.7 | 6.4 | 8.3 | 10.4 | 14.5 | 17.2 | 11.0 | 8.5 | 14,9 | 13.7 | ||||||
| 20 | 6.0 | 5.3 | 7.6 | 10.4 | 15.7 | 16.2 | 10.6 | 10.3 | 3.1 | 15.2 | 13.8 | |||||
| 21 | 5.2 | 4.8 | 5.3 | 10.4 | 14.1 | 18.4 | 11.7 | 9.8 | 4.4 | 2.2 | 15.5 | 13.9 | ||||
| 22 | 5.8 | 4.8 | 6.3 | 10.1 | 13.5 | 17.2 | 9.3 | 10.7 | 3.8 | 3.3 | 3.8 | 15.7 | 14.1 | |||
| 23 | 5.4 | 5.7 | 7.1 | 9.3 | 12.3 | 15.5 | 9.0 | 10.9 | 4.8 | 4.0 | 4.7 | 0.8 | 15.9 | 14.2 | ||
| 24 | 6.5 | 3.4 | 6.6 | 8.9 | 13.0 | 17.5 | 9.6 | 10.0 | 5.0 | 2.6 | 4.9 | 0.9 | 0.7 | 15.9 | 14.2 | |
| 25 | 5.3 | 4.1 | 4.8 | 9.7 | 13.1 | 18.3 | 8.9 | 12.4 | 4.9 | 2.0 | 4.6 | 1.5 | 0.8 | 0.2 | 16.1 | 14.3 |
| Cum. | 18.9 | 33.7 | 45.2 | 51.3 | 61.6 | 70.7 | 75.4 | 83.0 | 85.3 | 86.2 | 88.9 | 89.6 | 89.7 | 90.6 | ||
| Corr. | 18.9 | 14.7 | 11.6 | 6.1 | 10.3 | 9.1 | 4.7 | 7.5 | 2.4 | 0.9 | 2.7 | 0.7 | 0.2 | 0.9 | ||
Reports of initiation prior to age 11 were rounded up to 11.
Table IIId.
The Distribution of Age at First Use of Hard Drugs by Interview Year Compared with a Multiyear “Corrected” Distribution (NHSDA 1982–1995, 1968–1973 Birth Cohort)
| Interview age | Retrospective report of age at first use of hard drugs |
Avg. age |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 12a | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | Rep. | Corr. | |
| 12.0 | 0.1 | 11.0 | 11.0 | |||||||||||||
| 13.0 | 0.1 | 11.0 | 11.0 | |||||||||||||
| 14.0 | 0.3 | 2.0 | 12.7 | 12.9 | ||||||||||||
| 15.0 | 0.2 | 0.2 | 2.0 | 13.7 | 13.0 | |||||||||||
| 16.0 | 0.4 | 0.1 | 0.4 | 0.8 | 2.0 | 14.1 | 13.6 | |||||||||
| 17.0 | 0.1 | 0.1 | 0.4 | 0.5 | 1.7 | 2.5 | 15.1 | 14.4 | ||||||||
| 18.0 | 0.0 | 0.1 | 0.8 | 0.7 | 1.3 | 2.2 | 2.3 | 15.6 | 15.1 | |||||||
| 19.0 | 0.0 | 0.2 | 0.4 | 0.8 | 1.2 | 2.9 | 4.1 | 2.6 | 16.4 | 16.2 | ||||||
| 20.0 | 0.2 | 0.2 | 0.5 | 0.4 | 1.3 | 2.8 | 2.4 | 3.1 | 2.0 | 16.7 | 16.4 | |||||
| 21.0 | 0.1 | 0.1 | 0.1 | 0.5 | 1.2 | 1.8 | 2.8 | 1.8 | 2.5 | 2.0 | 17.4 | 16.4 | ||||
| 22.0 | 0.2 | 0.0 | 0.3 | 0.6 | 1.1 | 1.9 | 2.5 | 2.9 | 2.2 | 1.4 | 0.9 | 17.5 | 16.8 | |||
| 23.0 | 0.0 | 0.2 | 1.1 | 1.3 | 2.2 | 1.8 | 2.4 | 1.5 | 1.2 | 1.7 | 0.8 | 17.8 | 16.8 | |||
| 24.0 | 0.1 | 0.2 | 0.4 | 1.1 | 0.9 | 2.8 | 1.8 | 2.1 | 1.9 | 2.3 | 1.0 | 1.2 | 1.1 | 18.1 | 17.8 | |
| 25.0 | 0.1 | 0.3 | 0.3 | 0.7 | 1.5 | 2.6 | 3.1 | 1.4 | 2.1 | 1.1 | 0.6 | 0.4 | 0.5 | 18.4 | 17.8 | |
| Cum. | 0.1 | 0.1 | 2.2 | 2.4 | 3.7 | 5.3 | 7.5 | 12.1 | 12.9 | 12.8 | 14.2 | 14.2 | 16.9 | 14.6 | ||
| Corr. | 0.1 | 0.0 | 2.2 | 0.2 | 1.2 | 1.7 | 2.2 | 4.7 | 0.8 | 0.0b | 1.3 | 0.0 | 2.7 | 0.0b | ||
Reports of initiation prior to age 11 were rounded up to 11.
