Synopsis
This paper reports findings from a qualitative study that explored the attitudes and beliefs concerning colorectal cancer screening (CRC) among patients and health care providers in Appalachian Kentucky. We report results from five focus groups; three with primary care providers and two with patients. Providers discussed patient characteristics, financial issues and health care delivery system factors as challenges to screening. Participants reported fear, embarrassment, financial issues, lack of perceived need, qualities of the test, lack of provider recommendation, and health care delivery barriers. Although there were some areas of agreement, there are marked differences between the perceptions of Appalachian health care providers and participants regarding colorectal cancer screening. This paper compares and contrasts those perceptions and provides suggestions for culturally competent practice and culturally relevant research to improve CRC screening in this vulnerable population.
Keywords: Appalachian Kentucky, colorectal cancer, colonoscopy, rural
Introduction
Kentucky has the 2nd highest cancer death rate in the United States, with colorectal cancer (CRC) being one of the leading contributors to that excess mortality rate.1 The cancer burden for the rural Appalachian population, which comprises 54 of the 120 counties in Kentucky, is even higher than that of Kentucky in general. For the period 2000–2005, the age-adjusted mortality rate from all cancers for Kentucky 222.1/100,000, compared to 235.1/100,000 for the Appalachian region of the state.2 Colorectal cancer is also notable because mortality rates are elevated in Kentucky for both sexes. Furthermore, colorectal cancer screening represents an ideal opportunity to focus cancer control on both primary and secondary prevention as screening allows for detection and removal of colorectal polyps before they progress to cancer as well as early cancers themselves. Although screening guidelines for CRC are widely publicized, US screening rates remain extremely low with the Centers for Disease Control (CDC) reporting that fewer than 40% of CRC cases are found early.3
Colorectal cancer screening rates are low in Appalachia for a number of reasons. Appalachia, particularly the central Appalachian region that includes Kentucky, suffers from higher unemployment, fewer college graduates, higher poverty rates, lower levels of health insurance coverage, greater shortages of health care providers, and underfinanced health services. These factors have been found to have a significant negative impact on screening rates. 4 In addition, access to health care services, particularly the specialty care needed to provide endoscopic CRC screening tests, is limited in the Appalachian region. Behavioral Risk Factor Surveillance System survey data indicate that Kentuckians age 50 and older are less likely than residents of other states to report having had a blood stool test within the past two years (24% compared to 26.5% nationwide).3 For flexible sigmoidoscopy or colonoscopy, the difference in self-reported screening is more pronounced, with 47.2% of Kentucky respondents reporting ever having either flexible sigmoidoscopy or colonoscopy compared to 53.5% for the US. Since low screening rates are associated with elevated mortality rates, improved understanding of factors that impede screening is a key element in reducing mortality.
Few studies have examined the unique barriers to CRC screening for rural Appalachians. Wackerbarth and associates explored the factors that influence decision making regarding CRC screening among persons in non-Appalachian Kentucky.5 They conducted 30 semi-structured interviews with screened and unscreened persons between the ages of 48 and 55. Ten themes emerged from their research representing a wide range of concerns, including structural issues, the nature of the screening tests, individual’s health beliefs, and psychological issues. The researchers suggested as a next step that these findings be compared to perspectives of Appalachian residents.
There are also few studies that provide insight into the unique perspective of health care providers regarding CRC screening in this part of the country.6 Researchers used mixed methods to explore the perceptions of providers and staff from five primary care practices in rural Appalachian Kentucky. These health care providers participated in focus groups and completed surveys regarding the CRC screening practices of the patients in their practices. Physician/practice barriers included limited time, more pressing medical concerns, and reimbursement issues. They perceived the patient issues to include fear and embarrassment as primary barriers. In addition, providers questioned the importance of following US Preventive Services Task Force guidelines versus using personal experience when recommending screening for this population given many of their unique circumstances and beliefs. The purpose of this study is to explore the attitudes and beliefs concerning CRC screening among patients and health care providers in rural Appalachian Kentucky. The findings will be useful in developing culturally acceptable interventions to promote CRC screening among persons in this region.
