Abstract
Background:
Neurocytomas are benign central nervous system tumor composed of small cells with characteristics of neuronal differentiation; they are usually located in the supratentorial periventricular region, in close relation to the septum pellucidum and the foramen of Monro.
Case Description:
Herein we report a rare case of a neurocytoma located in the cerebellar hemisphere. To date there are only four such reported cases.
Conclusion:
Neurocytomas should be considered in the differential diagnosis of mass lesions in the cerebellum.
Keywords: Cerebellar hemisphere, neurocytoma, posterior fossa
INTRODUCTION
Neurocytomas are small cell tumors first described by Hassoun, et al.[10] The characteristics features of this rare tumor include 1) intraventricular location, 2) predominant occurrence in young adults around the third decade, 3) histopathological resemblance with oligodendrogliomas or ependymomas 4) expression of neuron-specific antigens and 5) ultrastructural features of neuronal differentiation.[3,9,10,23,31,33] They comprise 0.1-0.5% of all brain neoplasms and present mostly as supratentorial intraventricular or periventricular tumors.[33] There have been isolated reports of neurocytomas occurring at various sites within the cerebrum or spinal cord.[4,7,18,20,22,26] We report an unusual case of a neurocytoma occurring in the cerebellar hemisphere.
CASE REPORT
A 45-year-old woman presented with intermittent episodes of vertigo and dizziness of 5 years duration. A magnetic resonance (MR) image demonstrated an oblong 2×1.5 cm inferior right cerebellar hemispheric enhancing lesion which showed minimal mass effect [Figure 1]. Owing to our suspicion that the lesion may have represented a high-grade glioma or lymphoma we took the patient for elective needle biopsy with possibility of conversion to an open procedure for tumor resection. An intraoperative smear demonstrated discohesive cells within a delicate neuropil-like background. The nuclei showed some pleomorphism and the chromatin was clock-face to speckled [Figure 2a]. The preliminary diagnosis at the time of surgery was angiotrophic tumor, favoring lymphoma thus prompting the decision not to proceed with craniotomy. Permanent sections revealed a tumor composed of cells with small, round nuclei with speckled chromatin. Both perivascular and intratumoral acellular zones were noted. Mitoses were not identified [Figure 2b]. A Ki67 immunostain showed a very low proliferation index <1% [Figure 2c]. Lymphoma was ruled out with a negative immunostain for CD45 (common leukocyte antigen). The architectural appearance of the tumor made ependymoma a possibility, but immunostains for glial fibrillary acid protein (GFAP) and epithelial membrane antigen (EMA) were negative. A synaptophysin immunostain demonstrated diffuse positivity [Figure 2d]. These histopathological findings were consistent with a low-grade neurocytic tumor. While surgical resection was a consideration, the risks of injury to cerebellospinal tracts and the dentate nucleus were felt to be high. Given the relative paucity of neurologic symptoms, we elected to follow the lesion with periodic MRIs and close neurologic checks. There was no evidence of progression at 14-month follow-up.
Figure 1.
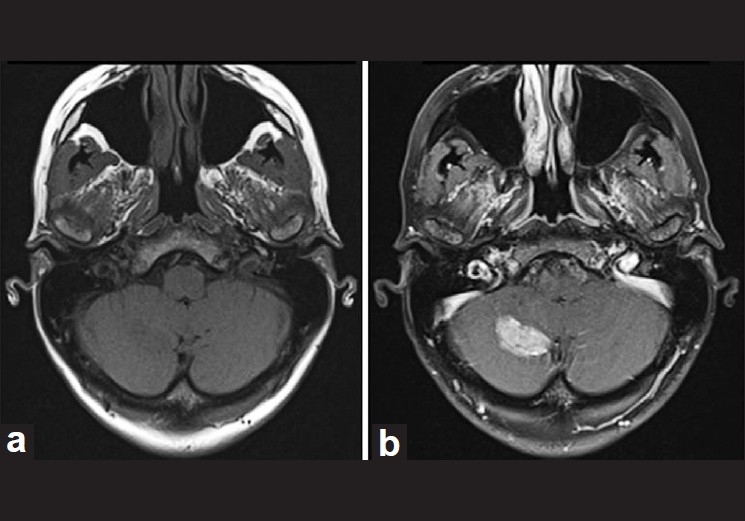
(a) Magnetic resonance imaging demonstrating the tumor in the right cerebellar hemisphere as a hypointense lesion in a T1-weighted image (b) and as a enhancing lesion in a gadolinium T1-weighted image
Figure 2.
