Abstract
Objective
To examine the mechanisms linking health literacy to physical activity and self-reported health.
Methods
From 2005–2007, patients (N=330) with hypertension were recruited from safety net clinics. Path analytic models tested the pathways linking health literacy to physical activity and self-reported health.
Results
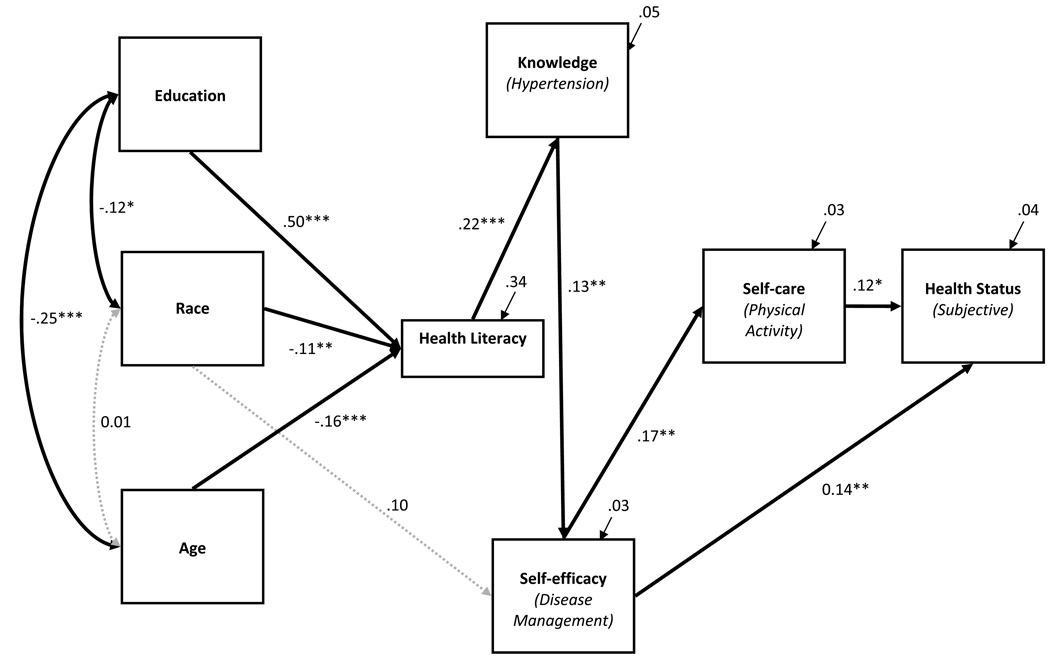
There were significant paths from health literacy to knowledge (r=0.22, P<0.001), knowledge to self-efficacy (r=0.13, P<0.01), self-efficacy to physical activity (r=0.17, P<0.01), and physical activity to health status (r=0.17, P<0.01).
Conclusions
Health education interventions should be literacy sensitive and aim to enhance patient health knowledge and self-efficacy to promote self-care behavior and desirable health outcomes.
Keywords: health literacy, health behavior, knowledge, self-efficacy, health status
Introduction
The association between limited health literacy and poor health has been supported across acute and chronic disease contexts.1–3 Patients’ health literacy skills may be the first step in a chain of factors impacting health.4,5 Although an accumulation of literature on the issue has emerged in the last 2 decades, the mechanisms by which health literacy impacts health are still unclear.5,6
Conceptual Causal Model Linking Health Literacy to Health
Paasche-Orlow and Wolf propose plausible causal pathways to explain the well-established association between health literacy and health.5 They describe systematic, interactional, and self-care mechanisms by which limited health literacy is most likely to lead to worse health outcomes.5 Drawing from the literature, they argue that social (eg, income, social support, culture, language), cognitive/physical (eg, memory, hearing, vision), and demographic (race/ethnicity, education, and age) factors determine health literacy skills. They then illustrate how limited health literacy might impact health outcomes at 3 distinct points along a continuum of health care, focusing on (1) access and use of health care,1,3,7 (2) provider-patient interactions,8 and (3) patient self-care.5 At each respective point, Paasche-Orlow and Wolf explore system factors (complexity, acute care orientation, tiered delivery model), provider factors (communication skills, teaching ability, time, patient-centered care), and extrinsic factors (support technologies, mass media, health education, resources) that could modify and/or mediate the relationship between patient health literacy and outcomes.5
Patient factors are also affected at each point along the continuum of health care.5 At the point of access and use of health care, limited health literacy could influence a patient’s navigation skills, self-efficacy, and/or perceived barriers to care.9 During provider-patient interactions, limited health literacy could infringe upon a patient’s knowledge, beliefs, and/or level of participation in clinical decision making.8 Limited health literacy could also negatively influence a patient’s motivation,10 problem-solving ability,11 self-efficacy,12 and/or knowledge4,12,13 required to accurately perform self-care behaviors. Paasche-Orlow and Wolf suggest that these aforementioned relationships operate in conjunction with system-, provider-, and extrinsic-level factors noted above and that these relationships exist within the causal pathway linking health literacy to outcomes.5
Health Literacy and Hypertension
Across chronic disease contexts, limited health literacy has been consistently related to determinants of self-care behavior (eg, knowledge and self-efficacy noted above),4,12,13 poor performance of self-care behavior (or the lack thereof),14 and worse health outcomes.3 In hypertension, limited health literacy has been associated with poor disease-related knowledge,4,15,16 poor medication-refill adherence,17 discrepancies in patient self-reported medication use with his or her medical record (ie, unreconciled medications),18 and worse blood pressure control.15 Limited health literacy has also been associated with an increased risk of hypertension, lower levels of physical function and activity, and worse subjective health status.19
Hypertension, Self-care, and Health Status
Leading health organizations endorse regular physical activity to prevent and treat hypertension and its complications.20 Regular physical activity has been shown to lower blood pressure,21 enhance endothelial vasodilator function,22 and prevent the development of left ventricular mass among individuals with hypertension.23 Synthesizing the research noted above and consistent with Paasche-Orlow and Wolf model, limited health literacy may affect both objective and subjective indicators of health status via compromised physical function and physical activity.19 Although Paasche-Orlow and Wolf do not explicitly discuss “behaviors” in their model, they do focus on “determinants of self-care,” which by nature highlights the importance of “self-care behaviors” in the causal chain. Determinants of physical activity in the hypertension literature are also consistent with the Paasche-Orlow and Wolf model. Specifically, motivation and self-efficacy have explained 44% of the variance in physical activity;24 and hypertension treatment knowledge has also shown predictive value.25
Empirical Validation of the Causal Pathways
The Paasche-Orlow and Wolf framework highlights both promising areas for intervention research and important gaps in our current understanding of the pathways linking health literacy to health outcomes. Their theoretical paper is one step in what needs to be an iterative process of model specification and clarification. Analytic approaches that test, validate, and/or refine the framework are needed to inform professional responses to the widespread problem of limited health literacy.26 For example, empirical support for the proposed relationships between health literacy, determinants of self-care, self-care behavior, and health outcomes would undoubtedly inform the design and content and improve the efficacy of patient-level interventions to address health literacy.
