Abstract
Objective
To determine whether longer durations of voucher-based reinforcement therapy (VBRT) increase long-term abstinence compared to standard durations.
Methods
Cocaine-abusing or dependent methadone-maintenance patients (N=130) were randomized to receive either Standard (12-week; n=62) or Extended (36-week; n=68) VBRT. Participants provided 3 urine samples weekly during VBRT, and each cocaine-negative sample produced a voucher exchangeable for goods and services.
Results
Extended VBRT produced longer durations of self-reported continuous abstinence during study Year 1 (M = 74 vs. 46 days; F(1,128) = 5.23, P = 0.024), but not during Year 2. However, each week of abstinence during Year 1 was associated with an increase of 9.19 days of abstinence during Year 2, regardless of study condition (t(1) = 4.92, P <0.001,).
Conclusions
Longer-duration VBRT can increase abstinence during VBRT, but may not maintain it afterwards. However, longer during-treatment abstinence begets later abstinence suggesting that further research regarding this relationship is needed.
Keywords: long-term maintenance, substance abuse, cocaine abuse, contingency management, voucher-based reinforcement therapy
There is a considerable body of research documenting the detrimental impact of drug abuse on the health of the substance abuser.1 The range of effects can be broad and devastating, potentially encompassing physical, emotional, social, legal, and vocational aspects of the drug user's life in a complex and interconnected way. Contingency management (CM) approaches are among the most efficacious for initiating drug abstinence,2,3 but as with many treatments for health behavior change, abstinence outcomes often are not maintained following treatment.
CM approaches consider drug use to be a form of operant behavior; behavior that is strengthened and maintained, at least in part, by the biochemical effects of the drug and is influenced by environmental factors consistent with basic principles of behavior. In a classic review of animal and human research across a wide variety of drugs of abuse, Griffiths et al provided a clear, empirically derived conceptual model for understanding drug abuse based in the principles of behavior analysis.4,5 They demonstrated that drug-taking by laboratory animals and by humans can be maintained by the delivery of the drug itself and can be decreased or eliminated by blocking the delivery of the drug or pretreating with pharmacologic agents that block the action of the drug on the relevant neurological receptors. They further showed that drug-taking can be decreased or eliminated by increasing the response cost or by the appropriate scheduling of competing nondrug reinforcers.
This model also suggests that ultimately some reinforcement is necessary to maintain a behavior, whether that behavior is drug use or drug abstinence. That is, drug use or drug abstinence can persist over long periods of time only if there are contingent reinforcers that sustain it.6 Research has also shown that although reinforcement is necessary to maintain a response, the passage of time alone does not eliminate a learned response; the response will quickly recover strength if it is again reinforced.7,8 In other words, lapses to old behavior can occur over long periods, even after new behaviors have been learned. Drug use is easily maintained and reinstated because of the immediate and consistently delivered biochemical consequences. However, reinforcement for the competing responses that make up drug abstinence tends to be relatively delayed and less certain.
The consequences that maintain a behavior can be completely artificial, wholly natural, or fall anywhere on a continuum between these 2 extremes. CM describes a variety of strategies that have been used to alter the immediate naturally occurring environmental consequences of behavior. CM approaches to drug abuse treatment can effectively initiate drug abstinence by changing the consequences of drug use so that (a) drug abstinence and drug use are more easily detected through frequent urinalysis monitoring; (b) drug abstinence is more immediately and reliably reinforced with nondrug reinforcers; and (c) drug use results in immediate and reliable loss of that reinforcement. Some CM programs have used consequences that fall towards the natural end of the continuum (eg, the Community Reinforcement Approach), but often artificial consequences are applied. One such example is voucher-based reinforcement therapy (VBRT).9 In VBRT drug use and abstinence are detected by urinalysis conducted 2 to 3 times weekly. Each sample that verifies drug abstinence immediately results in the presentation of a voucher that can be exchanged for a wide variety of goods or services, and continuous drug abstinence is reinforced by increasing the value of the voucher with each consecutive sample that tests drug-negative (ie, $2.50 for the first negative sample, escalating by $1.50 for each consecutive sample so that subsequent vouchers are valued at $3.75, $5.25, $6.75, etc). In addition, each sample that tests positive for cocaine metabolite results in a response-cost contingency in which the voucher value is reset so that the next sample testing drug-negative receives a voucher at the original value (ie, $2.50).
VBRT has a considerable amount of empirical support for initiating drug abstinence and maintaining it for periods of about 12 weeks,10-12 but it has infrequently been used as a longer-term behavioral maintenance strategy. Higgins et al13 presented data demonstrating that longer maximum durations of cocaine abstinence achieved during treatment were associated with greater cocaine abstinence at 6, 9, and 12 months after treatment entry. These correlative data are consistent with the possibility that longer CM treatments that support longer periods of continuous abstinence during treatment might result in longer durations of abstinence after treatment.
We are aware of one study by Silverman et al 14 that examined longer durations of VBRT. Methadone maintenance patients who abused cocaine were randomly assigned to one of 3 groups: usual care only (U); U plus methadone take-home doses contingent upon providing opiate- and cocaine-free urine samples (UM); and UM plus VBRT delivered on an escalating schedule (as described above with vouchers capped at $40.00) contingent upon providing cocaine-free urine samples (UMV). After a 10-week baseline usual care period, participants in the UM and UMV groups were exposed to their respective contingencies for 52 weeks, followed by a 9-week postintervention period in which VBRT was discontinued, but UM continued. Participants in the U group received no incentives for abstinence, but had the same thrice weekly urine sampling schedule during the 71-week study. Both the UM and UMV groups increased cocaine abstinence relative to the U group, but the addition of the voucher intervention resulted in the largest and most sustained abstinence. Furthermore, the UMV group maintained abstinence during the postintervention period, when VBRT was discontinued.