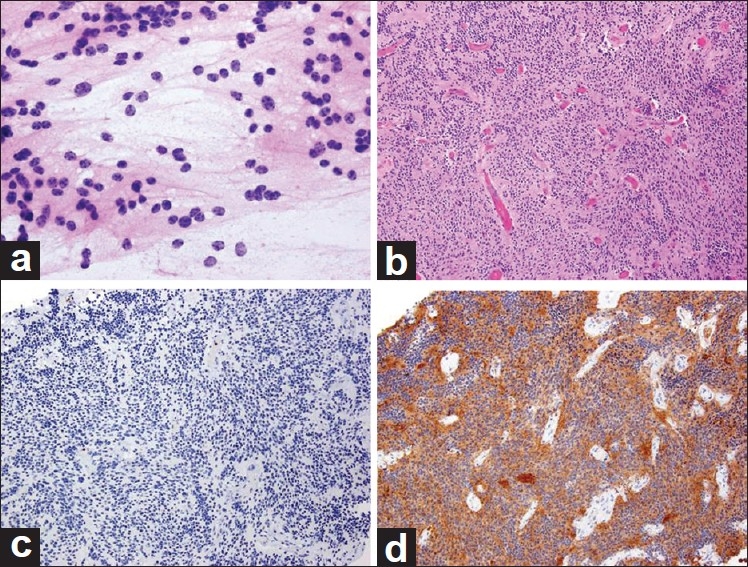
Histology slides. (a) Intraoperative smear (×400) showing discohesive cells with minimal cytoplasm and neurocytic nuclei with speckled chromatin. (b) (H and E, ×100) showing cells with small, round nuclei, minimal pleomorphism and no mitotic activity. Perivascular acellular zones and scattered intratumoral acellular zones, reminiscent of Homer-Wright rosettes were noted. (c) Ki67 immunostain (×100) showing a very low proliferation index <1%. (d) Synaptophysin immunostain (×100) showing diffuse positivity
DISCUSSION
Neurocytomas typically consist of dense areas of small cells with a patchy fibrillary network and demonstrate features of neuronal differentiation. They characteristically demonstrate positive reactivity for neuron-specific enolase and synaptophysin.[3,7,9,11,19,27,31] The differential diagnoses of neurocytoma includes ependymomas, oligodendrogliomas, dysembryoplastic neuroepithelial tumors (DNTs), and lymphoma.[9,17]
Oligodendrogliomas and ependymomas typically do not demonstrate patchy fibrillary stroma. They show a positive reactivity for GFAP and S-100 protein and negative for markers of neuronal differentiation, which are not the characteristics of neurocytomas.[9,29,31] DNTs demonstrate an abundance of ganglion cells and characteristically contain a mucoid matrix that is not observed in neurocytomas.[10,17]
Two additional and rather newly described entities of the cerebellum include rosette-forming glioneuronal tumor (RGNT) of the 4th ventricle and liponeurocytoma. RGNT of the 4th ventricle was first described in a series of 11 patients by Komori et al.[16] They appear to derive from pluripotential cells of the subependymal plate,[28] which could explain the cerebellar midline location in almost all the reported patients. To date there are 30 reported cases of these tumors. There is only one reported case of lateral cerebellar origin of RGNT.[21] Histopathologically, RGNT shows a biphasic neurocytic and glial architecture. RGNT can be differentiated from neurocytomas due to the presence of glial component. Liponeurocytomas are rare and slow-growing tumors located predominantly in the cerebellum.[6] In 2000, the World Health Organization (WHO) classified cerebellar liponeurocytoma as a distinct entity from medulloblastoma in terms of prognostic, epidemiological and clinical aspects. This rare tumor is WHO grade I–II, generally with an accordingly indolent behavior.[15] They occur generally in the cerebellum and are characterized by many lipidized cells found in clusters or scattered between small neoplastic cells. Immunohistochemical staining demonstrates both neuronal and glial differentiation. Mitotic activity is generally low in these lesions.[24] Liponeurocytomas can be differentiated from neurocytomas due to the presence of glial differentiation and lipoid component.