In this study, we sought to validate one third of the Paasche-Orlow and Wolf model. We focused solely on patient self-care pathways using data from adults with hypertension who were receiving care at safety net clinics in diverse areas of the United States. These data include variables on patient demographics, health literacy, disease-related knowledge, self-efficacy, and health status. Using a path analytic approach, we were able to test the following hypothesized paths in the Paasche-Orlow and Wolf model:
Patient demographic characteristics (race/ethnicity, education, and age) predict health literacy.
Health literacy predicts patient-level determinants of self-care (knowledge and self-efficacy).
Patient-level determinants of self-care predict self-care behavior (physical activity).
Self-care behavior predicts health status (subjective health).
In this way, the association between health literacy and health is hypothesized to be accounted for by a sequence of intervening variables (knowledge, self-efficacy, and self-care behavior).
METHODS
Setting and Participants
We recruited consecutive patients with diagnosed hypertension at scheduled appointments from 6 primary care safety net clinics in Grand Rapids, Michigan; Chicago, Illinois; and Shreveport, Louisiana. Clinics in Grand Rapids (n=2) and Chicago (n=2) were affiliated with federally qualified health centers. One clinic in Shreveport was a community health center; and the other, an ambulatory care clinic of a public hospital. The institutional review boards at each location approved the study procedures. Eligible participants were at least 18 years old, had a diagnosis of hypertension in their medical record, and had a clinic appointment between July 2006 and August 2007. Patients were ineligible if they did not speak English or if the clinic nurse determined (by interaction or chart documentation) they were too ill or cognitively impaired to participate. Nurses identified 377 potentially eligible patients scheduled for clinic appointments and referred them to study staff. Informed consent was obtained on 334 scheduled interviews. Four of these patients did not complete the interview (N=330). A response rate was determined following the American Association for Public Opinion Research (AAPOR) standards, estimating 87.5% of approached eligible patients participated in the study.27
Data Collection
Study personnel conducted in-person interviews in the clinics. Information on demographic characteristics, such as education (1= grades 1–8, 2=grades 9–11, 3=high school, 4=>high school), race/ethnicity (0=white, 1=African American), and age (continuous) were collected. Additional measures included health literacy, disease management knowledge, self-efficacy, physical activity, and subjective health.
Health Literacy
Patients’ health literacy was assessed using the short version of the Test of Functional Health Literacy in Adults (S-TOFHLA). The S-TOFHLA has 2 parts. One part is a reading comprehension assessment that involves passages of text about medical topics from which every fifth to seventh word is omitted. Patients must select a suitable word to insert in the missing place from 4 multiple-choice options. The second part assesses numeracy by presenting patients with questions to determine their ability to use and interpret numbers when reading hospital forms and labeled prescription vials. Scores on the S-TOFHLA range from 0 to 100 and can be categorized as follows: inadequate (0–53 correct answers), marginal (54–66), and adequate health literacy (67–100). The S-TOFHLA has demonstrated good internal consistency, reliability, and validity as a categorized and continuous measure of health literacy (α = 0.98).3,28–30 We relied on the continuous score to increase the predictive power in our path analytic models.
Knowledge
Hypertension knowledge was assessed by asking patients a series of questions about the characteristics and symptoms of high blood pressure. Fourteen multiple-choice items made up the scale, and a total score was taken from all questions. Patients were asked about a normal blood pressure reading, lifestyle activities that change blood pressure readings, symptoms of high blood pressure, and complications. The scale was developed for use in the Prudential Health Literacy Survey4 and was derived from a reliable and valid measure of hypertension knowledge (α = 0.70).16
Self-efficacy
Self-efficacy to manage high blood pressure was assessed by asking patients how confident they were in (1) doing all the things necessary to manage their blood pressure; (2) judging when changes in their blood pressure mean they should visit a doctor; (3) doing different activities and tasks to manage their blood pressure so as to reduce the need to see a doctor; (4) reducing the emotional distress caused by their blood pressure; and (5) doing things, other than just taking medication, to reduce how much their blood pressure affects their everyday life. Response options were in Likert format ranging from 1 = not at all confident to 10 = totally confident. In the current study, internal consistency reliability for this measure was α = 0.76.