Methods
Setting
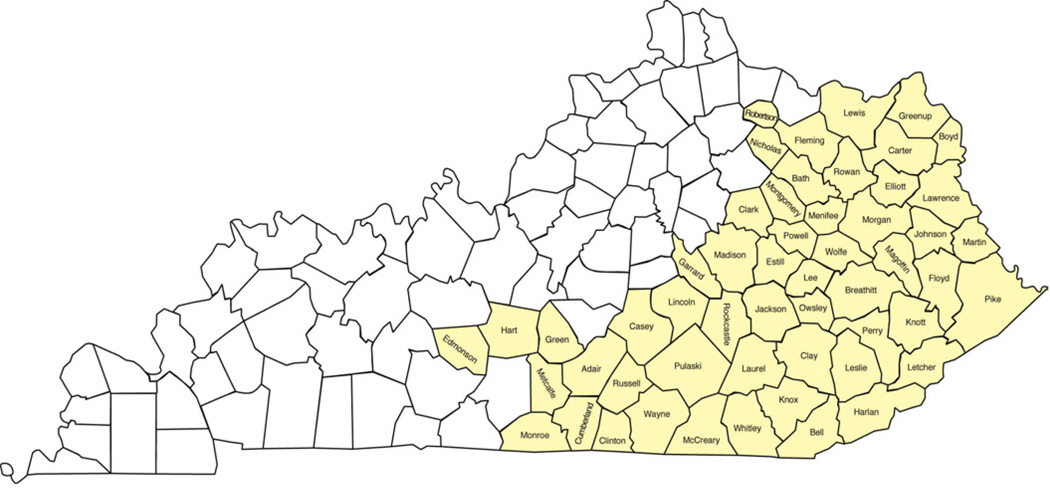
This study was conducted in rural Appalachian Kentucky (See Figure 1). This region has long been characterized by picturesque mountainous terrain, but limited road systems, isolation, high rates of poverty, and poor health.7 Even though conditions have improved since the “War on Poverty” and other “Great Society” programs that were initiated in the 1960s, economic, educational, and health disparities persist.8 The condition of the health care delivery system in Appalachian Kentucky is consistent with the economic conditions in the region. There has been a chronic shortage of health care providers and the services that are provided are often underfinanced. As a result, provision of preventive health services falls heavily on the public health system.9,10
Figure 1.
Appalachian Counties in Kentucky
To elicit a broad range of factors that shape perceptions about screening for colorectal cancer from the provider and patient points of view, we conducted five focus groups, three with primary care providers and two with patients. In addition to exploring the barriers to colorectal cancer screening according to guidelines, the focus groups elicited preferences for particular screening modalities among participants. The providers were asked about methods of enhancing screening in practice environments. We elected to undertake focus groups because of their potential to capture unrehearsed thoughts, feelings and opinions, and capitalize on the discussions of others.11,12
We included primary care providers because of their critical role in the screening process, and because health care in Appalachian Kentucky is provided mostly by primary care providers. Specialists who perform colorectal screening (flexible sigmoidoscopy or colonoscopy) are in short supply. Provider recommendation has been demonstrated to be a key factor in encouraging patients to obtain cancer screening.13 To enhance the generalizability of our findings, we chose to conduct focus groups with providers and patients in several different geographic areas of Appalachian Kentucky.
Sample and recruitment
We employed theoretical sampling, selecting participants on the basis of their potential ability to contribute to issues at hand, rather than attempting to recruit a representative sample.14 To garner a full range of input, we included different types of relevant health care providers (nurses, general practice physicians, specialists, office managers) in a variety of practice settings (private clinics, local health departments, federally-qualified community health centers) and involved a broad cross section of participants (varying in income, education, occupation, health status).
