Abstract
Objective:
To assess the efficacy of a modification for Prolonged Exposure (PE) therapy for single incident trauma in youth and examine the effective component(s) of treatment.
Method:
Fifteen youth (2 boys, 13 girls; mean age= 10.8 years) were treated with a developmentally modified version of PE called Trauma Mastery Therapy (TMT). The youth were evaluated pre-treatment, every 2 treatment sessions, and at 1 month follow-up. Primary outcome measure: the Child PTSD Symptom Scale (CPSS), a self administered PTSD questionnaire.
Results:
Post-treatment, 13 participants did not meet criteria for PTSD. Patients showed significant improvement at post-treatment. Analysis of variance models with pair-wise contrasts showed significantly higher scores at initiation of treatment as compared to the end of the exposure phase and, to a lesser extent, as compared to the psychoeducational phase, but no further significant improvement following the relapse prevention or follow-up phases.
Conclusions:
TMT appears to be a promising treatment for single incident trauma in youth. Flexibility within the structure of TMT may facilitate treatment success. The study suggests exposure, and to some extent, psychoeducation, to be important components of treatment. Additional research is required to further validate these initial findings.
Keywords: psychotherapy, PTSD, pediatric, prolonged exposure, single incident trauma
Introduction
Trauma is a universal and salient phenomenon. In the United States, 70% of adults and 40% of adolescents are reported to have experienced a traumatic event of a DSM-IV criterion A magnitude. According to the Centers for Disease Control and Prevention (CDC), 1,116,007 children were involved in motor vehicle accidents in the year 2008 in the United States alone. Eighteen percent of children who were involved in motor vehicle accidents are reported to be suffering from Post Traumatic Stress Disorder (PTSD) symptoms 6 months after the accident. Three to 100% of children experiencing a criterion A magnitude trauma will develop PTSD.
This wide range in incidence may be attributable to the different impact variable traumas have on the psyche, different diagnostic frameworks, or time elapsed since the trauma. In broad terms, traumas can be divided into natural versus intentional man-made trauma and single incident (type I) versus multiple-ongoing trauma (type II). Intuitively, man-made trauma may cause a higher incidence of Post Traumatic Stress Disorder than natural disasters. This assumption is corroborated by the literature. One might also assume that multiple, ongoing traumas (type II trauma) would cause a higher incidence of PTSD than single incident trauma (type 1 trauma). According to a leading expert in the field, it is not only the incidence or severity of psychological disorder that differs between type I and type II trauma, but the mechanism by which the disorder develops and its presentation. Type 1 traumas usually present with typical PTSD symptoms of childhood, whereas Type II traumas may be associated with denial, psychic numbing, or long-term personality problems (Terr, 1991).
In the past few years, several rigorous studies have been conducted regarding the treatment of sexual abuse and complex trauma in children, but the subject of single incident trauma is just starting to be addressed. In fact, we found only one treatment outcome study to address this population of children. In this state of the art study, Gilboa-Schechtman and colleagues study the efficacy of Prolonged Exposure (PE) therapy in comparison to Time Limited Dynamic Psychotherapy (TLDP) for the treatment of Post Traumatic Stress Disorder (PTSD) in adolescents who had undergone single incident trauma. Diverse treatment methods have been found to be effective in the treatment of adult PTSD: Cognitive Behavioral Therapies (CBT) including Trauma-Focused CBT (TF-CBT) and Prolonged Exposure (PE), narrative therapy, psychodynamic therapy, play therapy and Eye Movement Desensitization and Reprocessing (EMDR). However, a debate exists in the literature as to which treatment components are necessary for effectiveness. The aims of this paper are to present the results achieved with our modification of Prolonged Exposure for the treatment of pediatric single incident trauma, and to explore which treatment components are most closely associated with therapeutic success.
