Abstract
Information technology represents an excellent medium to deliver contingencies of reinforcement to change behavior. Recently, we have linked the Internet with a science-based, behavioral treatment for cigarette smoking: abstinence reinforcement therapy. Under abstinence reinforcement interventions, incentives are provided for objective evidence of abstinence. Several studies suggest that the intervention is effective in initiating abstinence. The intervention addresses limitations (access, cost, sustainability, dissemination potential) inherent in traditional abstinence reinforcement delivery models. It can also be applied to vulnerable, at-risk populations, and to other behavior to promote health. Information technologies offer unprecedented and rapidly expanding opportunities to facilitate behavior change.
Keywords: Cigarette smoking, abstinence reinforcement, Internet, contingency management, carbon monoxide
Cigarette smoking is the largest preventable risk factor for morbidity and mortality in developed countries. Smoking related diseases cost over $96 billion in medical expenses per year and over $97 billion in loss of productivity (CDC, 2008). Although the United States Public Health Service endorses various pharmacotherapies and counseling for smoking cessation, the majority of patients relapse within six months, even when both treatments are used together (Ahluwalia, Harris, Catley, Okuyemi, and Mayo; 2002; Eisenberg, Stitzer, and Henningfield, 1999; Fiore, Smith, Jorenby, and Baker, 1994; Hurt, Offord, Johnston, Dale, Khayrallah, Schroeder, et al., 1997). Several researchers have argued that innovative and more intensive smoking cessation programs are necessary (e.g., Fagerstrom, Kunze, Schoberberger, Breslau, Hughes, Hurt, et al., 1996; Stitzer, 1999). Over the past several years, we have developed and tested an innovative and intensive intervention: Internet-based abstinence reinforcement therapy. In this paper we will discuss the background and development of the intervention, and we will highlight potential future directions to promote smoking cessation and other health-related behavior.
Internet-based treatments for cigarette smoking
The Internet has emerged as a promising medium to deliver a range of treatments to promote health, including smoking cessation (e.g., Cobb, Graham, Bock, Papandonatos, and Abrams, 2005; Etter, 2006; Mallen, Blalock, and Cinciripini, 2006; Stoddard, Delucchi, Muñoz, Collins, Pérez, Augustson, and Lenert, 2005; Woodruff, Edwards, Conway, and Elliot 2007). Currently, over 212 million people report Internet use in the United States, which represents about 72% of the population (http://www.Internetworldstats.com/am/us.htm). Worldwide, there are over 1.5 billion Internet users, and the growth rate in users since 2000 has exceeded 340%. Estimates suggest that there are anywhere between 3.6 to 10 million active Internet searches per year for smoking cessation information in the United States (Cobb and Graham, 2006; data not available in other countries). Internet-based interventions can reduce or eliminate significant barriers to treatment. For example, they can they can narrow the “access gap” to treatment, and provide education and social support in asynchronous and synchronous formats (see McDaniel and Stratton, 2006 for a review).
A number of Internet based treatments for smoking cessation have been developed (e.g., Cobb et al., 2005; Etter, 2006; Mallen et al., 2006; Stoddard et al., 2005; Woodruff et al., 2007). The design of these Internet treatments has varied from chat rooms, to tailored feedback based on questionnaire answers, to behavioral strategies to cope with cravings. A recent review of Internet-based smoking cessation treatments suggested that 9 out of the 19 (47%) interventions showed improvements in smoking cessation compared to control at follow-up (Walters, Wright, and Shegog 2006). The magnitude of the difference in rates of abstinence among Internet and control treatments ranged from 4 to 13%. However, even in absolute terms, a rate of 13% could still result in a substantial quit rate. In an application to International Business Machines (IBM) employees, Graham et al. (2007) argued that their Internet-based program could result in about 2000 quitters in one year. This number assumes a 13% success rate and about 16,000 potential smokers at IBM.
Although the studies cited above indicate the formidable reach and convenience of the Internet, there may be ways to increase the efficacy of Internet-based treatment delivery. One method would be to deliver a “high dose” behavioral treatment such as abstinence reinforcement. Indeed, a large and growing number of studies indicate that contingent reinforcement of smoking abstinence can exert powerful and precise control over smoking1 (Alessi, Badger, Higgins, 2004; Crowley, MacDonald, Zerbe, Petty, 1991; Dallery and Glenn, 2005; Dallery, Glenn, and Raiff, 2007; Higgins, Heil, Solomon, Bernstein, Lussier, Abel, Lynch, Badger, 2004; Lamb, Kirby, Morral, Galbicka, Iguchi, 2004; Rand, Stitzer, Bigelow, Mead, 1989; Roll and Higgins, 2000; Roll, Higgins, Badger, 1996; Shoptaw, Jarvik, Ling, Rawson, 1996; Shoptaw, Rotheram-Fuller, Yang, Frosch, Nahom, Jarvick, Rawson, Ling., 2002; Stitzer and Bigelow, 1984, 1985; Tidey, O’Neill, and Higgins, 2002). Under abstinence reinforcement procedures, it is necessary to obtain objective evidence of smoking status. Such evidence provides the basis for reinforcement, which usually entails a monetary voucher that can be exchanged for goods and services. In most studies, positive consequences were contingent on specified reductions in breath carbon monoxide (CO). For example, Corby, Roll, Ledgerwood and Schuster (2000) applied a brief, one-week abstinence reinforcement intervention with adolescent smokers. In a within-subject reversal design, money was made contingent on COs of less than 8 parts per million (ppm). Large increases in the mean number of CO samples that were at or below 8 ppm were noted when contingent monetary payments were introduced.
There is also emerging evidence that abstinence reinforcement may produce higher rates of smoking reductions and abstinence than the nicotine patch (Glenn and Dallery, 2007; Tidey et al., 2002; Wiseman, Williams, and McMillan, 2005). Wiseman et al. (2005) found that a voucher-based reinforcement intervention alone produced greater decrements than a nicotine patch (21 mg) in a two-week intervention study with cocaine-abusing outpatients. Relative to placebo, the patch only produced small decreases in CO levels.
Intensive behavioral treatment may be particularly effective during the initial, critical weeks of a quit attempt. Abstinence during the first two weeks of a quit attempt predicts long-term treatment success (Garvey, Bliss, Hitchcock, Heinold, Rosner, 1992; Gourlay, Forbes, Marriner, Pethica, McNeil, 1994; Kenford, Fiore, Jorenby, Smith, Wetter, Baker, 1994; Yudkin, Jones, Lancaster, Fowler, 1996), and at least 75% of smokers relapse within 2–3 days following an initial unsupported quit attempt (Hughes, Gulliver, Fenwick, Valliere, Cruser, Pepper, Shea, Solomon, Flynn, 1992). When smoking status during this key period is manipulated experimentally, the long-term effects can still be predicted based on initial outcomes (Heil, Alessi, Plebani, Badger, Higgins, 2004; Higgins, Heil, Dumeer, Thomas, Solomon, Bernstein, 2006). Of course, Internet-based programs can be extended beyond these initial weeks, but the evidence about the importance of initial success encourages use of a combination of intensive monitoring and frequent reinforcement to help maximize continuous smoking abstinence during the initial weeks of the cessation effort.
Potential obstacles in applying abstinence reinforcement
A significant obstacle in applying abstinence reinforcement therapy to smokers is measuring CO on a daily basis for a sustained period. In several studies, COs were assessed for approximately one to two weeks (e.g., Corby et al., 2000; Roll et al., 1996; Stitzer and Bigelow, 1985; Tidey et al., 2002; cf. Alessi et al., 2004). Other studies have used rather laborious methods, which were also limited in terms of the frequency and duration of monitoring. For example, CO samples have been: (a) collected by research technicians who made evening visits to each participant’s home seven days per week (Crowley et al., 1991), (b) provided by adolescents who visited a clinic twice per day for one week (Corby et al., 2000), (c) delivered twice per week to a clinic by participants (Rand et al., 1989), and (d) delivered to a clinic by participants once per day (Lamb et al., 2004). Because breath CO has a half-life of about 6–8 hours (Crowley et al., 1991; Middleton and Morice, 2000), samples should be collected at least twice per day to accurately measure smoking status (Javors, Hatch, Lamb, 2005). In one case CO samples were collected three times per day (Alessi et al., 2004).
