Abstract
Purpose
Transurethral resection of the prostate (TURP) is still considered the gold standard in the treatment of benign prostatic hyperplasia (BPH). However, open prostatectomy is indicated for prostate glands over 75 ml. There have been few reports concerning the use of TURP for large prostate glands over 100 ml. Herein we compared the effectiveness of monopolar TURP, bipolar TURP, and open prostatectomy in prostate glands larger than 100 ml.
Materials and Methods
We reviewed the data of 48 patients with prostate glands larger than 100 ml. A total of 19, 17, and 12 patients underwent monopolar TURP (group A), bipolar TURP (group B), or open prostatectomy (group C), respectively. Preoperative International Prostate Symptom Score (IPSS), maximal flow rate (Qmax), prostate volume, resected tissue volume, resection velocity, and operative time were documented. Postoperative hemoglobin, serum sodium change, hospital stay, and postoperative 6-month IPSS and Qmax were evaluated.
Results
The prostate volumes did not differ significantly among the three groups. Operative time was similar in the two TURP groups, but open prostatectomy required a longer operative time. There was no significant difference in the resected prostate tissue or resection velocity between the two TURP groups. There was a marked decrease in postoperative serum sodium in the monopolar group compared with the other two groups. Among the groups, bipolar TURP required a shorter hospitalization. Postoperative IPSS, quality of life (QoL), and Qmax improved significantly in all groups.
Conclusions
Even for large prostate glands, the results of this study suggest that bipolar TURP is an effective and safe operation owing to the significant improvements in voiding symptoms, shorter hospitalization, and fewer complications such as transurethral resection syndrome.
Keywords: Complications, Prostatic hyperplasia, Transurethral resection of prostate
INTRODUCTION
Benign prostatic hyperplasia (BPH) is the most common benign tumor in men, and its incidence is age-related. Symptoms of BPH are caused by either obstructive components of the prostate glands or secondary changes to the bladder resulting from bladder outlet obstruction. There are many treatment alternatives, such as watchful waiting, pharmacologic medications, phytotherapy, minimally invasive therapy, transurethral resection of prostate (TURP), and open simple prostatectomy. Surgical management is often required when the symptoms induced by BPH are refractory to pharmacologic treatments. In those cases, TURP is the most frequently performed procedure for endoscopic management owing to its shorter hospitalization and low comorbidity and mortality. However, if the prostate gland is too large, conventional monopolar TURP has limitations, such as prolonged operation time with use of non-electrolyte irrigation fluid and monopolar current, which can result in transurethral resection (TUR) syndrome and an increased risk of bleeding. Open prostatectomy is indicated for prostate glands larger than 75 ml. Presently, there have also been a few reports regarding the utilization of TURP with bipolar energy in cases of prostate glands over 100 ml.
Therefore, with three procedures being used to surgically treat BPH and no clear agreement or comparison among the three, the purpose of this study was to compare the efficacy and safety of monopolar TURP, bipolar TURP, and open prostatectomy in large prostate glands.
MATERIALS AND METHODS
A retrospective study was conducted with 48 BPH patients who underwent monopolar TURP, bipolar TURP, or open prostatectomy. Exclusion criteria were abnormal digital rectal examination (DRE) findings, elevated prostate-specific antigen (PSA), and presence of neurogenic bladder, urethral stricture, bladder stone, or tumor. Among 48 BPH patients with prostate glands larger than 100 ml, 19 patients underwent monopolar TURP (group A), 17 patients underwent bipolar TURP (group B), and 12 patients underwent open prostatectomy (group C) from January 2004 to June 2009. In this study, all of the operations were performed by a single surgeon who had previously performed 143 cases of TURP on prostates smaller than 100 ml. Among the groups, 6, 7, and 4 patients, respectively, had concomitant diabetes mellitus (DM). A total of 8, 10, and 7 patients from each group had at least one episode of acute urinary retention in the past. Twenty-six patients had been on an alpha-1-adrenoreceptor blocker and 6 patients had been on a combination of an alpha-1-adrenoreceptor blocker and 5-alpha-reductase inhibitors for a mean duration of 1.2 months before the surgical interventions. Monopolar TURP was performed with a 24 Fr resectoscope (Karl Storz®, Tuttlingen, Germany) using Urosol® (CJ, Seoul, Korea). Bipolar TURP was performed with a 27 Fr continuous flow resectoscope (Gyrus ACMI®, Olympus Inc, Germany) using saline irrigation with the Gyrus Plasma-Kinetic Tissue Management System. At the end of the monopolar and bipolar TURP, a 20 Fr 3-way urethral Foley catheter was inserted and normal saline irrigation was applied. Continuous saline irrigation was done until the urine drained from the urethral Foley catheter became clear in the absence of irrigation. In cases of open prostatectomy, a 20 Fr 3-way urethral Foley catheter and suprapubic cystostomy catheter were inserted with continuous saline irrigation at a minimal rate to prevent urine passage blockage. The catheters were removed when the urine became clear without continuous saline irrigation. The patients were discharged upon spontaneous voiding.