Method
Subjects
Participants were 15 consecutively referred children attending the Child and Adolescent Anxiety Disorders Clinic at the Hospital for Sick Children, Toronto, who suffered a single incident trauma. All were diagnosed with Post Traumatic Stress Disorder based on semi-structured interview (see below). Youth with mental retardation, youth who had been treated with medication in the past 6 weeks or who had been abusing drugs, and cases of ongoing litigation were excluded. Therapy was initiated a minimum of 3 months after the trauma had occurred, as natural recovery from PTSD usually occurs within the first 3 months. Comorbid conditions included other anxiety disorders (Generalized Anxiety Disorder (13%); Social Phobia (6%); Specific Phobia (20%); Panic Disorder (6%), Oppositional Defiant Disorder (6%), and Parent-Child Relational Problem (13%). Demographic, trauma, and treatment characteristics of subjects are detailed in Table 1. The study was approved by the Hospital for Sick Children’s Research Ethics Board and all participants and their caregivers gave their consent or assent depending on age.
Table 1.
Patient, trauma and treatment characteristics
| Age in years (mean ± SD; range) | 10.8 ± 4.39; 5–17 |
| Gender (female) | 13 (86%) |
| Family status (parents married) | 12 (80%) |
| Trauma type | |
| Motor vehicle accident | 9 (60%) |
| Circumstantial injury | 4 (27%) |
| Non sexual assault | 1 (7%) |
| Sexual assault | 1 (7%) |
| Time since trauma in months (mean ± SD; range) | 13.5 ± 12.4; 3–36 |
| ≥ 1 comorbid disorder | 5 (33%) |
| Ethnicity | |
| ≥ 2 generation in Canada | 8 (53%) |
| Descent | |
| British/Scottish/Irish | 8 (53%) |
| Mixed | 2 (13%) |
| Chinese | 2 (13%) |
| Other | 3 (20%) |
| Treatment hours with patients (mean ± SD; range) | 13.3 ± 3.5; 5–16 |
| Treatment hours with parents (mean ± SD; range) | 3.6 ± 1.12; 1–5 |
Assessment time points
Assessment time points were as follows:
T0 - Diagnostic interview.
T1– 8 – every second treatment session.
T 9 – 1 month follow-up.
Measures
A senior child and adolescent psychiatrist (KM) and a child psychiatrist specializing in childhood Post Traumatic Stress Disorder (GAN), diagnosed participants at T0 and follow-up using the Schedule for Affective Disorders and Schizophrenia for School-Age Children (K-SADS-PL). This semi-structured interview is reported to have excellent reliability (both inter-rater and test-retest) and validity for use with clinical samples.
Youth participating in the treatment program were assessed at all assessment time points using the following self-report questionnaires filled in by the youth and their caregivers:
The Child PTSD Symptom Scale (CPSS). The CPSS is a 17 item self report scale which assesses DSM-IV PTSD symptoms. It demonstrates very good to excellent internal consistency (α = 0.89 for total score; α = 0.86 in our sample), moderate to excellent test-retest reliability (r = 0.84 for total score) and very good convergent validity (0.80).
The Multidimensional Anxiety Scale for Children (MASC) is a 39 item self report scale which assesses anxiety disorders in youth and distinguishes between different anxiety dimensions. It shows excellent internal reliability (α = 0.90 for total score; α = 0.85 in our sample) and satisfactory to excellent test-retest reliability (r = 0.80 for total score).
The Children’s Depression Inventory (CDI) is a 27 item self report scale which assesses the presence and severity of depressive symptoms in youth. It shows good internal reliability (α = 0.80; α= 0.83 in our sample).
The Children’s Global Assessment Scale (CGAS) was administered at T0, last treatment session and at T9 – follow-up, by an independent evaluator. The Clinical Global Impression (CGI) scale is a clinician-rated, 8 item Likert scale which assesses global functioning. It was rated by clinician, parent and child during the last treatment session and at follow-up.
