Abstract
Affordable and effective antiretroviral therapy (ART) adherence interventions are needed for many patients to promote positive treatment outcomes and prevent viral resistance. We conducted a two-arm randomized trial (n = 40 men and women receiving and less than 95% adherent to ART) to test a single office session followed by four biweekly cell phone counseling sessions that were grounded in behavioral self-management model of medication adherence using data from phone-based unannounced pill counts to provide feedback-guided adherence strategies. The control condition received usual care and matched office and cell phone/pill count contacts. Participants were baseline assessed and followed with biweekly unannounced pill counts and 4-month from baseline computerized interviews (39/40 retained). Results showed that the self-regulation counseling delivered by cell phone demonstrated significant improvements in adherence compared to the control condition; adherence improved from 87% of pills taken at baseline to 94% adherence 4 months after baseline, p < 0.01. The observed effect sizes ranged from moderate (d = 0.45) to large (d = 0.80). Gains in adherence were paralleled with increased self-efficacy (p < 0.05) and use of behavioral strategies for ART adherence (p < 0.05). We conclude that the outcomes from this test of concept trial warrant further research on cell phone-delivered self-regulation counseling in a larger and more rigorous trial.
Introduction
Combination HIV treatments have dramatically reduced viral burden, improved the health and quality of life of people living with HIV/AIDS, and contribute directly to significant declines in HIV-related mortality.1 HIV infection is successfully managed by antiretroviral therapy, but only when patients adhere to their medications. Unfortunately, not everyone who is prescribed antiretroviral therapies (ART) experiences the potential benefits of these medications.2,3 Significant numbers of patients receiving ART in both developed and developing countries have incomplete viral suppression and suboptimal clinical outcomes.4 Many people living with HIV/AIDS therefore require greater adherence monitoring and assistance than is possible with routine clinic visits. In addition, there is evidence that patients who live in impoverished urban and rural areas have fewer clinical contacts and are in even greater need of adherence assistance.5
Although ART regimens vary in how much adherence is necessary to sustain viral suppression. Earlier treatment regimens required nearly perfect adherence, with viral breakthrough possible with less than 95% adherence.3,6 However, advances in ART have brought more forgiving regimens, which often remain viral suppressive when adherence is as low as 85% of doses taken.7,8 There is general agreement that patients should nevertheless be told to take every dose of their medications and that adherence of less than 90% of doses taken should prompt corrective intervention. Current adherence interventions are typically delayed in their response to nonadherence, often intervening too late to avert treatment resistance.3,8 Adherence interventions require a more proactive stance that corrects nonadherence within a window of opportunity between missed doses and treatment resistance.9
Factors that contribute to incomplete HIV treatment adherence tend to be amenable to intervention, such as forgetting, depression, side effects, and substance use. Lapses between prescription refills are also a common source of nonadherence and render considerable risk for viral resistance. Parienti et al.9 showed that the risk for viral resistance for some of the most common drug combinations reaches 50% when treatment interruptions are sustained 16 days. This narrow window for detecting and correcting nonadherence often falls outside of usual care appointments and requires monitoring of patient adherence with rapid response to correct course and resume adherent behavior.10,11
Advances in telecommunications offer new opportunities to avoid drug resistance by assisting patients closer in time to when they are experiencing lapses in adherence. Unlike office-based counseling, cell phone counseling can reach patients in remote places as well as difficult to reach urban populations. Cell phone counseling can be conducted with flexible scheduling such that counseling can occur at the convenience of the patient. Indeed, patients who miss clinic appointments may be in most need of adherence interventions. The costs of missed clinic appointments are eliminated when counselors do not need to reschedule appointments and can simply contact another patient in the same time slot. Services delivered on the phone can also afford opportunities for immediate intervention and referral. Cell phones are nearly universal in the United States and other developed nations, with wide-scale and increasing use in developing countries; 93% of the U.S. population subscribes to cell phone service.12
The current study was an initial test of concept of an adherence intervention designed to reach patients by cell phone and sustain adherence between routine care visits. Previous research has shown that health behavior counseling can be delivered effectively over the phone.13–15 Cell phones offer an accessible, affordable and scalable platform for delivering health behavior interventions. For example, a recent cell phone delivered intervention in Kenya consisted of weekly text messaging between clinicians and patients, where the clinicians initiated contact by asking how the patient was doing and patients responded whether they needed assistance. The intervention demonstrated significant improvements in self-reported adherence to HIV treatment and reductions in HIV viral load.16 Phone-delivered voice service counseling interventions have also demonstrated promising outcomes. For example, Reynolds et al.17 tested a 16-week telephone-delivered medication adherence counseling intervention aimed at improving HIV treatment adherence. The intervention was based on principles of behavioral self-management, where missed doses were reported by the participant to the counselor who discussed and problem solved the circumstances of nonadherence. Reynolds et al.17 found that telephone support counseling resulted in significantly greater self-reported treatment adherence over a 16-month observation period compared to a standard of care control condition. The telephone adherence counseling also improved virologic response.