The cumulative percentage was lower than in a previous year. It was estimated that virtually no one initiated use at this age.
3.1.1. Alcohol
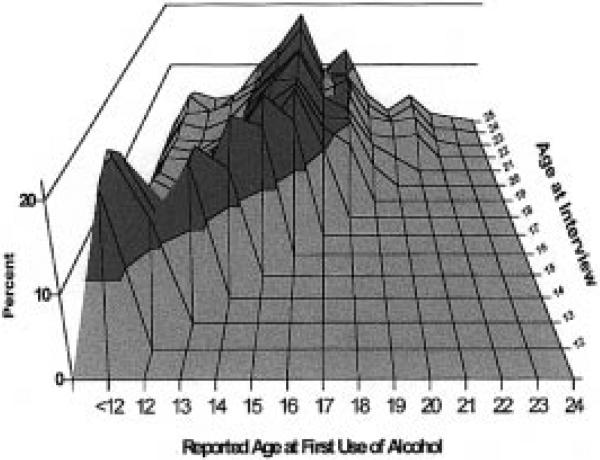
Table IIIa indicates how many fewer individuals reported early initiation of alcohol use at successive interview ages. Figure 1 provides a graphical presentation of the same information with the youngest interviews represented on the bottom of the 3D-surface plot and the oldest at the top. Many youths (18.1–20.7%) interviewed at ages 12–14 reported having initiated use of alcohol before age 12. However, older respondents were highly unlikely to report such early initiation. Figure 1 shows a flattening of the surface associated with reported early alcohol use with increased age at interview. Figure 1 also shows a moving ridge line in which the peak age of reported initiation moves forward (toward older ages) with increased age at interview. As discussed previously, this decline could have been primarily the result of forward telescoping. At each interview age, the distribution of reported age at first use follows a roughly unimodal distribution with the peak age increasing each year until age 18. Individuals interviewed at age 18 and after reported a modal age at first use of alcohol of 16. For older interview ages, two additional but smaller peaks start to appear at ages 18 and 21. The “corrected” distribution identifies four peak periods of alcohol initiation: prior to age 12 (18.9%), age 15 (10.3%), age 18 (7.5%), and age 21 (2.7%). The peak at age less than 12 most likely resulted from having grouped all ages from 1 to 11 together into a single category. However, it is worth highlighting this finding because of the stark contrast in the proportion reporting early alcohol initiation among young respondents compared to older interviewees. The second peak of the corrected distribution indicates somewhat more individuals initiating at age 15 than age 16. Again, this stands in contrast to the reports of older arrestees who were much more likely to report initiation at age 16. The corrected distribution shows two smaller yet distinct peaks at ages 18 and 21. However, the height of these peaks are much lower than reported by respondents at later interview ages, in compensation for the increased proportion identified as initiating prior to age 12.
Fig. 1.
Variation in reported age at first use of alcohol with interview year (NHSDA 1982–1995, 1968–1973 birth cohort).