Treatment Protocol and Adherence
The treatment program used, Trauma Mastery Therapy (TMT), is a modification of the Prolonged Exposure (PE) therapy manual, a cognitive behavioral therapy for the treatment of Post Traumatic Stress Disorder developed by Foa et al. for the treatment of adult patients. TMT adopts a modular, rather than a session-based approach. The treatment is divided into three phases: 1) psychoeducation and treatment planning (including relaxation techniques); 2) exposure, and 3) relapse prevention and graduation. The modules within each phase are structured to present a particular concept to the child and provide an in-session exercise to demonstrate or use the concept. The modular format allows flexibility in that the therapist may present one or more modules in each session depending on the child’s developmental level, attention span, and specific needs. The therapist may use different therapeutic techniques appropriate to different ages (e.g., younger patients may require more redirection and activities such as drawing or playing in comparison to older patients). Thus, the number of treatment sessions was variable (7 to 16) as was each session’s duration (30 to 90 minutes).
Another modification to the adult protocol was the involvement of caregivers. Mendlowitz and others found that concurrent parental involvement in treatment enhanced coping strategies in both children and their parents. With this in mind, a “touch-base” time with caregivers at the end of each session was added. Caregivers were also seen for an additional session, separate from their children, on every fourth child session.
A single therapist (GAN), trained in PE at the University of Pennsylvania’s Center for Treatment and Study of Anxiety (CTSA), administered therapy. Treatment fidelity and adherence was ensured following recommendations by Kazdin et al. (1988). All therapy sessions were videotaped. A senior therapist at the CTSA viewed the videotapes and provided weekly telephone supervision.
Statistical Analysis
Descriptive statistics were calculated for all variables of interest. Continuous measures were summarized using means and standard deviations whereas categorical measures were summarized using counts and percentages.
Repeated measures analysis of variance (ANOVA) models were used to analyze the change in measure scores across the following four time points:
Ti – Diagnostic interview
Te – 1st session of exposure component (after completion of psychoeducational component).
Tr – 1st session of relapse prevention component (after completion of exposure component).
Tf – Follow-up (after completion of relapse prevention component and follow-up).
Additionally, pair-wise Tukey’s tests were used to compare scores at each time point.
All analyses were carried out using SAS Version 9.1 (SAS Institute, Cary, NC, USA).
Results
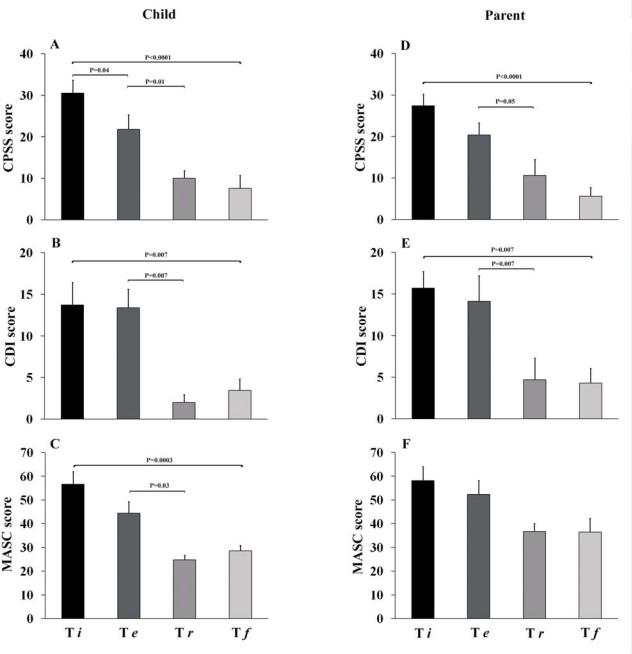
Thirteen of fifteen study participants did not meet criteria for Post Traumatic Stress Disorder post-treatment on the K-SADS-PL interview. The analysis of variance models showed significant (p<0.001) improvement in PTSD, anxiety and depression symptoms at post, as compared to pre- treatment. In an attempt to tease out the effective component of treatment, pair-wise Tukey’s tests were carried out on all measures to see differences between scores across four time periods: psychoeducation phase, exposure phase, relapse prevention and graduation phase, and follow-up phase. On most measures (see below) significant (p<0.01) symptom improvement was found after the exposure phase as compared to relapse prevention and follow-up phases. On the child PTSD measure (CPSS), a significant improvement was found in the psychoeducation phase as well. The parental evaluation of child anxiety scale (i.e., MASC by parent-report) was the only measure that did not show significant improvement across all four phases. Detailed results are shown in Table 2 and Figure 1.