Although these methods have some limitations, using breath CO as a basis for reinforcement also entails some advantages. Breath CO can be measured using a small, hand-held, lightweight, battery powered monitor. The measurement procedure requires participants to hold their breath for about 15 seconds, and then exhale into the mouthpiece. Thus, the procedure is non-invasive, relatively inexpensive, and provides immediate feedback. The monitor measures breath CO in parts per million based on the conversion of CO to a catalytically active electrode. After inhalation, CO displaces oxygen in red blood cells and forms carboxyhemoglobin (Middleton and Morice, 2000). It may remain in the blood for up to 24 hours, and may vary with gender and physical activity (Middleton and Morice, 2000). Schuh and Stitzer (1995) described the time course of changes in CO with abstinence. Ten participants smoked ad lib for 15 minutes before the session. After smoking, their average CO output was 30 ppm. After six hours of abstinence, their average CO was 13.8 ppm. Thus, breath CO is an easy to use and sensitive measure of recent smoking.
Nevertheless, CO-based measurement procedures may be too burdensome and infrequent for clinically practical and effective implementation of voucher reinforcement in an outpatient setting. The staffing required to make home visits, even for a small sample of patients, could become expensive and onerous. Although requiring patients to make visits to the clinic on a daily basis may be more practical, the requirement represents a substantial response effort. Such a response effort may limit the success of and access to the treatment. Also, because most clinics are only open during workdays, such visits could occur only five days a week. It would also be desirable if a potentially effective intervention could be available to smokers who live a considerable distance from a treatment provider, such as rural smokers (Aloise-Young, Wayman and Edwards, 2002; Epstein, Botvin and Spoth, 2003).
There are several potential solutions to these problems. One possibility would be to use abstinence reinforcement for a relatively brief period to initiate abstinence and then transition to an alternative biomarker of nicotine: cotinine (e.g., Higgins et al., 2004). Cotinine is a metabolite of nicotine that can be detected in urine or saliva and can provide a highly specific and sensitive assay for smoking status (Ahijevych, Tyndale, Dhatt, Weed, Browning, 2002; Hughes, Keely, Niaura, Ossip-Klein, Richmond, and Swan, 2003). Currently, cotinine analysis is relatively expensive but it could be collected just once per week to minimize costs (Ahijevych et al., 2002), which may have advantages in certain settings. New low-cost urinary dipstick techniques may prove to be useful (Parker, Lasater, Windsor, Wilkins, Upegui, Heimdal, 2002). One limitation of using cotinine is that, for obvious reasons, it cannot be used to measure smoking status in conjunction with nicotine replacement therapy (but see Jacob, Hatsukami, Severson, Hall, Yu, Benowitz, 2002 for techniques to distinguish cotinine derived from nicotine in tobacco). Another possibility would be to use remote, Internet-based technology to monitor smoking status (Dallery and Glenn, 2005; Dallery et al., 2007; Glenn and Dallery, 2007).
Internet-based abstinence reinforcement to promote smoking cessation
In several studies, we verified smoking status by employing user-friendly Internet technology to observe participants providing CO samples via a web camera. The results, discussed below, indicate that the voucher program produced high rates of abstinence. We were able to collect objective evidence of smoking status on a frequent and sustained basis. After the system was in place, there was excellent compliance with a two sample per day breath CO collection schedule. In one study, out of 1120 total samples scheduled in the study, over 97% were provided (Dallery et al., 2007). Thus, the Internet-based system obviated many of the logistical problems entailed by frequent CO monitoring. In addition, our study website provided access to cessation techniques, an individualized home page for each participant (which included a graph of the participant’s progress), and other cessation resources.
Dallery et al. (2007) used a home-based computer system was used to verify breath CO measurements. Twenty heavy smokers were loaned a laptop, web camera, and CO monitor. Samples were collected twice per day, with a minimum inter-sample interval of 8 hr. Ten CO samples were collected during the first baseline phase of the study (which lasted five days). Next, during the four-day “shaping” phase participants were provided with a $3.00 voucher each time they met a progressively decreasing CO criterion. The specific CO criteria were calculated based on the participants’ mean baseline CO, and on the requirement that at the end of four days the criterion had to be a CO level of 7 ppm. Shaping could be a crucial step in initiating abstinence (Lamb et al., 2004; Lamb, Morral, Galbicka, Kirby, Iguchi, 2005), but this remains an empirical question.
The main treatment phase was called the abstinence induction phase. This phase lasted 10 days (20 samples). To earn a voucher, the participant had to provide a negative CO sample, which was defined as a reading less than or equal to 7 ppm. The initial voucher value was $3.00, and this amount was increased by $.25 if a negative CO sample was provided. A $5.00 bonus voucher was earned for every third consecutive negative sample. The escalating schedule of reinforcement and the reset contingency appear to be critical in the success of voucher reinforcement procedures (e.g., Roll and Higgins, 2000; Roll et al., 1996), and such schedules are considered the standard in applications of abstinence reinforcement. If a participant’s CO level was positive, no voucher was earned for that session, and the voucher value was reset to $3.00. If the participant provided three consecutive negative CO samples, the voucher value resumed at whatever the value had been when the reset occurred.
After the main treatment phase, for four days, only the fourth and eighth samples were eligible for reinforcement (a $5.00 voucher). This was called the thinning phase. The last condition was a second baseline phase, which was identical to the first baseline phase. Participants could earn a total of $171.50 in vouchers during the study. As a point of comparison, the rate of voucher earnings in the study just described was slightly lower than other standard schedules that have produced high rates of drug abstinence (e.g., Higgins, Budney, Bickel, Foerg, Donham, Badger, 1994; Roll and Higgins, 2000; Roll et al., 1996; Silverman, Higgins, Brooner, Montoya, Cone, Schuster, Preston, 1996; Silverman, Wong, Umbricht-Schneiter, Montoya, Schuster, Preston, 1998). For example, in most standard schedules of voucher earnings for cocaine and heroin abstinence, a participant could earn $1155.00 for 12 weeks of abstinence. In other words, the earnings rate was $288.75 every three weeks for evidence of continued abstinence in these studies.
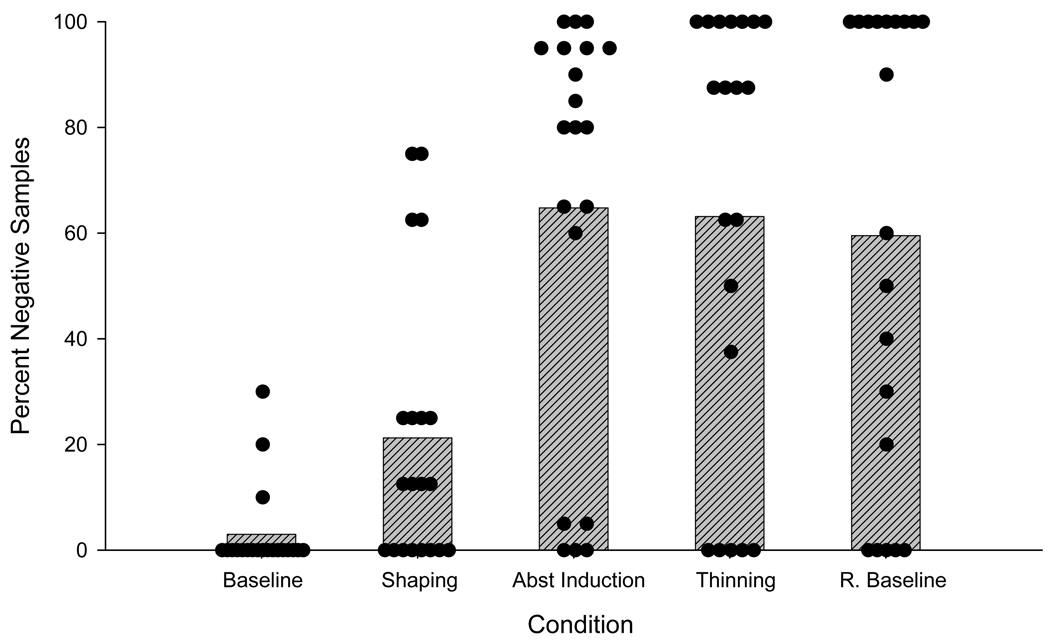
Figure 1 displays the percentage of CO samples that met criterion for abstinence. All participants continued to smoke during baseline conditions. As can be seen, the number of negative samples increased when the vouchers were introduced, and the abstinence induction phase promoted high levels of abstinence. Over 65% of the 400 CO samples were negative during treatment. It is interesting to note that smoking did not resume for ten participants in the return-to-baseline phase – no vouchers were available during this phase. Of course, a randomized, controlled study with follow up will be necessary to evaluate long term effects of abstinence reinforcement. Overall, however, the study suggests that Internet-based voucher programs can be highly effective in initiating smoking abstinence in a sample of heavy smokers.