Similar to the Silverman et al study,14 we investigated long-term VBRT; however, rather than comparing an extended period of VBRT to a usual care control or take-home medication group as other studies have done, we specifically examined the effect of the duration of VBRT on long-term maintenance of abstinence by directly comparing differing durations of voucher delivery. Also, we conducted the study in a community-based treatment program as opposed to a research-based clinic to increase the public health relevance of the findings. Because most states place significant restrictions on delivery of take-home medication, take-homes were not used as reinforcers. Instead, we used only VBRT delivered on the same escalating schedule as Silverman et al.14 The purposes of this study were to test the following hypotheses: (a) longer periods of VBRT would be associated with increased abstinence in both the first and second years, and (b) participants with longer durations of abstinence during study year one would continue to have longer durations of abstinence during study year 2.
Methods
Participants
Study participants were recruited from a large, urban, nonprofit, free-standing methadone maintenance treatment center that serves approximately 1000 clients with primary opiate dependence and is financed largely through state funds. In order to be eligible for the study participants had to have provided a cocaine-positive urine sample at study intake or to the clinic within the past 30-days, met DSM-IV criteria for current cocaine abuse or dependence, be receiving at least a 40 mg maintenance dose at the time of intake, and be able to fully participate in all study procedures (eg, provide scheduled urine samples, have no plans to leave the geographical area for the study duration). Clients were considered ineligible if they were on a methadone detoxification dosing schedule, had a spouse or significant other enrolled in the study protocol (to increase the likelihood of independent observations), or responded positively to the question “Have you ever had a problem with gambling?” (as potential rewards included lottery tickets).
Potential participants were referred to study staff by counselors at the methadone treatment program. We assessed 233 referred clients for eligibility and found that 58 (25%) of them were not appropriate referrals because they did not meet the basic inclusion criteria (eg, they did not have current cocaine use or were undergoing methadone detoxification). Four of the 175 potential participants declined participation, 3 were discharged from the treatment center or entered inpatient treatment before enrollment, and 37 were excluded because they did not complete the intake assessment. This resulted in 131 (74.9%) patients being urn randomized to one of 2 treatment conditions. The urn randomization procedure15 altered the allocation probability during the trial to rectify imbalances that might have occurred between the treatment conditions on 2 variables known to influence responsiveness to VBRT: cocaine and opiate intake urinalysis results.
One participant was determined to be ineligible during the first month of participation because of a kidney condition that prevented the reliable delivery of urine specimens consistent with the protocol. Thus, data from 130 participants were included in the final analyses. The study was approved and overseen by the institutional review boards for the Treatment Research Institute and the city of Philadelphia.
Intervention Procedures
Voucher program
Participants in both conditions earned vouchers for providing cocaine-negative urine samples according to a VBRT schedule similar to one with extensive empirical support that was developed by Higgins,9,16,17 and modified by Silverman14 for use over longer periods of time. Vouchers were redeemable for a wide choice of goods and services (eg, gift cards to stores and restaurants; bill or rent payment; and various prizes such as small appliances, home goods, and toiletries). Additionally participants could request specific items to further increase the likelihood that the goods and services would function as reinforcers. Under this schedule, participants provided an observed urine sample 3 times weekly (Monday, Wednesday, and Friday; procedures for weekly urine collection and urinalysis needed to implement VBRT were the same as for outcome assessments, which are described under Measures and Assessments below). For the first cocaine-negative urine sample provided, the participant received a voucher worth $2.50. For each consecutive cocaine-negative sample, voucher values escalated by $1.25 (eg, $3.75, $5, $6.25, etc) to a maximum value of $40. In addition, participants earned a $10 bonus voucher value for every 3 consecutive cocaine-negative samples provided. Participants providing a cocaine-positive sample, or failing to provide a scheduled sample, received no voucher for that day, and their voucher value was reset to $2.50. Following a reset, participants could restore their voucher value to the previously highest earned value by submitting 5 consecutive cocaine-negative samples.
Aftercare
Following VBRT, participants entered a 12-week aftercare period during which they were scheduled for urinalysis twice weekly (Monday and Thursday or Tuesday and Friday). They earned up to 24 one-dollar state lottery tickets, one for each cocaine-negative sample submitted.
Study conditions
Participants were randomized to either Standard or Extended VBRT. The Standard VBRT condition (n = 62) received the voucher schedule for 12 weeks, consistent with the schedule originally developed by Higgins.9 The maximum voucher earnings in this condition was $978.75. Participants in the Extended voucher condition (n = 68) received the voucher schedule for 36 weeks and could earn up to $3120.00 in vouchers.
Measures and Assessments
Assessment schedule
Participants completed biweekly and quarterly follow-up assessments over the course of the study. Weekly urinalysis assessments were provided for the purpose of administering contingencies during the treatment phase and are not presented here. Every other week during the first 48 weeks of the study, participants completed a short biweekly assessment (n=24). Every 3 months throughout the 2-year study, participants also completed a larger quarterly assessment battery (n=8). These assessments and their timing in relation to the intervention are depicted in Figure 1. Participants were paid $10 for each biweekly assessment, $30 for each quarterly assessment, and could earn a $25 bonus for completing 3 consecutive assessments on time. All payments were in the form of gift cards to local stores and restaurants. We used an intent-to-treat design where we attempted to contact participants at each assessment point whether or not they completed the full course of VBRT treatment or remained at the clinic.