Participants were recruited for the three provider focus groups through letters and follow-up telephone calls. The process began with development of a list of providers compiled through interactions with the Kentucky Medical Association and Kentucky Medical Licensure databases. Our research team reviewed the list and a diverse group of providers was contacted to participate in the study. The sample was selected to ensure geographic representation, to include providers in both solo and group practice, and to limit selection to those in adult primary care (general practice, family medicine, and general internal medicine).
Patient focus group participants were recruited through posting announcements in clinic waiting rooms and with the assistance of a community advisory board. Community advisory board members disseminated information about the focus groups through social and civic groups and worksites. We conducted two patient focus groups, one with those who had undergone screening within the past year and one with those who had been rarely (not within the past five years) or never screened for colorectal cancer. We organized the groups by screening status to make sure that we captured the views of unscreened individuals, as prior research suggests that the views of screened and unscreened persons may differ in important ways.15Upon acceptance of our invitation to join a luncheon or dinner and discussion of colorectal cancer issues, we arranged a convenient location and time.
Data Collection
Upon arrival, investigators greeted focus group participants, administered informed consent procedures, and answered all questions or concerns. Following these activities, we administered a brief sociodemographic questionnaire. The moderator then provided a general introduction to the focus group process, followed by a series of open-ended questions focusing on the barriers to colorectal cancer screening, knowledge of and perspectives about the various screening techniques, and, for the providers, methods of increasing screening in practices. The discussions lasted approximately 60–120 minutes, depending on the level of detail provided by the participants and the group dynamics. All protocols and procedures were approved by the institutional review board at the University of Kentucky.
Data Processing and Analysis
All sessions were tape recorded and professionally transcribed. Two qualitatively trained researchers independently reviewed the transcripts multiple times and data were content analyzed. We identified core categories of emerging substantive findings after conducting line-by-line analysis. These categories guided our initial coding, and eventually lead to the development of a codebook.16Several iterations of the codebook and repeated discussions on the interpretations of data enhanced the rigor of the process. Qualitative analysis tends to be recursive; thus, data collection, immersion in the transcripts, and subsequent coding and development of a codebook were carried out simultaneously.17
We did not use any qualitative data analysis software; however, we took several additional steps to insure the rigor and trustworthiness of the data analysis. First, the moderators and assistants supplied memo-writing and field observations. Second, we conducted member checks with the interview staff, most of whom reside in the Appalachian communities in which the focus groups occurred. Finally, we employed coding techniques to enhance the rigor in our data interpretation. Specifically, all of the transcripts were co-coded by at least two qualitative researchers using the codebook we developed, eventually leading to overall agreement in coding.
Results
The provider focus group participants included primary care physicians, physician assistants and nurse practitioners. The two patient focus groups included participants age 50 and older, without a history of colorectal cancer, and with a variety of education and income levels. A total of five focus groups were conducted, three with primary care providers and two with patients. The primary care provider focus groups ranged in number from five to seven participants. The patient focus groups included one group of 6 participants and one group of 11. The focus groups were conducted as planned, but although we framed our questions to address general perspectives on colorectal cancer screening each group quickly gravitated toward discussing colonoscopy as the only ‘good’ method of screening for colorectal cancer. Thus, in this paper we present data on provider and non-provider perspectives on colonoscopy, specifically focusing on perceived merits and limitations of this screening modality.
Results from Primary Care Provider Focus Groups
The providers identified two main categories of challenges to rural Appalachian patients’ receipt of CRC screening, especially colonoscopy. These include the overall categories of (1) patient characteristics and circumstances and; (2) health care delivery factors, including reimbursement issues.
Providers frequently described patient characteristics and circumstances that undermine screening. These characteristics include having multiple diseases that are given higher priority than prevention, patient perceptions of mistrust of the medical establishment, and lack of resources. In a population that tends to suffer from serious, complicated chronic conditions, like diabetes, COPD, and heart disease, prevention is often considered to be of less importance than treatment. The following statements represent provider perspectives on barriers associated with patient characteristics:
“Because they’re here for other medical problems and if they are quite sick with their heart or diabetes, you sometimes get so pulled up in that that you forget the preventative things.”