Figure 1.
Percent negative CO samples across all study conditions. Each point represents an average value for each individual participant, and shaded bars represent condition means. Reprinted from Drug and Alcohol Dependence, 86, Dallery, J., Glenn, I. M., and Raiff, B. R., An Internet-based abstinence reinforcement treatment for cigarette smoking, pp. 230–238, Copyright 2007, with permission from Elsevier.
During the course of the study, we identified two ways to improve the system. First, we observed that three participants self-reported smoking a few cigarettes and yet were still able to meet the CO criterion of ≤ 7 ppm. To our knowledge our 7 ppm cutpoint was the lowest CO cutpoint used to verify abstinence at the time. Research was published during data collection indicating that lower CO thresholds may be necessary in contingency management programs (Alessi et al., 2004; Javors et al., 2005). Second, we developed a secure system so that participants could use their own computers. In the Dallery et al. (2007) study, we administratively locked access to the laptop so participants could not alter the date and time properties of the computer or video file. (Presumably, if participants had access to these features, they could falsify a sample by creating and then saving a number of video samples after a period of abstinence, and then send them to the clinic at the appointed times).
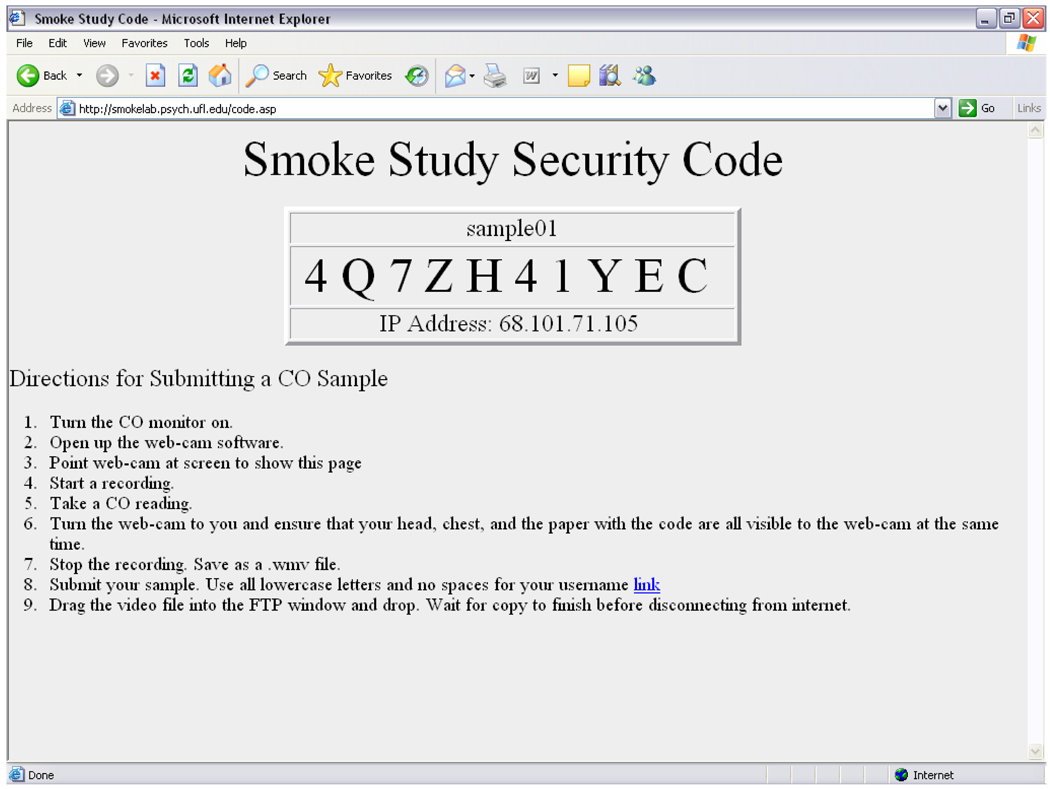
Thus, in the next phase of the research, we lowered the CO criterion to ≤ 4 ppm. Also, rather than locking and loaning laptops, we created a secure system by using a dedicated server. Participants logged onto the server when they were ready to leave a sample. A simple software application, housed on the server, generated a random string of numbers and letters, and saved the date and time associated with each string. The string was also displayed clearly on the participant’s computer screen (Figure 2 shows an example of a screen shot). The string was shown in the video sample the participant created at the time of the recording. We were able to easily compare the string in the video sample to the string generated in the server database, as well as the date and time when the sample was sent to the server. There was clear, visible evidence of who created each sample and when it was created. These innovations were incorporated and evaluated in a small study that also sought to decrease the cost associated with voucher reinforcement.
Figure 2.
Screenshot of what appeared when a participant logged onto the server. Each time a participant logged in a randomly determined, unique alphanumeric code was displayed on the screen. As verification, the server stored the time of the log in and the randomly generated code to match that shown by the participant in the video.
Methods to decrease cost
The most common concern with abstinence reinforcement is cost (Kirby, Benishek, Leggett, Dugosh, Kerwin, 2006). There are several funding strategies that could be employed to offset costs (Amass and Kamien, 2004; Petry, Martin, Cooney, Kranzler, 2000; Petry, Martin, Simcic, 2005; Silverman, Svikis, Robles, Stitzer, Bigelow, 2001), such as collecting community donations (Amass and Kamien, 2004). Another possibility would be to use a deposit contract model. Under such a model, participants earn back their monetary deposit based on evidence of abstinence. Such a model might be particularly appealing from a public health perspective, as another concern about abstinence reinforcement is that it provides incentives only to those who engage in some problem behavior. In a deposit contract model, participants pay a nominal amount for the opportunity to receive treatment, just like they do for most health care.
There is a long history of using deposit contracting to motivate weight loss, drug and alcohol reductions, and cigarette smoking cessation (Paxton, 1980, 1981, 1983; Winett, 1973). For example, Winett (1973) assessed the effects of reimbursing a $55 deposit for smoking reductions and then abstinence over a relatively brief period (two to four weeks). During a two-week maintenance phase, 24 out of 25 participants (excluding three dropouts) initiated and maintained smoking abstinence during the study. These participants recouped their deposit contingent on self-reported reductions and abstinence, which were also compared to reports by significant others. In contrast, only seven of seventeen in a non-contingent control group maintained abstinence over the same period. After six months, 50% of the participants in the contingent group reported not smoking, compared to 23.5% in the non-contingent group. Although several studies have provided evidence of the feasibility and effectiveness of using monetary deposits to promote cessation, the return of the deposits was typically contingent upon self-reports of smoking abstinence (with corroborations from significant others), rather than biochemical verification of abstinence.
In a small feasibility study, Dallery, Meredith and Glenn (2008) demonstrated that the deposit contract method can be used with abstinence reinforcement. Eight smokers were randomly assigned to a deposit contract ($50) or to a no-deposit group. Participants in the deposit group could recoup their deposit or earn vouchers for smoking reductions and abstinence (breath CO ≤ 4 ppm) during treatment phases. Treatment was delivered via the Internet-based method, as described above. Sixty-five percent of the samples were negative in the deposit group, while 63% of the samples were negative in the no-deposit group (missing samples were considered positive). The total amount distributed in voucher earnings in the deposit and no-deposit groups was $156.90 and $178.50, respectively. However, because $200 was paid to researchers by participants in the deposit group, a $43.10 surplus remained in this group. The surplus was used to supplement experimental costs in the no-deposit group (e.g. vouchers). By assigning individuals to groups after the informed consent process, we attempted to equate the groups in terms of willingness to provide a deposit (and possibly in terms of motivation to quit and financial means).
It is rather striking that despite no clinically meaningful difference in abstinence rates between groups, a small surplus remained in the deposit group after voucher distributions. Thus, use of deposit contracts could result in a more sustainable intervention with potentially substantial (depending on amount of the deposit and amount paid out in abstinence reinforcement) cost-offsets. There are several practical issues that would have to be addressed before a deposit contract method could be promoted to community providers. For instance, it will be necessary to find a balance between the amount of the deposit, treatment acceptability, and treatment effectiveness (Paxton, 1981, 1983). The most cost-effective approach may require larger incentives (Sindelar, Elbel, and Petry, 2007). It would not be desirable, however, if the cost of the treatment unduly discouraged participation for lower income smokers. One solution would be to use a sliding deposit scale, and corresponding earnings rate, based on income. We should emphasize, however, that the $50 deposit used in the feasibility study was less than a typical smoker would pay for cigarettes during the same period in the U.S. (i.e., approximately a three-week supply of cigarettes).
