Abstract
The objective of this study was to describe attitudes, opinions, and perceived health needs of HIV-infected women in the United States. In this cross-sectional study, women were invited to participate in the Women Living Positive survey, a structured interview instrument with 45 questions. Collected data were deidentified and the margin of error was calculated as four percentage points. Incoming toll-free phone interviews were conducted from December 21, 2006, through March 14, 2007 among subjects recruited from a U.S. national network of AIDS counseling centers. Seven hundred HIV-infected women (43% African American, 28.5% Hispanic, 28.5% Caucasian; median age, 42.5 years) receiving combination antiretroviral therapy for 3 years or more replied to recruitment flyers. Overall, 55% of survey participants had never discussed gender-specific HIV treatment issues with their HIV care providers. Of the 45% who did discuss these issues, almost all (96%) were satisfied. On average, one-third of the women had seen three or more providers since beginning HIV treatment; 43% indicated they had switched providers because of communication issues. Among women who had been or were pregnant at the time of the survey (n=159), more than half (57%) had not had pre-pregnancy discussions with their HIV provider about the most appropriate HIV regimens for women attempting to become pregnant. Significant communication gaps exist between HIV-infected women and their providers when discussing gender-specific treatment issues. These data highlight a need for U.S. health care providers to incorporate discussion of gender-specific issues, including preconception and reproductive counseling, into management strategies for HIV-infected women.
Introduction
Worldwide, women represent half of all adults living with HIV and AIDS.1 Over the past two decades there has been an increase in the proportion of women living with HIV/AIDS in the United States. The latest estimates from the Centers of Disease Control indicate that of the more than 1.1 million people living with HIV in the United States in 2006, 278,400 were women.2 By this account women represent approximately one quarter of the U.S. HIV-infected population, a significant increase from the 13% reported just a decade earlier in 1994.3
Many HIV-infected women express the desire to bear children, and the use of highly active antiretroviral therapy during pregnancy, along with appropriate use of caesarean section and avoidance of breast-feeding, have resulted in significantly decreased perinatal acquisition rates to less than 2% in the United States.4 Yet, there are scant data on the effectiveness with which medical providers address potential pregnancy in HIV-infected women. In a recent cross-sectional study of 181 predominantly African American HIV-infected women, 67% reported a general discussion about pregnancy and HIV with their primary health care provider, whereas 31% reported a personalized discussion about future childbearing plans. Of these personalized discussions, 64% were patient initiated.5 In light of the rising prevalence of HIV/AIDS among women in the United States, it is essential to understand the current attitudes, perceptions and health needs of this patient population. In addition, HIV disease, as well as antiretroviral therapy, may affect women differently than men and HIV-infected women face a unique set of health and psychosocial issues that may alter the course of their treatment and disease. Despite these anticipated differences, few studies have explored the gender-specific health needs of HIV-infected women. The Women Living Positive (WLP) survey (Supplementary Material; Supplementary data are available online at www.liebertonline.com/apc) provides direct feedback from women about the communication barriers with their health care providers regarding important issues, including preconception and reproductive counseling.
Methods
The WLP survey was designed with the input of HIV-infected women to explore their attitudes and behaviors as they relate to gender-specific health care needs, patient–health care provider communications and preconception counseling in the United States. A 15-min telephone survey was designed to effectively describe some aspects of the patients' relationships with HIV health care providers, treatment priorities, reproductive health issues (including questions about pregnancy and family planning) and emotional aspects of living with HIV. The survey consisted of a series of eligibility questions as well as 45 topic-specific questions. Respondents were anonymously interviewed by telephone from December 21, 2006, through March 14, 2007, by GfK Roper Public Affairs & Media (New York, NY), a public opinion polling firm. The survey was funded and managed by Boehringer Ingelheim Pharmaceuticals, Inc. (Ridgefield, CT) in consultation with The Well Project (Atlanta, GA; www.thewellproject.org), a nonprofit organization for women affected by HIV.
Study investigators sought a study population that would accurately reflect the regional, racial, and ethnic demographics of HIV-infected women in the United States. Participants were recruited via flyers from a diverse group of 29 AIDS information, counseling, and treatment centers across the United States, which directed HIV-infected women to call a toll-free number. Response rates could not be determined because of the recruitment method. Participants were designated to one of three possible groups: Caucasian; Hispanic or African American. The African American sample consisted of respondents who identified themselves as “African American or black, not of Hispanic origin,” the Caucasian sample consisted of respondents who identified themselves as “Caucasian or white, not of Hispanic origin,” and Hispanic women self-identified as Hispanic without membership in either of the other groups. Women belonging to other racial/ethnic groups were excluded. Interviews were conducted in Spanish and English, depending on the participant's preference.
