Abstract
Decreased level of high density-lipoprotein cholesterol (HDL-C) is a rigorous predictor for future cardiovascular events. Much effort is being made to develop HDL-C–raising pharmacotherapies in the attempt to avert the pandemic of atherosclerotic disease. Important properties by which HDL-C–raising compounds are effective involve improvement of cholesterol uptake from macrophages in plaque for transport back to the liver, improvement of endothelial function, and anti-inflammatory effects. Vascular imaging can aid in the determination which HDL-C–raising compounds are effective. Ultrasound and MRI have proved suitable for assessment of structural changes of the vessel wall. Ultrasound can also be used or assessment of endothelial function. 18F-fluordeoxyglucose positron emission tomography has opened up the possibility to assess vessel wall inflammation. In this article we discuss these various imaging techniques and how they can assess efficacy as well as provide pathophysiologic information on the mechanism of action of novel HDL-C–raising drugs.
Keywords: High-density lipoprotein cholesterol, Atherosclerosis, Intima-media thickness, Flow-mediated vasodilatation, Endothelial function, Ultrasound, Magnetic resonance imaging, Inflammation, 18F-fluordeoxyglucose positron emission tomography
Introduction
High-density lipoproteins (HDL) are small vesicles comprised of phospholipids and stabilizing proteins, such as apolipoprotein A-I and A-II (ApoA-I, ApoA-II), that are produced by the liver to carry cholesterol and triglycerides in the blood stream. Prospective epidemiologic studies demonstrated that an increase of 1 mg/dL in HDL-C is associated with a 2%–3% reduction in the risk of cardiovascular events, and the predictive value of HDL-C is complementary to that of low-density lipoprotein cholesterol (LDL-C) levels [1]. This has led to the wide acceptance of the hypothesis that HDL has protective properties against atherosclerosis.
One of the major protective mechanisms of action of HDL is the uptake of cholesterol from peripheral cells, such as foam cells in atherosclerotic plaques, after which cholesterol is either transported directly to the liver for excretion into the bile, or shuttled to LDL. This process is also termed “reverse cholesterol transport” (RCT). Other important properties of HDL include favorable effects on endothelial function as well as anti-inflammatory effects [2].
As a result of the pivotal role of HDL in protection against atherosclerosis, HDL has become the most promising target for pharmacologic intervention. In order to assess the efficacy of rapidly evolving novel HDL-C–raising compounds, non-invasive vascular imaging techniques can be utilized. An appealing facet of vascular imaging is that it can specifically address relevant processes in atherosclerosis, such as changes in vessel wall thickness, plaque size and composition, endothelial function, and plaque inflammation, which can aid the decision making on whether or not to proceed testing the drug in a large clinical endpoint study. In this review, we reflect on the various imaging techniques that can be used to assess the efficacy of HDL-C–raising therapies.
Intima-Media Thickness Measurement
Carotid intima-media thickness (CIMT) can be measured non-invasively with B-mode ultrasound. The lumen-intima and media-adventitia interfaces of the carotid artery walls cause reflection of the ultrasound waves, which become visible as the typical “double line pattern” on the ultrasound image (Fig. 1). Intimal thickening is the first manifestation of atherosclerosis and is caused by the accumulation of lipids in the artery wall that occurs over the course of decades. Therefore, favorable effects of HDL-C–raising drugs on CIMT progression may be related to improvement of the RCT.
Fig. 1.
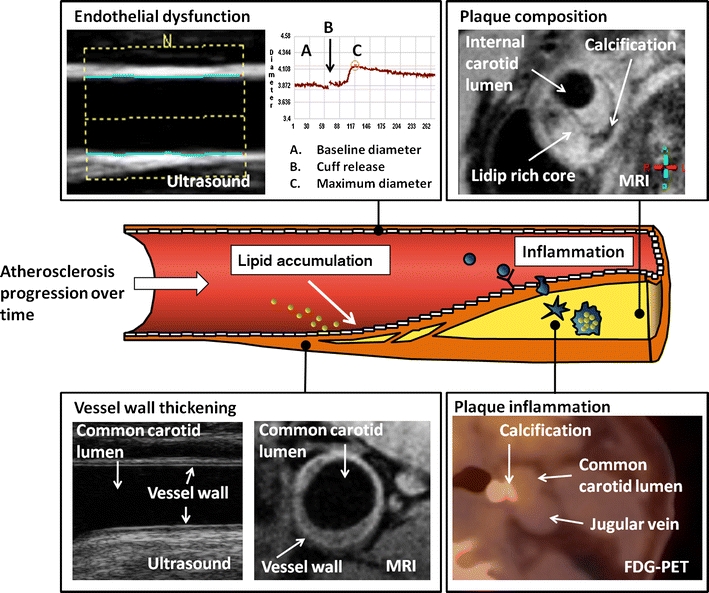
Various imaging modalities that can address different processes in atherosclerosis. Upper left: brachial artery endothelial function measurement with ultrasound (courtesy of Eric de Groot). The brachial artery diameter is measured at baseline and after cuff release and used to calculate the flow-dependent vasodilatation. Lower left: carotid vessel wall thickness measurement by ultrasound on the left (courtesy of Eric de Groot) and MRI on the right (courtesy of Aart Nederveen). Upper right: MRI of carotid artery plaque composition (courtesy of Aart Nederveen). Lower right: 18F-fluordeoxyglucose positron emission tomography (FDG-PET)/CT imaging of carotid artery plaque. Plaque calcification is visible on the CT scan (courtesy of Jan Bucerius)
Ultrasound CIMT offers good inter-scan and good inter- and intra-observer reproducibility with intraclass correlation coefficients above 0.90 in recent trials [3]. Furthermore, the measurement of CIMT has been validated in various large, prospective, epidemiologic studies. In fact, a systematic review and meta-analysis showed that the pooled estimates of hazard ratios per 0.10-mm difference in CIMT, adjusted for age and sex, are 1.15 for myocardial infarction (MI) and 1.18 for stroke (Table 1) [4]. The fact that no ionizing radiation is involved, no contrast agent needs to be injected, and the fact that ultrasound is relatively cheap and widely available has made the technique the most used measurement for assessment of cardiovascular drug efficacy.