There may be sufficient demand for a deposit contract treatment model to support its widespread use. There is evidence that smokers would pay for an effective treatment (Busch, Falba, Duchovny, Jofre-Bonet, O'Malley, Sindelar, 2004). The authors assessed willingness to pay for new, hypothetical treatment products. Most (84%) smokers reported that they would pay $50 per week for a treatment yielding a “modestly” effective, 50% success rate. The authors concluded that there would be a substantial market for more effective treatments, which could include Internet-based voucher reinforcement therapy. Because an Internet-based therapy has a potentially broad reach at a population level, this could represent a significant addition to the available treatment array and an important public health benefit, whether offered with or without a deposit contract feature. More work is necessary to evaluate the acceptability and effectiveness of a deposit contract.
Methods to increase access
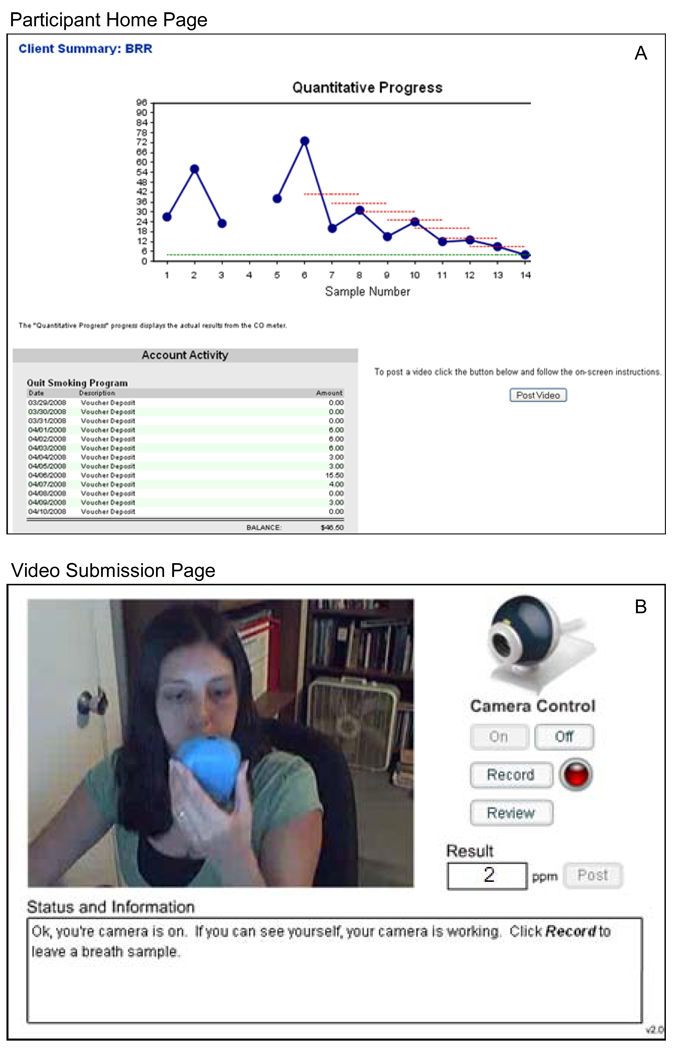
To further increase accessibility of the Internet-based intervention for smokers we recently developed a user-friendly, secure, and encrypted website: Mōtiv8 (Dallery, 2008; Wong, Martin, Dallery, Helmbrecht, Guenthner, Nuzzo, et al., 2008). Participants can login to the website from any computer with Internet access. The participant’s homepage is accessed over a secure, encrypted connection. It consists of a real-time graph of the participant's sample results (showing cumulative smoking abstinence), their earnings history, a box showing messages from the system administrator, a "Post Video" button, and a display showing their previous sample's date/time and the earliest date/time at which they can provide their next sample according to the intervention's required time interval between samples (see panel A in Figure 3).
Figure 3.
The top panel (A) is an example of a participant homepage, displaying the CO quantitative progress at the top, the voucher account balance, and the “Post Video” button. After a video is posted, the button becomes deactivated until the minimum inter-sample interval was met. The bottom panel (B) shows the video submission screen. Instructions for submitting videos appear below the web cam image. Participants are required to input their final CO result in the text box in order to earn a voucher.
When the participant clicks the "Post Video" button the program directs them to the bandwidth selector interface. The participant selects whether they are using a high-speed connection (e.g., DSL, cable modem, or satellite), or a low-speed connection (e.g., dialup over a phone line). Selecting the low-speed connection steps down the bandwidth requirement for the video upload. The video post interface walks the participant through the process of uploading a video sample and posting a result (see panel B in Figure 3). After the video recording, the participant enters the numerical result indicated on the CO meter into a text box. The result is fed into the automated voucher program where it is processed and the appropriate voucher amount, graphs, and cumulative earnings are immediately updated.
Prior to the development of Mōtiv8, participants recorded a video, saved the file to their computer, and then emailed the file to research assistants who verified the video and provided feedback regarding voucher earnings. This approach required measures to ensure the validity of the video file (e.g., initially loaning administratively locked laptops and later developing a server that generated a random alphanumeric string). Although these measures are relatively easy to implement, they would be relatively impractical for widespread dissemination. Furthermore, the method imposed inevitable delays to feedback regarding voucher earnings, ranging anywhere from a few hours to an entire day.
With Mōtiv8, not only is the video file saved directly to the server, making it virtually impossible for the participant to tamper with the authenticity of the video, but the website also provides immediate feedback regarding smoking status and voucher earnings. Indeed, reinforcer immediacy is known to be an important factor in behavior change (Skinner, 1938), and delay to voucher earnings has been shown to influence behavior in analog contingency management interventions (Roll, Reilly, Johanson, 2000). Research personnel are still required to view and verify the submitted videos, which is a simple process. Voucher earnings can be adjusted if a discrepancy exists between the CO value in the video and the value reported by the participant. This video-based method will remain, in all likelihood, an integral feature of any such monitoring program. Simply put, there are no remote methods to verify who is leaving a sample - clinicians must watch the procedure. It should be possible to integrate the CO output directly into the Mōtiv8 software which would obviate the need for user input.
Maintaining abstinence
Internet-based methods could be expanded to address another potential limitation of abstinence reinforcement therapy: maintenance of treatment gains (see Sigmon, Lamb, and Dallery, 2007 for a discussion). A number of participants will inevitably lapse or relapse following the intervention. There are several ways to develop lapse responsive and relapse prevention modifications to the intervention. For example, the study website represents a convenient way to access therapeutic support, either through the use of counselors or peer support. The website could incorporate additional features, such as access to message boards, moderated chat groups, and other smoking resources. Once enrolled, access to these features could be maintained indefinitely. Even the abstinence reinforcement component could be offered if it were integrated with the deposit contract model. For example, lapsers could make a deposit and recoup the deposit based on evidence of abstinence. This would serve as a “commitment response” and provide salient motivation to help them re-establish abstinence. Other methods to maintain abstinence could be considered as well, such as the use intermittent schedules of reinforcement (e.g., Petry, Martin, Cooney, and Kranzler, 2000) and the use of pharmacotherapy.
Applications to special populations
Internet-based abstinence reinforcement can be applied to vulnerable and hard to reach smokers. For example, reaching adolescent smokers has been a particularly challenging, yet critically important, task for cessation programs. Most adult smokers begin smoking during their adolescence (e.g., Chassin, Presson, Rose, and Sherman, 1996; Corby et al., 2000; Jefferis, Graham, Manor, and Power, 2003). Reynolds and associates have applied Internet-based abstinence reinforcement to a small group of adolescent smokers (Reynolds, Dallery, Shroff, Patak, and Leraas; 2008). In several respects, the methods were similar to the study described above (Dallery et al., 2007). It differed in three ways: three breath samples were collected per day instead of two, the CO target criterion was ≤ 5ppm instead of ≤ 7ppm, and cash instead of vouchers was used as the reinforcer (which was accumulated and delivered weekly). Of the possible 360 total CO samples to be collected in the study, 350 were actually obtained (97.2%). Relative to baseline periods, CO levels were substantially reduced during treatment, and in some cases prolonged periods of abstinence were observed. Given the relatively high rate of Internet and related technology use by adolescents, delivering abstinence reinforcement through such media may be particularly appealing and effective.