For the preoperative data, we collected the International Prostate Symptom Score (IPSS), maximal flow rate (Qmax), prostate volume, intraoperative resected tissue volume, resection velocity, and operation time, which were recorded and analyzed. Data collected postoperatively were the hemoglobin/sodium change, length of postoperative hospitalization, and postoperative 6-month IPSS, quality of life (QoL), and Qmax. All data were reviewed and evaluated retrospectively. The Kruskal-Wallis test, post hoc Tamhane's test, chi-square test, and Wilcoxon signed-rank test were performed to analyze the data. All statistical analyses were performed with SPSS ver. 18.0 (SPSS Inc, Chicago, IL, USA). p-values of less than 0.05 were deemed statistically significant.
RESULTS
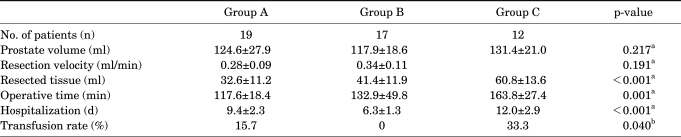
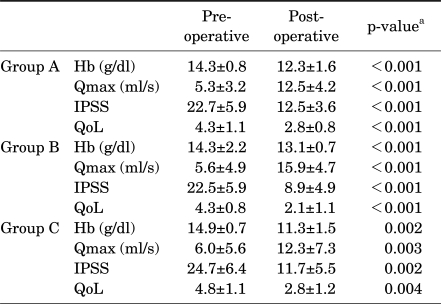
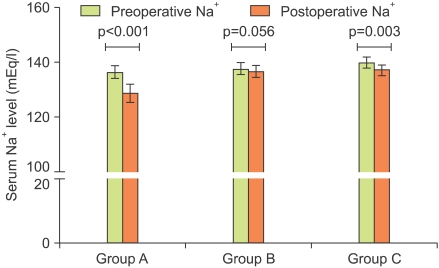
The preoperative prostate volumes of each group were 124.6±27.9 ml (A), 117.9±18.6 ml (B), and 131.4±21.0 ml (C), respectively (p=0.217) (Table 1). The preoperative mean serum sodium concentrations of each group were 136.4±2.3 mEq/l (A), 137.8±2.2 mEq/l (B), and 140.0±2.0 mEq/l (C). The preoperative mean serum hemoglobin of each group were 14.3±0.8 mEq/l (A), 14.3±2.2 mEq/l (B), and 14.9±0.7 mEq/l (C) (Table 2). The postoperative serum sodium levels of each group were 128.6±3.3, 136.7±2.2, and 137.2±2.0 mEq/l, respectively (Fig. 1). Six patients from the monopolar TURP group experienced a significant decrease in the serum sodium concentration. The mean reduction in serum sodium in these cases was 10.2±1.35 mEq/l. Postoperative serum sodium reduction below 125 mEq/l was deemed significant. The mean operation time was 117.6±18.4 minutes (A), 132±49.8 minutes (B), and 163.8±27.4 minutes (C), respectively (p=0.001). Resected prostatic tissue volumes were 32.6±11.2 ml (A), 41.4±11.9 ml (B), and 60.8±13.6 ml (C) (p<0.001). The resection velocity of groups A (0.28 ml/min) and B (0.34 ml/min) showed no statistically significant difference (p=0.191) (Table 1). Postoperative hemoglobin changes in the three groups showed a statistical significance (p<0.001, p<0.001, and p=0.002). Complications were noted in 5 cases in the monopolar TURP group and in 4 cases in the open prostatectomy group. In the monopolar group, there were 2 cases of TUR syndrome and 3 patients who required blood transfusions due to a mean reduction in hemoglobin of 4.2 g/dl. Even though the changes in hemoglobin were statistically significant, there were no postoperative hemoglobin changes severe enough to necessitate blood transfusions in the bipolar group. In the open prostatectomy group, 4 patients received blood transfusions. The mean reduction in those cases was by 5.1 g/dl. The transfusion rate of each group was 15%, 0%, and 33%, respectively. Factors including the color of the urine drained from the urethral Foley catheter and anemic conjunctiva postoperatively were triggers for deciding upon transfusion. No complications were noted in the bipolar TURP group. Postoperative hospital stays were 9.4±2.3 days, 6.3±1.3 days, and 12.0±2.9 days, respectively (p<0.001). Patients in the bipolar TURP group required shorter hospitalizations than did patients in the other groups. The postoperative 6-month IPSS/Qmax of all groups showed statistically significant improvement (Table 2). No cases of urethral or meatal strictures were noted during the 6-month follow-up period in either TURP group.
TABLE 1.
Preoperative characteristics and perioperative outcomes of the groups