Inclusion criteria included: HIV seropositivity by self-report, receipt of combination antiretroviral therapy for at least 3 years and older than 18 years. Women who qualified for the survey were compensated $25 for their time. Participants were surveyed anonymously; upon completion each was assigned a code to provide to the counseling center's administrator for compensation. Descriptive statistics were performed on responses; the margin of error was four percentage points. Data were weighted by census regions and ethnicity/race to match the demographic profile of adult HIV-infected women in the United States.
Results
The sample comprised 700 HIV-infected women: 200 Caucasian; 200 Hispanic and 300 African American. The median age was 42.5 years (range, 21–69 years; Table 1). Participants had been aware of their HIV status for a mean of 10.6 years and were receiving combination antiretroviral therapy for a mean of 8.1 years. Geographic distribution was as follows: 16%, West; 21%, Midwest; 33%, South; and 30%, Northeast. Thirty-nine percent of participants had children.
Table 1.
Demographic Information of HIV-Infected Women in the Study
| |
% Participants |
|||
|---|---|---|---|---|
| Variable | Total sample (n=700) | Caucasian (n=200) | Hispanic (n=200) | African American (n=300) |
| Marital status | ||||
| Married/living with partner | 28 | 35 | 37 | 23a |
| Single | 38 | 26 | 26 | 45a |
| Separated/divorced | 25 | 29 | 21 | 25 |
| Widowed | 9 | 9 | 16 | 7 |
| Education | ||||
| High school graduate or less | 61 | 51 | 69 | 61 |
| Some college | 23 | 30 | 17 | 23 |
| College graduate or more | 12 | 16 | 10 | 11 |
| Age, y | ||||
| Under 35 | 19 | 20 | 14 | 20 |
| 35–44 | 39 | 36 | 47a | 37 |
| 45 and older | 42 | 44 | 37 | 43 |
| Years with identified HIV infection, mean | 10.6 | 11.3 | 10.1 | 10.6 |
| Years on antiretroviral medication, mean | 8.1 | 8.9a | 7.6 | 8.0 |
| Have child/children | 39 | 30a | 40 | 41 |
| Caregiver (net) | 52 | 44 | 58 | 52 |
Significantly different from the other two subgroups at the 95% confidence level.
Perceived gender issues
Although nearly half (46%) felt that their disease affected them differently than men, a majority (55%) had never discussed possible gender-based differences in treatment response with their practitioners. Caucasian and African American women were less likely than Hispanic women to have discussed this issue with their HIV health care provider (58% and 61% versus 34%, respectively; p<0.05). Women with male HIV health care providers were significantly less likely than women with female providers to have discussed this topic (41% versus 51%, respectively; p<0.05). Of the 45% who did have this discussion with their providers, almost all (96%) were satisfied with the answers they received. Of note, on average one third of the women had seen three or more providers since they started receiving treatment for HIV, and 43% indicated that they had switched providers because of communication issues.
Reproductive, childbearing, and caregiver issues
The WLP survey also revealed a significant communication gap between HIV-infected women and their practitioners on reproductive issues. Of the 227 women who had been pregnant but were not pregnant at the time of the survey or those who would consider pregnancy, approximately half (48%) were never asked by their health care provider if they had or were considering having children. Of women who had been or were pregnant or were thinking about getting pregnant at the time of the survey (n=239), 57% had not discussed appropriate treatment options with their practitioners before becoming pregnant. Moreover, of those who were currently pregnant or who had been pregnant (n=159), only 64 (42%) had discussed their pregnancy and appropriate HIV treatment options with their HIV health care provider prior to becoming pregnant. Additionally, 42% of those who were currently pregnant or who had been pregnant were either “not very aware” or “not at all aware” of the treatment options for pregnant women with HIV.