Self-care Behavior (Physical Activity)
Physical activity frequency was measured with a single-item taken from a 2-item scale that measures both the frequency and duration of physical activity over the past 4 weeks.31 Response options were 1 = never, 2 = only once or twice, 3 = at least once a week, 4 = 3 to 4 times each week, and 5 = every day.
Health Status
Subjective health was assessed with a widely used general self-rated health question that asks respondents to report how they thought their health was in general.32 Response options were in Likert format ranging from 1 = Poor to 5 = Excellent. This single question has demonstrated strong predictive validity with self-care behaviors,33 objective indicators of health,33 and mortality.34 Relevant to our study is prior work showing that a single item of self-rated health is sensitive to changes in physical activity.35,36
Data Analyses
Patients were categorized as having inadequate health literacy (scores 0–53) or having marginal/adequate health literacy (scores 54–100) and compared using independent samples t-tests for continuous variables and chi-square tests for categorical variables. Structural equation models (SEM) specifying the relationships among variables were estimated using AMOS, version 17. Advantages of this procedure include the generality and flexibility of model specification and the ability to assess fit of the hypothesized model to the observed data. Model fit was examined with the comparative fit index (CFI) and root mean error of approximation (RMSEA).37 CFI values exceeding 0.90 and RMSEA values below 0.08 indicate adequate model fit.37 Hypotheses regarding the specific structural relations of the constructs in the model were also evaluated through inspection of the direction and magnitude of the path coefficients.
Two path analytic models were estimated with a correlation matrix generated by 330 cases, a sample size considered to be of adequate power to detect large effects.38,39 Demographic information (education, race, and age), health literacy, knowledge, self-efficacy, self-care, and subjective health variables were used to estimate one third of the Paasche-Orlow and Wolf framework (ie, patient factors within the self-care domain). Model 1 (the full model) tested whether demographic factors predicted health literacy; whether health literacy predicted determinants of self-care (knowledge and self-efficacy); whether determinants of self-care predicted self-care behavior (physical activity); and whether self-care behavior predicted health status (subjective health). Although we were interested in only these pathways, all potential paths between variables were included to test both those hypothesized to be significant and those hypothesized to be nonsignificant. Model 2 (the trimmed model) omitted all nonsignificant paths from Model 1. Chi-square difference tests were performed between models 1 and 2 to identify the most parsimonious and final model.
RESULTS
Table 1 provides both an overall statistical description of the study population and stratifies the sample by inadequate and marginal/adequate health literacy level. The mean age of patients was 53.6 years (SD=12.0); 67.9% were female, and 78.5% were African American. A third of subjects were recruited from each of the study sites: 30.6% from Chicago, 36.1% from Grand Rapids, and 33.3% from Shreveport. The majority of participants (65.8%) were unemployed, and 43.9% did not have any health insurance coverage. Subjects reported having hypertension for an average of 11 years (SD=10.0), and 47.6% had chart-confirmed controlled blood pressure.
Table 1.
Sociodemographic and Clinical Characteristics of Respondents Stratified by Health Literacy Level
| Variable | Total | Health Literacy | |
|---|---|---|---|
| (N=330) | Inadequate (n=100) |
Marginal/ Adequate (n=230) |
|
| Age, Mean (SD) | 53.6 (12.0) | 58.4 (11.7)*** | 51.5 (11.6) |
| Female, % | 67.9 | 63.0 | 70.6 |
| African American Race, % | 78.5 | 85.9 | 79.2 |
| Education, % | |||
| Grades 1–8 | 13.1 | 29.3*** | 6.1 |
| Grades 9–11 | 26.2 | 41.4*** | 19.7 |
| High School | 31.4 | 20.2*** | 36.2 |
| > High School | 29.3 | 9.1*** | 38 |
| Married, % | 30.6 | 25.0 | 33.2 |
| Insurance Coverage, % | |||
| Private | 10.0 | 12.0 | 9.1 |
| Medicare | 18.8 | 19.0 | 18.7 |
| Medicaid | 27.3 | 29.0 | 26.5 |
| None/free care | 43.9 | 40.0 | 45.7 |
| Employment, % | |||
| Full-time | 20.9 | 13.0* | 24.3 |
| Part-time | 13.3 | 12.0 | 13.9 |
| Unemployed/retired | 65.8 | 75.0 | 61.7 |
| Site, % | |||
| Chicago, IL | 30.6 | 26.0 | 32.6 |
| Grand Rapids, MI | 36.1 | 38.0 | 35.2 |
| Shreveport, LA | 33.3 | 36.0 | 32.2 |
| Years living with hypertension, Mean (SD) | 11.0 (10.0) | 13.7 (13.1)*** | 9.9 (8.5) |
| Knowledge Score, Mean (SD) | 11.0 (2.0) | 10 (2.5)*** | 11.3 (2.1) |
| Self-Efficacy Score, Mean (SD) | 37.2 (9.6) | 36.3 (9.5) | 37.6 (9.6) |
| Physical Activity Score, Mean (SD) | 3.2 (1.5) | 3.2 (1.6) | 3.2 (1.5) |
| Subjective Health Score, Mean (SD) | 2.6 (0.9) | 2.62 (1.0) | 2.6 (0.9) |
Note. Chi-square and student’s t-tests for group differences,
P<0.05,
P<0.01 and
P<0.001.