a: Kruskal-Wallis test, b: chi-square test
TABLE 2.
Comparison of perioperative parameters among the groups
Hb: serum hemoglobin concentration, Qmax: maximal flow rate, IPSS: International Prostate Symptom Score, QoL: quality of life, a: Wilcoxon signed-rank test
FIG. 1.
Perioperative change in serum sodium level among the groups.
DISCUSSION
Alpha-1-adrenoreceptor blockers and 5-alpha-reductase inhibitors are the mainstay of treatment for BPH and have been shown to have a higher cost-efficiency than TURP [1]. However, the most effective treatment modality is known to be the surgical resection of prostatic adenomas, which cause obstruction. Open prostatectomy is considered when the prostate gland is too large to be resected endoscopically. Previously, a prostate gland larger than 75 ml was an indication for open prostatectomy [2,3]. Concomitant bladder pathologies such as bladder diverticulum, bladder stones, urethral strictures, and a patient's inability to be in the dorsal lithotomy position are other indications for open prostatectomy [4]. Park and Chung reported that when comparing TURP with open prostatectomy, open prostatectomy renders better postoperative IPPS and a higher Qmax than does TURP due to the complete resection of adenomas, which leads to wider width and symmetry of the proximal prostatic urethra [5]. Open prostatectomy offers advantages such as a lower retreatment rate, more complete removal of prostate adenomas, and avoidance of TUR syndrome. However, risks of incontinence, retrograde ejaculation, perioperative hemorrhage, and longer hospitalization still remain [4]. Complication rates of open prostatectomy are known to range from 10% to 40% [6]. Conventional TURP was first developed in the United States in the 1920s and 1930s. Over the years, many advances in surgical instruments and technique have been made, and thus now TURP is recognized as the gold standard for the surgical treatment of BPH [6]. TURP is known to offer improvement in voiding symptoms and Qmax in over 80% of patients [7]. Morbidities associated with TURP have been decreasing over the past three decades [8]. However, perioperative hemorrhage and TUR syndrome, which is a consequence of excessive absorption of non-conductive irrigating solution, are still grave complications that can occur. TUR syndrome occurs in 2% of patients [8]. The risk is increased if the gland is larger than 45 ml and the resection time is longer than 90 minutes [9]. Thus, application of conventional TURP in large prostate glands is limited. However, new technical advances to conventional TURP with monopolar energy were made in early 2000, most notably the development of bipolar current in TURP. The most noticeable difference is that saline is used as an irrigant, which reduces the morbidities associated with TUR syndrome. As shown in our results, bipolar TURP when compared with monopolar TURP resulted in a lower risk of developing TUR syndrome due to a smaller change in serum sodium than with monopolar TURP. This enables surgeons to take a longer time to operate and to resect more prostatic tissue than is possible with monopolar TURP. Moreover, bipolar TURP seems to be more efficient for removing tissue and simultaneously controlling for bleeding when compared to monopolar TURP. It is noteworthy that no transfusions were required in the bipolar TURP group, whereas there were 3 transfusion cases in the monopolar TURP group. Also, when compared with the other groups, bipolar TURP required shorter postoperative hospitalization.
