Abstract
Patient falls and fall-related injuries are serious problems in hospitals. The Fall TIPS application aims to prevent patient falls by translating routine nursing fall risk assessment into a decision support intervention that communicates fall risk status and creates a tailored evidence-based plan of care that is accessible to the care team, patients, and family members. In our design and implementation of the Fall TIPS toolkit, we used the Spiral Software Development Life Cycle model. Three output tools available to be generated from the toolkit are bed poster, plan of care, and patient education handout. A preliminary design of the application was based on initial requirements defined by project leaders and informed by focus groups with end users. Preliminary design partially simulated the paper version of the Morse Fall Scale currently used in hospitals involved in the research study. Strengths and weaknesses of the first prototype were identified by heuristic evaluation. Usability testing was performed at sites where research study is implemented. Suggestions mentioned by end users participating in usability studies were either directly incorporated into the toolkit and output tools, were slightly modified, or will be addressed during training. The next step is implementation of the fall prevention toolkit on the pilot testing units.
Keywords: Inpatient falls, Prevention, Risk assessment, Risk factors
PROBLEM STATEMENT
Patient falls and fall-related injuries are serious problems in acute care hospitals. Falls and injuries resulting from inpatient falls are employed as standard, publicly reported metrics of the quality of nursing care. The Centers for Disease Control and Prevention has invested nearly $25 million in fall-related research and programs over the past two decades.1 Despite this worthy investment, there is insufficient evidence to date to link a specific fall prevention protocol with decreased falls in hospitalized patients. Nurses routinely complete a fall risk assessment on all hospitalized patients. Based on preliminary work completed at Partners HealthCare, we found that fall risk status is often documented by nurses in the patient record. However, not all members of the care team routinely access the nursing documentation, and verbal communication of fall risk status is inconsistent. A mechanism is needed to communicate a patient's fall risk assessment and the associated, tailored interventions to prevent falls.
LESSONS LEARNED FROM FOCUS GROUP INTERVIEWS
The Fall TIPS (Tailoring Interventions for Patient Safety) research study was conducted over four phases and was funded by the Robert Wood Johnson Foundation to translate routine fall risk assessment into interventions to prevent falls. This research project was reviewed and approved by the Partners HealthCare Human Subjects Committee. The first phase of the Fall TIPS study involved exploring the barriers and facilitators to fall prevention and existing fall prevention practices from the perspective of patients, family members, nurses, and other healthcare providers in hospitals. The second phase of the Fall TIPS study involved building a fall prevention toolkit (FPTK). The third phase evaluated the FPTK, and the fourth phase will include making recommendations for improvement of the FPTK and dissemination of research findings. This article describes phase 2 of the study; the software development process of the FPTK and the usability testing with end users.
After conducting qualitative focus group interviews with patients, family members, nurses, and other healthcare providers, the research group analyzed the transcripts using basic content analysis methods2 to interpret the obtained descriptive data. The complete analysis will be reported elsewhere.3 Interventions considered effective and feasible by bedside clinicians were abstracted from transcript analysis subthemes and grouped under the six areas of risk included on the Morse Fall Scale (MFS): history of falling, secondary diagnosis, ambulatory aid, intravenous (IV)/heparin lock, gait, and mental status. The MFS is the standard risk assessment tool used by all nurses at the participating hospitals. Research team members worked with an illustrator to develop a series of icons (copyrighted) to represent each of the MFS areas of risk and the associated fall prevention interventions that were identified though analysis of the qualitative interview transcripts.
The Fall TIPS application aims to prevent patient falls by translating routine nursing fall risk assessment into a decision support intervention that communicates fall risk status and creates a tailored evidence-based plan of care that is accessible to the care team, patients, and family members. The evidence-based interventions included in the Fall TIPS logic have been identified and validated by practicing nurses, physicians, physical therapists, and other interdisciplinary care providers. The Fall TIPS toolkit aims to provide a workflow-friendly solution that overcomes the usual silos associated with communication of fall risk status and evidence-based, feasible interventions to prevent patient falls in hospitals.
MODEL OVERVIEW
In our design and implementation of the Fall TIPS toolkit, we used the Spiral Software Development Life Cycle (SDLC) model. The SDLC model is a risk-reduction–oriented model that combines the features from the waterfall and the prototyping models.4 The advantage of the SDLC model is that it supports a product design that customers evaluate during each phase of development.5 This increases adaptation and results in a product that is accepted by users because as the needs of the project change, the software changes are made to accommodate the users. Although this model can be complicated and costly, it is the best model for this project based on our requirements for useful and defect-free software before implementation on busy patient care units.