Table 1.
Various imaging modalities that can be used for assessment of HDL-C–raising drugs
| Imaging modality | Outcome parameter | Reproducibility(ICC) | Predictive value of future CVD | Correlation with HDL-C | HDL-C–raising drugs investigated | |
|---|---|---|---|---|---|---|
| Vessel wall thickening | US | IMT | >0.90 [3] | HR 1.15 per 0.10 mm IMT difference [4] | Yes [5–7] | Niacin [8, 9, 10••, 11, 12], torcetrapib [13] |
| Plaque vulnerability | MRI | MWA or NWI | >0.95 [17] | Under investigation [23] | Yes [24•] | Niacin [27], dalcetrapib |
| MRI | AHA plaque type, LRNC, IPH, calcification | >0.90 [18] | HR 5–17 for presence of IPH or plaque rupture [19, 20, 21, 22•] | No [25, 26] | Niacin [28] | |
| Endothelial function | US | FMD (%) | >0.85 [29] | HR 0.84–0.91 per SD of FMD [30, 31••] | Yes [30, 32] | Niacin [33, 34], rHDL [35, 36], dalcetrapib [37] |
| Vessel wall inflammation | FDG-PET | SUV or TBR | >0.90 [46] | Under investigation [23] | Yes [44, 45] | Dalcetrapib |
AHA—American Heart Association; CVD—cardiovascular disease; FDG-PET—18F-fluordeoxyglucose positron emission tomography; FMD—flow-mediated vasodilatation; HDL-C—high-density lipoprotein cholesterol; HR—hazard ratio; ICC— intraclass correlation coefficient; IMT—intima-media thickness; IPH—intraplaque hemorrhage; LRNC—lipid-rich necrotic core; MWA—mean wall area; NWI—normalized wall index; rHDL—reconstituted high-density lipoprotein; SUV—standard uptake value; TBR—target-to-background ratio; US—ultrasound.
Various epidemiologic trials have investigated the relationship between HDL-C levels and CIMT and showed that low levels of HDL-C were associated with thicker CIMT. Recently, the Multi-Ethnic Study of Atherosclerosis, a cross-sectional study in 4792 subjects without coronary artery disease (CAD) or lipid-lowering therapy, showed that men with HDL-C ≤40 mg/dL and women with HDL-C ≤50 mg/dL with otherwise normal lipid levels had 0.021-mm thicker CIMT than subjects with normal HDL-C levels [5]. The Atherosclerosis Risk in Communities (ARIC) study showed in 15,792 subjects that decreased HDL-C levels were associated with accelerated progression of CIMT in a longitudinal follow-up study [6].
Furthermore, studies in families with genetic mutations in ATP-binding cassette transporter A1 (ABCA1), lecithin: cholesteryl acyltransferase (LCAT), or ApoA-I, causing marked decrease in HDL-C levels, showed that carriers had increased CIMT when compared to unaffected age-matched controls [7], supporting a causal role for HDL in protection against atherogenesis.
HDL-C–raising therapies have been investigated in various CIMT trials (Table 1). The efficacy of niacin on CIMT progression has been investigated in the Arterial Biology for the Investigation of the Treatment Effects of Reducing Cholesterol–HDL and LDL Treatment Strategies (ARBITER 2, 3 and 6–HALTS) [8, 9, 10••], the Cholesterol Lowering Atherosclerosis Study CLAS [11], and a study by Mack et al. [12]. These studies showed that niacin effectively slows atherosclerosis progression and its efficacy is already visible after a single year of therapy. A caveat, however, is that in addition to HDL-C, niacin also affects LDL-C, triglycerides, remnant particles, lipoprotein (a), and inflammatory biomarkers, so changes in CIMT cannot solely be attributed to its HDL-C–raising properties.
Another drug that raises HDL-C by inhibition of cholesteryl ester transfer protein (CETP) inhibition, torcetrapib, was investigated in the Rating Atherosclerotic Disease Change by Imaging with a New CETP Inhibitor (RADIANCE) 1 [3] and 2 [13] trials. The trials did not show any benefit of torcetrapib on CIMT progression. In fact, in RADIANCE 1, an increase of CIMT was observed. These unexpected findings were in line with the outcome of the morbidity and mortality study in 15,067 patients at high CAD risk, in which a marked increase in all-cause mortality was observed in the torcetrapib group [14]. Later studies revealed off-target effects of torcetrapib that may have annihilated the cardiovascular benefit of raising HDL. Torcetrapib raised blood pressure, accompanied by an upregulation of the renin angiotensin system and the endothelin system in both adrenals as well as aortic tissue [15].
