We present a rare case of spontaneous empyema necessitatis caused by Aspergillus fumigatus infection.
Case report
A 60-year-old woman presented with fever, chest wall pain and mild dyspnoea for days. The woman sought medical attention in the outpatient department. She stated that she had been healthy in the past and had no history of diabetes, hypertension or other disease. However, she had been a vegetarian for decades. She had no gross lesion in the chest wall and she also denied any trauma as well as travel history. Auscultation of the lung showed some rales and decreased breath sounds in right lower lung fields. The patient was then admitted for relevant studies under the impression of pneumonia with parapneumonic effusion on the right side.
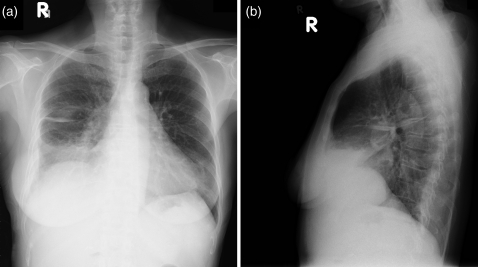
Laboratory data showed leukocytosis (18300 cells/ul), elevated C-reactive protein, and abnormally elevated serum level of creatinine (2.0 mg/dl). Chest radiograph showed pleural effusion in right lower lung field and interlobar space. Lateral view showed the haziness was mainly located in anterior aspect (Figures 1a and 1b). Subsequent CT scan of the chest showed pneumonic consolidation in the right middle lobe, loculated effusion near mediastinum and some effusions in the dependent pleural cavity (Figure 2a). Figure 2b also showed abscess formation in lung parenchyma. Chest tapping yielded minimal purulent effusion. She was treated for a short course of antibiotics emperically, including cephalosporin of second generation and amyloglycoside because there was no definite pathogen cultured from pleural effusion as well as sputum. Her symptoms of fever, dyspnoea and chest wall pain improved after a 2-week antibiotic treatment and she was discharged home. She came to the outpatient department once a month for follow-up and recovered well.
Figure 1.
Chest radiograph (PA and lateral view) showed haziness in right lower lung field. Figure 1B is the lateral view showing haziness was mainly located in anterior aspect
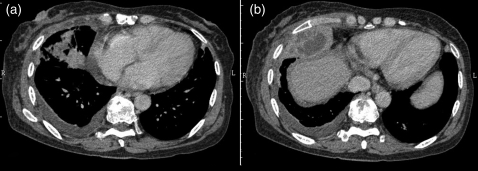
Figure 2.
a. Pneumonic consolidation, loculated pleural effusion. b. Abscess in lung parenchyma
Eight months later, the patient presented fever, up to 39°C, dyspnoea and chest pain. She was brought to the emergency room. Physical examination revealed fever, tachypnea, and pus discharge from the right lower chest wall in anterior aspect. The surrounding skin was also erythematous. She was admitted again. Subsequent CT scan of the chest showed rib erosion, cartilage destruction and necrosis both inside and outside of the chest wall (Figure 3a). Abscess formation was also seen in area of low density in the chest wall on CT scan of the chest (Figure 3b). There was no effusion in the dependent portion of the pleural cavity. Due to severe infection, the patient underwent anterior thoracotomy to open the pleural space. On skin incision, a lot of purulent discharge gushed out. There was one 12x10 cm residual space in the pleural space and chest wall due to collapsed right middle lobe and evacuation of the purulent fluids as well as necrotic soft tissues. The opened pleural space was not communicating to other portion of the pleural space because of dense fibrosis. Lung tissue did not expand adequately to fill the dead space. The space was packed with wet gauzes and prepared for later wound closure. Two destructed ribs were removed and a small portion of the fragile costal cartilages was removed. Debridement of the soft tissues was also performed in the same time.
Figure 3.
a. Destruction of the ribs and costal cartilages. b. chest wall infection from skin into the pleural space
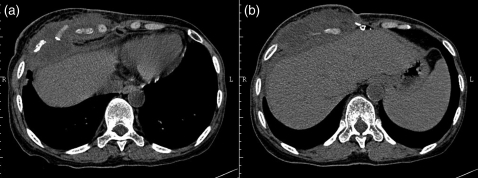
After wound care with open packing for 2 weeks, the dead space became much smaller. The wound was then closed with placement of one tube connecting to a vacuum bag. The drainage tube was removed 5 days after secondary wound closure. The patient was discharged one week later. The resected specimens showed abundant hyphae of Aspergillosis (Figure 4). Serum antigen for Aspergillosis was positive (1.976). When the diagnosis of fungal infection was established, the patient was treated with oral Itraconazole.
Figure 4.