Figure 1. Timing of Intervention and Assessments Over the 2-Year Study.
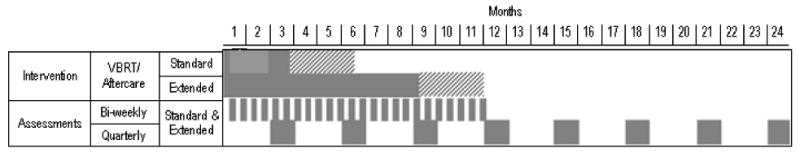
Note.
Bars indicate when an intervention or assessment occurred. The solid bars indicate the VBRT intervention and the biweekly and quarterly assessment periods. The bars with diagonal lines indicate the aftercare intervention.
Participant characteristics
The Addiction Severity Index (ASI) and a short demographics form derived from the Behavioral Risk Factor Surveillance System (BRFSS)18 were used to assess participant baseline characteristics. The ASI is a semi-structured interview that is the most widely used assessment instrument in addictions. It assesses functioning in 7 domains: psychiatric status, medical status, employment status, legal status, drug and alcohol use, and family/social functioning.19,20 It has high interrater reliability,19 good test-retest reliability,19,21 and evidence of concurrent and predictive criterion-related validity as well as construct validity across a wide range of populations.22,23 Composite scores are calculated for each domain to reflect a participant's severity index in that domain. Internal consistency in all 7 domains is adequate to excellent (Cronbach's alpha = .65 - .89).24
Urinalysis
All urine samples were observed by study staff, and temperature and adulterant tested (via temperature-integrated cups and Teco Diagnostics Drug Adulteration test strips) to ensure validity of the sample (ie, the sample is a current sample from the participant and not that of another person or adulterated with any foreign substance that might produce a false result). Samples that were determined invalid by this procedure were not further tested, but participants were allowed to provide another sample that was subjected to the same validity check. Valid samples were tested for the cocaine metabolite benzoylecgonine using ACON One Step Test Strips, which return a negative result indicating cocaine abstinence for concentrations below 300 ng/mL.
Self-reported cocaine use
Participants reported their cocaine use patterns by means of the Timeline Followback (TLFB) method25 at each biweekly and quarterly assessment. Using a calendar, participants marked each day that they used cocaine. Calendars were customized for each participant using notations with various anchoring points, such as holidays, birthdays, doctors' appointments, and paydays, to help participants recall their cocaine use. This measure has good reliability and validity for reporting periods of up to one year,26-28 and data show that subjects can specify when they used various drugs.28 At each assessment, participants completed the TLFB reporting back to their last assessment (approximately 2 weeks for the biweekly assessment and 3 months for a quarterly assessment). If a participant missed a scheduled assessment, he or she would fill out the TLFB calendar beginning on the day the last assessment was completed, resulting in a continuous and complete self-report of substance use for the full participation period.
Data Analysis
As a check on the urn randomization, demographic, drug use characteristics, and baseline status of participants in the 2 VBRT groups were compared using chi-square tests for dichotomous variables and t-tests for continuous variables. Group differences in time to the last data-collection point were examined using Kaplan-Meier survival analysis. Estimated survival functions were compared separately for Years 1 and 2.
Self-report validity
We verified the accuracy of the cocaine use reported on the TLFB by comparing participants' daily reports of use with the thrice or twice weekly urinalysis results from the first 24 weeks of the study. We calculated the following statistics for each week: (a) sensitivity (percent of those testing positive who reported use), (b) specificity (percent of those testing negative who reported no use), (c) overall percent agreement, and (d) kappa statistics. We then averaged these statistics over all 24 weeks. Kappa values can range from +1 to -1 with +1 indicating perfect agreement, 0 indicating no agreement above that expected by chance, and -1 indicating complete disagreement.
Longest duration of cocaine abstinence (LDA) outcomes
Analyses of group differences in cocaine abstinence were based on LDA during Years 1 and 2, which was calculated using the urinalysis-verified TLFB data. Year 1 data were derived from the TLFB assessments collected every other week during the first 48 weeks of the study. LDA from Year 2 was derived from TLFB assessments collected every 3 months and includes not only Year 2, but also the last 4 weeks of Year 1 (ie, weeks 49-104). Year 1 data were then adjusted using the biweekly urine sample provided at the time of the report so that participants who did not report using cocaine during the biweekly reporting period, but provided a cocaine-positive sample at the assessment were considered to have used cocaine for the entire reporting period. This procedure resulted in 69 adjustments made to Year 1 LDA (2.2%). During Year 2, urine samples were not collected frequently enough to adequately serve as a validity check, and thus, LDA calculations were based entirely on the self-report data.
For each of the measures of LDA, an analysis of variance (ANOVA) was used to determine if the 2 groups differed. A linear regression analysis was used to examine whether early abstinence (ie, Year 1 LDA) predicts later abstinence (ie, Year 2 LDA). This analysis included study condition as a covariate to control for any group effects, as well as an interaction term for group by Year 1 LDA.