MRI of Vessel Wall Thickness, Plaque Size, and Composition
MRI has emerged as one of the leading in vivo imaging techniques for atherosclerosis because it enables imaging of all stages of atherosclerosis, from healthy vessels to advanced disease (Fig. 1) [16, 17]. By obtaining multiple images, each differently weighted for the spin-lattice relaxation time (T1), the spin-spin relaxation time (T2), and the proton density (PD), plaque components such as intra-plaque hemorrhage, lipid-rich necrotic core, and calcification can be discriminated [16].
Assessment of vessel wall thickening by MRI reflects the accumulation of lipids in the intima of the vessel wall in the earlier stages of atherosclerosis, whereas identification of lipid-rich necrotic core depicts advanced atherosclerosis. Assessing changes in either vessel wall thickening or lipid-rich necrotic core size by treatment with HDL-C–raising drugs enables one to address the role of the favorable effects of HDL on RCT.
Imaging of vessel wall thickness has proved to be highly reproducible, with intraclass correlation coefficients above 0.95 [17]. Imaging of plaque size and composition has also shown good reproducibility, with intraclass correlation coefficients above 0.90 (Table 1) [18].The predictive value for future cardiovascular events of imaging vessel wall thickness by MRI has not yet been investigated. However, MRI of vessel wall thickness is highly correlated with ultrasound CIMT [17], so it is to be expected that the predictive value of both modalities will be in the same order of magnitude.
The relation between plaque size and composition has been investigated in various MRI studies. Underhill et al. [19] showed that compositional changes in MRI-characterized atherosclerotic plaque were associated with future risk of plaque surface disruption. In 85 patients with baseline 50%–79% carotid stenoses, increased plaque surface disruption at 3 years was predicted by baseline lipid-rich necrotic core size and intraplaque hemorrhage [19]. Takaya et al. [20] showed in a longitudinal follow-up study in 154 patients with asymptomatic 50%–79% carotid stenosis that presence of thin or ruptured fibrous cap and intraplaque hemorrhage were strong predictors of future ipsilateral cerebrovascular events with hazard ratios of 17.0 (P < 0.001) and 5.2 (P = 0.005), respectively. Similar results were found in a prospective longitudinal cohort study in 64 symptomatic patients where intraplaque hemorrhage was a strong predictor for future ipsilateral cerebrovascular events (hazard ratio 9.8; P = 0.03) [21].
Parmar et al. [22•] investigated 78 patients within 48 h of onset of transient ischemic attack (TIA) or stroke symptoms. Carotid MRI was performed in all participants, and plaques were classified according to the American Heart Association classification system. Type VI plaque (cap rupture, hemorrhage, and/or thrombosis) was the strongest predictor of a diagnosis of ipsilateral TIA or stroke, with an odds ratio of 11.7 [22•]. Larger studies that investigate the predictive value for cardiovascular events are currently ongoing and will provide more information on this topic in the near future (Table 1) [23].
A recent study that showed a strong relation between MRI vessel wall thickness and HDL-C was a study in carriers of LCAT mutations [24•]. In this study, 40 carriers were compared to 40 age-matched controls. Carriers had 38% decreased HDL-C levels, which was accompanied with a marked increase in vessel wall thickness when compared to unaffected controls, indicating that decreased HDL-C due to LCAT dysfunction leads to accelerated atherogenesis.
Concerning the relation between HDL-C and plaque size and composition assessed by MRI, no clear relationship was found in epidemiologic studies. In the ARIC study, carotid MRI was performed in 1769 subjects at baseline and after 18 years of follow-up. There was neither a relation between plaque size and HDL-C, nor was there a relation between presence of a lipid-rich necrotic core and HDL-C [25]. Similarly, no relation between lipid-rich necrotic core presence and HDL-C was found in 214 patients selected from the Multi-Ethnic Study of Atherosclerosis [26]. Interestingly, there was also a lack of relationship between lipid-rich necrotic core presence and other traditional risk factors. Reasons for this lack of relation with risk factors remain to be elucidated. Potentially technical limitations for identifying lipid-rich necrotic core may have played a role. Another issue might be the fact that patient selection was based on presence of advanced atherosclerosis in both studies. Selecting such a population might restrict the range of values and possible association with risk factors.
MRI of vessel wall thickness has also been used to investigate the efficacy of HDL-C–raising compounds (Table 1). Lee et al. [27] performed a double-blind, randomized placebo-controlled MRI study to assess if niacin on top of conventional statin therapy could reduce carotid atherosclerosis progression. MRI scans were performed at baseline and 1 year follow-up in 71 patients with low HDL-C (<40 mg/dL) and either type 2 diabetes with coronary heart disease (CHD) or carotid/peripheral atherosclerosis and showed that niacin significantly reduced progression of carotid wall thickness. Furthermore, an ongoing MRI trial, the dal-PLAQUE imaging study (ClinicalTrials.gov Identifier: NCT00655473), is currently investigating the efficacy of the cholesteryl ester transferase inhibitor dalcetrapib. This multi-center, randomized placebo-controlled trial is investigating the effect of dalcetrapib therapy on plaque progression in 130 patients with CHD or CHD-risk equivalent. MRI scans will be performed at baseline and after 6, 12, and 24 months of dalcetrapib therapy. Results are expected to be published in 2011.