The current study examined the effects of a brief cell phone-delivered adherence intervention designed to improve medication adherence in people living with HIV/AIDS. The intervention uses unannounced pill counts conducted via cell phones to monitor medication adherence and intervene proximal to missed doses to improve adherence. Unannounced pill counts conducted in people's homes as well as on the phone have proven reliable and valid for monitoring medication adherence.18–20 To our knowledge, this study is the first to test the concept of using unannounced pill counts as part of a medication adherence improvement intervention. We hypothesized that participants randomized to the experimental self-management counseling intervention would demonstrate greater treatment adherence than those who receive a contact-matched control condition.
Methods
Participants and setting
Participants were 26 men and 14 women recruited from infectious disease clinics in Atlanta, Georgia. Enrollment occurred between May 2010 and July 2010, and follow-ups were completed November 2010. Atlanta has one of the fastest growing HIV epidemics in the United States,21 with over 23,000 reported cases of AIDS and an HIV/AIDS rate of 23 per 100,000 population, exceeding the average 15 per 100,000 population in other major U.S. cities. Participants were screened as part of a community survey study and invited to participate if they met the study entry criteria: age 18 or older, receiving ART, and self-reported less than 95% adherent in the past month using a validated visual analogue adherence scale.22,23 We used 95% adherence for study entry because self-report measures tend to overestimate adherence and a high level of adherence would reduce false-negatives. All study protocols were approved by the University of Connecticut Institutional Review Board.
Randomization and blinding
Following informed consent, baseline assessments and training in cell phone operations and pill counting procedures, participants were randomly assigned to conditions. Allocation was accomplished by using a computer generated simple randomization scheme. Randomization was not breached throughout the trial. Recruitment, screening, and office-based assessment staff remained blinded to condition throughout the study and the adherence counselor never conducted outcome assessments.
Overview of study design
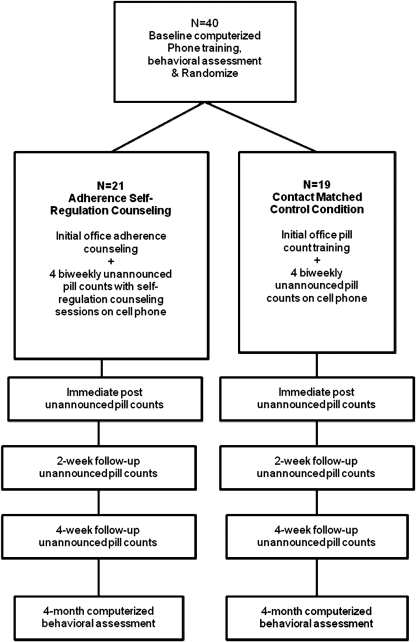
Figure 1 illustrates the randomized study design and flow of participants through the trial. During the initial study visit, all participants completed informed consent and a behavioral interview administered by audio-computer assisted structured interview (ACASI). Participants provided their most recent physician-certified viral load and CD4 counts abstracted from clinical records. Participants were also trained in the operations of their study cell phone and in procedures for conducting unannounced pill counts. Within 1 week of the initial office appointment participants received their first unannounced pill count. All participants received four additional biweekly calls during which their pills were counted. Participants randomized to the experimental counseling condition received 45-min counseling sessions that were initiated on the same calls after the pill counts. Adherence obtained from the pill counts was used as feedback for self-regulation counseling. In contrast, participants in the time-yoked control condition counted their pills but did not receive feedback on their adherence or counseling. We used the pill count obtained in the final counseling session as well as the control pill count to measure immediate-post counseling adherence. After the final counseling session, all unannounced follow-up pill counts for both conditions were conducted by the phone assessor. Two additional biweekly pill counts occurred in the 4 weeks following the counseling/matched contact period. Finally, participants returned to the research office to complete a second ACASI assessment 4 months after baseline, which was 2 months after the final counseling session/matched control condition.
FIG. 1.
Flow of participants through the randomized clinical trial.