Table 2.
Means and standard deviations for key measures*
| Ti (diagnostic interview) | Te (beginning of exposure phase) | Tr (beginning of relapse prevention phase) | Tf (follow up) | |
|---|---|---|---|---|
| Child PTSD Symptom Scale (CPSS) patient | 30.5 ± 3.2 | 21.8 ± 3.5 | 10.0 ± 1.9 | 7.6 ± 3.1 |
| Child PTSD Symptom Scale (CPSS) parent | 27.4 ± 2.8 | 20.4 ± 2.9 | 10.6 ± 3.9 | 5.6 ± 2.1 |
| Child Depression Inventory (CDI) patient | 13.7 ± 2.7 | 13.4 ± 2.2 | 2.0 ± 0.9 | 3.4 ± 1.4 |
| Child Depression Inventory (CDI) parent | 15.7 ± 2.0 | 14.1 ± 3.1 | 4.7 ± 2.6 | 4.3 ± 1.8 |
| The Multidimensional Anxiety Scale for Children (MASC) patient | 56.6 ± 5.3 | 44.4 ± 4.9 | 24.8 ± 1.9 | 18.6 ± 2.2 |
| The Multidimensional Anxiety Scale for Children (MASC) parent | 58.2 ± 5.9 | 52.4 ± 5.8 | 36.7 ± 3.3 | 36.5 ± 5.7 |
raw scores
Figure 1.
Change over Time in Key Measures.
Ti – diagnostic interview; Te – beginning of exposure phase; Tr – beginning of relapse prevention phase; Tf – follow up.
Clinical vignettes
A detailed description of all study participants is beyond the scope of this brief paper. The two vignettes below highlight the mechanisms by which TMT’s flexibility may have facilitated treatment gains. Ethnicity and other potentially identifying information have been deleted to maintain confidentiality.
J was 15 years old at the time of the study, born to a family self-described as “good God-fearing people”. In accordance with the way she was brought up, J wished to first have a sexual relationship only after marriage. She was sexually assaulted four months prior to our first consultation and a full range of PTSD symptoms ensued. Most strikingly, the interactions within the family had changed. J had told her parents about the rape and although her family was supportive, their attitude towards J had changed in two main areas: 1) J was no longer allowed to travel unaccompanied and 2) J no longer felt understood within her family. She constantly felt implicitly blamed for being “a slut”. During “imaginal exposure” processing J was able to articulate that she had never told anyone shameful parts of the story, for example, the fact that she was initially attracted to her abuser. She was certain the feeling of attraction made her a bad person. Her symptom levels dropped drastically after reviewing “healthy sexuality” psycho-educational material with her, enabling her to understand that her thoughts and feelings were common and legitimate. At this point, her family was advised to allow J a larger degree of freedom, and a plan that was agreeable to all family members was constructed as part of “in vivo exposure”. J’s symptom level dropped further after being able to repeat the narrative of her assault and confront trauma reminders. This vignette illustrates the importance of exposure modules, the importance of TMT’s “healthy sexuality” module which may be implemented at any stage of treatment, and the value of involving the family in treatment.