The average age at first use of alcohol exhibited a modest increase at each interview age up until the early twenties. This increase resulted from both individuals reporting first use of alcohol at each successive age and forward telescoping. At age 18, this difference was 1.2 years. This amount was substantially less than the 2.6 years of forward telescoping estimated with data from the Rutgers Project by comparing those individuals who reported use at both interviews (Golub et al., 1999). Clearly, the impact of forward telescoping among the earliest reported users of alcohol was partially offset by individuals who first initiated the use of alcohol between age 12 and age 18. By age 25, the impact of forward telescoping had crept up to 1.8 years. The distribution of ages at retrospectively reported first use of alcohol among 25 year olds had a mean of 16.1 years and a mode of 16 years. The mean age for the “corrected” distribution was only 14.3 years.
3.1.2. Tobacco
The decline across interview ages in reported age at first use of tobacco (Table IIIb) was substantial but smaller than observed with alcohol. The distribution of age at first use of tobacco reported by respondents interviewed at ages 12 to 20 typically peaked by age 11 or 12 and declined slowly in the teens. By the time of the age 21 interview, a second peak at age 16 emerged. The “corrected” distribution showed a peak period of first tobacco use occurring at age 13 or younger and then a smaller peak around ages 15–16. Much fewer individuals reported first initiating tobacco use after age 18.
Table IIIb.
The Distribution of Age at First Use of Tobacco by Interview Year Compared with a Multiyear “Corrected” Distribution (NHSDA 1982–1995, 1968–1973 Birth Cohort)
| Interview age | Retrospective report of age at first use of tobacco |
Avg. age |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 12a | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | Rep. | Corr. | |
| 12 | 22.9 | 11.0 | 11.0 | |||||||||||||
| 13 | 23.2 | 8.7 | 11.3 | 11.3 | ||||||||||||
| 14 | 25.3 | 8.7 | 7.7 | 11.6 | 11.7 | |||||||||||
| 15 | 18.3 | 9.0 | 7.3 | 10.2 | 12.2 | 11.8 | ||||||||||
| 16 | 15.1 | 10.3 | 9.7 | 7.8 | 8.0 | 12.7 | 12.2 | |||||||||
| 17 | 16.9 | 8.6 | 8.6 | 7.8 | 9.2 | 5.7 | 13.0 | 12.6 | ||||||||
| 18 | 17.2 | 7.5 | 8.4 | 7.9 | 7.7 | 7.5 | 5.0 | 13.4 | 12.9 | |||||||
| 19 | 16.2 | 9.3 | 7.9 | 8.0 | 8.1 | 8.0 | 5.1 | 3.7 | 13.7 | 13.3 | ||||||
| 20 | 16.2 | 8.3 | 7.7 | 8.7 | 7.9 | 7.6 | 5.1 | 3.5 | 2.8 | 13.9 | 13.5 | |||||
| 21 | 13.0 | 8.0 | 8.8 | 7.4 | 7.7 | 9.8 | 4.7 | 5.4 | 2.8 | 2.2 | 14.4 | 13.6 | ||||
| 22 | 13.0 | 8.8 | 6.9 | 7.5 | 8.5 | 9.2 | 5.4 | 5.0 | 2.7 | 2.7 | 1.1 | 14.5 | 13.7 | |||
| 23 | 11.6 | 7.4 | 5.8 | 6.7 | 7.0 | 8.5 | 6.4 | 6.8 | 2.4 | 2.7 | 2.0 | 0.4 | 14.9 | 13.7 | ||
| 24 | 11.5 | 8.4 | 7.6 | 8.3 | 7.8 | 10.6 | 5.4 | 4.8 | 1.8 | 1.5 | 1.2 | 1.5 | 0.4 | 14.7 | 13.7 | |
| 25 | 10.0 | 7.2 | 10.0 | 7.3 | 9.8 | 11.2 | 4.0 | 4.2 | 1.6 | 1.5 | 2.0 | 1.0 | 0.3 | 1.4 | 14.9 | 13.9 |
| Cum. | 22.9 | 31.9 | 41.7 | 44.8 | 50.8 | 56.8 | 61.3 | 66.4 | 68.0 | 69.9 | 70.9 | 67.8b | 70.8b | 71.7 | ||
| Corr. | 22.9 | 9.0 | 9.8 | 3.0 | 6.1 | 5.9 | 4.5 | 5.1 | 1.6 | 1.9 | 1.1 | 0.0 | 0.0 | 0.8 | ||
Reports of initiation prior to age 11 were rounded up to 11.