The Carotid Plaque Composition Study is a currently ongoing study in 123 CAD patients that is investigating the efficacy of niacin in combination with atorvastatin and colesevelam on plaque size and composition [28].
Brachial Artery Endothelial Function Assessment
Endothelial cells form the inner lining of the vasculature and are a key regulator in preserving vascular heath. B-mode ultrasound flow-mediated vasodilatation (FMD) of the brachial artery is a technique that can be utilized to assess beneficial effects of HDL-C–raising drugs on endothelial function [29]. The measurement is done by assessing end-diastolic brachial artery diameters continually before and after 5 min of forearm ischemia (Fig. 1). The superimposed blood flow and increased shear stress after ischemia stimulates local nitric oxide (NO) release from the endothelium, resulting in vasodilation.
Under standardized environmental conditions, with adequate imaging equipment, protocols, analysis software, and experienced sonographers, FMD has shown to be a reproducible measurement (Table 1) [29]. A major advantage of FMD is that effects of drugs can be observed after short-term treatment, and due to the non-invasive nature of this modality, measurements can be repeatedly performed in a short period of time.
To assess the capability of FMD to predict future cardiovascular events, the Cardiovascular Health Study was conducted [30]. Baseline FMD measurements were performed in 2792 adults aged 72 to 98 years and all participants were followed for 5 years. This study showed that FMD greater than the sex-specific median was a significant predictor of future cardiovascular events, with a hazard ratio of 0.91 (95% CI, 0.83–0.99; P = 0.02 per unit SD of FMD). Similar results were found in 3026 subjects of the Multi-Ethnic Study of Atherosclerosis, in which FMD was significantly associated with incident cardiovascular events, with a hazard ratio of 0.84 (95% CI, 0.71–0.99; P = 0.04 per unit SD of FMD) (Table 1) [31••].
Physiologic mechanisms linking HDL to endothelial function and NO bioavailability have been established in several experimental studies. Yuhanna et al. showed that HDL stimulates endothelial nitric oxide synthase (eNOS) via the scavenger receptor B type I (SR-BI) receptor through a process that requires ApoA-I binding. HDL-associated lysophospholipids were shown to be responsible for the vasodilatory effect of HDL via a lysophospholipid receptor (sphingosine-1-phosphate receptor), causing Akt-mediated activation of eNOS.
Yeboah et al. [32] showed in 2792 subjects in the Cardiovascular Health Study that HDL-C was highly correlated with FMD. Moreover, in 3026 subjects of the Multi-Ethnic Study of Atherosclerosis, decreased HDL-C levels were associated with decreased FMD, with a hazard ratio of 0.78 (95%CI, 0.64–0.96; P = 0.020 per unit SD of FMD) [32]. Other clinical evidence of the relation between HDL-C and endothelial function comes from studies in carriers of ApoA-I gene defects. Heterozygote carriers of such mutations have a 50% decrease in ApoA-I and 63% decrease in serum HDL-C levels and were also observed to have marked reduction in FMD when compared to controls [7].
Regarding HDL-C–raising drugs, a few small FMD studies investigating the effect of niacin have been performed with mixed results (Table 1). Benjό et al. [33] observed that niacin improved FMD when compared to placebo in 22 subjects. Warnholtz et al. [34] performed a randomized, double-blind, placebo-controlled trial in 106 CAD patients investigating the efficacy of 12 weeks of niacin therapy and found no effect on FMD, although some benefit on FMD was observed in the lowest HDL-C tertile.
Infusion of reconstituted HDL (rHDL) was investigated in studies by Spieker et al. [35] and Nieuwdorp et al. [36]. Endothelial function was measured by FMD as well as venous occlusion plethysmography, and both studies showed that rHDL infusion rapidly normalizes endothelium-dependent vasodilation by increasing NO bioavailability.
Currently, a randomized, placebo-controlled trial (dal-VESSEL) is being conducted to investigate the efficacy of the CETP protein inhibitor dalcetrapib on FMD in 476 patients with CAD or CAD-risk equivalents and HDL-C <50 mg/dL (ClinicalTrials.gov identifier: NCT00655538) [37••].
FDG-PET Imaging of Vessel Wall Inflammation
The inflammatory response to the accumulation of oxidized lipids in the artery wall plays a pivotal role in the atherosclerotic disease process, and plaque inflammation is associated with plaque rupture and atherothrombotic events. 18F-fluordeoxyglucose positron emission tomography (FDG-PET) is a highly sensitive modality that can be utilized as a surrogate imaging marker for vessel wall inflammation (Fig. 1) [38]. The effect of HDL-C–raising drugs on FDG uptake in the vessel wall can provide insight in the anti-inflammatory property of HDL in the atherosclerotic disease process.
To obtain FDG-PET images, positron-emitting radionuclides incorporated into a glucose analogue (FDG) are injected into the circulation of a patient prior to imaging. Subsequently, the circulating FDG will be actively taken up by cells via glucose transporters. Inside the cells, FDG is phosphorylated into FDG-6 phosphate by hexokinase and not further metabolized. This leads to a relatively increased uptake and retention of FDG in cells that are metabolically active [38]. The positrons that are emitted by FDG travel a short distance in the body (<1 mm) until they interact with an electron, producing two gamma photons that travel out of the body, in (almost) opposite directions, where they are detected by the scintillators of the PET scanner.
