Abstract
This paper reports on the development and validation of a set of icons designed to communicate fall risk status and tailored interventions to prevent patient falls in hospitals. The icons will populate a fall prevention toolkit to provide actionable alerts to nurses, nursing assistants, and other interdisciplinary health care team members and educational materials for patients and families in acute hospital settings.
Keywords: Fall prevention, communication, tailored interventions
1. Introduction
Patient falls and fall-related injuries are serious problems in hospitals globally. In the United States of America (USA), patient falls and fall-related injuries are employed as standard, publicly reported metrics of the quality of nursing care. Currently, there is insufficient evidence to link a specific fall prevention protocol with decreased falls in hospitalized patients. Fall TIPS (Tailoring Interventions for Patient Safety), a research study funded by The Robert Wood Johnson Foundation, (1) aims to establish links between nursing fall risk assessment, communication of risk status, and tailored interventions to prevent falls.
Phase-1 of the Fall TIPS study was a qualitative inquiry of interdisciplinary team members (nurses, physicians, physical and occupational therapists, and pharmacists) and nursing assistants to learn about current facilitators, barriers, and methods of communicating fall risk and intervention plans. Data from eight focus groups, four with professional staff and four with nursing assistants revealed several challenges. Nursing assistants had large variations in literacy levels. Common use of a “High Risk for Falls” sign at the bedside was viewed as too generic and too prevalent to be actionable. Participants were unanimous and vocal in their opinions that alerts related to patient-specific fall risk status and tailored interventions to prevent falls were needed at the bedside. Nurses participating in this project routinely assessed their patients for fall risk using the Morse Fall Scale (MFS), a standardized fall risk assessment instrument. (2) Several issues related to communication of fall risk status and associated tailored interventions to prevent falls were identified. 1) Practice was variable. 2) Fall risk communication was reliant on face to face synchronous communication. 3) Fall risk assessments were buried in the medical record or inconsistently available to the care team, patients or family. 4) Some existing fall prevention plans included a multi-page computer generated algorithm with a series of generic interventions (and described as a “dead document”). 5) In some instances the plan was nonexistent. In phase-2, information gleaned from the focus groups informed the development of a fall prevention toolkit (FPTK). The goal of the FPTK is to promote communication of current and accurate fall risk status and associated tailored interventions that are immediately accessible and actionable by the care team, patients and family members.
2. Objectives
The FPTK was designed to: 1) decrease the barriers and enhance facilitators to prevent falls identified in phase-1, 2) build upon existing workflow (routine fall risk assessment and the practice of placing signs above patients’ beds to indicate fall risk status), and 3) include a mechanism to tailor real time sign displays based on the most recent fall risk assessment. The research team identified the use of icons as a means to simplify and standardize communication across stakeholders and expanded the team to include an illustrator (JSD). (3) In the following phases of the Fall TIPS study, a set of icons to translate and communicate fall risk status and tailored interventions to prevent falls were developed, validated, and refined.
3. Materials and Methods
Procedures and Sample
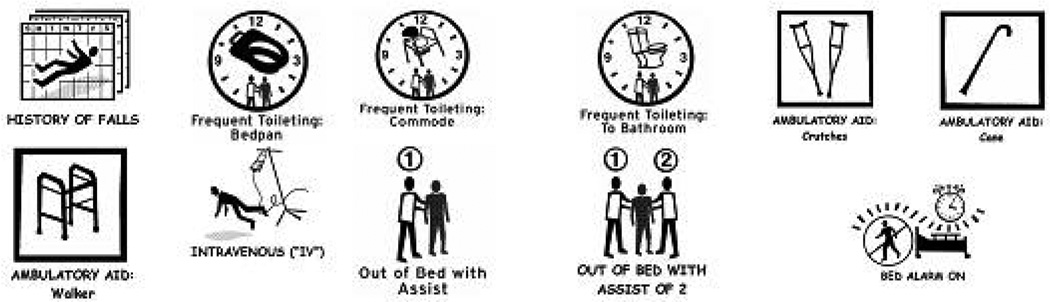
Basic content analysis methods (4) were used to interpret descriptive data obtained from Phase-1 focus group interviews. Interventions considered effective and feasible by care team members were grouped under the six areas of risk included on the MFS: 1) history of falling, 2) presence of secondary diagnosis, 3) use of ambulatory aid, 4) presence of intravenous therapy/heparin lock, 5) weak or impaired gait, and 6) overestimates/forgets limitations. The research team and illustrator used an iterative process to develop a series of icons (copy written) to represent each area of risk and associated fall prevention interventions. The use of icons, pictorial representations or images, has been found to assist clinicians, researchers and patients with condensing and integrating data (5;6) and improving comprehension, recall and performance with task completion. (7;8) Research team members individually evaluated the initial set of icons and collectively provided feedback on each icon. Revisions continued until the research team agreed that the icons were an adequate representation of the fall risk and intervention concepts. A total of 17 icons were developed to represent areas of fall risk and intervention (assist with frequent toileting, use wheelchair, ambulatory aid [walker, cane, crutches], assist of 1 or 2, bed alarm on/patient should not walk alone) concepts.