The cumulative percentage was lower than in a previous year. It was estimated that virtually no one initiated use at this age.
The distribution of age at first use of tobacco retrospectively reported at age 18 was similar to the “corrected” distribution derived from the interviews from age 12 through 18. This is reflected in the comparison of average age at first use reported each year with the average estimated from the “corrected” distribution. At age 18, the average age at reported first use of tobacco was 13.4 years, compared to 12.9 years for the analogous portion of the “corrected” distribution. By the time of the age 25 interview, this gap due to forward telescoping had widened to an entire year (14.9 versus 13.9 years of age).
3.1.3. Marijuana
The distribution of age at first use of marijuana was quite consistently reported at interviews from age 12 through age 20 (Table IIIc). For each interview age, the distribution was relatively uniform as opposed to having a large peak. Most of the respondents initiated marijuana use between age 12 and age 18. The difference in the average age reported at each interview age and the average derived from the appropriate portion of the “corrected” distribution was typically negligible (less than half a year). Starting with age 21, the impact of forward telescoping began to increase. The difference between the reported and the “corrected” average age at first use reached a maximum of 0.7 years for those interviewed at age 25.
Table IIIc.
The Distribution of Age at First Use of Marijuana by Interview Year Compared with a Multiyear “Corrected” Distribution (NHSDA 1982–1995, 1968”1973 Birth Cohort)
| Interview age | Retrospective report of age at first use of marijuana |
Avg. age |
||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| < 12a | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 | 21 | 22 | 23 | 24 | Rep. | Corr. | |
| 12 | 2.6 | 11.0 | 11.0 | |||||||||||||
| 13 | 4.2 | 3.5 | 11.5 | 11.7 | ||||||||||||
| 14 | 3.2 | 4.5 | 4.2 | 12.1 | 12.1 | |||||||||||
| 15 | 3.5 | 2.9 | 5.7 | 7.4 | 12.9 | 12.9 | ||||||||||
| 16 | 3.3 | 3.2 | 3.8 | 6.2 | 8.8 | 13.6 | 13.4 | |||||||||
| 17 | 2.3 | 2.7 | 3.9 | 5.2 | 7.5 | 7.7 | 14.2 | 13.7 | ||||||||
| 18 | 3.0 | 1.8 | 5.2 | 4.7 | 7.1 | 6.7 | 6.6 | 14.6 | 14.3 | |||||||
| 19 | 3.0 | 3.9 | 4.8 | 5.5 | 6.3 | 9.3 | 7.7 | 4.7 | 15.0 | 15.1 | ||||||
| 20 | 3.0 | 1.8 | 3.9 | 5.6 | 6.2 | 8.4 | 5.8 | 6.4 | 2.8 | 15.4 | 15.1 | |||||
| 21 | 2.3 | 2.0 | 3.7 | 5.1 | 5.8 | 9.6 | 6.8 | 7.9 | 3.6 | 2.4 | 15.9 | 15.5 | ||||
| 22 | 1.8 | 2.0 | 3.4 | 6.0 | 6.3 | 8.0 | 6.2 | 6.5 | 3.4 | 1.5 | 1.5 | 15.9 | 15.5 | |||
| 23 | 1.6 | 2.4 | 3.6 | 4.7 | 5.2 | 8.8 | 6.1 | 6.0 | 3.0 | 2.3 | 2.7 | 0.3 | 16.2 | 15.5 | ||
| 24 | 1.8 | 2.9 | 3.9 | 5.6 | 5.8 | 8.3 | 7.1 | 6.6 | 2.5 | 2.5 | 1.0 | 1.2 | 0.5 | 16.1 | 15.5 | |
| 25 | 1.9 | 2.2 | 3.3 | 3.1 | 7.4 | 10.7 | 6.9 | 5.7 | 3.0 | 1.4 | 1.0 | 1.1 | 0.5 | 0.3 | 16.2 | 15.5 |
| Cum. | 2.6 | 7.7 | 11.9 | 19.5 | 25.3 | 29.4 | 35.1 | 45.1 | 43.9 | 49.3 | 46.7 | 46.7 | 49.5 | 48.5 | ||
| Corr. | 2.6 | 5.1 | 4.2 | 7.7 | 5.7 | 4.1 | 5.8 | 10.0 | 0.0a | 4.1 | 0.0b | 0.0b | 0.3 | 0.0 | ||
Reports of initiation prior to age 11 were rounded up to 11.