Inflammatory cells, especially when they are activated, have high metabolic activity, and therefore high FDG uptake [38]. Studies in experimental atherosclerotic rabbit models showed that FDG accumulates in atherosclerotic lesions and correlates with the number of macrophages in the plaque [39]. Also, in human endarterectomy studies, FDG accumulation in plaque was shown to be correlated with plaque macrophage content [40].
Rominger et al. [41•] performed an FDG-PET imaging study in 334 otherwise asymptomatic cancer patients with a follow-up of 29 months and showed that target-to-background ratio (TBR) ≥1.7 was significantly associated with occurrence of future vascular events. Paulmier et al. [42] performed FDG-PET in a cohort of 1140 patients suffering from cancer, of which 45 were identified with high FDG uptake in the large arteries, who were then matched for age, gender, type of cancer, and conventional CVD risk factors with 56 patients with low FDG uptake in the large arteries. They showed that enhanced FDG uptake was predictive for a history of CVD and the occurrence of CVD in the 6 months after PET imaging [42]. Rudd et al. [43] performed a carotid FDG-PET scan shortly after symptom onset in eight patients suffering from TIA and showed that symptomatic carotid artery plaques had higher FDG uptake than asymptomatic plaques.
The High Risk Plaque Initiative is a large, ongoing epidemiologic study that includes FDG-PET imaging and will provide more information on the predictive value of FDG-PET in the near future [23].
The relation between FDG-PET and HDL-C levels and other risk factors has also been investigated. Tahara et al. [44] performed FDG-PET imaging in 261 patients recruited for cancer screening and found an independent relation between FDG uptake and HDL-C, waist circumference, hypertension, insulin resistance, C-reactive protein levels, and ultrasound CIMT. Rudd et al. [45] performed FDG-PET in 41 patients with cardiovascular disease or at least three cardiovascular risk factors and showed marked increased vessel wall inflammation in patients with a history of CAD versus no cardiovascular disease and also in men compared to women. FDG uptake also correlated with serum levels of the inflammatory biomarkers matrix metalloproteinase and negatively correlated with adiponectin [45]. The relation with HDL-C was not investigated in this study.
The fact that FDG-PET is a non-invasive measure of vessel wall inflammation with excellent reproducibility [46] has made this an attractive modality to assess efficacy of cardiovascular drugs with anti-inflammatory properties (Table 1).
Tahara et al. [47] imaged 43 patients suffering from cancer disease with FDG-PET before and after 3 months of medication with a low-dose statin (simvastatin, 20 mg daily). They found a significant reduction in carotid artery FDG uptake as compared to a placebo group [47].
Lee et al. [48] showed a 65% reduction in the number of vascular regions that accumulated FDG in a group of 60 asymptomatic subjects after 17 months of lifestyle and dietary modifications. Interestingly, both the studies by Tahara et al. [47] and Lee et al. [48] found that the magnitude of the FDG-PET signal reduction was closely related with the rise in HDL-C.
Recently, a study in 99 CAD patients investigated the effect of a p38 mitogen-activated protein kinase (p38MAPK) inhibitor on plaque inflammation as assessed by FDG-PET and observed a marked decrease in FDG uptake in the carotid arteries [49••]. Another recent study compared the effect of pioglitazone versus glimepiride therapy in 49 patients with impaired glucose tolerance and observed a marked reduction in FDG uptake in the pioglitazone group [50•].
Concerning HDL-C–raising therapies, the ongoing multi-center, randomized, placebo-controlled dal-PLAQUE imaging study (ClinicalTrials.gov identifier: NCT00655473) is using FDG-PET to investigate the efficacy of the cholesteryl ester transferase inhibitor dalcetrapib. FDG-PET imaging of the carotid and aortic arteries will be performed in 130 patients with CHD or CHD-risk equivalent, at baseline and after 3 and 6 months of dalcetrapib therapy.
Conclusions
Imaging of atherosclerosis can be utilized to assess efficacy as well as provide pathophysiologic information on the mechanism of action of novel of HDL-C–raising drugs. Much effort has been made over the past decades to develop ultrasound, MRI, and most recently FDG-PET to provide efficacy measures that can be used to assist in decision making and whether or not to proceed with novel anti-atherogenic drugs in costly and time-consuming mortality and morbidity trials. The current armamentarium of imaging modalities is capable of providing insight in drug effects on atherosclerosis progression, endothelial function, and vessel wall inflammation and will play a crucial role in evaluating emerging HDL-C–raising compounds.