Survey responses demonstrated a dichotomy between perceived societal views and the respondent's personal views on childbearing among HIV-infected women. Although a majority—61% overall: 61% African American, 62% Caucasian, 59% Hispanic—personally felt that they could have children with the appropriate medical care, 59% believed that society strongly urges them not to have children. Caucasian women were significantly more likely than Hispanic women to express this perception (67% versus 53%, respectively; p<0.05). Additionally, HIV-infected women living in the South were more likely than those in the Northeast or Midwest to experience this societal stigma (66% versus 52% and 55%, respectively; p<0.05). HIV-infected women who received care from a nurse practitioner or physician assistant were significantly less likely to note this attitude than those treated by an infectious disease specialist or family medicine/general practitioner (48% versus 62% and 62%, respectively; p<0.05).
Thirty-nine percent of the participants had children in their household, and 52% identified themselves as caregivers. In all, 43% reported that living with HIV has made it more difficult for them to take care of their families, including 53% of Hispanics, 40% of African Americans and 45% of Caucasians (p<0.05). Regionally, more women in the South versus the Northeast reported that living with HIV has made it more difficult for them to take care of their families (50% versus 37%, respectively; p<0.05).
Other issues of concern
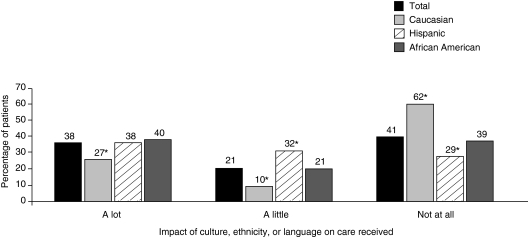
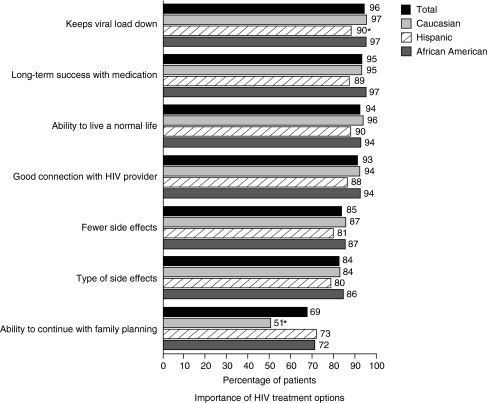
Fifty-nine percent felt that their culture, ethnicity or language has an effect on the care that they receive. Hispanic and African American women were more likely to report this than Caucasian women (Fig. 1). Women in the South were also more likely than those in the West or Northeast to feel that their culture, ethnicity or language affects care. However, a majority of HIV-infected women in the survey—regardless of their ethnicity—shared similar treatment priorities, indicating that factors such as suppressing viral load, achieving long-term success with medication and being able to live normal lives were important aspects of their HIV treatment (Fig. 2).
FIG. 1.
Women's perceptions of the effect of culture, ethnicity, or language on the level of care received by HIV-infected women. Participants' answers to: “To what extent, if at all, do you feel that your culture, ethnicity, or language impacts the care you receive?” Base: all women. *p<0.05 versus other two subgroups.
FIG. 2.
Treatment priorities among HIV-infected women. Participants' answers to: “When thinking about your HIV treatment options, how important are each of the following to you?” Base: all women. *p<0.05 versus other two subgroups.
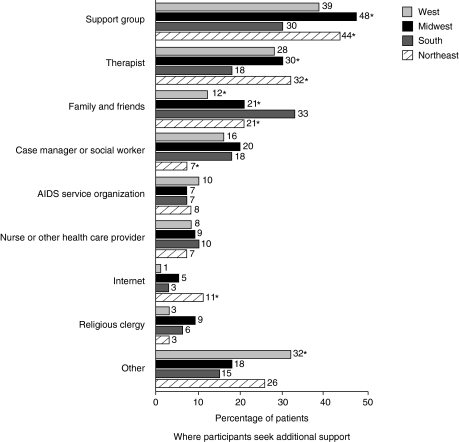
Overall, HIV-infected women who wanted additional support beyond what their practitioners could provide indicated they found it through support groups, therapists, family, and friends. Caucasian women primarily identified therapists as sources of additional support (38% compared with 25% and 23% for Hispanic and African American participants, respectively; p<0.05), while Hispanic and African American participants primarily identified support groups. Source of support varied by geographic location, with women in the Midwest and Northeast more likely to get additional support from a support group or a therapist while those in the South were more likely to get this support from family and friends (Fig. 3).
FIG. 3.
Sources of additional support for HIV-infected women: analysis by U.S. geographic region. Participants' answers to: “Where have you looked for this additional support?” Base: all women. *p<0.05 versus other two subgroups.