The cumulative percentage was lower than in a previous year. It was estimated that virtually no one initiated marijuana use at this age.
3.1.4. Hard Drugs
Relatively few individuals (less than 20%) reported having ever used any hard drugs by age 24 (Table IIId). The peak age of initiation, based on the “corrected” distribution, was 18. The difference in the average age as reported at each age and the “corrected” index exhibited substantial variation as a result of the small sample of hard drug users. The average age at first use of 12.7 reported at age 15 was actually slightly less than the average age of 12.9 estimated from the “corrected” distribution. At age 16, the average age at first use of hard drugs jumped to 13.7 which was more than a half-year larger than the average age estimated from the “corrected” distribution. A similar difference occurred with interviews at ages 17 and 18. However, the gap closed to a few tenths for the subsequent interview ages, 19 and 20, and subsequently widened to close to a year among the 21 to 25 year old interviewees. These findings suggest that there might have been moderate telescoping in the age at first hard drug use, although it was probably less than a year.
4. DISCUSSION
The distributions of age at first use of alcohol, tobacco, marijuana, and hard drugs as retrospectively reported to the NHSDA can be influenced by a variety of biases including sample selection, nondisclosure, and forward telescoping. This paper examined the relative impact of attrition and forward telescoping in the NHSDA by comparing the responses to data obtained from a longitudinal sample. The findings were consistent with the idea that what appeared to be substantial attrition from the sampling frame, especially for alcohol, could potentially be explained by forward telescoping. Clearly, additional comparisons with other longitudinal data would help to determine more precisely whether any attrition did occur, net of the impact of forward telescoping. Section 4.2 describes important directions for further research.
The retrospectively reported ages at first use in the NHSDA data can be corrected, straightforwardly, for either forward telescoping or attrition by viewing data collected in successive years as providing a repeated cross-section study for a birth cohort. Correcting for both biases simultaneously would require an accurate understanding of the size of the bias from each, a task that is beyond the scope of this paper. This paper employed a procedure for correcting for forward telescoping, but not attrition. The resulting distribution, like the NHSDA, still only pertains to those members of a birth cohort growing up in the type of households that are typically sampled by and respond to the program. This characteristic of the findings could be considered an important strength. Household residents represent the primary clientele for many practitioners in the substance abuse prevention and education fields. It might be best to use other data sources for the study of populations traditionally underrepresented by the NHSDA, such as surveys of individuals growing up in inner-city poverty-stricken neighborhoods (Golub and Johnson, forthcoming).
The “corrected” distribution is also limited by the extent to which individuals might not disclose whether they had ever used each substance. This seems like less of a problem with alcohol and tobacco because nearly all adults reported having initiated their use to the NHSDA. Nondisclosure may be more of a problem with marijuana and hard drugs due to their illegality and the stigma associated with their use.
The “corrected” distribution for age at first use of alcohol suggested that responses to the NHSDA by members of the 1968–1973 birth cohort were seriously distorted by forward telescoping. When interviewed at each successive age, substantially fewer of them reported first use of alcohol by 15. When interviewed at age 25, the average reported age at first use of alcohol was 16.1, compared to age 14.3 as estimated from the “corrected” distribution, a difference of close to 2 years. Perhaps even more importantly, the retrospective reports by 25 year olds indicated a modal age at first use of alcohol of 16. In contrast, the “corrected” distribution identified multiple peak ages for initial alcohol use at <12, 15, 18, and 21. The implications of this finding are discussed in Section 4.1.