Missing data
As is standard procedure in substance abuse research, all analyses were conducted with missing data points ignored and with missing data points imputed as cocaine-positive. The results of both sets of analyses were consistent with regard to significance and direction of result; therefore, we have reported the results of the missing imputed as positive analyses. Assuming that clients who fail to report for urinalysis tests have returned to cocaine use provides a more conservative estimate of abstinence duration and is consistent with reports from other VBRT studies.
Results
Participant Characteristics
Participant demographics and baseline characteristics are presented in Table 1. There were no significant differences between VBRT groups on any demographic characteristics. The only baseline characteristic in which there were group differences was ASI medical composite score (t(128) = 2.35, P = 0.02). Medical composite score was not included as a covariate in the analyses as it was not related to the outcome measures.
Table 1. Participant Baseline Characteristics.
| Standard (n=62) | Extended (n=68) | P value | |||||
|---|---|---|---|---|---|---|---|
| Mean | SD | % | Mean | SD | % | ||
| Mean Age | 40.7 | 10.6 | 43.5 | 10.4 | 0.13 | ||
| Male (%) | 61.3 | 67.7 | 0.45 | ||||
| Years of Education Completed | 11.7 | 2.2 | 11.9 | 2.4 | 0.61 | ||
| Married (%) | 19.5 | 10.3 | 0.14 | ||||
| Hispanic Ethnicity (%) | 1.6 | 5.9 | 0.19 | ||||
| Race (%) | |||||||
| White | 33.9 | 32.4 | 0.26 | ||||
| Black | 64.5 | 60.3 | |||||
| Other | 1.6 | 7.4 | |||||
| Employment Status, Past 30 Days (%) | |||||||
| Full-time (>20 days) | 11.5 | 10.5 | 0.98 | ||||
| Part-time (1-20 days) | 18.0 | 17.9 | |||||
| Days of Use, Past 30 Days | |||||||
| Cocaine | 18.4 | 10.1 | 17.3 | 9.1 | 0.49 | ||
| Alcohol | 2.1 | 5.1 | 4.3 | 8.8 | 0.09 | ||
| Heroin | 2.5 | 6.1 | 3.0 | 6.5 | 0.65 | ||
| Years of Use, Lifetime | |||||||
| Cocaine | 10.1 | 7.9 | 10.6 | 7.9 | 0.72 | ||
| Alcohol | 6.1 | 8.7 | 8.7 | 11.7 | 0.15 | ||
| Heroin | 11.6 | 9.5 | 13.9 | 10.9 | 0.19 | ||
| ASI composite scores | |||||||
| Medical | 0.29 | 0.36 | 0.44 | 0.37 | 0.02a | ||
| Employment | 0.82 | 0.21 | 0.82 | 0.24 | 0.94 | ||
| Alcohol | 0.03 | 0.09 | 0.07 | 0.14 | 0.12 | ||
| Drug | 0.37 | 0.37 | 0.37 | 0.08 | 0.72 | ||
| Legal | 0.18 | 0.18 | 0.15 | 0.22 | 0.35 | ||
| Family | 0.14 | 0.14 | 0.20 | 0.25 | 0.15 | ||
| Psychological | 0.25 | 0.25 | 0.25 | 0.24 | 0.88 | ||
Note.
Statistically significant difference between study groups
Follow-up Assessment Retention
There were no significant differences between the study conditions in follow-up retention. Retention to follow-up in Year 1 was 92.31%, 84.62%, 73.08%, and 58.46% at each quarter, respectively; and during Year 2, 70.77%, 66.15%, 65.38%, and 58.46% participants were retained at each quarter. These rates compare favorably with those of other studies in conducted community settings.29 Because participants completed the TLFB reporting back to their last assessment, we had self-reported drug use data up to the last follow-up assessment that the participant attended. As such, reporting follow-up rates at each assessment point is a conservative estimate of the data collected.
Self-report Validity
Self-reported cocaine use as measured by the TLFB method was validated against the thrice or twice weekly urinalysis results from the first 6 months of the study. Urinalysis data was matched to the self-report data using a method described by Ehrman and Robbins26 in which a urine-related report (URR) is calculated. The first step in this procedure is to determine the urine detection time for the substance. Previous studies using this method for cocaine use26,28 used a 4-day detection window based on evidence that cocaine metabolites (benzoylecgonine) can be detected in urine up to 4 days after use.30 However, we chose to use a 7-day urine detection time, because participants in this study were generally chronic cocaine users (Table 1), and studies involving high-dose chronic cocaine users have shown that cocaine metabolites are detectable in urine up to 7 days after the last reported use.31,32
We then calculated URRs. If a participant reported using cocaine during the detection time (ie, the urine sample collection day and 6 days prior), then the URR was considered positive. If they did not report any use, the URR was negative. We compared the URRs to their associated urinalysis result for each study week during the first 24 weeks of the study. The mean sensitivity, specificity, agreement rates, and kappa statistics are presented in Table 2.