The origin of the neurocytomas is not fully understood. Based on the predominant intraventricular location and properties of neurocytoma cells which can differentiate into both glia and neuron, it has been proposed that they originate from bipotential progenitor cells in the periventricular matrix.[3,12,13,30,32] On the other hand, it was recently reported that neural stem cells, which have the potential to differentiate into astrocytes, oligodentrocytes or neurons, reside not only in the periventricular area of cerebellum but also in the cerebellar cortex.[1,2] We postulate that cerebellar neurocytomas occurrring remote from the ventricle, as in our case, may originate from those neural stem cells in cerebellar cortex.
Surgical biopsy and, when safe, gross total resection is usually recommended as the initial treatment modality for patients with cerebellar neurocytoma. In the presented case, the patient's symptoms did not correlate with her MRI finding. The decision to proceed with biopsy was based on the radiographic suspicion that the lesion might represent a glioma, metastasis, lymphoma, inflammatory condition, or a demyelinating process.
There is no consensus regarding the role of postoperative adjuvant therapy for neurocytomas. In our case given the relatively small size of the lesion and benign pathology, we elected to follow the patient without any adjuvant therapy. Surgical resection will be considered should the lesion grow or symptoms related to the lesion develop.
To date there are only four reported cases of a neurocytoma in the cerebellum, three in the vermis and one in the cerebellar hemisphere.[5,8,14,25] While exceedingly rare, this entity should be considered in the differential diagnosis of enhancing lesions of the cerebellum.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2011/2/1/36/78246
Contributor Information
Hideki Ogiwara, Email: hideki_o@d5.dion.ne.jp.
Steve Dubner, Email: s-dubner@northwestern.edu.
Eileen Bigio, Email: e-bigio@northwestern.edu.
James Chandler, Email: jchandler@nmff.orgp.
REFERENCES
- 1.Alcock J, Lowe J, England T, Bath P, Sottile V. Expression of Sox1, Sox2 and Sox9 is maintained in adult human cerebellar cortex. Neurosci Lett. 2009;450:114–6. doi: 10.1016/j.neulet.2008.11.047. [DOI] [PubMed] [Google Scholar]
- 2.Alcock J, Sottile V. Dynamic distribution and stem cell characteristics of Sox1-expressing cells in the cerebellar cortex. Cell Res. 2009;19:1324–33. doi: 10.1038/cr.2009.119. [DOI] [PubMed] [Google Scholar]
- 3.Barbosa MD, Balsitis M, Jaspan T, Lowe J. Intraventricular neurocytoma: A clinical and pathological study of three cases and review of the literature. Neurosurgery. 1990;26:1045–54. [PubMed] [Google Scholar]
- 4.Brat DJ, Scheithauer BW, Eberhart CG, Burger PC. Extraventricular neurocytomas: Pathologic features and clinical outcome. Am J Surg Pathol. 2001;10:1252–60. doi: 10.1097/00000478-200110000-00005. [DOI] [PubMed] [Google Scholar]
- 5.Brandis A, Heyer R, Hori A, Walter GF. Cerebellar neurocytoma in an infant: An important differential diagnosis from cerebellar neuroblastoma and medulloblastoma? Neuropediatrics. 1997;28:235–8. doi: 10.1055/s-2007-973706. [DOI] [PubMed] [Google Scholar]