The bias in the retrospectively reported age at first use of tobacco was somewhat less extensive. When interviewed at age 25, the average reported age at first use of tobacco was 14.9, compared to 13.9 as estimated from the corrected distribution, a difference of only 1 year. Interestingly, the analyses suggested that there was substantially less telescoping in age at first use of marijuana and of hard drugs. The difference between the average ages estimated with the interviews at age 25 and the “corrected” distribution was 0.7 year (16.2–15.5 years) for marijuana and 0.6 year (18.4–17.8 years) for hard drugs. The somewhat greater accuracy in retrospective recall may have been the result of individuals having initiated their use of marijuana and hard drugs at a later age. Alternatively, research suggests that accurate recall may be related to the saliency of the event (Eisenhower et al., 1991). In this regard, for those individuals who have used marijuana or hard drugs the specifics of the occasion at which they first used each may tend to be a more memorable event.
One possible response to these findings might be to eschew the use of retrospective data as biased in favor of the use of longitudinal panel data. Certainly, caution is in order. However, as the nature and extent of the bias become better understood, such limitations can be directly controlled in more sophisticated analyses. A very important use for longitudinal data is to measure and correct for biases in retrospectively reported data. In this manner, advances in the analysis of longitudinal data can contribute greatly to the usefulness of the massive amount of cross-sectional data being collected on an ongoing basis.
4.1. The Impact of Forward Telescoping
The existence of extensive forward telescoping in reported age at first use has direct implications for providers of substance abuse prevention programs and for policy analysts. Several scholars have suggested that individuals who initiate alcohol and/or tobacco use at an early age are more likely to progress to use of illicit drugs and more likely to manifest problem use of any substance (Funkhouser et al., 1992; Grant, 1998; Grant and Dawson, 1997; Hawkins et al., 1992; Kandel, 1978; Mills and Noyes, 1984). Cross-cultural studies, however, suggest that early exposure to “culturally acceptable” use of alcohol can help individuals learn to use alcohol and avoid subsequent problem use (Hanson, 1996). Indeed, Labouvie et al. (1997) using the Rutgers Project data found only a weak association between age at onset and subsequent problem use, too weak to be of any clinical use.
Accurately determining whether early alcohol use is a risk or a protective factor in America today and for whom, requires being able to accurately measure an individual's age at first use. A simple retrospective report of age at first use of alcohol may be insufficient for this purpose. Golub et al. (forthcoming) found that the standard deviation in the difference in reported ages at first use of alcohol was over 3 years using the Rutgers Project data (the responses for other substances were somewhat more reliable). The unreliability of this response should severely limit its utility (at least by itself) for prediction of individual outcomes and assignment to prevention or treatment programs. Even if early initiation is a risk factor for problem use, forward telescoping could further limit the usefulness of this factor. In articular, some individuals evaluated at a relatively early age would be identified as seriously “at risk” for problem use because they reported an early age of initiation. However, many of these same individuals when evaluated at a later age would provide a later age at initiation and therefore not be identified as “at risk.” Thus, practitioners must consider an individual's age at the time of interview when evaluating a reported age at first use.
Perhaps the most obvious use of the distribution for first use is in determining the appropriate timing for alcohol awareness programs. In this regard, a difference of 1 or 2 years in the modal age at first use makes an important difference, if programs are to be introduced just before the age when individuals tend to start use. For example, the responses by respondents at age 25 suggests that the modal ages for first alcohol use are 15 and 16. Based on this information, alcohol awareness programs might be introduced to 14 year olds in seventh and eighth grades. However, the “corrected” distribution suggests that there are multiple waves of alcohol initiation prevailing around ages <12, 15, 18, and 21. Perhaps it is persons under age 12 that are most at risk of subsequent problem use. In this case, alcohol awareness programs would be more appropriately targeted at 10 years olds in fourth and fifth grades.
Similarly, these “corrected” distributions suggest that much more initial tobacco use occurs during the elementary school years than might otherwise be thought using uncorrected distributions. The modal age at first marijuana use based on the “corrected” distribution is closer to 14 years than the 16-year-old mode reported by 25-year-old interviewees. The modal age at first hard drug use appears to be accurately reported as about 18 years old.