Seventy-three percent overall indicated that living with HIV has caused them to struggle “a great deal” or “somewhat” in managing their daily lives (70% of African American, 79% of Caucasian, and 78% of Hispanic participants). Twenty-seven percent described have often experienced five or more feelings commonly associated with depression, with one third experiencing changes in sleep patterns, loss of energy, unexplained aches or pains, feelings of sadness or worry and anxiety. Although 58% indicated they were comfortable talking to their providers about their depression-related feelings, women in the South were significantly less likely to feel comfortable than those in the rest of the country (47% versus 58%, respectively; p<0.05).
Discussion
Despite the fact that women now comprise more than one fourth of all persons living with HIV in the United States, the data from the WLP survey suggest that there are enormous opportunities for improved communication between health care providers and HIV-infected women regarding gender-based issues, particularly as they relate to management of HIV infection in anticipation of and/or during pregnancy. This survey provided a platform for a broad selection of women with HIV to describe their concerns regarding patient–provider communication, and brought to light several important issues. The fact that less than half of the participants had discussed gender-based issues with their health care providers may relate to lack of experience or comfort among providers in raising these issues. It is also possible that HIV practitioners do not anticipate discussing family planning and pregnancy with their patients because of a general lack of focus or priority on this subject, or an expectation that this subject will be addressed by other health care providers. Additionally, a lack of gender-specific knowledge on the part of the provider may preclude such discussions. Although there continues to be a relative lack of data on how treatment of HIV-infected women may differ from the data regarding men, there has been a marked increase in the presentation and publication of treatment studies in women in recent years. Several pharmacokinetic studies have been performed in pregnant women,6–8 and recent analyses of the Pregnancy Registry data provide a measure of reassurance on the effects of in utero antiretroviral exposure.9 Therefore, data are available to providers regarding safety and dosing of some antiretroviral agents in pregnant women. Data on optimal combination antiretroviral therapy during pregnancy is limited; much of the information comes from mother-to-child transmission-prevention trials. While these trials have clearly established the efficacy of antiretroviral agents in preventing HIV transmission, they provide only limited data on optimal antiretroviral agent combinations for tolerability and efficacy during pregnancy.
Although there is abundant evidence that pregnancy in HIV-infected women is associated with successful outcomes and low risk of mother-to-child transmission, the social stigma surrounding this issue remains strong. Many HIV-infected mothers fear that the disease will gravely disrupt their ability to raise their children. In the WLP survey, HIV-infected women commonly felt stigmatized by society. Women also fear the possibility of losing their children and the likelihood that their children will be ostracized if their mother's HIV status is disclosed.10 As a result of these concerns HIV-infected women, particularly those who serve as caregivers, may keep their HIV status confidential for as long as possible and may even be hesitant to seek early medical care.11 These factors may explain, in part, why a significant proportion of HIV-infected women in the United States are diagnosed with HIV or seek treatment late in the course of their disease.12
In addition to fears over social stigmatization, factors such as poverty, barriers that affect access to health care (such as lack of medical insurance or competing subsistence needs),13 cultural and language barriers may hinder early diagnosis and treatment.12 HIV providers must recognize that these important barriers exist and proactively address them with their patients. An HIV provider may be one of the few persons with whom an HIV-infected woman may frankly discuss the implications and impact of HIV infection on their family responsibilities.
Studies of recently approved antiretroviral agents show low participation rates by nonpregnant women, with 10–12% of treatment experienced women enrolling in studies14–18 and higher rates of participation in treatment-naïve trials.19,20 As a result, none of these randomized prospective trials have been powered to assess outcomes in men versus those in women. In the HEAT20 and CASTLE19 trials, two studies assessing combination antiretroviral therapy in treatment-naïve patients, women represented 18% and 31% of participants, respectively, and neither efficacy nor safety results were stratified by gender. A review from the federally-funded Adult AIDS Clinical Trials Group (ACTG) suggests that demographic factors such as a patient's ethnicity and geographic location may limit study enrollment more than specific trial exclusionary criteria. At the time of the ACTG review African American women comprised more than 50% of the total HIV-infected female population in the United States, but accounted for less than 25% of women entering the ACTG trials. Furthermore, relative to the regional prevalence of HIV/AIDS among women, fewer women from the Southeast and Mid-Atlantic regions enrolled in these trials compared with the rest of the country.21
One study that was powered to compare safety and efficacy outcomes in men and women was the recently presented Gender, Race, and Clinical Experience (GRACE) trial. In this study of 287 women and 142 men, virologic response by an intent-to-treat analysis was higher in men (58.5%) than women (50.9%).22 However, a greater proportion of HIV-infected women compared with men prematurely discontinued from the study; after accounting for this difference, rates of virologic response rates among men and women were similar.22 Although multiple reasons were given for discontinuations in GRACE, the data suggest that women may have unique needs that must be addressed to ensure retention in care.