Intervention conditions
Behavioral self-regulation counseling
The experimental adherence counseling in this study was based on self-regulation models of medication adherence.17,24 The models explain medication adherence from the patient's perspective and personal experiences. Self-regulation models posit that adherence is directly influenced by illness experiences (e.g., symptoms, medication side effects), social interactions, sources of information, and cognitive/affective processes. These models suggest the content of adherence interventions should directly address adherence factors by providing accurate information, building behavioral skills, and providing affective support. For example, medication-related beliefs and affective responses to medications can interfere with adherence. Based on self-regulation models, our cell phone intervention was framed around corrective feedback guided behavioral self-regulation counseling for medication adherence. The intervention was delivered by an adherence counselor using resources that mirror those typically available in routine clinical services.25
The initial counseling session was conducted in a 45-min face-to-face office visit with an adherence counselor. In session 1, the counselor explained the goals of pill count monitoring and self-regulation counseling. The session included information on how HIV impacts the immune system and how antiretroviral medications slow the progression of HIV disease. Considerable emphasis was placed on how changes in CD4 cells and viral load are related to health and can be affected by medications. The concept of resistance was covered in practical terms, emphasizing the potential for HIV to become treatment resistant. The counselor also conducted a behavioral assessment to formulate a personalized adherence plan. Participants worked with the counselor to identify barriers to taking medications, such as side effects, forgetting doses, sleeping through doses, substance use, mood, and barriers to reaching the pharmacy. The participant discussed their antiretroviral medications, one by one, identifying the medications and creating a profile of times and dosing. The counselor engaged the participant in a discussion of his or her daily lives, integrating their medications into their routines, and the barriers a participant may experience in taking his or her medications.
For the subsequent four biweekly counseling sessions, the adherence counselor called participants on their project cell phone. The first phone session occurred within 1 week of the office visit followed by three additional biweekly phone sessions. Attempts to contact participants occurred within a 7-day window. The counselor initiated the calls with a check-in on how the participant had been doing. This discussion focused on health and medication-related issues. During the biweekly phone sessions the counselor reminded participants that the purpose of the counseling was to increase their medication awareness and help them stay on track. Each session began with a pill count followed by the counselor calculating adherence while on the phone and delivering immediate corrective feedback. Participants who were greater than or equal to 90% adherent to their medications according to the pill count reviewed their medications taken over the previous 2 weeks, were reinforced for their adherence, and established a plan for remaining adherent. The counselor probed the participant regarding challenges they faced and decisions they made about their medications over the previous 2 weeks. Guided by the objective feedback, the counselor asked about specific strategies used to maintain adherence.
Participants who were less than 90% adherent to their HIV medications as determined by pill count, systematically worked through missed doses and problem solved barriers encountered. The counselor provided participants with feedback on their adherence and asked about the circumstances of their most recent missed doses of medication. Challenges identified by the participant were subjected to a problem solving scheme that entailed identifying alternatives, strategies that could have averted the missed doses, and an action plan for maintaining adherence under similar circumstances in the future. Self-regulation counseling included medication management skills including organization, planning, and using pill boxes. Participants who identified a particular need, such as post-it reminders, or an alarm clock/watch were mailed supportive devices. The adherence counselor specifically revisited past challenges and action plans at subsequent sessions. The final session ended with a detailed plan for participants to self-monitor and sustain their adherence, and reinforced what was working well.
Contact-matched control condition
The control condition received their usual care and had the same number of study contacts as participants who received self-regulation counseling, including the initial office visit to learn how to operate their project cell phone and procedures for conducting unannounced pill counts. Participants in this condition received biweekly pill count cell phone calls that did not include feedback on their adherence or counseling. The biweekly contact calls were made by an assessment staff person rather than the counselor.
Measures
Demographic, health and behavioral assessments were administered at baseline and 4-month follow-up using ACASI procedures.26 Participants were asked their age, ethnicity, years of education, income, HIV symptoms, and employment and disability status. HIV treatment adherence was monitored using unannounced pill counts.
Primary outcome
ART adherence
HIV treatment adherence was monitored with biweekly unannounced telephone-based pill counts. Unannounced pill counts are reliable and valid in assessing HIV treatment adherence when conducted in participants' homes and on the telephone.18,19 Participants were provided with a cell phone that restricted service for project contacts and emergency use (e.g., 911). Participants were called at unscheduled times to count their pills 2 and 4 weeks after counseling ended. Pill counts occurred over 10- to 17-day intervals and were conducted for each ART medication participants were taking. Pharmacy information from pill bottles was also collected to verify the number of pills dispensed between calls. Adherence was calculated as the ratio of pills counted relative to pills prescribed taking into account the number of pills dispensed. Two consecutive pill counts were necessary for computing adherence. Adherence data represents the percentage of pills taken as prescribed averaged across medications.