Another potential impact of forward telescoping involves the evaluation of trends in substance use across successive birth cohorts. Forward telescoping can easily cause an analyst to misinterpret a cross-sectional study as suggesting that an increase in problem drug use is imminent. For example, a comparison of the reported age at first use by individuals who are currently age 15 with those who are now 25 would likely indicate that individuals coming of age today are starting substance use at an earlier age, even if they are not. (The average age at first use reported by 25 year olds would be artificially high due to forward telescoping.) For this analysis, a more appropriate comparison would be the reported age at first use of individuals age 15 today with the reported age at first use of individuals age 15 provided 10 years ago. Such data are now routinely available from the NHSDA and Monitoring the Future Programs.
4.2. Directions for Further Research
Clearly, further research is needed into biases in self-reported age at first use. Additional analyses with longitudinal data are needed to determine the extent to which the observed decline in early initiators in the NHSDA is due to attrition from the sampling frame or forward telescoping. Unfortunately, most longitudinal studies we have learned about did not reask subjects about their age at first use; rather, they asked about any prior use at the first interview and then asked about any recent use at subsequent interviews. In this regard, we would be pleased to hear from anyone who has appropriate longitudinal data in which the same respondents were asked to indicate their age at first use of various substances at two or more occasions.
Additionally, there is the question of nonresponse. Further research is needed to determine the extent to which individuals disclose lifetime use of various substances and those individual attributes associated with nondisclosure. Perhaps use of biological tests like hair samples that have the potential for detecting use in the last several months could be used to develop such insights.
Not only is it important to identify the impact of various potential biases on widely used survey data like the NHSDA, if the impacts are large, then it is also important to determine whether the biases tend to shift over time or not. For those biases that are large and can shift over time, procedures should be instituted to identify substantial shifts as they occur. So far, the bias caused by forward telescoping appears to be substantial, although it is not clear to what extent it has changed with time. Further research is needed to determine if the impact of attrition and nondisclosure of lifetime use (net of forward telescoping) are substantial enough to warrant continual monitoring.
ACKNOWLEDGMENTS
This research was supported by grants from the Robert Wood Johnson Foundation's Substance Abuse Policy Program (033027), the National Institute on Drug Abuse (DA-03395), and the National Institute on Alcohol Abuse and Alcoholism (AA-05823). Points of view and opinions expressed do not necessarily reflect the positions of these funding organizations, National Development and Research Institutes, or the Center of Alcohol Studies, Rutgers University.
REFERENCES
- Bailey SL, Flewelling RL, Rachal JV. The characterization of inconsistencies in self-reports of alcohol and marijuana use in a longitudinal study of adolescent. J. Stud. Alc. 1992;53:636–647. doi: 10.15288/jsa.1992.53.636. [DOI] [PubMed] [Google Scholar]
- Biemer PP, Witt M. Repeated measures estimation of measurement bias for self-reported drug use with applications to the National Household Survey on Drug Abuse. In: Harrison L, Hughes A, editors. Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates, NIDA Research Monograph 167. 1997. pp. 439–476. NIH Publication No. 97-4147. [PubMed] [Google Scholar]
- Brewer WF. Memory for randomly sampled autobiographical events. In: Neisser U, Winograd E, editors. Remembering Reconsidered: Ecological and Traditional Approaches to the Study of Memory. Cambridge; New York: 1988. pp. 21–90. [Google Scholar]
- Eisenhower D, Mathiowetz NA, Morganstein D. Recall error: sources and bias reduction techniques. In: Biemer PP, Groves RM, Lyberg LE, Mathiowetz NA, Sudman S, editors. Measurement Errors in Surveys. Wiley; New York: 1991. pp. 127–144. [Google Scholar]
- Elliott DS. Longitudinal research in criminology. Promise and practice (unpublished manuscript) 1992.
- Fendrich M, Vaughn CM. Diminished lifetime substance use over time: An inquiry into differential underreporting. Public Opin. Q. 1994;58:96–123. [Google Scholar]
- Funkhouser JE, Goplerud EN, Bass RO. The current status of prevention strategies. In: Jansen MA, editor. A Promising Future: Alcohol and Other Drug Problem Prevention Services Improvement. Government Printing Office; Washington, DC: 1992. pp. 17–82. OSAP Prevention Monograph No. 10, DHHS Publication No. (ADM) 92-1807. [Google Scholar]
- General Accounting Office (GAO) Drug Use Measurement: Strengths, Limitations and Recommendations for Improvement. 1993. GAO/PEMD-93-18.