Thirteen percent of patients reported having left school prior to the ninth grade, and another 26.2% had not completed high school. Approximately one third (31.4%) of the sample were high school graduates; fewer years of schooling was significantly associated with inadequate health literacy skills, as well as older age, current unemployment, and greater number of years living with hypertension (Table 1). One third (30.3%) of patients were classified as having inadequate health literacy skills, and another 8.2% had marginal health literacy. Inadequate health literacy was also associated with older age, current unemployment/retirement status, and a greater number of years living with hypertension. Means and standard deviations for the knowledge, self-efficacy, physical activity, and subjective health variables are presented in Table 1.
Model 1 demonstrated excellent data fit, χ2(3 N=330) = 5.42, P=0.14, CFI=0.99, RMSEA=0.05 (90% CI: 0.00–0.11). There were significant, direct paths from education, race, and age to health literacy (ie, fewer years of education, African American race, and older age were independently associated with lower health literacy scores). Additional significant path included health literacy to knowledge (ie, higher health literacy scores were associated with more knowledge); self-efficacy to self-care behavior (ie, greater self-efficacy was associated with more physical activity); and self-care behavior to health status (ie, more physical activity was associated with more favorable subjective health ratings). In addition, race was directly related to self-efficacy (ie, African American race was associated with greater self-efficacy); and self-efficacy was directly related to health status (ie, greater self-efficacy was associated with more favorable subjective health ratings). All remaining paths were not significant, including paths from demographic factors to knowledge, self-efficacy, self-care behavior, or health status; health literacy to self-efficacy, self-care behavior, or health status; and knowledge to self-care behavior or health status.
Model 2 estimated a trimmed version of Model 1, retaining all significant paths and omitting all nonsignificant paths in Model 1. The trimmed model with structural parameters and tests of significance of individual paths appears in Figure 1. Model 2 demonstrated excellent data fit, χ2(16, N=330)=16.75, P=0.40, CFI=1.00, RMSEA=0.01 (90% CI: 0.00–0.05). All significant paths in Model 1 remained significant in Model 2 except for the path from race to self-efficacy (ie, African American race was no longer directly related to self-efficacy). Examination of the squared multiple correlation coefficients in the model showed that the demographic factors explained 34% of the variability in health literacy score, a percentage considered to be a moderate effect for multiple predictor models.40 Health literacy explained 5% of the variability in knowledge; knowledge explained 3% of the variability in self-efficacy; self-efficacy explained 3% of the variability in self-care behavior (physical activity); and self-efficacy and self-care behavior explained 4% of the variability in health status (subjective health). These are all small effects. A chi-square difference test was performed against Model 1, χ2(13, N=330)=11.33, ns. The difference was nonsignificant permitting the retention of the trimmed version as the more parsimonious and final model.
Figure 1.
Estimated Trimmed Model With Predicted Pathways From Literacy to Health Status
Note. Coefficients are standard path coefficients. For tests of individual paths, *P<0.05, **P<0.01 and ***P<0.001. Overall model fit, χ2(16, N=330)=16.75, P=0.40, CFI=1.00, RMSEA=0.01 (90% CI: 0.00–0.05). For tests of significance of individual paths, *P<0.05, **P<0.01 and ***P<0.001.
DISCUSSION
Conceptual frameworks propose explicit linkages between known determinants of health, with the ultimate goal of locating strategic entry points for intervention. Rooted in prior research, these frameworks require empirical validation prior to their use in developing practical strategies for responding to relevant health problems. We performed a cross-sectional path analysis on data collected from patients with hypertension at federally qualified health centers in 3 states to evaluate predicted pathways linking health literacy to health outcomes. Consistent with the Paasche-Orlow and Wolf framework5 and hypothesis 1, demographic factors (education, race, and age) were directly related to health literacy, were unrelated to all other variables, and explained one third of the variability in the health literacy score. Consistent with the framework and hypotheses 2–4, health literacy was directly related to knowledge,4 self-efficacy was directly related to self-care behavior (physical activity),41,42 and self-care behavior was directly related to health status (subjective health).
Studies in the health literacy, hypertension, and health behavior change literatures support the aforementioned findings. Demographic characteristics, specifically education, race, and age, have been related to health literacy across chronic disease contexts, including hypertension.43 Prior research has also supported an independent, direct link between health literacy and hypertension knowledge, with limited health literacy being consistently associated with poor knowledge.4,15,16 Other hypertension studies have supported an independent, direct link between self-efficacy and physical activity,24,42 as well as an association between physical activity and subjective health.24 Here, we explored the role of health literacy and knowledge, which had not been a focus of these latter studies. Although our findings are consistent with prior research, they uniquely extend what is known about the relationship between health literacy and health outcomes. Evidence in support of intervening upon a sequence of modifiable factors in health promotion programs is a significant contribution to both the health literacy and health behavior change literatures and, to our knowledge, has not been done to date.