Adherence assessed at the 4-month follow-up was measured using a single item rating scale that asked participants to estimate the percentage of their HIV medication doses that they had taken in the previous month. This adherence rating scale has been supported in previous research, including significant associations with HIV viral load and correlating r = 0.48 with unannounced pill counts.18,22
Secondary outcomes
Medication adherence self-efficacy
Based on social cognitive theory27 we developed a measure of self-efficacy that presented three situations in which taking medications may be challenging. Our measure allowed participants to judge how confident they were that they could take their medications under the circumstances presented.28 The scale consists of three realistic and personally relevant scenarios within which there were potential challenges for nonadherence. The scenarios varied in circumstances, social relationships, affective states, and settings. One scene concerned sleeping at the time medications should be taken, another concerned visiting with a sister, and the third scenario concerned visiting with an old friend. For each scene, participants rated their confidence to take their medications under those circumstances using an 11-point ascending confidence scale, with responses 0 = “Cannot do,” 5 = “Moderately certain I can do,” and 10 = “Certain I can do.”
Adherence behavioral strategies
To assess adherence strategies, participants indicated whether they had used 14 common strategies for improving medication adherence (see Results for complete list of strategies).29,30 Each strategy was asked about its use in the past month. We also created a summary index of the total number of strategies used as a summary score, α = 0.70.
Process measures
The adherence counselor completed session checklists and written process notes following each cell phone counseling session. Notes were taken regarding participant use of adherence strategies between sessions, specific challenges and problem solving strategies, adherence tools sent to participants, and reinforcements for adherence. The counselor's notes were examined as a process component to the evaluation.
Counselor training
The counselor in this trial was a female master's level social worker with experience working in AIDS services. We specifically selected the counselor to represent the skills and professional background that are common for adherence counselors and case managers working in AIDS care settings. The counselor was trained in the protocol and was supervised in weekly project meetings.
Statistical analyses
Outcome analyses used an intent-to-treat approach in which all available data from participants was included in the analyses regardless of their exposure to the intervention sessions. Initial analyses tested for baseline equivalence between conditions and effects of attrition on dependent measures using t-tests for continuous variables and contingency table χ2 tests for categorical measures. Primary outcomes were tested with analyses of covariance controlling for baseline adherence between the intervention conditions on the immediate postcounseling, 2-week, and 4-week pill count adherence and 4-month follow-up adherence rating scale. Differences between conditions on the self-efficacy scales were also tested using analyses of covariance controlling for baseline. For these analyses we report Wilks' λ for the multivariate tests with η2 to index effect size and F statistics for the univariate tests and their associated d values to index effect size.31 Behavioral strategies were tested using logistic regressions with baseline and follow-up values in separate models for each strategy. The summary index of strategies was also tested in a separate model. Odds ratios and 95% confidence intervals are reported for the logistic regressions.
Results
We retained 39 of the 40 participants over the 4-month observation period; 1 control participant was lost to follow-up. Session completion rates for the self-management counseling reached 99% (83/84), with only one participant missing one of the four cell phone counseling sessions. Initial comparisons between conditions on all baseline characteristics and adherence did not indicate any significant differences between conditions, indicating that the randomization scheme achieved balanced conditions (Table 1).
Table 1.
Demographic and Health Characteristics of Participants Allocated to Behavioral Self-Regulation Counseling and Contact-Matched Control Condition
| |
Self-regulation counseling |
Contact control condition |
|
||
|---|---|---|---|---|---|
| Characteristic | n | % | n | % | χ2 |
| Men | 13 | 62 | 13 | 68 | |
| Women | 8 | 38 | 6 | 32 | 0.18 |
| Transgender | 1 | 5 | 2 | 10 | 0.47 |
| African American | 19 | 90 | 18 | 95 | |
| White | 2 | 10 | 1 | 5 | 0.26 |
| Income < $10,000 | 11 | 52 | 12 | 63 | |
| $11–20,000 | 7 | 33 | 5 | 26 | |
| $21,000+ | 3 | 15 | 2 | 10 | 1.2 |
| Unemployed | 5 | 24 | 5 | 26 | |
| Disabled | 13 | 62 | 10 | 53 | 2.4 |
| History of IDU | 7 | 33 | 6 | 32 | 0.9 |
| Undetectable viral load | 18 | 85 | 14 | 78 | 0.4 |
| CD4 count < 200 | 5 | 24 | 3 | 18 | 0.2 |
| M | SD | M | SD | t | |
|---|---|---|---|---|---|
| Age | 51.1 | 4.7 | 50.9 | 7.7 | 0.1 |
| Education | 12.4 | 2.1 | 12.4 | 1.9 | 0.1 |
| Years since testing HIV+ | 14.8 | 7.6 | 14.5 | 5.1 | 0.1 |
| CD4 cell count | 607.1 | 355.8 | 532.3 | 362.7 | 0.6 |
| HIV symptoms | 6.5 | 2.4 | 6.5 | 2.6 | 0.1 |
IDU, injection drug use; SD, standard deviation.