Table 2. Validity of Self-reported Cocaine Use as Compared to Urinalysis Results.
| Mean | SD | Range | |
|---|---|---|---|
| Sensitivity (%) | 85.2 | 6.3 | 74.4 -100.0 |
| Specificity (%) | 92.4 | 4.7 | 79.7 - 97.8 |
| Agreement Rate (%) | 89.5 | 4.3 | 78.7 - 97.7 |
| Kappa | 0.78 | 0.10 | 0.46 - 0.95 |
Longest Duration of Abstinence
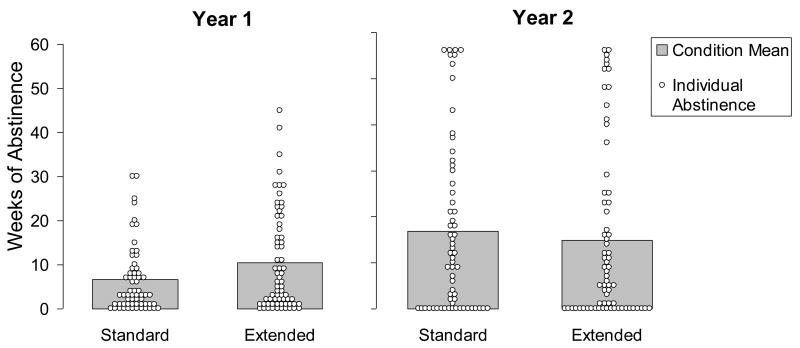
Individual and condition averages of the LDA for cocaine during years 1 and 2 are presented in Figure 2. In Year 1, participants in the Standard condition reported an average LDA of 6.61 weeks (46.26 days, SD = 53.03). Participants in the Extended condition reported an average of 10.51 weeks (73.60 days, SD = 79.31), a statistically significant difference (F(1,128) = 5.23, P = 0.024, ES = 0.41). In Year 2, participants in the Standard condition averaged 16.91 weeks of continuous abstinence (118.34 days, SD = 131.06), whereas participants in the Extended condition averaged 14.83 weeks (103.78 days, SD = 130.53), a nonsignificant difference (F(1,128) = 0.40, P = 0.53, ES = 0.11).
Figure 2. Longest Duration of Abstinence by Study Year and Condition.
Note.
Open circles show individual data; each one indicates the maximum duration of abstinence achieved by a single study participant.
The results of a linear regression analysis, shown in Table 3, indicated that weeks of continuous abstinence in Year 1 was a significant predictor of days of continuous abstinence in Year 2 (t(1) = 4.92, P <0.001, ES = 0.70). Each week of continuous abstinence in Year 1 was associated with an increase of 9.19 (SE = 1.87) days of continuous abstinence in Year 2. There were no significant effects for any other factor (ie, condition or condition by Year 1 abstinence interaction).
Table 3. Linear Regression of Year 2 Longest Duration of Abstinence.
| β | SE | p-value | |
|---|---|---|---|
| Year 1 LDA (weeks) | 9.19 | 1.87 | <0.001 |
| Condition (Extended v Standard) | -21.21 | 26.21 | 0.42 |
| Year 1 LDA * Condition | -0.40 | 0.32 | 0.21 |
Discussion
This study is the first to examine the effect of long-term delivery of VBRT for cocaine abstinence on the long-term maintenance of abstinence and to directly compare different durations of VBRT. Results suggest that increasing the length of VBRT for individuals in methadone maintenance treatment does lead to increased abstinence during the intervention. Participants who received VBRT for 36 weeks had approximately one more month (27 days) of cocaine abstinence compared to participants who received only the standard 12-week intervention. Unfortunately, these results were not maintained beyond the Extended VBRT intervention. During study Year 2, the duration of abstinence for participants in the Extended condition was not significantly better than that for participants in the Standard condition. Given previous research showing that initial abstinence begets later abstinence,13 these findings may appear inconsistent. If VBRT increases duration of abstinence in Year 1, and longer durations of abstinence in Year 1 predict longer durations of abstinence in Year 2, why did the Extended VBRT condition not lead to longer durations of abstinence in Year 2?
One possible explanation is that a third variable contributes to not only the increased duration of abstinence during VBRT in Year 1 but also to the maintenance of abstinence after VBRT during Year 2. For example, a similar VBRT intervention in the Silverman et al 14 study produced longer durations of abstinence for a greater proportion of participants relative to our study, and abstinence was maintained during a 9-week maintenance period after VBRT ended. However, in the Silverman et al study, participants received contingent methadone take-home doses during VBRT and afterwards; thus a third variable was operating. Providing contingent take-home doses to methadone patients has been shown to reduce drug use in its own right.33, 34 Although large differences between the 2 studies make it difficult to make direct comparisons between them, it seems possible that the addition of methadone take-homes in the Silverman et al study may have added to the effect of the VBRT intervention and helped to maintain abstinence after VBRT ended.
Consistent with previous correlational research showing that initial abstinence begets later abstinence in both VBRT and traditional care,13 results from this study show that independent of voucher duration, participants who were able to achieve longer durations of abstinence during the first study year were more likely to remain abstinent during the second study year. For every week of increased abstinence in Year 1, there was a one-week increase in abstinence during Year 2. Additional variables that could potentially contribute to the effectiveness of VBRT in Year 1 and maintenance of abstinence in Year 2 may have been less obvious than the additional clinic-delivered reinforcement in the Silverman et al study. For example, some of the individuals who achieved longer periods of abstinence during VBRT and maintained abstinence longer in years 1 and 2 may have had additional drug-use consequences operating outside of the clinic, such as being closely monitored by legal authorities (eg, parole officer, drug court), an employer, or by family members that provided effective social contingencies. Other research suggests that increased activity in nondrug-related activities is associated with better abstinence outcomes following treatment,35,36 and it is possible that such activities or conditions associated with them (eg, social interaction) function to reinforce behaviors that effectively compete with drug use.