Inconsistent with the Paasche-Orlow and Wolf framework5 and hypothesis 2 were nonsignificant paths from health literacy to self-efficacy,44 self-efficacy to health status, and knowledge to self-care behavior. Instead, we found that knowledge was the only significant predictor of self-efficacy, allowing health literacy to be indirectly related to self-efficacy through knowledge. Some studies have shown health literacy predicting self-efficacy,14 whereas others have found no association.44 We propose that health literacy may affect self-efficacy through knowledge, but more research is needed to support this. In our study, self-efficacy was an independent, direct predictor of health status. Studies in other chronic disease contexts have shown strong associations between self-efficacy and self-rated health.45–48 However, less is known about this relationship in the context of hypertension. Lastly, knowledge was unrelated to self-care behavior in our study. This finding is both consistent with behavior change frameworks49 and prior studies showing knowledge to be poorly correlated with behavior, specifically physical activity.50,51
Our findings ruled out several alternative relationships between variables. As illustrated in the Paasche-Orlow and Wolf framework, the impact of demographic factors (education, race, age) on hypertension knowledge, self-efficacy, self-care behavior, and health status was entirely explained by health literacy. This is consistent with research showing that health literacy explains demographic differences in self-care behavior and health outcomes.52,53 In our study, health literacy had no direct relationship with health status. Although this finding is consistent with the Paasche-Orlow and Wolf framework, it is inconsistent with studies in health literacy.43,54 One study in particular found a direct link between health literacy and health status that was not mediated by intermediate factors, such as disease knowledge and health behavior.54 Because these findings were based on an elderly sample, additional research is needed to rule out cognitive decline as an alternative explanation. Lastly, we found that knowledge had no direct relationship with health status, which has been both theoretically argued49 and empirically supported in other work.54
Several limitations are inherent in this study. First, the data were based on self-reported information, introducing the possibility of deliberate or unconscious misinformation.55 Furthermore, the measures of self-care behavior and health status were both single-item measures, which have been criticized for introducing bias and not being comprehensive in measurement.56,57 However, the single-item measures used in this study had been previously used and validated in other research.31,32 The health status item in particular has demonstrated strong predictive validity with self-care behaviors,33 objective indicators of health,33,58 and mortality;34,59 has been used as a dependent variable in path analytic models;54,60 and does not violate SEM assumptions for endogenous variables.38
Second, although our findings propose causal relationships between variables, the cross-sectional nature of the data precludes causal conclusions and can most appropriately speak to associations between constructs observed at a single point in time. Consequently, we have relied on theory and literature to direct our conclusions. Future prospective research is needed to investigate the longitudinal effects of these constructs on changes in health behaviors and health outcomes.
Third, the current results pertain most directly to populations similar to participants in this study. These findings should be confirmed in other populations to see if they can be generalized. Future work guided by the model proposed in Figure 1 would provide a more comprehensive conceptualization of the core constructs believed to implicate hypertension self-management.
Finally, although relations between the variables in our study were statistically significant, the magnitude of the relationships was rather modest. Future models should include measures of patient motivation and problem solving; additional self-care behaviors, and objective measures of health status, which may explain more of the variability in the sequence of intervening variables linking health literacy to health outcomes. Duration of and control of high blood pressure are important factors that are likely to impact both health behaviors and outcomes among patients with hypertension. In an effort to be consistent with the Paasche-Orlow and Wolf model, duration of disease (eg, hypertension) was not accounted for in our analyses. We also did not include blood pressure control, mainly because it is a very dynamic outcome (ie, patients can be controlled and uncontrolled by turns) – and being in control has a lot to do with activities of the clinicians (eg, providing the proper type and dosage of medication and being available to follow up with patients). We were also unable to classify patients as having prehypertension, stage 1 or stage 2 hypertension.
Despite these limitations, this study is the first to our knowledge to show an indirect pathway from health literacy to health status via widely recognized determinants of self-care (knowledge and self-efficacy) and actual self-care behavior (physical activity). Our findings are just one step in what should be an iterative process of model specification and clarification. Future studies that can both validate our findings and extend them would provide the most useful explanation of the relationship between health literacy and health outcomes and inform professional responses to the problem in many diverse contexts of health care.61 In the meantime, we suggest, based on our findings, that health literacy-sensitive interventions should aim to enhance disease-specific knowledge that, in turn, will enhance self-efficacy, so that self-efficacy will, in turn, promote the performance of self-care behaviors needed for desirable health outcomes. Future qualitative and quantitative research to determine the most influential techniques to promote knowledge, self-efficacy, and self-care behavior among patients with limited health literacy is needed.
Our findings support the role patient knowledge plays in linking health literacy to health outcomes for patients with hypertension, highlighting the potential impact of patient education efforts as a means of improving health outcomes. However, intervening to improve knowledge may prove challenging. Providers do not have the time. Patients may have other priorities and competing cultural views about hypertension. Effective mechanisms to promote patient education regarding hypertension for patients with limited health literacy will need to be developed and integrated into care.
Acknowledgements
Funding for this study was provided by a research grant awarded to Cherry Street Health Services by the Michigan Department of Community Health. Dr. Osborn performed this research under the support of a Diversity Supplement Award (NIDDK P60 DK020593-30S2).
Contributor Information
Chandra Y. Osborn, Assistant Professor of Medicine, Vanderbilt University School of Medicine, Center for Health Services Research, 1215 Twenty-First Ave South, Ste 6000, MCE - North Tower, Nashville, TN 37232-8300, Phone: (615) 936-8468, Fax: (615) 936-1269, chandra.osborn@vanderbilt.edu.
Michael K. Paasche-Orlow, Assistant Professor of Medicine, Boston University School of Medicine, Section of General Internal Medicine, 801 Massachusetts Ave, 2nd floor, Boston, MA 02118, Phone: (617) 414-5877, Fax: (617) 414-4676, michael.paascheorlow@bmc.org.