- 6.Buccoliero AM, Caldarella A, Bacci S, Gallina P, Taddei A, Di Lorenzo N, et al. Cerebellar liponeurocytoma: Morphological, immunohistochemical, and ultrastructural study of a relapsed case. Neuropathology. 2005;25:77–83. doi: 10.1111/j.1440-1789.2004.00574.x. [DOI] [PubMed] [Google Scholar]
- 7.Coca S, Moreno M, Martos JA, Rodriguez J, Barcena A, Vaquero J. Case report.Neurocytoma of spinal cord. Acta Neuropathol. 1994;87:537–40. doi: 10.1007/BF00294182. [DOI] [PubMed] [Google Scholar]
- 8.Enam SA, Rosenblum ML, Ho KL. Neurocytoma in the cerebellum.Case report. J Neurosurg. 1997;87:100–2. doi: 10.3171/jns.1997.87.1.0100. [DOI] [PubMed] [Google Scholar]
- 9.Figarella-Branger D, Pellissier JF, Daumas-Duport C, Delisle MB, Pasquier B, Parent M, et al. Central neurocytomas.Critical evaluation of a small-cell neuronal tumor. Am J Surg Pathol. 1992;16:97–109. [PubMed] [Google Scholar]
- 10.Hassoun J, Gambarelli D, Grisoli F, Pellet W, Salamon G, Pellissier JF, et al. Central neurocytoma.An electron-microscopic study of two cases. Acta Neuropathol. 1982;56:151–6. doi: 10.1007/BF00690587. [DOI] [PubMed] [Google Scholar]
- 11.Hassoun J, Söylemezoglu F, Gambarelli D, Figarella-Branger D, von Ammon K, Kleihues P. Central neurocytoma: A synopsis of clinical and histological features. Brain Pathol. 1993;3:297–306. doi: 10.1111/j.1750-3639.1993.tb00756.x. [DOI] [PubMed] [Google Scholar]
- 12.Ishiuchi S, Nakazato Y, Iino M, Ozawa S, Tamura M, Ohye C. In vitro neuronal and glial production and differentiation of human central neurocytoma cells. J Neurosci Res. 1998;51:526–35. doi: 10.1002/(SICI)1097-4547(19980215)51:4<526::AID-JNR12>3.0.CO;2-1. [DOI] [PubMed] [Google Scholar]
- 13.Ishiuchi S, Tamura M. Central neurocytoma: an immunohistochemical, ultrastructural and cell culture study. Acta Neuropathol (Berl) 1997;94:425–35. doi: 10.1007/s004010050729. [DOI] [PubMed] [Google Scholar]
- 14.Kapoor N, Gandhi A, Chaurasia AK. Central neurocytoma in the vermis of the cerebellum. Indian J Pathol Microbiol. 2009;52:108–9. doi: 10.4103/0377-4929.44989. [DOI] [PubMed] [Google Scholar]
- 15.Kleihues P, Cavenee WK, editors. Vol. 1. Lyon, France: International Agency for Research on Cancer; 2000. Pathology and genetics of tumours of the nervous system. World Health Organization Classification of Tumours. [Google Scholar]
- 16.Komori T, Scheithauer BW, Hirose T. A rosette-forming glioneuronal tumor of the fourth ventricle. Am J Surg Pathol. 2002;26:582–91. doi: 10.1097/00000478-200205000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Leung SY, Gwi E, Ng HK, Fung CF, Yam KY. Dysembryoplastic neuroepithelial tumor. A tumor with small neuronal cells resembling oligodendroglioma. Am J Surg Pathol. 1994;18:604–14. [PubMed] [Google Scholar]
- 18.Louis DN, Swearingen B, Linggood RM, Dickersin GR, Kretschmar C, Bhan AK, et al. Clinical study.Central nervous system neurocytoma and neuroblastoma in adults-report of eight cases. J Neurooncol. 1990;9:231–8. doi: 10.1007/BF02341154. [DOI] [PubMed] [Google Scholar]
- 19.Maiuri F, Spaziante R, De Caro ML, Cappabianca P, Giamundo A, Iaconetta G. Central neurocytoma: Clinico-pathological study of 5 cases and review of the literature. Clin Neurol Neurosurg. 1995;97:219–28. doi: 10.1016/0303-8467(95)00031-e. [DOI] [PubMed] [Google Scholar]