Receiving an HIV diagnosis, coping with the disease on a day-to-day basis, and living with fears and concerns throughout the course of the disease can place a substantial psychological burden on HIV-infected patients. Although our study found that 27% of participants had five or more feelings commonly associated with depression, other studies have reported even higher rates of depression. In the HIV Epidemiology Research Study (HERS), 42% of the 765 HIV-positive women enrolled had chronic depressive symptoms,23 while 50% of the 2058 HIV-positive study participants in the Women's Interagency HIV Study (WIHS) had symptoms of clinical depression.24 Further evidence suggests that women living in rural areas are at greater risk for developing depression because characteristics of rural environments, such as physical isolation and concerns over social stigma, may limit their ability to or the likelihood of seeking help.25 Regardless of differences between sociodemographic groups, rates of depression have been consistently higher among HIV-infected women collectively compared with HIV-infected men.25 Chronic depression also has been linked to higher mortality rates in HIV-infected women. In the HERS cohort chronically depressed HIV-positive women were twice as likely to die compared with those with limited or no depressive symptom.23 Therefore, routine screening for depression and other psychological illnesses should be incorporated into the disease management plan for all HIV-infected women, and adequate medication and counseling services should be offered to those who meet the criteria for clinical depression.
Sociodemographic factors affect the manner in which HIV-infected women receive support from the community. Social support and coping mechanisms are vital parts of overall disease management. Adequate social support can influence psychological well-being,26,27 improve quality of life,28 and facilitate factors such as medication adherence, which may ultimately determine the progression of HIV disease.29
Our understanding of the unique health concerns of HIV-infected women in the United States is slowly increasing. It is imperative that this knowledge is successfully incorporated into clinical practice. Women now constitute roughly 25% of the individuals in the US in whom a new diagnosis of HIV is made.3 Our data suggest that much remains to be accomplished in ensuring optimal care for women with HIV. Many HIV care providers still do not incorporate a discussion of gender-specific issues into patient visits. The results of the WLP survey indicate that practitioners should proactively discuss issues such as family and reproductive planning with their HIV-infected patients. HIV providers should encourage open discussions about other treatment-related, psychosocial, and emotional aspects of HIV disease. At this point in the history of HIV management providers are not simply preventing death but are implementing long-term treatment strategies to enable patients to live long and fulfilling lives. This goal can only be achieved for HIV-infected women through careful attention to gender-specific issues and by establishing an environment for open communication. The shortcomings in clinical practice perceived by HIV-infected women in the WLP survey could be addressed by offering training for HIV health care providers on gender-specific issues and how to better communicate with their patients about important issues, such as family planning and childbearing.
Supplementary Material
Acknowledgments
This study was funded by Boehringer Ingelheim Pharmaceuticals, Inc. and developed in collaboration with The Well Project.
K.S., S.H., J.A., J.F., S.S., D.A.B., and S.A. had full access to all the data in the study and take full responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: S.S., S.A., D.A.B. Study conduct and data collection and management: S.A. Data analysis and interpretation: K.S., D.A.B., S.A., J.A.A., J.F., S.H., S.S. Manuscript preparation and critical review: K.S., D.A.B., S.A., J.A.A., J.F., S.H., S.S. Manuscript approval: K.S., D.A.B., S.A., J.A.A., J.F., S.H., S.S. We acknowledge Devanshi Amin, Pharm.D., for her editorial assistance with the preparation of this report and Ann Wainwright, Boehringer Ingelheim Pharmaceuticals, Inc., for her support in the execution of the survey. We are grateful to all the survey participants for their time and energy.
Author Disclosure Statement
Dr. Kathleen Squires, Dr. Sally Hodder, Ms. Dawn Averitt Bridge, and Mr. Staats Abrams are consultants for Boehringer Ingelheim Pharmaceuticals, Inc. and Dr. Stephen Storfer is employed by Boehringer Ingelheim Pharmaceuticals, Inc. Drs. Judith Aberg and Judith Feinberg have received honoraria from Boehringer Ingelheim Pharmaceuticals, Inc. for participation in advisory boards.