Stacy Cooper Bailey, Program Director, Health Literacy and Learning Program, Northwestern University Feinberg School of Medicine, Institute for Healthcare Studies, 750 N Lake Shore Drive, 10th floor, Chicago, IL 60611, Phone: (312) 503-5586, Fax: (312) 503-2777, stacy-bailey@northwestern.edu.
Michael S. Wolf, Associate Professor of Medicine and Learning Sciences, Northwestern University Feinberg School of Medicine, Institute for Healthcare Studies, 750 N Lake Shore Drive, 10th floor, Chicago, IL 60611, Phone: (312) 503-5592, Fax: (312) 503-2777, mswolf@northwestern.edu.
REFERENCES
- 1.Baker DW, Parker RM, Williams MV, et al. The relationship of patient reading ability to self-reported health and use of health services. Am J Public Health. 1997;87(6):1027–1030. doi: 10.2105/ajph.87.6.1027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Davis TC, Wolf MS. Health literacy: implications for family medicine. Fam Med. 2004 Sep;36(8):595–598. [PubMed] [Google Scholar]
- 3.Dewalt DA, Berkman ND, Sheridan S, et al. Literacy and health outcomes: a systematic review of the literature. J Gen Intern Med. 2004 Dec;19(12):1228–1239. doi: 10.1111/j.1525-1497.2004.40153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gazmararian JA, Williams MV, Peel J, et al. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003 Nov;51(3):267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 5.Paasche-Orlow MK, Wolf MS. The causal pathways linking health literacy to health outcomes. Am J Health Behav. 2007 Sep–Oct;31 Suppl 1:S19–S26. doi: 10.5555/ajhb.2007.31.supp.S19. [DOI] [PubMed] [Google Scholar]
- 6.von Wagner C, Steptoe A, Wolf MS, et al. Health literacy and health actions: a review and a framework from health psychology. Health Educ Behav. 2009 Aug;36(5):860–877. doi: 10.1177/1090198108322819. [DOI] [PubMed] [Google Scholar]
- 7.Beitler JJ, Chen AY, Jacobson K, et al. Health literacy and health care in an inner-city, total laryngectomy population. Am J Otolaryngol. Jan–Feb;31(1):29–31. doi: 10.1016/j.amjoto.2008.09.011. [DOI] [PubMed] [Google Scholar]
- 8.Amalraj S, Starkweather C, Nguyen C, et al. Health literacy, communication, and treatment decision-making in older cancer patients. Oncology (Williston Park) 2009 Apr 15;23(4):369–375. [PubMed] [Google Scholar]
- 9.Baker DW, Parker RM, Williams MV, et al. The health care experience of patients with low literacy. Arch Fam Med. 1996 Jun;5(6):329–334. doi: 10.1001/archfami.5.6.329. [DOI] [PubMed] [Google Scholar]
- 10.Verhoeven L, Snow C, editors. Literacy and Motivation: Reading Engagement in Individuals and Groups. Mahwah, NJ: Lawrence Erlbaum Associates Publishers; 2001. 326 pp. vii, 2001. [Google Scholar]
- 11.Kaminski RA, Good RH III, editors. Assessing Early Literacy Skills in a Problem-Solving Model: Dynamic Indicators of Basic Early Literacy Skills: Shinn, Mark R. 1998. [Google Scholar]
- 12.Torres RY, Marks R. Relationships among health literacy, knowledge about hormone therapy, self-efficacy, and decision-making among postmenopausal health. J Health Commun. 2009 Jan–Feb;14(1):43–55. doi: 10.1080/10810730802592247. [DOI] [PubMed] [Google Scholar]
- 13.Wolf MS, Davis TC, Cross JT, et al. Health literacy and patient knowledge in a Southern US HIV clinic. Int J STD AIDS. 2004 Nov;15(11):747–752. doi: 10.1258/0956462042395131. [DOI] [PubMed] [Google Scholar]
- 14.Wolf MS, Davis TC, Osborn CY, et al. Literacy, self-efficacy, and HIV medication adherence. Patient Educ Couns. 2007 Feb;65(2):253–260. doi: 10.1016/j.pec.2006.08.006. [DOI] [PubMed] [Google Scholar]
- 15.Pandit AU, Tang JW, Bailey SC, et al. Education, literacy, and health: mediating effects on hypertension knowledge and control. Patient Educ Couns. 2009 Jun;75(3):381–385. doi: 10.1016/j.pec.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 16.Williams MV, Baker DW, Parker RM, et al. Relationship of functional health literacy to patients' knowledge of their chronic disease. A study of patients with hypertension and diabetes. Arch Intern Med. 1998 Jan 26;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- 17.Gazmararian JA, Kripalani S, Miller MJ, et al. Factors associated with medication refill adherence in cardiovascular-related diseases: a focus on health literacy. J Gen Intern Med. 2006 Dec;21(21):1215–1221. doi: 10.1111/j.1525-1497.2006.00591.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Persell SD, Osborn CY, Richard R, et al. Limited health literacy is a barrier to medication reconciliation in ambulatory care. J Gen Intern Med. 2007 Nov;22(11):1523–1526. doi: 10.1007/s11606-007-0334-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kim SH. Health literacy and functional health status in Korean older adults. J Clin Nurs. 2009 Aug;18(16):2337–2343. doi: 10.1111/j.1365-2702.2008.02739.x. [DOI] [PubMed] [Google Scholar]