Approval was obtained for end point users to participate as content judges for icon validation testing. Clinical leadership identified potential participants who were then contacted via email or personal invitation and invited to take part in validation testing. A total of 32 professionals and 22 assistants from four hospitals in the greater Boston, MA area participated. Professionals were mostly nurses (78%), female (100%) and white (88%) with a median age of 42 years and a median of 9 years experience at their respective hospitals. Nursing assistants were mostly female (82%), Black or African American (50%), with a median age of 44 years, with 5–18 years (median=12) of formal schooling and a median of 7 years experience in their respective hospitals.
Following an established method (9) of asking content judges to rate items for computation of a content validity index (CVI) and the criterion of credibility (10) to learn if the icons were acceptable and how they could be improved, we prepared icon validity and ranking forms to use during four focus groups of professionals and four with nursing assistant potential end-point users of the FPTK. After consent was obtained, participants were given the CVI form for rating each icon using a 6-point scale to rate the degree to which each icon accurately represented the corresponding fall risk or intervention concept (1 = strongly agree the icon represented the concept) to (6 = strongly disagree that the icon represented the concept) and to write comments. Participants next independently rank ordered three clusters (four each) of icons representing the same concept using a 4-point scale in which “1” identified the icon that best represented the concept and “4” identified the ion that most poorly represented the concept. Participants wrote individual comments and then discussed comments with the group to improve the icons for giving people a quick picture of a patient’s fall risk and actions to prevent patient falls.
Analytic Methods
Responses for the 6-point CVI and 4-point ranking were entered into the Statistical Package for Social Sciences Software (SPSS), version 10.0 and mean scores were computed. Results were calculated separately for professionals and assistants. A word-processing package was used to record comments. All quantitative data and comments from both groups were displayed on a spreadsheet beside each icon to inform icon selection decisions for the FPTK.
4. Results
CVI mean score ratings for the icons ranged from a low (strongly agree that the icon represented the concept) of 1.21 (professionals) and 1.18 (nursing assistants) for the icon to represent the concept, “out of bed with assist of 1” to a high (slightly agree) of 3.15 (professionals) and 3.0 (nursing assistants) for one of the icons designed to represent “history of falling (see figure 1).”
Figure 1.
Icons with highest/lowest CVI scores
Professionals and assistants both ranked an icon with a falling figure displayed on a calendar as their first choice to depict “history of falling.” The retained icons for “assist with frequent toileting” and “bed alarm on/patient should not walk alone” were ranked first by assistants and second by professionals. Participants wrote many comments that both supported the quantitative data and were extremely useful for further icon refinement; e.g., professionals’ comments about the history of falling icon in figure 1 were: “I don’t think clock helps- I would think it means patient falls at a specific time, Sundowner; Not helpful for semi-private rooms, One clock in the room makes me think all patients in room are fall prevention; To me it means only certain times; Probably cause is letting me know that I have to keep an eye on my patients by the hour, This one is ok.” Assistants comments were: “Reinforces time; Make slightly larger; This could mean patient more likely to fall at a particular time of day and not history falls; This seems good, but only over period of a day, not really ‘history’; Makes me think about time and falls but would wonder if it was specific to this hospitalization; Clock confuses me; Confused: almost looks like the patients falls are scheduled.” A request was made to include icons that provided information about the type of toileting assistance needed (e.g., bedpan, commode or bathroom).
The research team selected the icon with the best CVI and ranking by both professional and nursing assistant groups. Where the results were conflicting, icon selection preference was given to the assistant group because of their lower literacy level. From the review/analysis of comments for each icon, a list of enhancements was generated for the illustrator to refine the icons. As suggested, three icons with specific mode of toileting were developed and the icon for use of ambulatory aid was divided into three discrete icons.