PRELIMINARY DESIGN
A preliminary design of the application was created based on initial requirements defined by senior project leaders, feedback gathered from users during focus group sessions, and by incorporating the MFS assessment currently used in hospitals involved in the research study. This design was created to get an idea of the desired look and feel for the Fall TIPS application. The first design consisted of four distinct columns: MFS risk factors, responses to the MFS risk, interventions specific to the MFS areas of risk, and numeric score of the selected MFS risk response. Remaining fields on the toolkit included patient name, patient medical record number, patient location in the hospital, and total MFS score.
One of the major issues found with this design was that some interventions were listed more than once if they were shared by different MFS risks. For example, secondary diagnosis and IV/heparin lock risks both share the intervention, “implement toileting schedule,” and this intervention was listed in both rows of each MFS risk. This resulted in a cluttered display that was potentially confusing for users. The preliminary design also did not include any of the output tools generated by the toolkit.
REQUIREMENTS FOR DESIGN AND DEVELOPMENT OF THE FIRST PROTOTYPE
The first step of the SDLC model is to gather detail and requirements from end users of the system.6 As previously noted, focus group sessions were conducted to ensure a good understanding of the barriers that exist in the current workflow and what is necessary to help users acclimate to a new system and workflow. Requirements were defined for six toolkit components based on focus group feedback and team expertise (Table 1).
Table 1.
Requirements for First Prototype
| Component | Requirements |
|---|---|
| MFS | (1) Easy to use |
| (2) Same look/feel as current version used at hospitals | |
| (3) Automatic calculation of total score | |
| (4) Responses are exclusive (cannot pick more than one response) | |
| (5) More information for risks | |
| (6) Generate tools (bed poster, plan of care, patient education, aide assignmenta) | |
| Interventions | (1) Scaled-down list |
| (2) Autoselect interventions based on risk responses | |
| (3) Allow for customization (modifying interventions) | |
| Bed poster | (1) Easy to see |
| (2) Customized for each patient | |
| Plan of care | (1) Group risk with interventions and display related icon |
| (2) Patient banner with problem displayed on top | |
| Patient education | (1) Easy to read |
| (2) Tailored based on patient's areas of risk identified with the MFS | |
| Aide assignmenta | (1) Created for nursing assistants |
| (2) List of patients on floor | |
| (3) Tailored interventions with icons listed on assignment sheet |
Initially, the design had four tools that were created based on the selected answers in the toolkit: bed poster, plan of care, patient education, and aide assignment. Further discussions with users resulted in eliminating the aide assignment form from the toolkit since the bed poster would serve the same function for the nursing assistants.
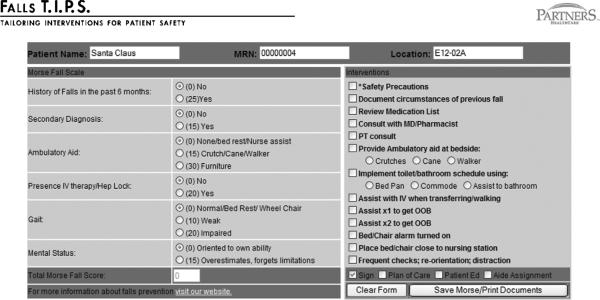
Based on information gathered from focus group interviews, feedback from our team of experts, and literature findings, a prototype was designed to incorporate predefined risk interventions and the output tools necessary for a successful implementation of the Fall TIPS toolkit. The first prototype resolved issues found in the preliminary design: repeating interventions lead to possible user confusion, and score displayed for each risk took up valuable real estate on the form (Figure 1).
FIGURE 1.
First Fall TIPS toolkit prototype.
The first prototype was designed such that when responses to MFS risks are selected on the toolkit, the associated interventions are autochecked. The application handled the possibility of duplicate interventions by assigning a primary risk for each duplicate intervention. For example, ambulatory aid risk = furniture and mental status risk = overestimates share “bed alarm turned on” as an intervention. However, the primary risk for “bed alarm turned on” intervention is mental status risk = overestimates. Therefore, if both risks are present, the intervention would display next to only the mental status risk. If only ambulatory aid risk = furniture is present, the bed-alarm intervention would display next to the ambulatory aid risk.