- 20.Chobanian AV, Bakris GL, Black HR, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003 May 21;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 21.Nelson L, Jennings GL, Esler MD, et al. Effect of changing levels of physical activity on blood-pressure and haemodynamics in essential hypertension. Lancet. 1986 Aug 30;2(8505):473–476. doi: 10.1016/s0140-6736(86)90354-5. [DOI] [PubMed] [Google Scholar]
- 22.Higashi Y, Sasaki S, Kurisu S, et al. Regular aerobic exercise augments endothelium-dependent vascular relaxation in normotensive as well as hypertensive subjects: role of endothelium-derived nitric oxide. Circulation. 1999 Sep 14;100(11):1194–1202. doi: 10.1161/01.cir.100.11.1194. [DOI] [PubMed] [Google Scholar]
- 23.Palatini P, Visentin P, Dorigatti F, et al. Regular physical activity prevents development of left ventricular hypertrophy in hypertension. Eur Heart J. 2009 Jan;30(2):225–232. doi: 10.1093/eurheartj/ehn533. [DOI] [PubMed] [Google Scholar]
- 24.Lee YS, Laffrey SC. Predictors of physical activity in older adults with borderline hypertension. Nurs Res. 2006 Mar–Apr;55(2):110–120. doi: 10.1097/00006199-200603000-00006. [DOI] [PubMed] [Google Scholar]
- 25.Knuth AG, Bielemann RM, Silva SG, et al. Public knowledge on the role of physical activity in the prevention and treatment of diabetes and hypertension: a population-based study in southern Brazil. Cad Saude Publica. 2009 Mar;25(3):513–520. doi: 10.1590/s0102-311x2009000300006. [DOI] [PubMed] [Google Scholar]
- 26.Olsen J. What characterises a useful concept of causation in epidemiology? J Epidemiol Community Health. 2003 Feb;57(2):86–88. doi: 10.1136/jech.57.2.86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Johnson TP, Owens L. Survey response rate reporting in the professional literature; Proceedings of the 2003 American Statistical Association Conference Section on Survey Research Methods; Alexandria, VAL: American Statistical Association; 2004. pp. 127–133. [Google Scholar]
- 28.Baker DW, Williams MV, Parker RM, et al. Development of a brief test to measure functional health literacy. Patient Educ Couns. 1999 Sep;38(1):33–42. doi: 10.1016/s0738-3991(98)00116-5. [DOI] [PubMed] [Google Scholar]
- 29.Parker RM, Baker DW, Williams MV, et al. The test of functional health literacy in adults: a new instrument for measuring patients' literacy skills. J Gen Intern Med. 1995 Oct;10(10):537–541. doi: 10.1007/BF02640361. [DOI] [PubMed] [Google Scholar]
- 30.Osborn CY, Weiss BD, Davis TC, et al. Measuring adult literacy in health care: performance of the newest vital sign. Am J Health Behav. 2007 Sep–Oct;31 Suppl 1:S36–S46. doi: 10.5555/ajhb.2007.31.supp.S36. [DOI] [PubMed] [Google Scholar]
- 31.Troped PJ, Saunders RP, Pate RR, et al. Correlates of recreational and transportation physical activity among adults in a New England community. Prev Med. 2003 Oct;37(4):304–310. doi: 10.1016/s0091-7435(03)00137-3. [DOI] [PubMed] [Google Scholar]
- 32.Idler EL, Russell LB, Davis D. Survival, functional limitations, and self-rated health in the NHANES I Epidemiologic Follow-up Study, 1992. First National Health and Nutrition Examination Survey. Am J Epidemiol. 2000 Nov 1;152(9):874–883. doi: 10.1093/aje/152.9.874. [DOI] [PubMed] [Google Scholar]
- 33.Haddock CK, Poston WS, Pyle SA, et al. The validity of self-rated health as a measure of health status among young military personnel: evidence from a cross-sectional survey. Health Qual Life Outcomes. 2006;4:57. doi: 10.1186/1477-7525-4-57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.DeSalvo KB, Bloser N, Reynolds K, et al. Mortality prediction with a single general self-rated health question. A meta-analysis. J Gen Intern Med. 2006 Mar;21(3):267–275. doi: 10.1111/j.1525-1497.2005.00291.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rohrer JE, Herman DC, Merry SP, et al. Validity of overall self-rated health as an outcome measure in small samples: a pilot study involving a case series. J Eval Clin Pract. 2009 Apr;15(2):366–369. doi: 10.1111/j.1365-2753.2008.01017.x. [DOI] [PubMed] [Google Scholar]
- 36.Han MA, Kim KS, Park J, et al. Association between levels of physical activity and poor self-rated health in Korean adults: The Third Korea National Health and Nutrition Examination Survey (KNHANES), 2005. Public Health. 2009 Oct;123(10):665–669. doi: 10.1016/j.puhe.2009.08.005. [DOI] [PubMed] [Google Scholar]
- 37.Ridgon E. CFI versus RMSEA: comparison of two fit indexes for structural equation modeling. Structural Equation Modeling. 1996;3:369–379. [Google Scholar]
- 38.Kline R. Principles and Practice of Structural Equation Modeling. 2nd ed. New York: Guilford; 2004. [Google Scholar]
- 39.Loehlin JC. Latent Variable Models: An Introduction to Factor, Path, and Structural Analysis. Hillsdale, NJ: Lawrence Erlbaum Associates; 1992. [Google Scholar]
- 40.Cohen J. Statistical Power Analysis for Behavioral Sciences. New York: Academic Press; 1997. (Rev. ed.) [Google Scholar]