- Golub AL, Johnson BD. Substance use progression and hard drug abuse in inner-city New York. In: Kandel DB, editor. Stages and Pathways of Involvement in Drug Use: Examining the Gateway Hypothesis. Cambridge; New York: (to appear) (accepted for publication) [Google Scholar]
- Golub AL, Labouvie E, Johnson BD. Response reliability and the study of adolescent substance use progression. J. Drug Issues. 2000;30:103–118. [Google Scholar]
- Grant BF. Age at smoking onset and its association with alcohol consumption and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J. Substance Abuse. 1998;10:59–73. doi: 10.1016/s0899-3289(99)80141-2. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA. Age at onset to alcohol use and its association with DSM-IV alcohol abuse and dependence: Results from the National Longitudinal Alcohol Epidemiologic Survey. J. Substance Abuse. 1997;9:103–110. doi: 10.1016/s0899-3289(97)90009-2. [DOI] [PubMed] [Google Scholar]
- Hanson DJ. Alcohol Education: What We Must Do. Praeger; Westport, CT: 1996. [Google Scholar]
- Harrison L. The validity of self-reported data on drug use. J. Drug Issues. 1995;25:91–111. [Google Scholar]
- Hawkins B, Catalano RP, Miller JY. Risk and protective factors for alcohol and other drug problems in adolescence and early adulthood: Implications for substance abuse prevention. Psychol. Bull. 1992;112:64–105. doi: 10.1037/0033-2909.112.1.64. [DOI] [PubMed] [Google Scholar]
- Horwitz AV, White HR. Gender role orientation and styles of pathology among adolescents. J. Health Soc. Behav. 1987;28:158–170. [PubMed] [Google Scholar]
- Johnson RA, Gerstein DR, Rasinski KA. Recall decay and telescoping in self-reports of alcohol and marijuana use: Results from the National Household Survey on Drug Abuse [NHSDA]. In Proc. Am. Assoc. Pub. Opin. Research. 1997 [Google Scholar]
- Johnston LD, O'Malley PM. The recanting of earlier reported drug use by young adults. In: Harrison L, Hughes A, editors. Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates. 1997. pp. 59–80. NIDA Research Monograph 167, NIH Publication No. 97-4147. [PubMed] [Google Scholar]
- Kandel DB. Convergence in prospective longitudinal surveys of drug use in normal populations. In: Kandel DB, editor. Longitudinal Research on Drug Use: Empirical Findings and Methodological Issues. Hemisphere; Washington, DC: 1978. pp. 3–38. [Google Scholar]
- Labouvie E, Bates ME, Pandina RJ. Age of first use: Its reliability and predictive utility. J. Stud. Alc. 1997;58:638–643. doi: 10.15288/jsa.1997.58.638. [DOI] [PubMed] [Google Scholar]
- Mills CJ, Noyes HL. Patterns and correlates of initial and subsequent drug use among adolescents. J. Consult. Clin. Psychol. 1984;52(2):231–243. doi: 10.1037//0022-006x.52.2.231. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration (SAMHSA) National Household Survey on Drug Abuse: Population Estimates 1996. 1997. Department of Health and Human Services Publications No. (SMA) 97-3137. [Google Scholar]
- Tonry M, Ohlin LE, Farrington DP. Human Development and Criminal Behavior: New Ways of Advancing Knowledge. Springer-Verlag; New York: 1991. [Google Scholar]
- Wright D, Gfroerer J, Epstein J. The use of external data sources and ratio estimation to improve estimates of hardcore drug use from the NHSDA. In: Harrison L, Hughes A, editors. Validity of Self-Reported Drug Use: Improving the Accuracy of Survey Estimates. 1997. pp. 447–497. NIDA Research Monograph 167, NIH Publication No. 97-4147. [PubMed] [Google Scholar]