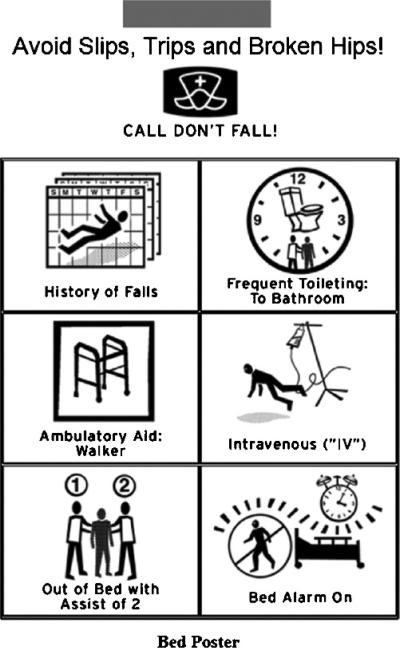
Other development work involved design of icons for specific interventions considered to be fundamental in reducing falls. The areas of risk and interventions that have associated icons are history of falls, assist with toileting, assist with ambulating, bed alarm on, assist with IV, and out-of-bed assistance. In response to feedback from focus group participants, design of icons assist with toileting and assist with ambulating was further elaborated to represent a specific toileting or ambulating aid, depending on the user's selection in the toolkit. More discussion on the development of the icons is reported elsewhere.7
The first prototype also contained functionality that displayed the total calculated MFS score at the bottom of the scale on the toolkit and updated the total score as each risk answer was selected. The numerical value of each MFS risk answer was indicated by listing that number next to each answer to allow users to see the weight of each MFS answer upon the total score.
The three output tools available to be generated from the toolkit are bed poster, plan of care, and patient educational handout. The bed poster was designed as a one sheet printout placed above the patient's bed and displayed icons representing tailored risks and interventions so that nurses, nursing aids, and others at the patient's bedside would have a visual alert of how to care for a patient. The plan-of-care document was developed to assist nurses and other professional caregivers with day-to-day care of their patients. The patient's risks with their associated interventions were listed on the plan of care, along with the same icons for the interventions displayed on the bed poster. The patient education form simply listed reasons for why the patient is at risk for falling and suggestions of how to prevent falls. The first section entitled, “Why are you at risk for falls?” listed patients' risks in a patient-friendly manner. The interventions were listed in a section captioned, “How will we work together to prevent you from falling,” and listed the interventions using patient-friendly verbiage. The associated icons were displayed in a horizontal row below the intervention section. This was done so that the patient and family members could make a correlation with the icons displayed on the bed poster and receive an explanation of each.
The database design started early and used Entity-Relationship Modeling8 to ensure that the database supported all data elements needed to be collected for research analysis. Several team members reviewed the analysis plan and the entity-relationship diagram to discuss data elements and match the fields in the database with data in the analysis plan. As new features and functionalities were added in each phase of development, database alterations were made to support those changes. During the pilot (nurse champions only) phase of the project, champion users will be implementing the Fall TIPS application in their daily workflow. This phase in our project implementation will identify any issues with the data structure and will verify that all pertinent data for the study are included in the data structure. Reports will be written to validate that the database design supports the data analysis necessary for the Fall TIPS project.
Heuristic Evaluation
Heuristic evaluation of the first toolkit prototype and tool outputs was conducted by a usability expert and was guided by Jacob Nielsen's 10 usability guidelines:
visibility of system status,
match between system and the real world,
user control and freedom,
consistency and standards,
error prevention,
recognition rather than recall,
flexibility and efficiency of use,
aesthetic and minimalist design,
help users recognize, diagnose, and recover from errors, and
help and documentation.9
During the heuristic evaluation phase, we were able to identify several areas where our first prototype and output tools were not adhering to the usability principles listed above and made changes to ensure that they are ready for user testing.
Requirements Analysis Based on Heuristic Evaluation
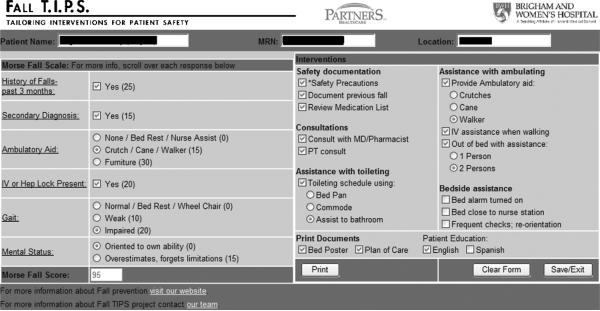
In the first prototype, all interventions were displayed in one column and in the same order as risks listed on the toolkit. Our usability expert suggested grouping interventions into the following five functional role categories: safety documentation, consultations, assistance with toileting, assistance with ambulating, and bedside assistance, listing interventions under each heading. These changes made design more aesthetic and reduced interface clutter, as well as gave the user a better mental and visual understanding of the risk to intervention functionality.