Previous research agrees with our findings pertaining to bipolar TURP. Starkman et al reported that the patients treated with Gyrus TURP had their catheter removed a mean of 1.4 days earlier than the monopolar TURP group [10]. Eaton and Francis, reported that among 40 patients, 32 patients could be discharged on the day of operation with use of the Gyrus system [11]. de Sio et al reported shorter catheterization and hospitalization for bipolar TURP patients [12]. In a multicenter study regarding bipolar TURP, operators preferred bipolar TURP over monopolar TURP owing to cleaner resection surfaces (64%) and higher accuracy when resecting the apex of the prostate glands (93%) [13]. Considering that utilization of monopolar TURP in large prostate glands is limited, Bhansali et al compared bipolar TURP with monopolar TURP in their series of 70 patients with prostate glands >60 ml and reported that bipolar TURP showed excellent results in terms of perioperative blood loss, change in serum sodium, and duration of catheterization [14]. Baek et al reported perioperative outcomes of bipolar TURP in patients with prostate glands > 80 ml in their series and found that bipolar TURP showed advantages such as less serum sodium change and less hemoglobin change [15]. In 2006, Kim et al reported that bipolar TURP is superior to monopolar TURP with fewer surgical complications [16]. Kim et al also stated that TURP with bipolar energy rendered postoperative outcomes similar to those of monopolar TURP but with fewer complications, shorter catheterization, shorter hospitalization time, and lower cost [17]. Unlike the above-mentioned reports, we studied only prostate glands larger than 100 ml and compared the perioperative parameters of monopolar and bipolar TURP and open prostatectomy, which is indicated for prostate glands larger than 75 ml. The patients had not been on alpha-1-adrenoreceptor blockers or 5-alpha-reductase inhibitors for a long period of time, because it was hard to expect satisfactory alleviations of voiding symptoms with medication alone with a prostate gland size of larger than 100 ml. In this study, volumes of prostate weights resected were lower than those reported previously, especially in the open prostatectomy group. The lower volumes of prostatic tissue removed in this study can be accounted for by the smaller adenoma sizes in the open prostatectomy group compared with those of previous reports. In addition, the lower prostate weights removed in both TURP groups may be accounted for by the surgeon's experience rather than a cautery effect. Despite the lower volumes of prostatic tissues removed than in previous literature, bipolar TURP and open prostatectomy resulted in significantly improved postoperative 6-month Qmax and IPSS, showing no statistically significant difference between the two groups in postoperative change in Qmax and IPSS at the 6-month follow-up.
One limitation of this study is that monopolar and bipolar TURP were not performed with randomization. The learning curve could therefore have affected the postoperative parameters of bipolar TURP. A second limitation of this study is that the size of the study population was relatively small. Last, the patients were not randomized to exclude concomitant conditions, such as diabetes mellitus or episodes of acute urinary retention, that could have affected voiding symptoms.
CONCLUSIONS
Bipolar TURP showed similar efficacy to monopolar TURP and open prostatectomy in improving voiding symptoms while rendering shorter hospitalizations, a low transfusion rate, and fewer complications such as TUR syndrome. Bipolar TURP can be considered as a safe substitute for monopolar TURP and open prostatectomy even for large prostate glands over 100 ml.
Footnotes
The authors have nothing to disclose.