- 41.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc Sport Sci Rev. 2000 Apr;28(2):85–88. [PubMed] [Google Scholar]
- 42.Cromwell SL, Adams MM. Exercise, self-efficacy, and exercise behavior in hypertensive older African-Americans. J Natl Black Nurses Assoc. 2006 Jul;17(1):17–21. [PubMed] [Google Scholar]
- 43.Hanchate AD, Ash AS, Gazmararian JA, et al. The Demographic Assessment for Health Literacy (DAHL): a new tool for estimating associations between health literacy and outcomes in national surveys. J Gen Intern Med. 2008 Oct;23(10):1561–1566. doi: 10.1007/s11606-008-0699-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.DeWalt DA, Boone RS, Pignone MP. Literacy and its relationship with self-efficacy, trust, and participation in medical decision making. Am J Health Behav. 2007 Sep–Oct;31 Suppl 1:S27–S35. doi: 10.5555/ajhb.2007.31.supp.S27. [DOI] [PubMed] [Google Scholar]
- 45.Sarkar U, Ali S, Whooley MA. Self-efficacy and health status in patients with coronary heart disease: findings from the heart and soul study. Psychosom Med. 2007 May;69(4):306–312. doi: 10.1097/PSY.0b013e3180514d57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Salbach NM, Mayo NE, Robichaud-Ekstrand S, et al. Balance self-efficacy and its relevance to physical function and perceived health status after stroke. Arch Phys Med Rehabil. 2006 Mar;87(3):364–370. doi: 10.1016/j.apmr.2005.11.017. [DOI] [PubMed] [Google Scholar]
- 47.Cross MJ, March LM, Lapsley HM, et al. Patient self-efficacy and health locus of control: relationships with health status and arthritis-related expenditure. Rheumatology (Oxford) 2006 Jan;45(1):92–96. doi: 10.1093/rheumatology/kei114. [DOI] [PubMed] [Google Scholar]
- 48.Riazi A, Thompson AJ, Hobart JC. Self-efficacy predicts self-reported health status in multiple sclerosis. Mult Scler. 2004 Feb;10(1):61–66. doi: 10.1191/1352458504ms986oa. [DOI] [PubMed] [Google Scholar]
- 49.Fisher WA, Fisher JD, Harman J. The Information-Motivation-Behavioral Skills Model: a general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social Psychological Foundations of Health and Illness. Malden, MA: Blackwell; 2003. pp. 82–106. [Google Scholar]
- 50.Hays LM, Clark DO. Correlates of physical activity in a sample of older adults with type 2 diabetes. Diabetes Care. 1999 May;22(5):706–712. doi: 10.2337/diacare.22.5.706. [DOI] [PubMed] [Google Scholar]
- 51.Dishman RK, Sallis JF, Orenstein DR. The determinants of physical activity and exercise. Public Health Rep. 1985 Mar–Apr;100(2):158–171. [PMC free article] [PubMed] [Google Scholar]
- 52.Osborn CY, Paasche-Orlow MK, Davis TC, et al. Health literacy: an overlooked factor in understanding HIV health disparities. Am J Prev Med. 2007 Nov;33(5):374–378. doi: 10.1016/j.amepre.2007.07.022. [DOI] [PubMed] [Google Scholar]
- 53.Wolf MS, Knight SJ, Lyons EA, et al. Literacy, race, and PSA level among low-income men newly diagnosed with prostate cancer. Urology. 2006 Jul;68(1):89–93. doi: 10.1016/j.urology.2006.01.064. [DOI] [PubMed] [Google Scholar]
- 54.Cho YI, Lee SY, Arozullah AM, et al. Effects of health literacy on health status and health service utilization amongst the elderly. Soc Sci Med. 2008 Apr;66(8):1809–1816. doi: 10.1016/j.socscimed.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 55.Prince SA, Adamo KB, Hamel ME, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Act. 2008;5:56. doi: 10.1186/1479-5868-5-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ferrari P, Friedenreich C, Matthews CE. The role of measurement error in estimating levels of physical activity. Am J Epidemiol. 2007 Oct 1;166(7):832–840. doi: 10.1093/aje/kwm148. [DOI] [PubMed] [Google Scholar]
- 57.van Doorslaer E, Jones AM. Inequalities in self-reported health: validation of a new approach to measurement. J Health Econ. 2003 Jan;22(1):61–87. doi: 10.1016/s0167-6296(02)00080-2. [DOI] [PubMed] [Google Scholar]
- 58.Ried LD, Tueth MJ, Handberg E, et al. Validating a self-report measure of global subjective well-being to predict adverse clinical outcomes. Qual Life Res. 2006 May;15(4):675–686. doi: 10.1007/s11136-005-3515-2. [DOI] [PubMed] [Google Scholar]
- 59.Thombs BD, Ziegelstein RC, Stewart DE, et al. Physical health status assessed during hospitalization for acute coronary syndrome predicts mortality 12 months later. J Psychosom Res. 2008 Dec;65(6):587–593. doi: 10.1016/j.jpsychores.2008.06.004. [DOI] [PubMed] [Google Scholar]
- 60.Smith PM, Frank JW, Mustard CA, et al. Examining the relationships between job control and health status: a path analysis approach. J Epidemiol Community Health. 2008 Jan;62(1):54. doi: 10.1136/jech.2006.057539. [DOI] [PubMed] [Google Scholar]
- 61.Jukkala A, Deupree JP, Graham S. Knowledge of limited health literacy at an academic health center. J Contin Educ Nurs. 2009 Jul;40(7):298–302. doi: 10.3928/00220124-20090623-01. quiz 303-294, 336. [DOI] [PubMed] [Google Scholar]