M was 9 years old at the time of the study. She presented as a chubby, highly anxious young woman with a concrete style of thinking. Six months prior to our first consultation, she was trapped in an elevator along with her younger sister and mother for 45 minutes. In order to escape, she had to maneuver, together with the other temporary inhabitants of the elevator, through a crack between doors and two floors in order to rescue herself. A full range of PTSD symptoms followed this incident, including avoidance of elevators – an inconvenience when living on the 16th floor. M was anxious to the point of barely speaking at the beginning of therapy. Many sessions were required for the initial module in order to gain her trust. She never transformed into a chatty child but, surprisingly, was able to draw her ordeal in great detail, remembering elements of the trauma that her mother and sister did not recall. She improved slowly, through addressing details in the drawings, understanding her thoughts about her family at that moment (“they didn’t care about me”), and using a gradual exposure hierarchy. Eventually, M was able to conveniently take the elevator up to her 16th floor apartment. This vignette illustrates the importance of “flexibility within conformity”, in that a longer than usual period was allowed to gain M’s trust and develop the treatment alliance. It also highlights the benefit of using different modes of communication when practicing imaginal exposure with children at different developmental stages, in this instance drawing.
Discussion
Initially, patients showed a high symptom level and significant distress as a result of single incident traumas such as a motor vehicle accident, proximity to bears, an unexpected deep cut, or a sexual assault. Consistent with our first aim, we found a significant decrease in Post Traumatic Stress Disorder symptoms as well as in overall anxiety and depression in participants after treatment, as demonstrated by both patient and caregiver reports and clinician ratings. At the end of the program, 87% of patients no longer met DSM-IV criteria for PTSD. The analysis of variances models showed significant decrease in PTSD, depression, and anxiety symptoms at post-as compared to pre-treatment. Thus, this modified version of PE appears to hold promise in the treatment of youth with single-incident PTSD.
A possible overall contributor to treatment success is the modular approach taken by TMT. This approach is based on empirical evidence which suggests flexibility in implementation, within overall conformity to clearly articulated treatment goals and procedures, improves treatment outcome relative to rigid, manualized treatments.
Consistent with our second aim (exploring treatment components associated with therapeutic change), pair-wise Tukey’s tests showed a significant drop in symptoms to occur following the exposure phase in four out of six measures. The only two measures which did not show significant improvement were the child CPSS and caregiver MASC. Child CPSS showed PTSD symptoms improved significantly after the psychoeducational phase and continued to improve significantly through the exposure phase but not following the relapse prevention and follow-up phase. Child anxiety as perceived by their caretaker (MASC) was the only measure that did not show significant change throughout all treatment phases. The consistent and significant drop in symptom level after the exposure phase suggests the exposure component of therapy to be the most predictive for symptom reduction. Although adult studies strongly suggest the exposure component to be the most predictive of symptom reduction, we are not aware of studies that showed specific and significant improvement following this phase. The fact that our flexible protocol allowed the therapist to spend a variable number of sessions on each module and to use a variety of therapeutic techniques, leaving only the essence of exposure constant, further strengthens this point.
Conclusion
Our study is a pilot case series, and has the limitations of a small sample, a wide age range, and no control group. Although fidelity was carefully monitored, provision of therapy by a single therapist may further limit generalizability. Nevertheless, the study gives evidence for TMT’s ability to be a flexible and promising treatment for youth suffering from PTSD after single incident trauma and suggests that exposure is a key contributor to treatment success.
Acknowledgments / Conflicts of Interest
The study was funded by the Department of Psychiatry Endowment Fund, the Hospital for Sick Children, Toronto, Canada. We would like to thank Alex Kiss, PhD. for his contribution to statistical analysis and Edna Foa for her help and support.