Primary adherence outcomes
Table 2 shows the means and standard deviations for the baseline and follow-up adherence outcomes. Multivariate analysis controlling for baseline adherence, indicated significant differences between conditions on the four follow-up assessments, Wilks' λ = 0.696, F = 3.17, p < 0.05, η2 = 0.297. Planned univariate analyses tested the differences between conditions at the immediate post, F(1,36) = 9.06, p < 0.01, 2-week follow-up, F(1,36) = 8.58, p < 0.01, 4-week follow-up, F(1,36) = 4.56, p < 0.05, and 4-month follow-up, F(1,36) = 3.32, p < 0.07. The effect sizes for these outcomes are shown in Table 2, which ranged between medium (d = 0.45) and large (d = 0.80).
Table 2.
Unannounced Pill Count Adherence and 4-Month Follow-Up Adherence Rating Scale Values for Participants Allocated to Behavioral Self-Regulation Counseling and Contact Comparison Condition
| |
Self-regulation counseling |
Contact control condition |
|||||
|---|---|---|---|---|---|---|---|
| Adherence | n | M | SD | n | M | SD | d |
| Baseline | 21 | 87.4 | 17.7 | 18 | 91.0 | 9.7 | |
| Immediate postcounseling | 20 | 95.3 | 5.8 | 19 | 81.2 | 24.0 | 0.80 |
| 2-weeks postcounseling | 20 | 90.9 | 11.2 | 18 | 81.0 | 17.6 | 0.67 |
| 4-weeks postcounseling | 21 | 92.8 | 9.0 | 17 | 81.1 | 22.0 | 0.69 |
| 4-months follow-up rating scale | 21 | 94.1 | 9.8 | 18 | 87.8 | 17.2 | 0.45 |
SD, standard deviation.
Secondary self-efficacy and strategies outcomes
Table 3 shows the outcomes from the self-efficacy scales. Results of the multivariate analysis for the three scenarios, controlling for baselines, indicated significant differences between conditions on the 4-month follow-up responses, Wilks' λ = 0.782, F = 2.97, p < 0.05, η2 = 0.253. Planned univariate tests showed that conditions differed on the two social scenarios, but not the sleeping scenario (Table 3). In each case, the behavioral self-management counseling condition demonstrated greater self-efficacy for medication adherence at the follow-up.
Table 3.
Medication Self-Efficacy Among Participants Allocated to Behavioral Self-Regulation Counseling and Contact Comparison Condition
| |
Self-regulation counseling |
Contact control condition |
|
|
||
|---|---|---|---|---|---|---|
| Challenge scenario | M | SD | M | SD | F | d |
| Sleeping, medication next to you | 8.9 | 1.4 | 8.3 | 2.1 | 0.10 | 0.33 |
| Visiting with sister | 7.8 | 1.9 | 6.2 | 2.9 | 5.51 | 0.65 |
| Visiting with old friend | 8.5 | 1.5 | 7.0 | 3.2 | 5.90 | 0.60 |
With respect to behavioral strategies for adherence, results indicated that participants who received behavioral self-management counseling reported using a significantly greater number of adherence strategies at the 4-month follow-up than the control condition (Table 4). For specific strategies, participants who received counseling were more likely to have used pill boxes, stored their medications in open places, used routine activities, and other reminders not specified.
Table 4.