- 20.Miller DC, Kim R, Zagzag D. Neurocytomas: Non-classical sites and mixed elements. J Neuropathol Exp Neurol. 1992;51:364. [Google Scholar]
- 21.Marhold F, Preusser M, Dietrich W, Prayer D, Czech T. Clinicoradiological features of rosette-forming glioneuronal tumor (RGNT) of the fourth ventricle: Report of four cases and literature review. J Neurooncol. 2008;90:301–8. doi: 10.1007/s11060-008-9661-y. [DOI] [PubMed] [Google Scholar]
- 22.Nishio S, Takeshita I, Kaneko Y, Fukui M. Cerebral neurocytoma.A new subset of benign neuronal tumors of the cerebrum. Cancer. 1992;70:529–37. doi: 10.1002/1097-0142(19920715)70:2<529::aid-cncr2820700225>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 23.Nishio S, Tashima T, Takeshita I, Fukui M. Intraventricular neurocytoma: Clinicopathological features of six cases. J Neurosurg. 1988;68:665–70. doi: 10.3171/jns.1988.68.5.0665. [DOI] [PubMed] [Google Scholar]
- 24.Owler BK, Makeham JM, Shingde M, Besser M. Cerebellar liponeurocytoma. J Clin Neurosci. 2005;12:326–9. doi: 10.1016/j.jocn.2004.05.017. [DOI] [PubMed] [Google Scholar]
- 25.Pal L, Santosh V, Gayathri N, Das S, Das BS, Jayakumar PN, et al. Neurocytoma/rhabdomyoma (myoneurocytoma) of the cerebellum. Acta Neuropathol. 1998;95:318–23. doi: 10.1007/s004010050805. [DOI] [PubMed] [Google Scholar]
- 26.Polli FM, Salvati M, Miscusi M, Delfini R, Giangaspero F. Neurocytoma of the spinal cord: Report of three cases and review of the literature. Acta Neurochir (Wien) 2009;151:569–74. doi: 10.1007/s00701-009-0305-6. [DOI] [PubMed] [Google Scholar]
- 27.Robbins P, Segal A, Narula S, Stokes B, Lee M, Thomas W. Central neurocytoma.A clinicopathological, immunohistochemical and ultrastructural study of 7 cases. Pathol Res Pract. 1995;191:100–11. doi: 10.1016/S0344-0338(11)80559-5. [DOI] [PubMed] [Google Scholar]
- 28.Rosenblum MK. The 2007 WHO classification of nervous system tumors: Newly recognized members of the mixed glioneuronal group. Brain Pathol. 2007;17:308–13. doi: 10.1111/j.1750-3639.2007.00079.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tzaan WC, Ho YS, Chang CN, Lin TK, Wong CW. Intraventricular neurocytoma: Four cases report. J Neurooncol. 1992;13:239–46. doi: 10.1007/BF00172476. [DOI] [PubMed] [Google Scholar]
- 30.Vallat-Decouvelaere A, Gauchez P, Varlet P, Delisle M, Popovic M, Boissonnet H, et al. Socalled malignant and extra-ventricular neurocytomas: Reality or wrong diagnosis. A critical review about two overdiagnosed cases. J Neurooncol. 2000;48:161–72. doi: 10.1023/a:1006494308864. [DOI] [PubMed] [Google Scholar]
- 31.von Deimling A, Janzer R, Kleihues P, Wiestler OD. Patterns of differentiation in central neurocytoma.An immunohistochemical study of eleven biopsies. Acta Neuropathol. 1990;79:473–9. doi: 10.1007/BF00296105. [DOI] [PubMed] [Google Scholar]
- 32.Westphal M, Stavrou D, Nausch H, Valdueza JM, Herrmann HD. Human neurocytoma cells in culture show characteristics of astroglial differentiation. J Neurosci Res. 1994;38:698–704. doi: 10.1002/jnr.490380612. [DOI] [PubMed] [Google Scholar]
- 33.Yasargil MG, von Ammon K, von Deimling A, Valavanis A, Wichmann W, Wiestler OD. Central neurocytoma: Histopathological variants and therapeutic approaches. J Neurosurg. 1992;76:32–7. doi: 10.3171/jns.1992.76.1.0032. [DOI] [PubMed] [Google Scholar]