References
- 1.UNAIDS. Worldwide HIV and AIDS Statistics. 2009. www.avert.org/worldstats.htm. [Feb 28;2011 ]. www.avert.org/worldstats.htm
- 2.HIV prevalence estimates—United States, 2006. Morb Mortal Wkly Rep. 2008;57:1073–1076. [PubMed] [Google Scholar]
- 3.Update: AIDS among women—United States, 1994. MMWR Morb Mortal Wkly Rep. 1995;44:81–84. [PubMed] [Google Scholar]
- 4.Cooper ER. Charurat M. Mofenson L, et al. Combination antiretroviral strategies for the treatment of pregnant HIV-1–infected women and prevention of perinatal HIV-1 transmission. J Acquir Immune Defic Syndr. 2002;29:484–494. doi: 10.1097/00126334-200204150-00009. [DOI] [PubMed] [Google Scholar]
- 5.Finocchario-Kessler S. Dariotis JK. Sweat MD, et al. Do HIV-infected women want to discuss reproductive plans with providers, and are those conversations occurring? AIDS Patient Care STDs. 2010;24:317–323. doi: 10.1089/apc.2009.0293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mirochnick M. Best BM. Stek AM, et al. Lopinavir exposure with an increased dose during pregnancy. J Acquir Immune Defic Syndr. 2008;49:485–491. doi: 10.1097/QAI.0b013e318186edd0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ripamonti D. Cattaneo D. Maggiolo F, et al. Atazanavir plus low-dose ritonavir in pregnancy: pharmacokinetics and placental transfer. AIDS. 2007;21:2409–2415. doi: 10.1097/QAD.0b013e32825a69d1. [DOI] [PubMed] [Google Scholar]
- 8.Hirt D. Urien S. Ekouevi DK, et al. Population pharmacokinetics of tenofovir in HIV-1–infected pregnant women and their neonates (ANRS 12109) Clin Pharmacol Ther. 2009;85:182–189. doi: 10.1038/clpt.2008.201. [DOI] [PubMed] [Google Scholar]
- 9.Squires K. Olmscheid B. Guyer B. Zhang S. TDF-containing antiretroviral regimens in pregnancy: Findings from the Antiretroviral Pregnancy Registry. 49th Interscience Conference on Antimicrobial Agents and Chemotherapy (ICAAC); San Francisco. Sep 12–15;2009 .2009. [Google Scholar]
- 10.Marlink R. Kao H. Hsieh E. Clinical care issues for women living with HIV and AIDS in the United States. AIDS Res Hum Retroviruses. 2001;17:1–33. doi: 10.1089/088922201750056753. [DOI] [PubMed] [Google Scholar]
- 11.Sowell RL. Seals B. Moneyham L. Guillory J. Demi A. Cohen L. Barriers to health-seeking behaviors for women infected with HIV. Nursingconnections. 1996;9:5–17. [PubMed] [Google Scholar]
- 12.Squires KE. Gender differences in the diagnosis and treatment of HIV. Gend Med. 2007;4:294–307. doi: 10.1016/s1550-8579(07)80060-x. [DOI] [PubMed] [Google Scholar]
- 13.Hader SL. Smith DK. Moore JS. Holmberg SD. HIV infection in women in the United States: Status at the Millennium. JAMA. 2001;285:1186–1192. doi: 10.1001/jama.285.9.1186. [DOI] [PubMed] [Google Scholar]
- 14.Merck & Co. Inc ISENTRESS® (raltegravir) [full prescribing information] www.merck.com/product/usa/pi_circulars/i/isentress/isentress_pi.pdf. [Apr 22;2010 ]. www.merck.com/product/usa/pi_circulars/i/isentress/isentress_pi.pdf
- 15.Pfizer Labs SELZENTRY® (maraviroc) tablets [full prescribing information] http://us.gsk.com/products/assets/us_selzentry.pdf. [Apr 22;2010 ]. http://us.gsk.com/products/assets/us_selzentry.pdf
- 16.Boehringer Ingelheim Pharmaceuticals, Inc APTIVUS® (tipranavir) capsules, oral solution [full prescribing information] http://bidocs.boehringer-ingelheim.com/BIWebAccess/ViewServlet.ser?docBase=renetnt&folderPath=/Prescribing+Information/PIs/Aptivus/10003515+US+01.pdf. [Apr 22;2010 ]. http://bidocs.boehringer-ingelheim.com/BIWebAccess/ViewServlet.ser?docBase=renetnt&folderPath=/Prescribing+Information/PIs/Aptivus/10003515+US+01.pdf