Abundant fungal hyphae are seen in cartilages (a), intercostal muscles (b) and soft tissues in chest wall (c)
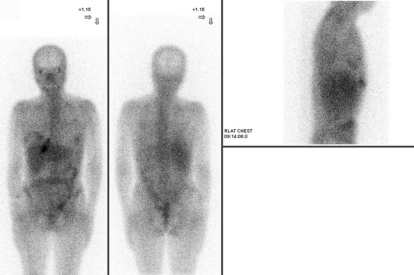
When she came back to the outpatient department, there was still one small wound of poor healing and she still complained of pain in the chest wall. Although the patient remained afebrile and there was no sign of infection in the skin, we worried about the patient's condition. Subsequent inflammation (Gallium) scan, showed active inflammation in the right lower chest wall (Figure 5). Because of persistent poor healing of the wound, the underlying cartilage infection was in doubt. She then was admitted for resection of all right-side costal cartilages, with some muscle tissues and skin in doubt. The wound was closed with a local rotational skin flap. Subsequent pathology confirmed the existence of abundant hyphae of Aspergillosis in these resected regions. The result of polymerase chain reaction for tuberculosis was negative. After 10 days of treatment, the patient was discharged. We continued oral Itraconazole treatment for more than one month after the last operation. After 13-month follow-up, the patient was still alive and has no evidence of recurrence.
Figure 5.
Gallium scan showed active inflammation in the right side of the lower anterior chest wall
Discussion
Fungal infection is a rare cause of empyema thoracis. Bone erosion may sometimes be seen in cases of Actinomycosis.1 Fungal infection of the pulmonary system usually presents with low grade fever and indolent clinical course. Aspergillus empyema was only rarely reported in the literature.2,3 To the best of our knowledge, this is the first reported case of Aspergillosis empyema necessitatis without antecedent surgery or tuberculosis infection. Patients who have Aspergillosis infection usually are immunocompromized. The predisposing factors are diabetes, prior tuberculosis infection, chronic lung disease, receiving chemotherapy, and post-transplantation state, et cetera.4 Aspergillus fumigatus has two forms, including conidiophores and hyphae. The fungus may grow in water, soil, some animal and plants materials. Infection of the lung is usually caused by direct inhalation of the spores. The patient lacks any specific exposure history. Sometimes, Aspergillosis may be found in the destroyed lung after infection of tuberculosis or after a radical operation.5 However, the patient has no such history of tuberculosis and she has no prior history of surgery.
Management of Aspergillosis empyema is very difficult.5 Such fungal infection can be very mild in symptoms but may have extended growing in soft tissues. Antifungal medications, including intravenous Voriconazole or Amphtericin, should be considered in invasive fungal infection.6,7 After extended involvement of soft tissues, successful treatment could only be achieved by radical resection of the involved soft tissues. Without radical resection and prolonged course of anti-fungal medications, treatment may fail. In this patient, we avoided intravenous Voriconazole or Amphotericin because she has chronic renal insufficiency. Costal cartilage extension is another major problem in such a condition. Because costal cartilage is free of abundant blood supply, fungal infection in the cartilages is hardly cured by medications alone.8 Resection, especially radical resection, of the costal cartilage has the highest chance of cure. In the patient's condition, we did not proceed to radical resection of the costal cartilage as we did not know she was infected by Aspergillus fumigatus. She underwent a second operation because of a positive inflammation scan and persistent poor healing of the wound. In brief, empyema necessitatis caused by Aspergillus fumigatus, especially when the cartilages are involved, should be managed with radical resection and anti-fungal medications.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publication was obtained from the patient
Guarantor
C-HC
Contributorship
C-HC wrote the report; C-HC and H-CL performed the surgery; HC and T-TT performed and analysed the PCR results; T-TH collected the patient's clinical and pathological data and references
Acknowledgements
None
Reviewer
Stefan Limmer
References
- 1.Pinarli FG, Mutlu B, Celenk C, et al. Pulmonary actinomycosis mimicking chest wall tumor in a child. Jpn J Infect Dis 2005;58:247–9 [PubMed] [Google Scholar]
- 2.Parry MF, Coughlin FR, Zambetti FX Aspergillus empyema. Chest 1982;81:768–70 [DOI] [PubMed] [Google Scholar]
- 3.Karnak D, Koksal D, Beder S, Kayacan O A rare cause of empyema in a non-immunocompromised case and successful combined treatment. Postgrad Med J 2004;80:184–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samarakoon P, Soubani AO Invasive pulmonary aspergillosis in patients with COPD: a report of five cases and systematic review of the literature. Chron Respir Dis 2008;5:19–27 [DOI] [PubMed] [Google Scholar]
- 5.Lampo N, Spiliopoulos A, Licker M, Tschopp JM Management of postpneumonectomy Aspergillus empyema extending into the thoracic wall: a plea for radical surgery and caution when using liposomal amphotericin B. Interact Cardiovasc Thorac Surg 2003;2:682–4 [DOI] [PubMed] [Google Scholar]
- 6.van't Hek LG, Verweij PE, Weemaes CM, et al. Successful treatment with voriconazole of invasive aspergillosis in chronic granulomatous disease. Am J Respir Crit Care Med 1998;157:1694–6 [DOI] [PubMed] [Google Scholar]
- 7.Krishnan-Natesan S, Chandrasekar PH Current and future therapeutic options in the management of invasive aspergillosis. Drugs 2008;68:265–82 [DOI] [PubMed] [Google Scholar]
- 8.Ontell FK, Moore EH, Shepard JA, Shelton DK The costal cartilages in health and disease. Radiographics 1997;17:571–7 [DOI] [PubMed] [Google Scholar]