Referencing Nielsen's usability guidelines of error prevention and user control, we decided to make modifications to the functional buttons on the toolkit. To prevent possible user errors, the location of the two main functional buttons (clear form and save/print) was exchanged. The clear-form button was located directly below the risk selections, and we anticipated users unintentionally selecting this button during navigation through the toolkit. This decision was made to prevent users from clearing the form rather than saving it. A third, close/exit button was added to the toolkit to allow users easy exit from the application (Figure 2).
FIGURE 2.
Third Fall TIPS toolkit prototype.
During heuristic evaluation, we came to conclusion that the toolkit lacked validity and feedback of the system for users. In the first prototype, once a user selected save/print button, the toolkit would close, and the user was left to assume that their information was saved without receiving any visual confirmation. It was decided to add a processing message that will be displayed once save/print button is selected to allow users to know that the information they entered was saved. Other changes made to the toolkit included adding age and sex of the patient to the patient-name field to offer additional information for the provider that may be pertinent to the risk of falling. All text fields displaying patient information were disabled to prevent users from altering data printed on the output tools.
Heuristic evaluation was performed on the three output tools as well. Our usability expert worked with the research team to revise the patient education form layout to be more visually appealing. Group member also suggested lowering the reading level of information for it to be understandable for patients of varying language skills. After a few consultations with the research team, a revised version of the patient education was produced containing shortened text and using the layout suggested by our usability expert.
DESIGN AND DEVELOPMENT OF THE SECOND PROTOTYPE
Strengths and weaknesses of the first prototype were identified by heuristic evaluation. Our usability expert provided suggestions on how we could reduce screen clutter and the number of clicks for a user. The strengths of the first prototype were that it was similar to the existing MFS documentation (paper and applications) used at the hospitals involved in the research study. The weakness of the toolkit was that its user interface was cluttered. This was a result of having some unnecessary controls on the screen for the risk answers and interventions listed in one column, with no organization (Figure 1).
The patient education tool underwent major changes in layout so that it was easier to read and follow. The first version of the patient education document displayed the risks for the patient on top, under the heading, “Why are you at risk for falls?” If the patient had a history of falling, the risk displayed would be: “You have fallen before and may fall again.” Interventions were displayed under the heading, “How will we work together to prevent you from falling while in the hospital?” The intervention for history of falling would read: “Tell your nurse about any recent falls.” The major change we made to the document was displaying the interventions and icons together in a table format so that the patient or family member could make a direct connection with the intervention and the icon.
CODING IMPLEMENTATION
The design and development of the toolkit, up until after the heuristic evaluation of the first prototype, were client side programming. HTML, DHTML, and JavaScript were the three technologies used to develop the preliminary design, first prototype, and second prototype. HTML and JavaScript (Oracle, Redwood Shores, CA) were used to develop the Fall TIPS toolkit application. DHTML and JavaScript were used to dynamically build the three tools generated by the toolkit. The second prototype changed from primarily client-based software to a client-server architecture. The toolkit was created as a stand-alone Web-based ASP.NET application. Partners HealthCare Systems supports a Services Oriented Architecture (SOA). SOA is a method for systems development and integration where functionality is grouped around business processes and packaged as interoperable services.10 Simple object access protocol (SOAP) Web services were used to retrieve patient information from the study entities. An SQL database was created to store data selected in the Fall TIPS toolkit.
USABILITY TESTING WITH END USERS
Usability testing was performed at sites where research study is implemented: the Massachusetts General Hospital in Boston, MA and Brigham and Women's Hospital in Boston, MA. Users consisted of three groups: providers who would be using the toolkit during the research study, individuals who will not be using the application, and an informatics practice committee group. Approximately 25 people participated in usability testing of the toolkit and printouts.
Usability studies conducted were observational, where users were given at least two different scenarios to perform and were observed interacting with the application while completing assigned tasks. Five different scenarios were written for the purpose of this study, each containing four different tasks. Each task guided the user to perform a series of actions through the toolkit that we anticipated typical users to encounter when using the application.