A large number of participants in both conditions were unable to initiate abstinence from cocaine (see Figure 2). Over the first year of the study, 19% of Standard participants and 15% of Extended participants were unable to achieve even one week of abstinence, and 55% and 46%, respectively, were unable to remain abstinent for 4 weeks. Similar results were found in the second study year, where 40% of Standard participants and 41% of Extended participants had fewer than 4 weeks of abstinence. Because of the well-established efficacy of VBRT in increasing abstinence,9-12,14 we elected to omit a usual care control group, and thus, we were unable to compare these rates to a no-treatment group. Despite this limitation, these results suggest a poor response to VBRT. In recent years there have been numerous studies looking at various baseline characteristics that predict response to VBRT and other CM interventions. One of the most consistent findings from these studies is that participants who provide a cocaine-positive urine sample at study intake or have increased cocaine use during a baseline phase are less likely to respond to CM interventions.37,38 In the present study, more than 3 quarters of participants (78%) provided a cocaine-positive urine sample at study intake. Extrapolating from previous research, less than one quarter of participants were likely to respond to the intervention. The reason for this may be the significant delay between the last time using cocaine and the first negative specimen that many chronic cocaine users experience.31,32 This produces a long delay between abstaining from cocaine use and contact with the reinforcer. Immediacy in reinforcer delivery has been shown to be directly related to the effectiveness of the reinforcer in a wide variety of studies, including studies of VBRT.12
This study relied on self-report measures to determine the longest duration of abstinence across 2 years. Results from analyses comparing the TLFB data to urinalysis results collected in the first 6 months of the study suggest that the TLFB was a valid measure of drug use for this time period. Based on criteria provided by Landis and Koch,39 the average kappa across study weeks (Table 2) suggests substantial agreement between urinalysis and self-reported cocaine use. Additionally, all self-report data from the first year of the study were verified with biweekly urinalysis results. If a participant reported no use, but provided a positive urine sample, the data for the full 2-week reporting period were considered positive. This procedure lends additional validity to the self-report data for study Year 1.
Unfortunately, one limitation of the study is that we were not able to verify reports of cocaine use during the second study year. Urine results were collected only every 3 months during Year 2 and so were not frequent enough to verify the self-report data. The strong validity data provided during the first study year somewhat mitigate this problem. Although it is possible that participants were biased in the reporting of cocaine abstinence during Year 2, there is no clear reason to assume that the validity of their reports would change compared to the first year. Also, we attempted to minimize this bias at the time of data collection by training study staff to compare self-reports with urinalysis results during each follow-up appointment. For example, if a participant reported no cocaine use in the past 3 months, but provided a cocaine-positive urine sample, staff would probe the participant to reconsider his or her responses on the TLFB measure. Nonetheless, these procedures do not rule out the possibility of overreporting cocaine abstinence during the second study year.
Another limitation is that the study suffered from a higher than desirable loss-to-follow-up. Although retention is good in methadone maintenance treatment, it is still common for patients to leave treatment or transfer to another clinic, as was the case during the course of this 2-year study. Although we made extensive efforts to follow up with all participants, we were unable to maintain contact with several, and some of the participants we contacted refused or failed to attend the follow-up appointments. In order to improve our follow-up rates, we increased our payment for the final 3 quarterly assessment batteries from $30 to $50, as research has shown that higher payments can increase follow-up rates without increasing drug use.40 This appeared to slightly increase our follow-up compliance; however, this change was not made soon enough to effectively alter the overall follow-up rates. Fortunately, there were no differences in retention between the study groups. Also the rates compare favorably to those of other community-based studies.29
The results of this study provide some insight into VBRT and into the maintenance of cocaine abstinence. First, it suggests that extending the type of reinforcement schedule used in this study for as long as 9 months is not likely to be sufficient to produce longer durations of abstinence after treatment, at least not in similar community-based methadone maintenance programs. However, we cannot rule out the possibility that a different reinforcement schedule, or longer durations of treatment, may have resulted in a greater proportion of participants responding to VBRT. If there were a larger proportion of participants responding to VBRT, it is possible that differences in long-term maintenance would have emerged between the 2 conditions. Additional studies exploring such parameters are needed.
Second, because longer durations of abstinence during the first study year predicted longer durations of abstinence in the second year independent of duration of VBRT, this study suggests that outside variables may be contributing to positive responses to VBRT and to longer-term maintenance of cocaine abstinence. Research that examines a patient's response to treatment and to maintenance of abstinence in the context of a wider variety of variables within and outside of the treatment program may help us gain a better understanding of the types of naturally occurring contingencies that operate during treatment and in recovery.
Acknowledgments
This research was supported by a grant from the National Institute on Drug Abuse (R01DA017444). None of the authors represent any interests that could be interpreted as influential in this research. We would also like to acknowledge the research staff members who worked on this study: Julie Wosak, Tanya Faranda-Diedrich, Alicia Padovano, Rachel Corbin, Robert Gardner, Brian Versek, Laurie Jacobs, Elena Bresani, Jessica Gustafson, Tyler Case, Julianne Hancock, and Meridith Carter. Finally, we would like to express our appreciation to Larry Norton, Laverne Fish, Joanne Claypool, Joanne Wolf, and the other staff and the patients of Parkside Recovery who participated in this study.
Contributor Information
Carolyn M. Carpenedo, Email: ccarpenedo@tresearch.org, Project Coordinator, Treatment Research Institute, 600 Public Ledger Building, 150 South Independence Mall West, Philadelphia, PA 19106, (215) 399-0980, (215) 399-0987 (fax).