Another population that may benefit from a remote-based treatment is rural smokers. A disproportionate number of smokers reside in rural areas, where smoking cessation programs may be at considerable distance (Aloise-Young, Wayman, and Edwards, 2002; Epstein, Botvin, and Spoth, 2003). In 2002, current smoking rates in this region were as high as 40%, compared to 23.2% for the United States, and Kentucky has the highest lung cancer mortality rate in the United States: 78.3 per 100,000. This rate is 35% higher than the rate of 58 per 100,000 in the United States. Stoops and colleagues applied Internet-based abstinence reinforcement to smokers in the rural Appalachian region of Kentucky (Stoops, Dallery, Fields, Nuzzo, Schoenberg, Martin, et al., 2009). The retention rate was high, with 85% of participants in this difficult to reach population completing the entire 6-week intervention. Sixty-eight participants were randomly assigned to one of two groups. Those assigned to the experimental group earned vouchers contingent on meeting breath CO cutpoints (CO≤4ppm), and those assigned to the control group received an equivalent amount in vouchers but independent, or non-contingent, of smoking status. Participants in the experimental group submitted three times more negative samples, and were significantly more likely to exhibit sustained periods of abstinence, compared to participants in the control group. Overall, the results suggest that the Internet-based intervention has significant promise with this special population.
Applications to other behavior
Internet-based methodologies can also be used to increase the accessibility and feasibility of contingency management interventions for behavior other than smoking (Kosten, 2007; Carroll and Rounsaville, 2007). For example, contingency management has been used to reinforce adherence to prescription and non-prescription medication protocols, such as the complicated HIV antiretroviral protocol (Rosen, Dieckhaus, McMahon, Valdes, Petry, Cramer, Rounsaville, 2007; Sorenson, Haug, Delucchi, Gruber, Kletter, Batki, Tulskey, Barnett, Hall, 2007) and nicotine replacement therapy for smoking cessation (Hanson, Allen, Jensen, Hatsukami, 2003; Mooney, Babb, Jensen, Hatsukami, 2005). Furthermore, contingency management has also been applied to behavior associated with promoting general health, such as increasing engagement in exercise regimens (Epstein, McKenzie, Valoski, Klein, Wing, 1994; Dapcich-Miura and Hovell, 1979), facilitating adherence with prescribed diets (Epstein et al., 1994; Dapcich-Miura and Hovell, 1979), encouraging behavior necessary to control diabetes (Duvinsky, Jacobs, Foy, 1987; Lowe and Lutzker, 1979), and establishing consistent monitoring of lung capacity by asthmatic children and adolescents (Burkhart, Rayens, Oakley, Abshire, and Zhang, 2007). In many of the studies mentioned, the contingencies were either applied to self-reports (Lowe and Lutzker, 1979; Mooney et al., 2005), by-products of the behavior (e.g., chewed pieces of nicotine gum; Mooney et al., 2005), or continuous monitoring via inpatient housing (Dapcich-Miura and Hovell, 1979; Duvinsky, Jacobs, and Foy, 1987). In a few cases the contingencies were applied to information collected on automated devices that the participant took home (e.g., a pill container that tracked the date and time it was opened, Rosen et al., 2007, Sorenson et al., 2007; an electronic peak flow meter, Burkhart et al., 2007). Although such automated devices offer advantages over self-reports, concerns still exist regarding fidelity because the person who used the device is not observed.
A simple extension of the interventions just described would involve participants creating a video recording while using the automated device or while engaging in the target behavior. For instance, rather than relying on an automated pill dispenser that tracks the date and time that the container was opened, the participant could video record themselves taking the pill at the assigned times. This would be an improvement over the automated pill dispenser; the procedure would verify that the person of interest opened the container and consumed the pill. Not only would incorporating Internet-based technologies increase the fidelity of treatment, it might also increase accessibility and acceptability, as participants would not be required to attend a clinic and would not have to maintain logs or rely on recall for self-reports.
We recently extended the Internet-based monitoring system to improve adherence to blood glucose monitoring recommendations with four teenagers (aged 12–17) diagnosed with Type 1 diabetes (Raiff and Dallery, under review). Blood glucose testing is a critical aspect of effective diabetes management, providing the information necessary to adjust insulin dose, diet and exercise (American Diabetes Association, 2008). Teenagers are supposed to test their blood glucose at least 4–6 times per day (Silverstein et al., 2005). Prior to the Internet-based contingency management intervention, participants in the study tested their blood glucose an average of 1.7 times per day (range 0–4). During the intervention teens could earn $1.00 for every video they submitted showing them test their blood glucose, or showing stored glucose tests if Internet access was not available. Participants could only earn money if they submitted at least 4 videos per day, and they could submit up to 8 videos per day, as long as the tests were separated by at least one hour. During the intervention all participants increased their frequency of testing to an average of 5.7 per day (range 4–8). When the intervention was removed, testing decreased to an average of 3.1 tests per day (range 2–5) suggesting some carry-over effects. This preliminary study shows the feasibility and efficacy of extending Internet-based contingency management procedures to novel populations and problems. More research will be necessary to initiate and maintain long-term adherence to self-management regimens.
Ethical issues in Internet-based contingency management
The use of the Internet poses special ethical considerations regarding treatment accessibility and bias, confidentiality of electronic information, obtaining informed consent, identity verification, and risk assessment. Although Internet-based interventions can reduce the “access gap” by making it available to special populations such as those living in rural environments, it also limits the intervention to those who have Internet access in their homes. This potential for bias of Internet access in the home could be addressed by implementing the intervention in a workplace or other setting such as a library where the Internet could be accessed (e.g., Graham et al., 2007). As Internet use increases, and as Internet capabilities are integrated into cellular phone technology, we expect these inequities will decrease. Also, in countries other than the United States, different inequities certainly exist in Internet access, and these will have to be considered on a case-by-case basis. As in all research studies, the potential for bias should be considered in terms of recruitment procedures, study design, and data interpretation.
Another concern with Internet data collection is ensuring the confidentiality and security of the electronic files. We have taken a number of precautions to ensure the confidentiality and security of electronic information. In particular, electronic information never contained the name of the participant – instead a study username was used and all electronic information was identified by the username. The server was protected from outside intrusion by multiple firewalls. Administrative access to the server only occurred using Secure Shell (SSH), a secure, encrypted protocol for remotely connecting to a machine. Security was periodically monitored using network mapping tools, like nmap which probe machines for vulnerabilities and report the results to the system administrator. A software Port Scan Attack Detector (PSAD) monitored the servers and notified administrators if they came under attack. An Advanced Intrusion Detection Environment (AIDE) detected if any unauthorized changes were made to the machine. Servers were also backed up nightly to external hard drives using an encrypted file system. These precautions did not and would not guarantee security, and researcher should enlist all tools to minimize the risks associated with a breach of data-security, and participants should be informed about the potential risks of electronic data collection.
Internet-based research may pose special problems for obtaining informed consent and ensuring the identity and age of participants (Kraut et al., 2004). The studies described in this review involved in-person consent, therefore verification of participants’ identity and age was obtained via driver’s license or comparable identification card. However, future studies may be conducted entirely online and will require additional measures. A video-based consent process could take place, using video conferencing sites such as Skype or Google Chat, where participants can be given the opportunity to ask questions based on the consent form before signing and faxing the form, as well as show their drivers licenses to the camera for age and identity verification. In some cases it might be possible to waive the written signature for informed consent. In this case, participants could provide informed consent online by clicking a button agreeing to the terms of the study. It may be necessary to take additional steps to ensure that participants understand the consent form, such as including a brief quiz (Kraut et al., 2004).
Finally, risk assessment may be more difficult when experiments are conducted remotely rather than in person (Kraut et al., 2004). If an adverse event related to the experiment arises, researchers may not be aware of it because of limited contact between the researcher and participant. Participants should receive clear instructions on how to contact research staff if an adverse event should arise. Additional steps should be considered by researchers to increase the likelihood that such information is obtained. For instance, participants could be queried periodically about the occurrence of adverse events while they are in the study.
Using the Internet to conduct research and implement treatment interventions requires special ethical considerations like those described in this section; however, the present discussion is far from exhaustive. When conducting such research there may be additional concerns specific to the study design that warrant consideration, and these issues and steps to minimize risk should be discussed and approved by the researcher’s Institutional Review Board or other regulatory agency.
Conclusion
The Internet provides unprecedented reach, convenience, and accessibility. Although disparities still exist in access to Internet-based health care, there is some evidence that the “access gap” can be reduced through Internet based methods (McDaniel and Stratton, 2006). The developments discussed in this paper address the majority of limitations (cost, dissemination, sustainability) inherent in traditional abstinence reinforcement interventions. Other technologies could further increase accessibility to abstinence reinforcement treatment, such as cellular phones or pocket PCs. Admittedly, much of the work described in this paper is still in its infancy, and more research is necessary before we can evaluate the cost effectiveness of the intervention. Nevertheless, technological innovations hold considerable promise as a way to increase the accessibility and effectiveness of abstinence reinforcement for smoking cessation and other health-related behavior.