Medication Adherence Strategies Among Participants Allocated to Behavioral Self-Regulation Counseling and Contact Comparison Condition
| |
Self-regulation counseling |
Contact control condition |
Adjusted |
|||
|---|---|---|---|---|---|---|
| Strategy | n | % | n | % | OR | 95% CI |
| Pill box | 14 | 67 | 7 | 39 | 2.7 | 1.14–6.64 |
| Store in the open | 16 | 76 | 10 | 56 | 1.5+ | 0.91–2.73 |
| Store in case or bag | 8 | 38 | 4 | 22 | 1.60 | 0.81–3.115 |
| Timer | 7 | 33 | 4 | 22 | 1.44 | 0.67–3.065 |
| Alarm watch | 7 | 33 | 2 | 11 | 1.81 | 0.79–4.13 |
| Person reminder | 2 | 10 | 3 | 16 | 0.84 | 0.31–2.27 |
| Meal time | 7 | 33 | 7 | 39 | 1.01 | 0.49–2.07 |
| Bedtime | 10 | 48 | 7 | 39 | 1.09 | 0.50–2.35 |
| Routine activity | 11 | 52 | 4 | 22 | 2.2+ | 0.85–5.64 |
| Wrote down | 1 | 5 | 1 | 6 | 1.04 | 0.33–3.26 |
| Calendar | 0 | 0 | ||||
| Reminders | 1 | 5 | 2 | 10 | 0.86 | 0.34–2.17 |
| Pharmacy | 2 | 10 | 1 | 5 | 0.48 | 0.08–2.66 |
| Other reminders | 3 | 16 | 7 | 33 | 2.05 | 0.91–4.63 |
| Total strategies | 4.1 | 2.3 | 2.8 | 2.25 | 1.17 | 1.01–1.36 |
OR, odds ratio; CI, confidence interval.
Process evaluation
An examination of the counselor notes indicated four common adherence challenges addressed in the sessions; time management, side effects/symptom management, sleep management, and medications management. Participants in need of time management were most likely to lead busy lives and found it difficult to keep up with their medications. Because these participants often reported forgetting their medications they explored various reminder and alarm strategies. The counselor offered these participants watch alarms and other low cost devices to help them remember to take their pills. These participants also benefitted from developing strategies with regard to taking their medications with them, integrating medications into daily routines, and planning ahead to order and pick up medication refills. For side-effects and symptom management, participants learned to better track their medications to avoid overdosing. They also discussed their symptoms with their medical providers and pharmacists. Participants in need of sleep management experienced a range of difficulties including sleeping through morning doses, falling asleep before night doses, and complaining of insomnia attributed to medications. To address sleep issues participants altered their sleep schedule by napping, changing sleep times, or more commonly changing medication times. Finally, participants who found it difficult to manage their medications often kept their pills in more than one place and in various storage containers. These participants were offered pill boxes and worked with the counselor on strategies for organizing and sorting their medications.
Although the self-management needs were not mutually exclusive, few participants in this trial needed assistance with more than one behavioral management domain. In addition, while participants may have experienced problems commonly related to nonadherence, such as depression or substance use, these factors were not identified by participants as areas in need of assistance. Thus, the counseling used a pragmatic approach that directly addressed needs identified by participants with strategies to improve adherence.
Discussion
The current findings contribute to the growing literature that supports using telecommunications to deliver behavioral counseling for health improvement.13,15,17 The intervention that was examined in this study was relatively brief, delivered over the course of 4 biweekly 45-min counseling sessions conducted using cell phones. While the intervention could have been delivered using regular land phone service, hard to reach patients often do not have phones and when they do their service is commonly interrupted. Providing patients with restricted service cell phones is a low-cost resource for increasing contact and access with providers. In addition, the counseling utilized unannounced pill counts as a means of monitoring patient adherence. Self-reported adherence is unreliable as an assessment method of adherence and is equally suspect in clinical care. Providing participants with objective feedback on the medications they actually took offered new insights by informing participants of doses that they were often unaware of missing medications. Reflecting back on a brief 2-week period afforded participants opportunities for examining missed doses and the circumstances they found most challenging.
The intervention demonstrated increased adherence from an average that was suboptimal to levels needed to suppress viral replication (e.g., more than 90% adherence).7,9 Participants who received the self-regulation counseling had an average of 90% adherence or greater throughout the follow-up period, including two months after counseling finished. These findings were paralleled by increases in self-efficacy for medication adherence and use of behavioral strategies, two theoretical mechanisms of change in self-regulation models.24 The 4 months that were covered during the intervention and observation period mirrors the lag that commonly occurs between clinical office visits. A practice model of this approach may include an initial office visit with an adherence counselor and subsequent phone sessions that could resume as needed. Alternatively, text messages may offer a low cost alternative to maintaining adherence between office visits.16 However, text messages have not been tested as boosters to phone counseling interventions for treatment adherence. Future research is needed to test brief behavioral self-management counseling intervention in a larger more rigorous trial, and examining alternatives for sustaining gains in adherence over time should be part of those studies.