Acknowledgments
Disclosure
Zahi A. Fayad is board member of Roche and has received grants from Siemens and Philips. Raphaël Duivenvoorden reports no potential conflict of interest relevant to this article.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance •• Of major importance
- 1.Gordon DJ, Probstfield JL, Garrison RJ, et al. High-density lipoprotein cholesterol and cardiovascular disease. Four prospective American studies. Circulation. 1989;79:8–15. doi: 10.1161/01.cir.79.1.8. [DOI] [PubMed] [Google Scholar]
- 2.Besler C, Heinrich K, Riwanto M, et al. High-density lipoprotein-mediated anti-atherosclerotic and endothelial-protective effects: a potential novel therapeutic target in cardiovascular disease. Curr Pharm Des. 2010;16:1480–93. doi: 10.2174/138161210791051013. [DOI] [PubMed] [Google Scholar]
- 3.Kastelein JJ, van Leuven SI, Burgess L, et al. Effect of torcetrapib on carotid atherosclerosis in familial hypercholesterolemia. N Engl J Med. 2007;356:1620–30. doi: 10.1056/NEJMoa071359. [DOI] [PubMed] [Google Scholar]
- 4.Lorenz MW, Markus HS, Bots ML, et al. Prediction of clinical cardiovascular events with carotid intima-media thickness: a systematic review and meta-analysis. Circulation. 2007;115:459–67. doi: 10.1161/CIRCULATIONAHA.106.628875. [DOI] [PubMed] [Google Scholar]
- 5.Paramsothy P, Knopp RH, Bertoni AG, et al. Association of combinations of lipid parameters with carotid intima-media thickness and coronary artery calcium in the MESA (Multi-Ethnic Study of Atherosclerosis) J Am Coll Cardiol. 2010;56:1034–41. doi: 10.1016/j.jacc.2010.01.073. [DOI] [PubMed] [Google Scholar]
- 6.Chambless LE, Folsom AR, Davis V, et al. Risk factors for progression of common carotid atherosclerosis: the Atherosclerosis Risk in Communities Study, 1987–1998. Am J Epidemiol. 2002;155:38–47. doi: 10.1093/aje/155.1.38. [DOI] [PubMed] [Google Scholar]
- 7.Hovingh GK, de Groot E, van der Steeg W, Boekholdt SM, Hutten BA, Kuivenhoven JA, Kastelein JJ. Inherited disorders of HDL metabolism and atherosclerosis. Curr Opin Lipidol. 2005;16(2):139–45. doi: 10.1097/01.mol.0000162318.47172.ef. [DOI] [PubMed] [Google Scholar]
- 8.Taylor AJ, Sullenberger LE, Lee HJ, et al. Arterial biology for the investigation of the treatment effect of reducing cholesterol (ARBITER) 2. A double-blind, placebo controlled study of extended-release niacin on atherosclerosis progression in secondary prevention patients treated with statins. Circulation. 2004;110:3512–7. doi: 10.1161/01.CIR.0000148955.19792.8D. [DOI] [PubMed] [Google Scholar]
- 9.Taylor AJ, Lee HJ, Sullenberg LE. The effect of 24 months of combination statin and extended-release niacin on carotid intima-media thickness: ARBITER 3. Curr Med Res Opin. 2006;22:2243–50. doi: 10.1185/030079906X148508. [DOI] [PubMed] [Google Scholar]
- 10.Taylor AJ, Villines TC, Stanek EJ, et al. Extended-release niacin or ezetimibe and carotid intima–media thickness. N Engl J Med. 2009;361:2113–22. doi: 10.1056/NEJMoa0907569. [DOI] [PubMed] [Google Scholar]
- 11.Blankenhorn DH, Selzer RH, Crawford DW, et al. Beneficial effects of cholestipol-niacin therapy on common carotid artery. Two- and four-year reduction in intima-media thickness measured by ultrasound. Circulation. 1993;88:20–8. doi: 10.1161/01.cir.88.1.20. [DOI] [PubMed] [Google Scholar]
- 12.Mack WJ, Selzer RH, Hodis HN, et al. One-year reduction and longitudinal analyses of carotid intima-media thickness associated with colestipol/niacin therapy. Stroke. 1993;24:1779–83. doi: 10.1161/01.str.24.12.1779. [DOI] [PubMed] [Google Scholar]
- 13.Bots ML, Visseren FL, Evans GW, et al. RADIANCE 2 Investigators. Torcetrapib and carotid intima-media thickness in mixed dyslipidaemia (RADIANCE 2 study): a randomised, double-blind trial. Lancet. 2007;370:153–60. doi: 10.1016/S0140-6736(07)61088-5. [DOI] [PubMed] [Google Scholar]
- 14.Barter PJ, Caulfield M, Eriksson M, et al. Effects of torcetrapib in patients at high risk for coronary events. N Engl J Med. 2007;357:2109–22. doi: 10.1056/NEJMoa0706628. [DOI] [PubMed] [Google Scholar]
- 15.Vergeer M, Bots ML, van Leuven SI, et al. Cholesteryl ester transfer protein inhibitor torcetrapib and off-target toxicity: a pooled analysis of the rating atherosclerotic disease change by imaging with a new CETP inhibitor (RADIANCE) trials. Circulation. 2008;118:2515–22. doi: 10.1161/CIRCULATIONAHA.108.772665. [DOI] [PubMed] [Google Scholar]
- 16.Yuan C, Beach KW, Smith LH, Jr, et al. Measurement of atherosclerotic carotid plaque size in vivo using high resolution magnetic resonance imaging. Circulation. 1998;98:2666–71. doi: 10.1161/01.cir.98.24.2666. [DOI] [PubMed] [Google Scholar]