The team agreed to display simple text with each icon to improve recognition/interpretation of the fall risk and assessment concepts as per work in ergonomics and human factors. (11) Figure 2 shows the 11 icons that will populate the FPTK.
Figure 2.
FPTK Icons
5. Discussion and Conclusions
Icons are frequently used in healthcare, but limited information exists that describes methods for initial development and validation testing. (12) The few published papers on this topic (12;13) employed different approaches, but all describe a sequential process with domain experts, followed by end-users and concluding with graphical experts. Our method involved first obtaining abundant information about barriers to and facilitators of communicating fall risk and then development and communication of specific intervention plans from diverse end users. Ongoing collaboration between the research team and illustrator from the very beginning of the icon development phase to the final refinement was vital. We remained engaged with end users who quantitatively validated and ranked icons using established rating methods and provided suggestions for improvement. This iterative approach allowed us to identify and build upon the set of icons that were rated and ranked most positively by end users. We identified icons that were understandable to both professionals and nursing assistants. There were minor differences between these two groups in how icons were rated and ranked, but no icons ranked less than favorably by either group were included in the final set developed for the FPTK. End user comments were used to improve icons with relatively high rankings but variable CVI ratings across the two groups. Complex concepts (e.g., “assist with frequent toileting”) required multiple iterations and refinement to include specific toileting mode, while uncomplicated concepts (e.g., “ambulatory aid: walker”) received high CVI scores by initial validation testing with end users. The final set of icons incorporated end user feedback and facilitates immediate recognition/interpretation.
Patient falls in hospitals are a common and often preventable adverse event. Nurses routinely conduct fall risk assessment on all patients, but communication of fall risk status and tailored interventions to prevent falls is variable at best and sometimes even non-existent. Alerts related to patient-specific fall risk status and tailored interventions to prevent falls are needed at the bedside for everyone who enters the patient’s room. Icons provide a mechanism to communicate alerts that are understood and actionable across all stakeholders.
References
- 1.Robert Wood Johnson Foundation. [Accessed Sept. 3, 2008];Interdisciplinary Nursing Quality Research Initiative. www.inqri.org.
- 2.Morse JM. Preventing patient falls. Thousand Oaks: Sage Publications; 1997. [Google Scholar]
- 3.John S. [Accessed Sept. 3, 2008];Dykes Illustration. www.jsdykes.com.
- 4.Miles MB, Huberman AM. Qualitative data analysis. 2 ed. Thousand Oaks: SAGE; 1994. [Google Scholar]
- 5.Powsner SM, Tufte ER. Graphical summary of patient status. Lancet. 1994;344(8919):386–389. doi: 10.1016/s0140-6736(94)91406-0. [DOI] [PubMed] [Google Scholar]
- 6.Lancet LS, Martin CG, Cantor SB, et al. Influence of data displays format on physician investigators' decisions to stop clinical trials. Brit Med J. 1999;318(7197):1527–1531. doi: 10.1136/bmj.318.7197.1527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Morrow DG. Icons improve older and younger adults' comprehension of medication information. J Gerontology B Psychol Sciences:Social Sciences. 1998;53(4):P240–P244. doi: 10.1093/geronb/53b.4.p240. [DOI] [PubMed] [Google Scholar]
- 8.Kools M, van de Wiel MW, Ruiter RA, et al. Pictures and text in instructions for medical devices: effects on recall and actual performance. Pt Educ & Counsel. 2006;64(1–3):104–111. doi: 10.1016/j.pec.2005.12.003. [DOI] [PubMed] [Google Scholar]
- 9.Waltz CF, Strickland OL, Lenz ER. Measurement in nursing and health research. 3 ed. Philadelphia: F.A. Davis Company; 2005. [Google Scholar]
- 10.Wyatt J, Altman D. Prognostic models: Clinically useful or quickly forgotten? British Medical Journal. 1995;311(9):1539–1541. [Google Scholar]
- 11.Karwowski W. International Encyclopedia of Ergonomics and Human Factors. New York: Taylor & Francis; 2006. [Google Scholar]
- 12.Payne PR, Starren JB. Quantifying visual similarity in clinical iconic graphics. JAMIA. 2005;12(3):338–345. doi: 10.1197/jamia.M1628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ruland CM, Starren J, Vatne TM. Participatory design with children in the development of a support system for patient-centered care in pediatric oncology. JBI. 2008;41(4):624–635. doi: 10.1016/j.jbi.2007.10.004. [DOI] [PubMed] [Google Scholar]