References
- Adler-Nevo G, Manassis K. Psychosocial treatment of pediatric posttraumatic stress disorder: The neglected field of single-incident trauma. Depression and Anxiety. 2005;22:177–189. doi: 10.1002/da.20123. [DOI] [PubMed] [Google Scholar]
- Breslau N, Davis GC. Posttraumatic stress disorder in an urban population of young adults: Risk factors for chronicity. American Journal of Psychiatry. 1992;149:671–675. doi: 10.1176/ajp.149.5.671. [DOI] [PubMed] [Google Scholar]
- Bryant B, Mayou R, Wiggs L, Ehlers A, Stores G. Psychological consequences of road traffic accidents for children and their mothers. Psychological Medicine. 2004;34:335–346. doi: 10.1017/s0033291703001053. [DOI] [PubMed] [Google Scholar]
- Foa EB. Psychosocial treatment of posttraumatic stress disorder. Journal of Clinical Psychiatry. 2000;61(Suppl 5):43–48. [PubMed] [Google Scholar]
- Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, Street GP. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology. 1999;67:194–200. doi: 10.1037//0022-006x.67.2.194. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hearst-Ikeda D, Perry KJ. Evaluation of a brief cognitive-behavioral program for the prevention of chronic PTSD in recent assault victims. Journal of Consulting and Clinical Psychology. 1995;63:948–955. doi: 10.1037//0022-006x.63.6.948. [DOI] [PubMed] [Google Scholar]
- Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: Outcome at academic and community clinics. Journal of Consulting and Clinical Psychology. 2005;73:953–964. doi: 10.1037/0022-006X.73.5.953. [DOI] [PubMed] [Google Scholar]
- Foa EB, Johnson KM, Feeny NC, Treadwell KR. The child PTSD Symptom Scale: A preliminary examination of its psychometric properties. Journal of Clinical Child Psychology. 2001;30:376–384. doi: 10.1207/S15374424JCCP3003_9. [DOI] [PubMed] [Google Scholar]
- Garrison CZ, Bryant ES, Addy CL, Spurrier PG, Freedy JR, Kilpatrick DG. Posttraumatic stress disorder in adolescents after Hurricane Andrew. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1193–1201. doi: 10.1097/00004583-199509000-00017. [DOI] [PubMed] [Google Scholar]
- Giaconia RM, Reinherz HZ, Silverman AB, Pakiz B, Frost AK, Cohen E. Traumas and posttraumatic stress disorder in a community population of older adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34:1369–1380. doi: 10.1097/00004583-199510000-00023. [DOI] [PubMed] [Google Scholar]
- Gilboa-Schechtman E, Foa EB, Shafran N, Aderka IM, Powers MB, Rachamim L, et al. Prolonged exposure versus dynamic therapy for adolescent PTSD: A pilot randomized controlled trial. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:1034–1042. doi: 10.1016/j.jaac.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillies D, O’Brien L, Rogers P, Meekings C. Psychological therapies for the prevention and treatment of post-traumatic stress disorder in children and adolescents. Cochrane Database of Systematic Reviews. 2010 doi: 10.1002/14651858.CD006726.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green BL, Grace MC, Vary MG, Kramer TL, Gleser GC, Leonard AC. Children of disaster in the second decade: A 17-year follow-up of Buffalo Creek survivors. Journal of the American Academy of Child and Adolescent Psychiatry. 1994;33:71–79. doi: 10.1097/00004583-199401000-00011. [DOI] [PubMed] [Google Scholar]
- Guy W. ECDEU assessment manual for psychophramacology. Rockville, Md.: Department of health education and welfare; 1976. [Google Scholar]
- Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): Initial reliability and validity data. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36:980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- Kendall PC, Chu B, Gifford A, Hayes C, Nauta M. Breathing life into a manual: Flexibility and creativity with manual-based treatments. Cognitive & Behavioral Practice. 1998;5:177–198. [Google Scholar]