Kimberly C. Kirby, Email: kkirby@tresearch.org, Principal Investigator, Treatment Research Institute, 600 Public Ledger Building, 150 South Independence Mall West, Philadelphia, PA 19106, (215) 399-0980, (215) 399-0987 (fax).
Karen L. Dugosh, Email: kdugosh@tresearch.org, Quantitative Psychologist, Treatment Research Institute, 600 Public Ledger Building, 150 South Independence Mall West, Philadelphia, PA 19106, (215) 399-0980, (215) 399-0987 (fax).
Beth J. Rosenwasser, Email: brosenwasser@tresearch.org, Behavioral Interventions Section Coordinator, Treatment Research Institute, 600 Public Ledger Building, 150 South Independence Mall West, Philadelphia, PA 19106, (215) 399-0980, (215) 399-0987 (fax).
Donald L. Thompson, Email: DThompson@nhsonline.org, Senior Director, Practice Development Group, NHS Human Services Eastern Region, 906 Bethlehem Pike, Erdenheim, PA 19038, (215) 836-3186, (215) 233-9487 (fax).
References
- 1.Chen CY, Lin KM. Health consequences of illegal drug use. Curr Opin Psychiatry. 2009;22(3):287–292. doi: 10.1097/yco.0b013e32832a2349. [DOI] [PubMed] [Google Scholar]
- 2.Chambless DL, Baker MJ, Baucom DH, et al. Update on empirically validated therapies II. Clin Psychol. 1998;51(1):3–16. [Google Scholar]
- 3.Chambless DL, Ollendick TH. Empirically supported psychological interventions: controversies and evidence. Annu Rev Psychol. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- 4.Griffiths RR, Bigelow GE, Henningfield JE. Similarities in animal and human drug taking behavior. In: Mello NK, editor. Advances in Substance Abuse: Behavioral and Biological Research. Greenwich, CT: JAI Press; 1980. [Google Scholar]
- 5.Stitzer M. Classic texts revisited. Re: Similarities in Animal and Human Drug-Taking Behavior by Roland R. Griffiths, George E. Bigelow, Jack E. Henningfield, in: Advances in Substance Abuse, Volume 1, JAI Press Inc., 1980,ppabcxyzpp190. Addiction. 2005;100(8):1196–1197. doi: 10.1111/j.1360-0443.2005.01237.x. [DOI] [PubMed] [Google Scholar]
- 6.Kirby KC, Bickel WK. Toward an explicit analysis of generalization: a stimulus control interpretation. Behav Anal. 1988;11(2):115–129. doi: 10.1007/BF03392465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouton ME. A learning theory perspective on lapse, relapse, and the maintenance of behavior change. Health Psychol. 2000;19(1 Suppl):57–63. doi: 10.1037/0278-6133.19.suppl1.57. [DOI] [PubMed] [Google Scholar]
- 8.Skinner BF. Are theories of learning necessary? Psychol Rev. 1950;57(4):193–216. doi: 10.1037/h0054367. [DOI] [PubMed] [Google Scholar]
- 9.Higgins ST, Budney AJ, Bickel WK, et al. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Arch Gen Psychiatry. 1994;51(7):568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- 10.Higgins ST, Alessi SM, Dantona RL. Voucher-based incentives. A substance abuse treatment innovation. Addict Behav. 2002;27(6):887–910. doi: 10.1016/s0306-4603(02)00297-6. [DOI] [PubMed] [Google Scholar]
- 11.Higgins ST, Heil SH, Lussier JP. Clinical implications of reinforcement as a determinant of substance use disorders. Annu Rev Psychol. 2004;55:431–461. doi: 10.1146/annurev.psych.55.090902.142033. [DOI] [PubMed] [Google Scholar]
- 12.Lussier JP, Heil SH, Mongeon JA, et al. A meta-analysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101(2):192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- 13.Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer term cocaine abstinence. Exp Clin Psychopharmacol. 2000;8(3):377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- 14.Silverman K, Robles E, Mudric T, et al. A randomized trial of long-term reinforcement of cocaine abstinence in methadone-maintained patients who inject drugs. J Consult Clin Psychol. 2004;72(5):839–854. doi: 10.1037/0022-006X.72.5.839. [DOI] [PubMed] [Google Scholar]
- 15.Stout RL, Wirtz PW, Carbonari JP, et al. Ensuring balanced distribution of prognostic factors in treatment outcome research. J Stud Alcohol. 1994 12:S70–S75. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- 16.Silverman K, Wong CJ, Umbricht-Schneiter A, et al. Broad beneficial effects of cocaine abstinence reinforcement among methadone patients. J Consult Clin Psychol. 1998;66(5):811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]
- 17.Higgins ST, Wong CJ, Badger GJ, et al. Contingent reinforcement increases cocaine abstinence during outpatient treatment and 1 year of follow-up. J Consult Clin Psychol. 2000;68(1):64–72. doi: 10.1037//0022-006x.68.1.64. [DOI] [PubMed] [Google Scholar]
- 18.Nelson DE, Holtzman D, Bolen J, et al. Reliability and validity of measures from the Behavioral Risk Factor Surveillance System (BRFSS) Soz Praventivmed. 2001;46(Suppl 1):S3–S42. [PubMed] [Google Scholar]