Footnotes
When applied to smoking, the goal of such behavioral interventions is abstinence from smoking. It may be possible, however, to apply contingency management to reduce the frequency and/or intensity of some target behavior (e.g., alcohol use). As such, contingency management could be used as a harm reduction strategy (Kellogg & Kreek 2005).
References
- Ahijevych KL, Tyndale RF, Dhatt RK, Weed HG, Browning KK. Factors influencing cotinine half-life in African American and Caucasian women. Nicotine and Tobacco Research. 2002;4:423–431. doi: 10.1080/1462220021000018452. [DOI] [PubMed] [Google Scholar]
- Ahluwalia JS, Harris KJ, Catley D, Okuyemi KS, Mayo MS. Sustained release bupropion for smoking cessation in african Americans. Journal of the American Medical Association. 2002;288:468–474. doi: 10.1001/jama.288.4.468. [DOI] [PubMed] [Google Scholar]
- Alessi SM, Badger GJ, Higgins ST. An experimental examination of the initial weeks of abstinence in cigarette smokers. Experimental and Clinical Psychopharmacology. 2004;12:276–287. doi: 10.1037/1064-1297.12.4.276. [DOI] [PubMed] [Google Scholar]
- Aloise-Young PA, Wayman JC, Edwards RW. Prevalence of cigarette smoking among rural adolescents in the United States. Substance Use and Misuse. 2002;37:613–630. doi: 10.1081/ja-120004276. [DOI] [PubMed] [Google Scholar]
- Amass L, Kamien J. A Tale of Two Cities: Financing Two Voucher Programs for Substance Abusers Through Community Donations. Experimental and Clinical Psychopharmacology. 2004;12:147–155. doi: 10.1037/1064-1297.12.2.147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Diabetes Association. Diabetes Care, 31(suppl_1) 2008. Standards of Medical Care in Diabetes--2008; pp. S12–S54. [DOI] [PubMed] [Google Scholar]
- Burkhart PV, Rayens MK, Oakley MG, Abshire DA, Zhang M. Testing an intervention to promote children's adherence to asthma self-management. Journal of Nursing Scholarship: An Official Publication of Sigma Theta Tau International Honor Society of Nursing / Sigma Theta Tau. 2007;39:133–140. doi: 10.1111/j.1547-5069.2007.00158.x. [DOI] [PubMed] [Google Scholar]
- Busch SH, Falba TA, Duchovny N, Jofre-Bonet M, O'Malley SS, Sindelar JL. Value to smokers of improved cessation products: Evidence from a willingness-to-pay survey. Nicotine and Tobacco Research. 2004;6:631–639. doi: 10.1080/14622200410001727885. [DOI] [PubMed] [Google Scholar]
- Carroll KM, Rounsaville BJ. A perfect platform: combining contingency management with medications for drug abuse. The American Journal of Drug and Alcohol Abuse. 2007;33:343–365. doi: 10.1080/00952990701301319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control. Annual smoking-attributable mortality, years of potential life lost, and economic costs—United States 2000–2004. Morbidity and Mortality Weekly Report. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Chassin L, Presson CC, Rose JS, Sherman SJ. The natural history of cigarette smoking from adolescence to adulthood: demographic predictors of continuity and change. Health Psychology: Official Journal of the Division of Health Psychology, American Psychological Association. 1996;15:478–484. doi: 10.1037//0278-6133.15.6.478. [DOI] [PubMed] [Google Scholar]
- Cobb NK, Graham AL. Characterizing Internet searchers of smoking cessation information. Journal of Medical Internet Research. 2006;8 doi: 10.2196/jmir.8.3.e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cobb NK, Graham AL, Bock BC, Papandonatos G, Abrams DB. Initial evaluation of a real-world Internet smoking cessation system. Nicotine Tobacco Research. 2005;7:207–216. doi: 10.1080/14622200500055319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corby EA, Rolly JM, Ledgerwood DM, Schuster CR. Contingency management interventions for treating the substance abuse of adolescents: A feasibility study. Experimental and Clinical Psychopharmacology. 2000;8:371–376. doi: 10.1037//1064-1297.8.3.371. [DOI] [PubMed] [Google Scholar]
- Crowely TJ, MacDonald MJ, Zerbe GO, Petty TL. Reinforcing breath carbon monoxide reductions in chronic obstructive pulmonary disease. Drug and Alcohol Dependence. 1991;29:47–62. doi: 10.1016/0376-8716(91)90021-p. [DOI] [PubMed] [Google Scholar]
- Dallery J. Technological innovations in behavioral treatments for cigarette smoking; Symposium presentation at the College on Problems of Drug Dependence in Puerto Rico; 2008. [Google Scholar]
- Dallery J, Glenn IM. Effects of an Internet-based voucher reinforcement program for smoking abstinence: a feasibility study. Journal of Applied Behavior Analysis. 2005;38:349–357. doi: 10.1901/jaba.2005.150-04. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dallery J, Glenn IM, Raiff BR. An Internet-based abstinence reinforcement treatment for cigarette smoking. Drug and Alcohol Dependence. 2007;86:230–238. doi: 10.1016/j.drugalcdep.2006.06.013. [DOI] [PubMed] [Google Scholar]
- Dallery J, Meredith S, Glenn I. A deposit contract method to deliver abstinence reinforcement for cigarette smoking. Journal of Applied Behavior Analysis. 2008;41:609–615. doi: 10.1901/jaba.2008.41-609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dapcich-Miura E, Hovell MF. Contingency management of adherence to a complex medical regimen in an elderly heart patient. Behavior Therapy. 1979;10:193–201. [Google Scholar]
- Duvinsky JD, Jacobs HE, Foy DW. Contingency management of food misbehavior in a psychiatric patient with diabetes. Journal of Behavior Therapy and Experimental Psychiatry. 1987;18:179–183. doi: 10.1016/0005-7916(87)90033-4. [DOI] [PubMed] [Google Scholar]
- Eisenberg T, Stitzer ML, Henningfield JE. Current issues in nicotine replacement. In: Seidman DF, Covey LS, editors. Helping the Hard-Core Smoker: A Clinician’s Guide. Mahwah, NJ: Lawrence Erlbaum Associates; 1999. [Google Scholar]
- Epstein JA, Botvin GJ, Spoth R. Predicting smoking among rural adolescents: social and cognitive processes. Nicotine and Tobacco Research: Official Journal of the Society for Research on Nicotine and Tobacco. 2003;5:485–491. doi: 10.1080/1462220031000118577. [DOI] [PubMed] [Google Scholar]
- Epstein LH, McKenzie SJ, Valoski A, Klein KR, Wing RR. Effects of mastery criteria and contingent reinforcement for family-based child weight control. Addictive Behaviors. 1994;19:135–145. doi: 10.1016/0306-4603(94)90038-8. [DOI] [PubMed] [Google Scholar]
- Etter J. Internet-based smoking cessation programs. International Journal of Medical Informatics. 2006;75:110–116. doi: 10.1016/j.ijmedinf.2005.06.014. [DOI] [PubMed] [Google Scholar]
- Fagerstrom KO, Kunze M, Schoberberger R, Breslau N, Hughes JR, Hurt RD, Puska P, Ramström L, Zatoński W. Nicotine dependence versus smoking prevalence: comparisons among countries and categories of smokers. Tobacco Control. 1996;5:52–56. doi: 10.1136/tc.5.1.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fiore MC, Smith SS, Jorenby DE, Baker TB. The effectiveness of nicotine patch for smoking cessation: A meta-analysis. Journal of the American Medical Association. 1994;271:1940–1947. [PubMed] [Google Scholar]
- Galbicka G. Shaping in the 21st century: Moving percentile schedules into applied settings. Journal of Applied Behavior Analysis. 1994;27:739–760. doi: 10.1901/jaba.1994.27-739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garvey AJ, Bliss RE, Hitchcock JL, Heinold JW, Rosner B. Predictors of smoking relapse among self-quitters: A report from the Normative Aging Study. Addictive Behaviors. 1992;17:367–377. doi: 10.1016/0306-4603(92)90042-t. [DOI] [PubMed] [Google Scholar]