Example of a Scenario
Your patient is a 75-year-old woman who was transferred from the emergency department to your care unit. She tells you that she fell in her bathroom a few years ago when she experienced a heart attack. Because she is also ill with breast cancer, she is receiving chemotherapy drugs through a central IV line. She tells you that even though she has been using furniture to get around and is very unsteady on her feet, she feels confident and overly independent and does not think she requires any assistance while walking.
Steps to complete the task:
Go to falls assessment toolkit
Complete MFS
Save and print all documents
Data and feedback collected during usability studies were analyzed, and changes to the toolkit and output tools were proposed to the research team for approval during weekly meetings.
An after-task online survey was created and distributed to users who participated in the observation studies. Questions in the survey consisted of user opinions about layout and color scheme, ease of use, ease of learning, overall satisfaction and usefulness of the toolkit, and suggestions for improvement. Data collected from the survey were analyzed and confirmed user's overall satisfaction with the application.
Issues and Findings From Usability Studies
Users conveyed helpful suggestions, which influenced further improvements to the toolkit and the three output tools. The types of issues, suggestions, and concerns that came about from usability studies were divided into five categories for analysis: toolkit, bed poster, plan of care, patient education form, and workflow concerns.
Toolkit Issues
The toolkit closed after saving and printing, at the action of one button; however, our users requested for the toolkit not to close automatically; they wanted to choose when to exit the application themselves. Another suggestion collected from usability studies was to make the underlined MFS risks links more evident. The MFS risks consisted of links containing information about each risk, but to our users, this was not evident. A visual cue was requested, such as a hover-over rather than a standard mouse arrow that was originally implemented. Some users also requested more information on how to score a patient using MFS. For example, they wanted to know what classifies the patient as having a weak gait as opposed to having an impaired gait. We also received feedback from many users requesting a visual display of how the numeric number of the patient's MFS score translates to the level of fall risk. If a patient scored at high risk for a fall, users wanted this information displayed on the toolkit in addition to the total MFS score.
Sign Printout Issues
Bed poster sign (Figure 3) received uniform approval from our usability groups. A few users had concerns that the printout was not large enough and wanted to see if there was a possibility of maximizing all of the available space on a page. Our users also noticed a misspelling in one of the icons.
FIGURE 3.
Bed poster.
Plan-of-Care Printout Issues
Our original plan-of-care printout contained a sign/resolve field for each risk that was selected from the toolkit. Users were concerned that having these fields will make documentation time consuming and cumbersome. In addition, users suggested adding date, time, total MFS score, and signature sections to the printout.
Patient-Education Printout Issues
Some users were concerned that the form contains too much reading information that may not make sense from a patient's perspective. Users also requested foreign language versions of the document, specifically Spanish, so that every patient can benefit from fall education tailored to them.
Workflow Issues
We encountered some workflow issues brought up by users that will be addressed during training before the go-live at each hospital. Some users questioned how interventions were selected by the system on the toolkit, the logic behind autoselection based on the chosen risk response. To some users, it not clear whether selected consult interventions were sent electronically to an appropriate department. During training, we will emphasize that the toolkit displays only the suggested interventions, and it will be up to the provider to schedule consult appointments. MD/pharmacist consult and review medication list interventions were not clear to all users, the reason, and their purpose. A number of users also had concerns of how the new toolkit application will fit in or take over their current MFS assessment process. A group of users mentioned that they would prefer to be able to retrieve and see each assessment completed for patients online, rather than printing out forms for each assessment and adding them to the patient's care book. Because this request requires an electronic clinical documentation at hospital institutions and is out of scope for this project, we were not be able to accommodate it.
Requirements Analysis Based on Usability Testing and Design of Prototype 3
Suggestions mentioned by users were either directly incorporated into the toolkit and output tools, were slightly modified, or will be addressed during training. The usability study team created a bug/enhancement tracking tool as a central place for managing requirements and bug fixes for the toolkit and output tools. This tool contained general description of each request, severity or importance, request decision, and issues encountered during coding and testing of that request.
End users requested a Spanish version of the patient education form. To accommodate this request, translation of the text and icons had to be performed. We also added a new checkbox to the toolkit for users to select a Spanish version of the document. English will remain to be the preselected option during first fall risk assessment; however, users will be able to select a Spanish version from the tool-kit for Spanish-speaking patients.