Results of the current intervention study should be interpreted in light of its limitations. The study was an initial test of concept trial and these results should only be considered preliminary. The sample size for this trial was small and participants were only followed for a short period of time. Although improvements in adherence were promising in the shorter-term, the difference between conditions was no longer significant at the 4-month follow-up. While the primary outcome relied on an objective measure of medication adherence, it was infeasible to examine the impact of the intervention on health improvement and viral suppression. The participants were also drawn from a convenience sample and cannot be considered representative of people receiving ART. This initial test of the intervention concept also used only one counselor and cannot therefore control for counselor characteristics, skill level, or delivery style. Finally, we are unable to determine which elements of the intervention, including the office-based counseling session, medication adherence feedback, or skills covered in the counseling, account for the positive outcomes. With these limitations in mind, we believe that these results are promising and the intervention should be tested in a larger more rigorous trial. There is a significant need for brief, feasible, affordable and effective adherence interventions for people living with HIV/AIIDS and the concept for the model tested in this study warrants further examination.
Acknowledgment
This project was supported by grants from the National Institute of Mental Health (NIMH) grant R01-MH82633.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Collaboration H-C. The Effect of combined antiretroviral therapy on the overall mortality of HIV-infected individuals. AIDS. 2010;24:123–137. doi: 10.1097/QAD.0b013e3283324283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lima VD. Bangsberg DR. Harrigan PR, et al. Risk of viral failure declines with duration of suppression on highly active antiretroviral therapy irrespective of adherence level. J Acquir Immune Defic Syndr. 2010;55:460–465. doi: 10.1097/QAI.0b013e3181f2ac87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bangsberg DR. Kroetz DL. Deeks SG. Adherence-resistance relationships to combination HIV antiretroviral therapy. Curr HIV/AIDS Rep. 2007;4:65–72. doi: 10.1007/s11904-007-0010-0. [DOI] [PubMed] [Google Scholar]
- 4.Braitstein P. Brinkhof MW. Dabis F, et al. Mortality of HIV-1-infected patients in the first year of antiretroviral therapy: Comparison between low-income and high-income countries. Lancet. 2006;367:817–824. doi: 10.1016/S0140-6736(06)68337-2. [DOI] [PubMed] [Google Scholar]
- 5.Heckman TG. Somlai AM. Kalichman SC, et al. Psychosocial differences between urban and rural people living with HIV/AIDS. J Rural Health. 1998;14:138–145. doi: 10.1111/j.1748-0361.1998.tb00615.x. [DOI] [PubMed] [Google Scholar]
- 6.Bangsberg DR. Deeks SG. Is average adherence to HIV antiretroviral therapy enough? J Gen Intern Med. 2002;17:812–813. doi: 10.1046/j.1525-1497.2002.20812.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bangsberg D. Less Than 95% adherence to nonnucleoside reverse-transcriptase inhibitor therapy can lead to viral suppression. Clin Infect Dis. 2006;43:939–441. doi: 10.1086/507526. [DOI] [PubMed] [Google Scholar]
- 8.Volberding PA. Deeks SG. Antiretroviral therapy and management of HIV infection. Lancet. 2010;376:49–62. doi: 10.1016/S0140-6736(10)60676-9. [DOI] [PubMed] [Google Scholar]
- 9.Parienti JJ. Das-Douglas M. Massari V, et al. Not all missed doses are the same: sustained NNRTI treatment interruptions predict HIV rebound at low-to-moderate adherence levels. PLoS ONE. 2008;3:e2783. doi: 10.1371/journal.pone.0002783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bangsberg DR. Preventing HIV antiretroviral resistance through better monitoring of treatment adherence. J Infect Dis. 2008;197(Suppl 3):S272–278. doi: 10.1086/533415. [DOI] [PubMed] [Google Scholar]
- 11.Haberer JE. Kahane J. Kigozi I, et al. Real-time adherence monitoring for HIV antiretroviral therapy. AIDS Behav. 2010;14:1340–1346. doi: 10.1007/s10461-010-9799-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.CTIA Advocacy CW. Wireless quick facts. www.ctia.org/advocacy/research/index.cfm/aid/10323. [Jan 14;2011 ]. www.ctia.org/advocacy/research/index.cfm/aid/10323