- 17.Duivenvoorden R, de Groot E, Elsen BM, et al. In vivo quantification of carotid artery wall dimensions: 3.0-Tesla MRI versus B-mode ultrasound imaging. Circ Cardiovasc Imaging. 2009;2:235–42. doi: 10.1161/CIRCIMAGING.108.788059. [DOI] [PubMed] [Google Scholar]
- 18.Li F, Yarnykh VL, Hatsukami TS, et al. Scan-rescan reproducibility of carotid atherosclerotic plaque morphology and tissue composition measurements using multicontrast MRI at 3 T. J Magn Reson Imaging. 2010;31:168–76. doi: 10.1002/jmri.22014. [DOI] [PubMed] [Google Scholar]
- 19.Underhill HR, Yuan C, Yarnykh VL, et al. Predictors of surface disruption with MR imaging in asymptomatic carotid artery stenosis. Am J Neuroradiol. 2009;31:487–93. doi: 10.3174/ajnr.A1842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Takaya N, Yuan C, Chu B, et al. Association between carotid plaque characteristics and subsequent ischemic cerebrovascular events: a prospective assessment with MRI: initial results. Stroke. 2006;37:818–23. doi: 10.1161/01.STR.0000204638.91099.91. [DOI] [PubMed] [Google Scholar]
- 21.Altaf N, Daniels L, Morgan PS, et al. Detection of intraplaque hemorrhage by magnetic resonance imaging in symptomatic patients with mild to moderate carotid stenosis predicts recurrent neurological events. J Vasc Surg. 2008;47:337–42. doi: 10.1016/j.jvs.2007.09.064. [DOI] [PubMed] [Google Scholar]
- 22.Parmar JP, Rogers WJ, Mugler JP, 3rd, et al. Magnetic resonance imaging of carotid atherosclerotic plaque in clinically suspected acute transient ischemic attack and acute ischemic stroke. Circulation. 2010;122:2031–8. doi: 10.1161/CIRCULATIONAHA.109.866053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.http://www.hrpinitiative.com
- 24.Holleboom AG, Duivenvoorden R, van den Bogaard B, et al. Patients with Low Plasma High Density Lipoprotein-Cholesterol due to Mutations in the Gene Encoding for Lecithin: Cholesterol Acyl Transferase have Increased Atherosclerosis: A 3.0 Tesla MRI Study. Circulation. 2010;122:A17773. [Google Scholar]
- 25.Wagenknecht L, Wasserman B, Chambless L, et al. Correlates of carotid plaque presence and composition as measured by MRI: the Atherosclerosis Risk in Communities Study. Circ Cardiovasc Imaging. 2009;2:314–22. doi: 10.1161/CIRCIMAGING.108.823922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Wasserman BA, Sharrett AR, Lai S, et al. Risk factor associations with the presence of a lipid core in carotid plaque of asymptomatic individuals using high-resolution MRI: the multi-ethnic study of atherosclerosis (MESA) Stroke. 2008;39:329–35. doi: 10.1161/STROKEAHA.107.498634. [DOI] [PubMed] [Google Scholar]
- 27.Lee JM, Robson MD, Yu LM, et al. Effects of high-dose modified-release nicotinic acid on atherosclerosis and vascular function: a randomized, placebo-controlled, magnetic resonance imaging study. J Am Coll Cardiol. 2009;54:1787–94. doi: 10.1016/j.jacc.2009.06.036. [DOI] [PubMed] [Google Scholar]
- 28.Zhao XQ, Phan BA, Chu B, et al. Testing the hypothesis of atherosclerotic plaque lipid depletion during lipid therapy by magnetic resonance imaging: study design of Carotid Plaque Composition Study. Am Heart J. 2007;154:239–46. doi: 10.1016/j.ahj.2007.04.035. [DOI] [PubMed] [Google Scholar]
- 29.Donald AE, Halcox JP, Charakida M, et al. Methodological approaches to optimize reproducibility and power in clinical studies of flow-mediated dilation. J Am Coll Cardiol. 2008;51:1959–64. doi: 10.1016/j.jacc.2008.02.044. [DOI] [PubMed] [Google Scholar]
- 30.Yeboah J, Crouse JR, Hsu FC, et al. Brachial flow-mediated dilation predicts incident cardiovascular events in older adults: the Cardiovascular Health Study. Circulation. 2007;115:2390–7. doi: 10.1161/CIRCULATIONAHA.106.678276. [DOI] [PubMed] [Google Scholar]
- 31.Yeboah J, Folsom AR, Burke GL, et al. Predictive value of brachial flow-mediated dilation for incident cardiovascular events in a population-based study: the multi-ethnic study of atherosclerosis. Circulation. 2009;120:502–9. doi: 10.1161/CIRCULATIONAHA.109.864801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Yeboah J, Burke GL, Crouse JR, et al. Relationship between brachial flow-mediated dilation and carotid intima-media thickness in an elderly cohort: the Cardiovascular Health Study. Atherosclerosis. 2008;197:840–5. doi: 10.1016/j.atherosclerosis.2007.07.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Benjó AM, Maranhão RC, Coimbra SR, et al. Accumulation of chylomicron remnants and impaired vascular reactivity occur in subjects with isolated low HDL cholesterol: effects of niacin treatment. Atherosclerosis. 2006;187:116–22. doi: 10.1016/j.atherosclerosis.2005.08.025. [DOI] [PubMed] [Google Scholar]