- Glenn IM, Dallery J. Effects of Internet-based voucher reinforcement and a transdermalnicotine patch on cigarette smoking. Journal of Applied Behavior Analysis. 2007;40:1–13. doi: 10.1901/jaba.2007.40-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gourlay SG, Forbes A, Marriner T, Pethica D, McNeil JJ. Prospective study of factors predicting outcome of transdermal nicotine treatment in smoking cessation. British Medical Journal. 1994;309:842–846. doi: 10.1136/bmj.309.6958.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham AL, Cobb NK, Raymond L, Sill S, Young J. Effectiveness of an Internet-based worksite smoking cessation intervention at 12 months. Journal of Occupational and Environmental Medicine. 2007;49:821–828. doi: 10.1097/JOM.0b013e3180d09e6f. [DOI] [PubMed] [Google Scholar]
- Hanson K, Allen S, Jensen S, Hatsukami D. Treatment of adolescent smokers with the nicotine patch. Nicotine and Tobacco Research. 2003;5:515–526. doi: 10.1080/14622200307243. [DOI] [PubMed] [Google Scholar]
- Heil SH, Alessi SM, Plebani J, Badger GJ, Higgins ST. An experimental test of the influence of prior cigarette smoking abstinence on future abstinence. Nicotine and Tobacco Research. 2004;6:471–479. doi: 10.1080/14622200410001696619. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Budney AJ, Bickel WK, Foerg F, Donham, Badger MS. Incentives improve outcome in outpatient behavioral treatment of cocaine dependence. Archives of General Psychiatry. 1994;51:568–576. doi: 10.1001/archpsyc.1994.03950070060011. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Dumeer AM, Thomas CS, Solomon LJ, Bernstein IM. Smoking status in the initial weeks of quitting as a predictor of smoking-cessation outcomes in pregnant women. Drug and Alcohol Dependence. 2006;85:138–141. doi: 10.1016/j.drugalcdep.2006.04.005. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Heil SH, Solomon LJ, Bernstein IM, Lussier JP, Abel RL, Lynch ME, Badger GJ. A pilot study on voucher-based incentives to promote abstinence from cigarette smoking during pregnancy and postpartum. Nicotine and Tobacco Research. 2004;6:1015–1120. doi: 10.1080/14622200412331324910. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Gulliver SB, Fenwick JW, Valliere WA, Cruser K, Pepper S, Shea P, Solomon LJ, Flynn BS. Smoking cessation among self-quitters. Health Psychology. 1992;11:331–334. doi: 10.1037//0278-6133.11.5.331. [DOI] [PubMed] [Google Scholar]
- Hughes JR, Keely JP, Niaura RS, Ossip-Klein DJ, Richmond RL, Swan GE. Measures of abstinence in clinical trials: issues and recommendations. Nicotine and Tobacco Research. 2003;5:13–25. [PubMed] [Google Scholar]
- Hurt RD, Sachs DPL, Glover ED, Offord KP, Johnston JA, Dale LC, Khayrallah MA, Schroeder DR, Glover PN, Sullivan CR, Croghan IT, Sullivan PM. A comparison of sustained-release bupropion and placebo for smoking cessation. New England Journal of Medicine. 1997;17:1195–1202. doi: 10.1056/NEJM199710233371703. [DOI] [PubMed] [Google Scholar]
- Internet World Stats: Usage and Population Statistics. United States of America Internet Usage and Broadband Usage Report. Website: http://www.internetworldstats.com/am/us.htm.
- Jacob P, Hatsukami D, Severson H, Hall S, Yu L, Benowitz NL. Anabasine and anatabine as biomarkers for tobacco use during nicotine replacement therapy. Cancer Epidemiology, Biomarkers and Prevention. 2002;11:1668–1673. [PubMed] [Google Scholar]
- Javors MA, Hatch JP, Lamb RJ. Cut-off levels for breath carbon monoxide as a marker for cigarette smoking. Addiction. 2005;100:159–167. doi: 10.1111/j.1360-0443.2004.00957.x. [DOI] [PubMed] [Google Scholar]
- Jefferis B, Graham H, Manor O, Power C. Cigarette consumption and socio-economic circumstances in adolescence as predictors of adult smoking. Addiction. 2003;98:1765–1772. doi: 10.1111/j.1360-0443.2003.00552.x. [DOI] [PubMed] [Google Scholar]
- Kellogg SH, Kreek MJ. Gradualism, identity, reinforcements, and change. International Journal of Drug Policy. 2005;16:369–375. [Google Scholar]
- Kenford SL, Fiore MC, Jorenby DE, Smith SS, Wetter D, Baker TB. Predicting smoking cessation, who will quit with and without the nicotine patch. Journal of the American Medical Association. 1994;271:589–594. doi: 10.1001/jama.271.8.589. [DOI] [PubMed] [Google Scholar]
- Kirby KC, Benishek LA, Leggett Dugosh K, Kerwin ME. Substance abuse treatment providers’ beliefs and objections regarding contingency management: Implications for dissemination. Drug and Alcohol Dependence. 2006;85:19–27. doi: 10.1016/j.drugalcdep.2006.03.010. [DOI] [PubMed] [Google Scholar]
- Kosten TR. Pharmacotherapy for addictions: partnering with contingency management. The American Journal of Drug and Alcohol Abuse. 2007;33:341–342. doi: 10.1080/00952990701312415. [DOI] [PubMed] [Google Scholar]
- Kraut R, Olsen J, Banaji M, Bruckman A, Cohen J, Couper M. Psychological research online: report of board scientific affairs’ advisory group on the conduct of research on the Internet. American Psychologist. 2004;59:105–117. doi: 10.1037/0003-066X.59.2.105. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Kirby KC, Morral AR, Galbicka G, Iguchi MY. Improving contingency management programs for addiction. Addictive Behaviors. 2004;29:507–523. doi: 10.1016/j.addbeh.2003.08.021. [DOI] [PubMed] [Google Scholar]
- Lamb RJ, Morral AR, Galbicka G, Kirby KC, Iguchi MY. Shaping Reduced Smoking in Smokers Without Cessation Plans. Experimental and Clinical Psychopharmacology. 2005;13:83–92. doi: 10.1037/1064-1297.13.2.83. [DOI] [PubMed] [Google Scholar]
- Lowe K, Lutzker JR. Increasing compliance to a medical regimen with a juvenile diabetic. Behavior Therapy. 1979;10:57–64. [Google Scholar]
- Mallen MJ, Blalock JA, Cinciripini PM. Using technology to serve patients and practitioners: a comprehensive tobacco-cessation program for cancer patients. Counseling and Psychotherapy Research. 2006;6:196–201. [Google Scholar]
- McDaniel AM, Stratton RM. Internet-Based Smoking Cessation Initiatives: Availability, Varieties, and Likely Effects on Outcomes. Disease Management and Health Outcomes. 2006;14:275–285. [Google Scholar]
- Middleton ET, Morice AH. Breath carbon monoxide as an indication of smoking habit. Chest. 2000;117 doi: 10.1378/chest.117.3.758. 758-163. [DOI] [PubMed] [Google Scholar]
- Mooney M, Babb D, Jensen J, Hatsukami D. Interventions to increase use of nicotine gum: A randomized, controlled, single-blind trial. Nicotine and Tobacco Research. 2005;7:565–579. doi: 10.1080/14622200500185637. [DOI] [PubMed] [Google Scholar]
- Parker DR, Lasater TM, Windsor R, Wilkins J, Upegui DI, Heimdal J. The accuracy of self-reported smoking status assessed by cotinine test strips. Nicotine and Tobacco Research. 2002;4:305–309. doi: 10.1080/14622200210142715. [DOI] [PubMed] [Google Scholar]
- Paxton R. The effects of a deposit contract as a component in a behavioral programme for stopping smoking. Behavior Research and Therapy. 1980;18:45–50. doi: 10.1016/0005-7967(80)90068-6. [DOI] [PubMed] [Google Scholar]
- Paxton R. Deposit contracts with smokers: varying frequency and amount of repayments. Behavior Research and Therapy. 1981;19:117–123. doi: 10.1016/0005-7967(81)90035-8. [DOI] [PubMed] [Google Scholar]
- Paxton R. Prolonging the effect of deposit contracts with smokers. Behavior Research and Therapy. 1983;21:425–433. doi: 10.1016/0005-7967(83)90012-8. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Cooney JL, Kranzler HR. Give them prizes, and they will come: Contingency management for treatment of alcohol dependence. Journal of Consulting and Clinical Psychology. 2000;68:250–257. doi: 10.1037//0022-006x.68.2.250. [DOI] [PubMed] [Google Scholar]
- Petry NM, Martin B, Simcic F., Jr Prize Reinforcement Contingency Management for Cocaine Dependence: Integration With Group Therapy in a Methadone Clinic. Journal of Consulting and Clinical Psychology. 2005;73:354–359. doi: 10.1037/0022-006X.73.2.354. [DOI] [PubMed] [Google Scholar]