- 13.Lawler SP. Winkler E. Reeves MM, et al. Multiple health behavior changes and co-variation in a telephone counseling trial. Ann Behav Med. 2010;39:250–257. doi: 10.1007/s12160-010-9188-2. [DOI] [PubMed] [Google Scholar]
- 14.Stein MD. Herman DS. Bishop D, et al. A telephone-based intervention for depression in HIV patients: Negative results from a randomized clinical trial. AIDS Behav. 2007;11:15–23. doi: 10.1007/s10461-006-9131-5. [DOI] [PubMed] [Google Scholar]
- 15.Heckman TG. Carlson B. A randomized clinical trial of two telephone-delivered, mental health interventions for HIV-infected persons in rural areas of the United States. AIDS Behav. 2007;11:5–14. doi: 10.1007/s10461-006-9111-9. [DOI] [PubMed] [Google Scholar]
- 16.Lester RT. Ritvo P. Mills EJ, et al. Effects of a mobile phone short message service on antiretroviral treatment adherence in Kenya (WelTel Kenya1): A randomised trial. Lancet. 2010;376:1838–1845. doi: 10.1016/S0140-6736(10)61997-6. [DOI] [PubMed] [Google Scholar]
- 17.Reynolds NR. Testa MA. Su M, et al. Telephone support to improve antiretroviral medication adherence: A multisite, randomized controlled trial. J Acquir Immune Defic Syndr. 2008;47:62–68. doi: 10.1097/QAI.0b013e3181582d54. [DOI] [PubMed] [Google Scholar]
- 18.Bangsberg DR. Hecht FM. Charlebois ED, et al. Comparing objective measures of adherence to HIV antiretroviral therapy: Electronic medication monitors and unannounced pill counts. AIDS Behav. 2001;5:275–281. [Google Scholar]
- 19.Kalichman SC. Amaral CM. Cherry C, et al. Monitoring antiretroviral adherence by unannounced pill counts conducted by telephone: Reliability and criterion-related validity. HIV Clin Trials. 2008;9:298–308. doi: 10.1310/hct0905-298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kalichman SC. Amaral CM. Stearns H, et al. Adherence to antiretroviral therapy assessed by unannounced pill counts conducted by telephone. J Gen Intern Med. 2007;22:1003–1006. doi: 10.1007/s11606-007-0171-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.El-Sadr WM. Mayer KH. Hodder SL. AIDS in America—Forgotten but not gone. N Engl J Med. 2010;362:967–970. doi: 10.1056/NEJMp1000069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kalichman SC. Amaral CM. Swetzes C, et al. A simple single-item rating scale to measure medication adherence: Further evidence for convergent validity. J Int Assoc Physicians AIDS Care. 2009;8:367–374. doi: 10.1177/1545109709352884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Giordano TP. Guzman D. Clark R, et al. Measuring adherence to antiretroviral therapy in a diverse population using a visual analogue scale. HIV Clin Trials. 2004;5:74–79. doi: 10.1310/JFXH-G3X2-EYM6-D6UG. [DOI] [PubMed] [Google Scholar]
- 24.Reynolds NR. The problem of antiretroviral adherence: A self-regulatory model for intervention. AIDS Care. 2003;15:117–124. doi: 10.1080/0954012021000039815. [DOI] [PubMed] [Google Scholar]
- 25.Wang H. Zhou J. Huang L, et al. Effects of nurse-delivered home visits combined with telephone calls on medication adherence, quality of life in HIV-infected heroin users in Hunan of China. J Clin Nurs. 2010;19:380–388. doi: 10.1111/j.1365-2702.2009.03048.x. [DOI] [PubMed] [Google Scholar]
- 26.Gribble JN. Miller HG. Cooley PC, et al. The impact of T-ACASI interviewing on reported drug use among men who have sex with men. Subst Use Misuse. 2000;35:869–890. doi: 10.3109/10826080009148425. [DOI] [PubMed] [Google Scholar]
- 27.Bandura A. Self-Efficacy: The Exercise of Control. New York: Freeman; 1997. [Google Scholar]
- 28.Kalichman SC. Cain D. Fuhrel A, et al. Assessing medication adherence self-efficacy among low-literacy patients: Development of a pictographic visual analogue scale. Health Educ Res. 2005;20:24–35. doi: 10.1093/her/cyg106. [DOI] [PubMed] [Google Scholar]
- 29.Catz SL. Kelly JA. Bogart LM, et al. Patterns, correlates, and barriers to medication adherence among persons prescribed new treatments for HIV disease. Health Psychol. 2000;19:124–133. [PubMed] [Google Scholar]
- 30.Kalichman SC. Cain D. Cherry C, et al. Pillboxes and antiretroviral adherence: Prevalence of use, perceived benefits, and implications for electronic medication monitoring devices. AIDS Patient Care STDs. 2005;19:49–55. doi: 10.1089/apc.2005.19.833. [DOI] [PubMed] [Google Scholar]
- 31.Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]