- 19.McLellan AT, Luborsky L, Cacciola J, et al. New data from the Addiction Severity Index. Reliability and validity in three centers. J Nerv Ment Dis. 1985;173(7):412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- 20.McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 21.Drake RE, McHugo GJ, Biesanz JC. The test-retest reliability of standardized instruments among homeless persons with substance use disorders. J Stud Alcohol. 1995;56(2):161–167. doi: 10.15288/jsa.1995.56.161. [DOI] [PubMed] [Google Scholar]
- 22.Hendriks VM, Kaplan CD, van Limbeek J, et al. The Addiction Severity Index: Reliability and validity in a Dutch addict population. J Subst Abuse Treat. 1989;6(2):133–141. doi: 10.1016/0740-5472(89)90041-x. [DOI] [PubMed] [Google Scholar]
- 23.Hodgins DC, el-Guebaly N. More data on the Addiction Severity Index. Reliability and validity with the mentally ill substance abuser. J Nerv Ment Dis. 1992;180(3):197–201. doi: 10.1097/00005053-199203000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Leonhard C, Mulvey K, Gastfriend DR, et al. The Addiction Severity Index: a field study of internal consistency and validity. J Subst Abuse Treat. 2000;18(2):129–135. doi: 10.1016/s0740-5472(99)00025-2. [DOI] [PubMed] [Google Scholar]
- 25.Sobell LC, Sobell MB. Timeline follow-back: a technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen JP, editors. Measuring Alcohol Consumption: Psychosocial and Biochemical Methods. Totowa, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- 26.Ehrman RN, Robbins SJ. Reliability and validity of 6-month timeline reports of cocaine and heroin use in a methadone population. J Consult Clin Psychol. 1994;62(4):843–850. doi: 10.1037//0022-006x.62.4.843. [DOI] [PubMed] [Google Scholar]
- 27.Hersh D, Mulgrew CL, Van Kirk J, et al. The validity of self-reported cocaine use in two groups of cocaine abusers. J Consult Clin Psychol. 1999;67(1):37–42. doi: 10.1037//0022-006x.67.1.37. [DOI] [PubMed] [Google Scholar]
- 28.Fals-Stewart W, O'Farrell TJ, Freitas TT, et al. The timeline followback reports of psychoactive substance use by drug-abusing patients: psychometric properties. J Consult Clin Psychol. 2000;68(1):134–144. doi: 10.1037//0022-006x.68.1.134. [DOI] [PubMed] [Google Scholar]
- 29.Peirce JM, Petry NM, Stitzer ML, et al. Effects of lower-cost incentives on stimulant abstinence in methadone maintenance treatment: A National Drug Abuse Treatment Clinical Trials Network study. Arch Gen Psychiatry. 2006;63(2):201–208. doi: 10.1001/archpsyc.63.2.201. [DOI] [PubMed] [Google Scholar]
- 30.Hawks RL, Chiang CN. Examples of specific drug assays. NIDA Res Monogr. 1986;73:84–112. [PubMed] [Google Scholar]
- 31.Burke WM, Ravi NV, Dhopesh V, et al. Prolonged presence of metabolite in urine after compulsive cocaine use. J Clin Psychiatry. 1990;51(4):145–148. [PubMed] [Google Scholar]
- 32.Preston KL, Epstein DH, Cone EJ, et al. Urinary elimination of cocaine metabolites in chronic cocaine users during cessation. J Anal Toxicol. 2002;26(7):393–400. doi: 10.1093/jat/26.7.393. [DOI] [PubMed] [Google Scholar]
- 33.Stitzer ML, Iguchi MY, Felch LJ. Contingent take-home incentive: effects on drug use of methadone maintenance patients. J Consult Clin Psychol. 1992;60(6):927–934. doi: 10.1037//0022-006x.60.6.927. [DOI] [PubMed] [Google Scholar]
- 34.Chutuape MA, Silverman K, Stitzer M. Use of methadone take-home contingencies with persistent opiate and cocaine abusers. J Subst Abuse Treat. 1999;16(1):23–30. doi: 10.1016/s0740-5472(97)00318-8. [DOI] [PubMed] [Google Scholar]
- 35.Farabee D, Rawson R, McCann M. Adoption of drug avoidance activities among patients in contingency management and cognitive-behavioral treatments. J Subst Abuse Treat. 2002;23(4):343–350. doi: 10.1016/s0740-5472(02)00297-0. [DOI] [PubMed] [Google Scholar]
- 36.Rogers RE, Higgins ST, Silverman K, et al. Abstinence-contingent reinforcement and engagement in non-drug-related activities among illicit drug abusers. Psychol Addict Behav. 2008;22(4):544–550. doi: 10.1037/0893-164X.22.4.544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Stitzer ML, Peirce J, Petry NM, et al. Abstinence-based incentives in methadone maintenance: interaction with intake stimulant test results. Exp Clin Psychopharmacol. 2007;15(4):344–350. doi: 10.1037/1064-1297.15.4.344. [DOI] [PubMed] [Google Scholar]
- 38.Sofuoglu M, Gonzalez G, Poling J, et al. Prediction of treatment outcome by baseline urine cocaine results and self-reported cocaine use for cocaine and opioid dependence. Am J Drug Alcohol Abuse. 2003;29(4):713–727. doi: 10.1081/ada-120026256. [DOI] [PubMed] [Google Scholar]
- 39.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. [PubMed] [Google Scholar]
- 40.Festinger DS, Marlowe DB, Dugosh KL, et al. Higher magnitude cash payments improve research follow-up rates without increasing drug use or perceived coercion. Drug Alcohol Depend. 2008;96(1-2):128–135. doi: 10.1016/j.drugalcdep.2008.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]