- Raiff BR, Dallery J. Internet-based contingency management to increase blood-glucose testing in adolescents diagnosed with Type 1 diabetes. Journal of Applied Behavior Analysis. doi: 10.1901/jaba.2010.43-487. (under review) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rand CS, Stitzer ML, Bigelow GE, Mead AM. The effects of contingent payment and frequent workplace monitoring on smoking abstinence. Addictive Behaviors. 1989;14:121–128. doi: 10.1016/0306-4603(89)90041-5. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Dallery J, Shroff P, Patak M, Leraas K. A web-based contingency management program with adolescent smokers. Journal of Applied Behavior Analysis. doi: 10.1901/jaba.2008.41-597. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Higgins ST. A within-subject comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Drug and Alcohol Dependence. 2000;58:103–109. doi: 10.1016/s0376-8716(99)00073-3. [DOI] [PubMed] [Google Scholar]
- Roll JM, Higgins ST, Badger GJ. An experimental comparison of three different schedules of reinforcement of drug abstinence using cigarette smoking as an exemplar. Journal of Applied Behavior Analysis. 1996;29:495–505. doi: 10.1901/jaba.1996.29-495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roll JM, Reilly MP, Johanson C. The influence of exchange delays on cigarette versus money choice: A laboratory analog of voucher-based reinforcement therapy. Experimental and Clinical Psychopharmacology. 2000;8:366–370. doi: 10.1037//1064-1297.8.3.366. [DOI] [PubMed] [Google Scholar]
- Rosen MI, Dieckhaus K, McMahon TJ, Valdes B, Petry NM, Cramer J, Rounsaville MD. Improved adherence with contingency management. AIDS patient care and STDs. 2007;21:30–40. doi: 10.1089/apc.2006.0028. [DOI] [PubMed] [Google Scholar]
- Schuh KJ, Stitzer ML. Desire to smoke during spaced intervals. Psychopharmacology. 1995;120:289–295. doi: 10.1007/BF02311176. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Ferguson SG, Gwaltney CJ, Balabanis MH, Shadel WG. Reduction of abstinence-induced withdrawal and craving using high-dose nicotine replacement therapy. Psychopharmacology. 2006;184:637–644. doi: 10.1007/s00213-005-0184-3. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Jarvik ME, Ling W, Rawson RA. Contingency management for tobacco smoking in methadone-maintained opiate addicts. Addictive Behavior. 1996;21:409–412. doi: 10.1016/0306-4603(95)00066-6. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Rotheram-Fuller E, Yang X, Frosch D, Nahom D, Jarvick ME, Rawson RA, Ling W. Smoking cessation in methadone maintenance. Addiction. 2002;97:1317–1328. doi: 10.1046/j.1360-0443.2002.00221.x. [DOI] [PubMed] [Google Scholar]
- Sigmon SC, Lamb RJ, Dallery J. Tobacco. In: Higgins ST, Silverman K, Heil SH, editors. Contingency management in substance abuse treatment. New York: The Guilford Press; 2008. [Google Scholar]
- Silverman K, Higgins ST, Brooner RK, Montoya ID, Cone EJ, Schuster CR, Preston KL. Sustained cocaine abstinence in methadone maintenance patients through voucher-based reinforcement therapy. Archives of General Psychiatry. 1996;53:409–415. doi: 10.1001/archpsyc.1996.01830050045007. [DOI] [PubMed] [Google Scholar]
- Silverman K, Svikis D, Robles E, Stitzer ML, Bigelow GE. A reinforcement-based therapeutic workplace for the treatment of drug abuse: Six-month abstinence outcomes. Experimental and Clinical Psychopharmacology. 2001;9:14–23. doi: 10.1037/1064-1297.9.1.14. [DOI] [PubMed] [Google Scholar]
- Silverman K, Wong CJ, Umbricht-Schneiter A, Montoya ID, Schuster CR, Preston KL. Broad beneficial effects of reinforcement for cocaine abstinence in methadone patients. Journal of Consulting and Clinical Psychology. 1998;66:811–824. doi: 10.1037//0022-006x.66.5.811. [DOI] [PubMed] [Google Scholar]
- Silverstein J, Klingensmith G, Copeland K, Plotnick L, Kaufman F, Laffel L, et al. Care of children and adolescents with type 1 diabetes: a statement of the American Diabetes Association. Diabetes Care. 2005;28:186–212. doi: 10.2337/diacare.28.1.186. [DOI] [PubMed] [Google Scholar]
- Skinner BF. The behavior of organisms. New York: Appleton-Century-Crofts; 1938. [Google Scholar]
- Sorensen JL, Haug NA, Delucchi KL, Gruber V, Kletter E, Batki SL, Tulskey JP, Barnett P, Hall S. Voucher reinforcement improves medication adherence in HIV-positive methadone patients: A randomized trial. Drug and Alcohol Dependence. 2007;88:54–63. doi: 10.1016/j.drugalcdep.2006.09.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sindelar J, Elbel B, Petry NM. What do we get for our money? Cost-effectiveness of adding contingency management. Addiction. 2007;102:309–316. doi: 10.1111/j.1360-0443.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- Stitzer ML. Combined behavioral and pharmacological treatments for smoking cessation. Nicotine and Tobacco Research. 1999;1:S181–S187. doi: 10.1080/14622299050012041. [DOI] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE. Contingent reinforcement for carbon monoxide reduction: Within-subject effects of pay amount. Journal of Applied Behavior Analysis. 1984;17:477–483. doi: 10.1901/jaba.1984.17-477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stitzer ML, Bigelow GE. Contingent reinforcement for reduced breath carbon monoxide levels: Target specific effects on cigarettes smoking. Addictive Behaviors. 1985;10:345–349. doi: 10.1016/0306-4603(85)90030-9. [DOI] [PubMed] [Google Scholar]
- Stoddard JL, Delucchi KL, Muñoz RF, Collins NM, Pérez EJ, Augustson E, Lenert LL. Smoking cessation research via the Internet: a feasibility study. Journal of Health Communication. 2005;10:27–41. doi: 10.1080/10810730590904562. [DOI] [PubMed] [Google Scholar]
- Stoops WW, Dallery J, Fields NM, Nuzzo P, Schoenberg NE, Martin C, Casey B, Wong C. An Internet-Based Abstinence Reinforcement Smoking Cessation Intervention in Rural Smokers. Drug and Alcohol Dependence. 2009 doi: 10.1016/j.drugalcdep.2009.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tidey JW, O’Neill S, Higgins ST. Contingent monetary reinforcement of smoking reductions, with and without transdermal nicotine, in outpatients with schizophrenia. Experimental and Clinical Psychopharmacology. 2002;10:241–247. doi: 10.1037//1064-1297.10.3.241. [DOI] [PubMed] [Google Scholar]
- Walters ST, Wright JA, Shegog R. A review of computer and Internet-based interventions for smoking behavior. Addictive Behaviors. 2006;31:264–277. doi: 10.1016/j.addbeh.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Winett RA. Parameters of deposit contracts in the modification of smoking. The Psychological Record. 1973;23:49–60. [Google Scholar]
- Wiseman Eve J, Williams DK, McMillan DE. Effectiveness of Payment for Reduced Carbon Monoxide Levels and Noncontingent Payments on Smoking Behaviors in Cocaine-Abusing Outpatients Wearing Nicotine or Placebo Patches. Experimental and Clinical Psychopharmacology. 2005;13:102–110. doi: 10.1037/1064-1297.13.2.102. [DOI] [PubMed] [Google Scholar]
- Wong CJ, Martin CA, Dallery J, Helmbrecht T, Guenthner G, Nuzzo PA, Grabinski M, Kelly TH. Poster presentation at the College on Problems of Drug Dependence; San Juan, Puerto Rico: 2008. [Google Scholar]
- Woodruff SI, Edwards CC, Conway TL, Elliot SP. Pilot test of an Internet virtual world chat room for rural teen smokers. Journal of Adolescent Health. 2001;29:239–243. doi: 10.1016/s1054-139x(01)00262-2. [DOI] [PubMed] [Google Scholar]
- Yudkin PL, Jones L, Lancaster T, Fowler GH. Which smokers are helped to give up smoking using transdermal nicotine patches? Results from a randomized, double-blind, placebo-controlled trial. British Journal of General Practice. 1996;46:145–148. [PMC free article] [PubMed] [Google Scholar]