- 17.Tibotec Therapeutics INTELENCE® (etravirine) tablets [full prescribing information] www.intelence-info.com/intelence/assets/pdf/INTELENCE_PI.pdf. [Apr 22;2010 ]. www.intelence-info.com/intelence/assets/pdf/INTELENCE_PI.pdf ,
- 18.Tibotec Therapeutics PREZISTA® (darunavir) tablet, film coated for oral use [full prescribing information] http://www.prezista.com/prezista/documents/us_package_insert.pdf. [Apr 22;2010 ]. http://www.prezista.com/prezista/documents/us_package_insert.pdf ,
- 19.Molina JM. Andrade-Villanueva J. Echevarria J, et al. Once-daily atazanavir/ritonavir compared with twice-daily lopinavir/ritonavir, each in combination with tenofovir and emtricitabine, for management of antiretroviral-naive HIV-1-infected patients: 96-week efficacy and safety results of the CASTLE study. J Acquir Immune Defic Syndr. 2008;53:323–332. doi: 10.1097/QAI.0b013e3181c990bf. [DOI] [PubMed] [Google Scholar]
- 20.Smith KY. Patel P. Fine D, et al. Randomized, double-blind, placebo-matched, multicenter trial of abacavir/lamivudine or tenofovir/emtricitabine with lopinavir/ritonavir for initial HIV treatment. AIDS. 2009;23:1547–1556. doi: 10.1097/QAD.0b013e32832cbcc2. [DOI] [PubMed] [Google Scholar]
- 21.Cotton DJ. Finkelstein DM. He W. Feinberg J. Determinants of accrual of women to a large, multicenter clinical trials program of human immunodeficiency virus infection. The AIDS Clinical Trials Group. J Acquir Immune Defic Syndr. 1993;6:1322–1328. [PubMed] [Google Scholar]
- 22.Currier J. Averitt Bridge D. Hagins D, et al. Sex-based outcomes of darunavir-ritonavir therapy: a single-group trial. Ann Intern Med. 2010;153:349–357. doi: 10.1059/0003-4819-153-6-201009210-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ickovics JR. Hamburger ME. Vlahov D, et al. Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA. 2001;285:1466–1474. doi: 10.1001/jama.285.11.1466. [DOI] [PubMed] [Google Scholar]
- 24.Barkan SE. Melnick SL. Preston-Martin S, et al. The Women's Interagency HIV Study. WIHS Collaborative Study Group. Epidemiology. 1998;9:117–125. [PubMed] [Google Scholar]
- 25.Moneyham L. Murdaugh C. Phillips K, et al. Patterns of risk of depressive symptoms among HIV-positive women in the southeastern United States. J Assoc Nurses AIDS Care. 2005;16:25–38. doi: 10.1016/j.jana.2005.05.005. [DOI] [PubMed] [Google Scholar]
- 26.Kempf MC. McLeod J. Boehme AK, et al. A qualitative study of the barriers and facilitators to retention-in-care among HIV-positive women in the rural southeastern United States: Implications for targeted interventions. AIDS Patient Care STDs. 2010;24:515–520. doi: 10.1089/apc.2010.0065. [DOI] [PubMed] [Google Scholar]
- 27.Vyavaharkar M. Moneyham L. Corwin S. Saunders R. Annang L. Tavakoli A. Relationships between stigma, social support, and depression in HIV-infected African American women living in the rural Southeastern United States. J Assoc Nurses AIDS Care. 2010;21:144–152. doi: 10.1016/j.jana.2009.07.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sowell RL. Seals BF. Moneyham L. Demi A. Cohen L. Brake S. Quality of life in HIV-infected women in the south-eastern United States. AIDS Care. 1997;9:501–512. doi: 10.1080/713613191. [DOI] [PubMed] [Google Scholar]
- 29.Vyavaharkar M. Moneyham L. Tavakoli A, et al. Social support, coping, and medication adherence among HIV-positive women with depression living in rural areas of the southeastern United States. AIDS Patient Care STDS. 2007;21:667–680. doi: 10.1089/apc.2006.0131. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.