- Keppel-Benson JM, Ollendick TH, Benson MJ. Post-traumatic stress in children following motor vehicle accidents. Journal of Child Psychology and Psychiatry. 2002;43:203–212. doi: 10.1111/1469-7610.00013. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kovacs M. The Children’s Depression, Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- Laor N. Commentary: To move development forward: A tribute to Donald Cohen. Israeli Journal of Psychiatry and Related Sciences. 2001;38:235–237. [PubMed] [Google Scholar]
- Lavie P. Post-Traumatic Stress Disorder and Sleep. New England Journal of Medicine. 2002;346:1335. [Google Scholar]
- March J, Amaya-Jackson J, Pynoos R. Pediatric post-traumatic stress disorder. In: Weiner J, editor. Textbook of child and adolescent psychiatry. 2nd ed. Washington: American Psychiatric Press; 1996. [Google Scholar]
- March JS, Parker JD, Sullivan K, Stallings P, Conners CK. The Multidimensional Anxiety Scale for Children (MASC): Factor structure, reliability, and validity. Journal of the American Academy of Child and Adolescent psychiatry. 1997;36:554–565. doi: 10.1097/00004583-199704000-00019. [DOI] [PubMed] [Google Scholar]
- Mendlowitz SL, Manassis K, Bradley S, Scapillato D, Miezitis S, Shaw BF. Cognitive-behavioral group treatments in childhood anxiety disorders: The role of parental involvement. Journal of the American Academy of Child and Adolescent psychiatry. 1999;38:1223–1229. doi: 10.1097/00004583-199910000-00010. [DOI] [PubMed] [Google Scholar]
- Mirza KA, Bhadrinath BR, Goodyer IM, Gilmour C. Post-traumatic stress disorder in children and adolescents following road traffic accidents. British Journal of Psychiatry. 1998;172:443–447. doi: 10.1192/bjp.172.5.443. [DOI] [PubMed] [Google Scholar]
- Nader K, Pynoos R, Fairbanks L, Frederick C. Children’s PTSD reactions one year after a sniper attack at their school. American Journal of Psychiatry. 1990;147:1526–1530. doi: 10.1176/ajp.147.11.1526. [DOI] [PubMed] [Google Scholar]
- Pine DS, Cohen JA. Trauma in children and adolescents: risk and treatment of psychiatric sequelae. Biological Psychiatry. 2002;51:519–531. doi: 10.1016/s0006-3223(01)01352-x. [DOI] [PubMed] [Google Scholar]
- Resick PA, Nishith P, Weaver TL, Astin MC, Feuer CA. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology. 2002;70:867–879. doi: 10.1037//0022-006x.70.4.867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rey JM, Starling J, Wever C, Dossetor DR, Plapp JM. Inter-rater reliability of global assessment of functioning in a clinical setting. Journal of Child Psychology and Psychiatry. 1995;36:787–792. doi: 10.1111/j.1469-7610.1995.tb01329.x. [DOI] [PubMed] [Google Scholar]
- Rothbaum BO, Foa EB. Post-traumatic stress disorder and sleep. New England Journal of Medicine. 2002;346:1334–1335. [PubMed] [Google Scholar]
- Shaffer D, Gould MS, Brasic J, Ambrosini P, Fisher P, Bird H, et al. A children’s global assessment scale (CGAS) Archives of General Psychiatry. 1983;40:1228–1231. doi: 10.1001/archpsyc.1983.01790100074010. [DOI] [PubMed] [Google Scholar]
- Stallard P, Velleman R, Salter E, Howse I, Yule W, Taylor G. A randomised controlled trial to determine the effectiveness of an early psychological intervention with children involved in road traffic accidents. Journal of Child Psychology and Psychiatry. 2006;47:127–134. doi: 10.1111/j.1469-7610.2005.01459.x. [DOI] [PubMed] [Google Scholar]
- Terr LC. Childhood traumas: an outline and overview. American Journal of Psychiatry. 1991;148:10–20. doi: 10.1176/ajp.148.1.10. [DOI] [PubMed] [Google Scholar]
- Van Ommeren M, de Jong JT, Komproe I. Post-traumatic stress disorder and sleep. New England Journal of Medicine. 2002;346:1334–1335. doi: 10.1056/NEJM200204253461719. [DOI] [PubMed] [Google Scholar]