To offer more information and guidance to users on selecting responses to the MFS, it was decided to add hover-over text for each risk response, providing a brief overview and instructing users under which circumstances to select a given response. To make the MFS risk links more evident, we decided to convert the mouse arrow to a standard, well-recognized hand sign when a user hovers over the risk, as well as adding hover-over text instructing user to click on the link for more information. In addition, the risk information files accessed by clicking on a risk were modified to give users specific information on the risk and how to score a patient within that category.
An “in progress” message consisting of image and text was added to give users confirmation that information entered on the toolkit is being saved. The message will display when a user selects “save/exit” button and would remain until the data entered on the toolkit is saved to the database. While this message is displayed, users will not be able to perform any action on the toolkit. Once the data are saved, the message will be removed, and the user will be able to navigate throughout the toolkit.
Due to a high number of requests to see the MFS range for each patient (high or low) on the toolkit, we made a decision to change the color of total MFS score greater or equal to 45 from black to red, signaling to the user that a patient is at high risk for a fall. Our group decided to take this route of giving the user a visual cue as opposed to telling them whether the patient is at low or high risk for falls.
Enhancements were also made to the output tools. All users participating in the usability study were pleased with the bed poster printout. To make the patient education form more user-friendly and accepted, it was decided that further usability evaluation is needed with actual patients. The plan-of-care printout also underwent changes following feedback from users. Total MFS score was added to the form to allow users to see how a patient scored during the previous assessment. To help users distinguish each form, the form title was added at the bottom of the page to each printout.
DISCUSSION AND CONCLUSIONS
The development and usability testing of the Fall TIPS toolkit were completed using an iterative approach. With the SDLC model as the conceptual underpinning of this work, our design and usability team built the original prototype based on end-user requirements generated from focus group interviews. The team then worked closely with end users to revise and refine the toolkit to address user concerns and workflow issues. The next step for the research team is implementation of the FPTK on the pilot-testing units. While we believe that the Fall TIPS tool-kit is “ready” for implementation, we view the pilot testing as an additional opportunity to evaluate the degree to which the FPTK meets user expectations and supports fall prevention practices in the context of busy patient care workflows. Based on user feedback gathered during pilot testing, we will make additional modifications before full implementation. While we will limit code changes after implementation to changes essential for operation and use of the FPTK, we will continue to solicit and record end-user feedback. End-user feedback will be used to generate a set of recommended enhancements for a production level FPTK.
Acknowledgments
This project was funded by the Robert Wood Johnson Foundation Interdisciplinary Nursing Quality Research Initiative and Partners HealthCare.
REFERENCES
- 1.Centers for Disease Control and Prevention [Accessed September 16, 2008]; http://www.cdc.gov/.
- 2.Miles MB, Huberman AM. Qualitative Data Analysis: An Expanded Sourcebook. 2nd ed. SAGE; Thousand Oaks, CA: 1994. [Google Scholar]
- 3.Dykes PC, Carroll D, Benoit A, Hurley A, Middleton B. Why do patients in acute hospitals fall? Can patient falls be prevented? J Nurs Adm. 2009;39(6):299–304. doi: 10.1097/NNA.0b013e3181a7788a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Human Base India Inc, an Information Technology Company [Accessed September 23, 2008];Software Development Life Cycle Models. http://www.humanbaseindia. com/training/SDLC.htm.
- 5.Spiral model [Accessed September 23, 2008];Wikipedia. The Free Encyclopedia. http://en.wikipedia. org/wiki/Spiral_model.
- 6.Boehm BW. A Spiral model of software development and enhancement. IEEE Comput. 1988;21:61–72. [Google Scholar]
- 7.Hurley AC, Dykes PC, Carroll DL, Dykes PC, Middleton B. Fall TIP: validation of icons to communicate fall risk status and tailored interventions to prevent patient falls. Stud Health Technol Inform. 2009;146:455–459. [PMC free article] [PubMed] [Google Scholar]
- 8.Spiral model [Accessed October 11, 2008];Wikipedia. The Free Encyclopedia. http://en. wikipedia.org/wiki/Entity-relationship_model.
- 9.useit.com: Jakob Nielsen on usability and web design. [Accessed September 16, 2008];Ten usability heuristics. http://www.useit.com/papers/heuristic/heuristic_list.html.
- 10.Service-oriented architecture [Accessed September 23, 2008];Wikipedia. The Free Encyclopedia. http://en.wikipedia.org/wiki/Service-oriented_architecture.