References
- 1.Lowe FC, McDaniel RL, Chmiel JJ, Hillman AL. Economic modeling to assess the costs of treatment with finasteride, terazosin, and transurethral resection of the prostate for men with moderate to severe symptoms of benign prostatic hyperplasia. Urology. 1995;46:477–483. doi: 10.1016/S0090-4295(99)80258-1. [DOI] [PubMed] [Google Scholar]
- 2.Barba M, Leyh H, Hartung R. New technologies in transurethral resection of the prostate. Curr Opin Urol. 2000;10:9–14. doi: 10.1097/00042307-200001000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Tubaro A, Carter S, Hind A, Vicentini C, Miano L. A prospective study of the safety and efficacy of suprapubic transvesical prostatectomy in patients with benign prostatic hyperplasia. J Urol. 2001;166:172–176. [PubMed] [Google Scholar]
- 4.Oesterling J. Retropubic and suprapubic open prostatectomy. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Philadelphia: Saunders; 2007. p. 2852. [Google Scholar]
- 5.Park SW, Chung MK. The results of retropubic prostatectomy and transurethral resection of prostate; compare both results, and then investigate the cause of different results. Korean J Urol. 2004;45:309–314. [Google Scholar]
- 6.Kim DK, Kim SJ, Moon HS, Park SY, Kim YT, Choi HY, et al. The role of TURP in the detection of prostate cancer in BPH patients with previously negative prostate biopsy. Korean J Urol. 2010;51:313–317. doi: 10.4111/kju.2010.51.5.313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Holtgrewe HL. Transurethral prostatectomy. Urol Clin North Am. 1995;22:357–368. [PubMed] [Google Scholar]
- 8.Mebust WK. Transurethral prostatectomy. Urol Clin North Am. 1990;17:575–585. [PubMed] [Google Scholar]
- 9.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complications. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–247. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 10.Starkman JS, Santucci RA. Comparison of bipolar transurethral resection of the prostate with standard transurethral prostatectomy: shorter stay, earlier catheter removal and fewer complications. BJU Int. 2005;95:69–71. doi: 10.1111/j.1464-410X.2005.05253.x. [DOI] [PubMed] [Google Scholar]
- 11.Eaton AC, Francis RN. The provision of transurethral prostatectomy on a day-case basis using bipolar plasma kinetic technology. BJU Int. 2002;89:534–537. doi: 10.1046/j.1464-410x.2002.02673.x. [DOI] [PubMed] [Google Scholar]
- 12.de Sio M, Autorino R, Quarto G, Damiano R, Perdonà S, di Lorenzo G, et al. Gyrus bipolar versus standard monopolar transurethral resection of the prostate: a randomized prospective trial. Urology. 2006;67:69–72. doi: 10.1016/j.urology.2005.07.033. [DOI] [PubMed] [Google Scholar]
- 13.Patel A, Adshead JM. First clinical experience with new transurethral bipolar prostate electrosurgery resection system: controlled tissue ablation (coblation technology) J Endourol. 2004;18:959–964. doi: 10.1089/end.2004.18.959. [DOI] [PubMed] [Google Scholar]
- 14.Bhansali M, Patankar S, Dobhada S, Khaladkar S. Management of large (>60 g) prostate gland: PlasmaKinetic Superpulse (bipolar) versus conventional (monopolar) transurethral resection of the prostate. J Endourol. 2009;23:141–145. doi: 10.1089/end.2007.0005. [DOI] [PubMed] [Google Scholar]
- 15.Baek M, Paick SH, Lee BK, Kang MB, Lho YS, Jung SI, et al. The efficacy of bipolar transurethral resection of the prostate in patients with large prostates (>80 g) and analysis of the postoperative results based on the resection ratio. Korean J Urol. 2008;49:1087–1093. [Google Scholar]
- 16.Kim HG, Lee BK, Paick SH, Lho YS. Efficacy of bipolar transurethral resection of the prostate: comparison with standard monopolar transurethral resection of the prostate. Korean J Urol. 2006;47:377–380. [Google Scholar]
- 17.Kim JY, Moon KH, Yoon CJ, Park TC. Bipolar transurethral resection of the prostate: a comparative study with monopolar transurethral resection. Korean J Urol. 2006;47:493–497. [Google Scholar]