- 34.Warnholtz A, Wild P, Ostad MA, et al. Effects of oral niacin on endothelial dysfunction in patients with coronary artery disease: results of the randomized, double-blind, placebo-controlled INEF study. Atherosclerosis. 2009;204:216–21. doi: 10.1016/j.atherosclerosis.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 35.Spieker LE, Sudano I, Hürlimann D, et al. High-density lipoprotein restores endothelial function in hypercholesterolemic men. Circulation. 2002;105:1399–402. doi: 10.1161/01.CIR.0000013424.28206.8F. [DOI] [PubMed] [Google Scholar]
- 36.Nieuwdorp M, Vergeer M, Bisoendial RJ, et al. Reconstituted HDL infusion restores endothelial function in patients with type 2 diabetes mellitus. Diabetologia. 2008;51:1081–4. doi: 10.1007/s00125-008-0975-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.•• Kastelein JJ, Duivenvoorden R, Deanfield J, et al.: Rationale and design of dal-VESSEL: a study to assess the safety and efficacy of dalcetrapib on endothelial function using brachial artery flow-mediated vasodilatation. Curr Med Res Opin. 2010 Dec 6. This is the first large, randomized, placebo-controlled ultrasound FMD trial to investigate the efficacy of the HDL-C–raising drug dalcetrapib. [DOI] [PubMed]
- 38.Rudd JHF, Hyafil F, Fayad ZA. Inflammation imaging in atherosclerosis. Arterioscler Thromb Vasc Biol. 2009;29:1009–16. doi: 10.1161/ATVBAHA.108.165563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Zhang Z, Machac J, Helft G, et al. Non-invasive imaging of atherosclerotic plaque macrophage in a rabbit model with F-18FDG PET: a histopathological correlation. BMC Nucl Med. 2006;6:3. doi: 10.1186/1471-2385-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Tawakol A, Migrino RQ, Bashian GG, et al. In vivo 18F-fluorodeoxyglucose positron emission tomography imaging provides a noninvasive measure of carotid plaque inflammation in patients. J Am Coll Cardiol. 2006;48:1818–24. doi: 10.1016/j.jacc.2006.05.076. [DOI] [PubMed] [Google Scholar]
- 41.Rominger A, Saam T, Wolpers S, et al. 18F-FDG PET/CT identifies patients at risk for future vascular events in an otherwise asymptomatic cohort with neoplastic disease. J Nucl Med. 2009;50:1611–20. doi: 10.2967/jnumed.109.065151. [DOI] [PubMed] [Google Scholar]
- 42.Paulmier B, Duet M, Khayat R, et al. Arterial wall uptake of fluorodeoxyglucose on PET imaging in stable cancer disease patients indicates higher risk for cardiovascular events. J Nucl Cardiol. 2008;15:209–17. doi: 10.1016/j.nuclcard.2007.10.009. [DOI] [PubMed] [Google Scholar]
- 43.Rudd JH, Warburton EA, Fryer TD, et al. Imaging atherosclerotic plaque inflammation with [18F]-fluorodeoxyglucose positron emission tomography. Circulation. 2002;105:2708–11. doi: 10.1161/01.CIR.0000020548.60110.76. [DOI] [PubMed] [Google Scholar]
- 44.Tahara N, Kai H, Yamagishi S, et al. Vascular inflammation evaluated by [18F]-fluorodeoxyglucose positron emission tomography is associated with the metabolic syndrome. J Am Coll Cardiol. 2007;49:1533–9. doi: 10.1016/j.jacc.2006.11.046. [DOI] [PubMed] [Google Scholar]
- 45.Rudd JH, Myers KS, Bansilal S, et al. Relationships among regional arterial inflammation, calcification, risk factors, and biomarkers: a prospective fluorodeoxyglucose positron-emission tomography/computed tomography imaging study. Circ Cardiovasc Imaging. 2009;2:107–15. doi: 10.1161/CIRCIMAGING.108.811752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rudd JH, Myers KS, Bansilal S, et al. (18)Fluorodeoxyglucose positron emission tomography imaging of atherosclerotic plaque inflammation is highly reproducible: implications for atherosclerosis therapy trials. J Am Coll Cardiol. 2007;50:892–6. doi: 10.1016/j.jacc.2007.05.024. [DOI] [PubMed] [Google Scholar]
- 47.Tahara N, Kai H, Ishibashi M, et al. Simvastatin attenuates plaque inflammation: evaluation by fluorodeoxyglucose positron emission tomography. J Am Coll Cardiol. 2006;48:1825–31. doi: 10.1016/j.jacc.2006.03.069. [DOI] [PubMed] [Google Scholar]
- 48.Lee SJ, On YK, Lee EJ, et al. Reversal of vascular 18F-FDG uptake with plasma high-density lipoprotein elevation by atherogenic risk reduction. J Nucl Med. 2008;49:1277–82. doi: 10.2967/jnumed.108.052233. [DOI] [PubMed] [Google Scholar]
- 49.Elkhawad M, Rudd JH, Sarov-Blat L, et al. Inhibition of p38 Mitogen-Activated Protein Kinase Attenuates Vascular and Systemic Inflammation in Patients with Atherosclerosis as Assessed by 18-F Fluorodeoxyglucose PET-CT. Circulation. 2010;122:A16936. [Google Scholar]
- 50.Mizoguchi M, Tahara N, Nitta Y, et al. Pioglitazone Attenuates Atherosclerotic Plaque Inflammation in Impaired Glucose Tolerance -Evaluation by Serial 18FFluorodeoxyglucose- Positron Emission Tomography/Computed Tomography. Circulation. 2010;122:A16505. [Google Scholar]