“It (screening) has to be physician initiated so you have a large population who has minimal physician contact, then you have those who come in with other concerns at that time, then they don’t raise that issue and as physicians, we kind of focus initially on what the chief complaint is at that time.”
In addition, the providers felt that there were cultural/attitudinal issues preventing screening, including perceptions that cancer is a death sentence, mistrust of providers other than patients’ “own doctor”, and lack of “appropriate” priorities. For example, one provider noted,
“There’s a kind of a cultural thing here. I don’t know exactly how to describe it or articulate it. A lot of the people up in here prefer to deal with people they know. I think folks up in this part of the hills are particularly reluctant to go anywhere else unless they absolutely have to.”
Providers also recognized that patients’ financial concerns, specifically the inability of patients to afford copayments and deductibles, were barriers to CRC screening.
“Without a diagnosis, the insurance won’t pay for just a routine colonoscopy or sigmoidoscopy at the very minimum, so that’s probably the biggest roadblock …”
Many providers noted that colonoscopy is so expensive that they do not often recommend it for their patients who lack health insurance, a considerable portion of this patient population. Even for those with health insurance, providers sometimes are reluctant to suggest the procedure, knowing that out of pocket costs may be prohibitive.
“Someone just close to me had one done … we have insurance and it was still around $300.00 or $400.00 with the deductibles and the copays…”
Providers also pointed to characteristics of the colonoscopy that they felt undermined patient acceptability of screening. In addition to the costs of the procedures, providers believed that many of their patients would find the preparation for the procedure unacceptable, or that the procedure itself would deter patients from pursuing colonoscopy.
Another theme that emerged that undermined screening involved health care delivery system barriers, including the lack of reimbursement for CRC screening counseling and the inadequate supply of specialist providers.
“The single most basic thing is that there are little, very few financial rewards for doing it. The, our healthcare system, just what I said before, isn’t set up to encourage preventive care.”
“There’s no reimbursement for sitting down and discussing all that with the patient.”
Yet another theme that emerged involved the inadequate supply of specialist providers capable of undertaking colonoscopy. Lacking gastroenterologists or others who have the specialized training and equipment to perform colonoscopy, patients must seek care outside of their counties. Providers complained that patients had to travel long distances to visit a gastroenterologist.
“Its 45 to 60 minutes to the closest doctor that does them. This requires a great deal of advanced planning, reliable transportation, and acceptance of the hassle and costs associated with traversing mountain roads.”
Compounding that, the specialized care often carried a higher co-payment than other services causing financial strain,
“It’s difficult for them to travel, difficult for them to pay the co-payment and all that…”
Furthermore, providers suggested that so many people lack even a general practice provider that it is unlikely many patients would obtain a referral to a specialist.
Results from Patient Focus Groups
The patient focus groups provided a more expansive description of challenges to colonoscopy than the primary care provider groups. These could broadly be categorized as residing in their own characteristics, features of the screening tests themselves, and provider and health care system factors. Participants conceptualized their own barriers as fear, inadequate knowledge, distrust of the medical system and providers, and to a lesser degree than anticipated, financial limitations, and more pressing health concerns.
Fear and lack of knowledge regarding screening guidelines were viewed as important challenges to patients receiving CRC screening. Many focus group members indicated that they preferred not to know if they had the disease for fear it was a “death sentence”.“Now I also think people are afraid. If they have problems, they’re afraid to have it because they’re afraid they will have cancer.”
Lack of knowledge and confusion regarding the guidelines surrounding CRC screening were also important factors influencing receipt of screening. People also were uncertain if they needed the test if they did not have a family history of colorectal cancer.
“…We don’t have a history of that in my family…well it’s every other generation. I do emphasize it for them (children), even though I don’t think about it for me because there’s no history there in my family. If there was a history, I probably would’ve already had one.”
Although patients did mention financial issues, they did not see this as a barrier as much as the other issues surrounding CRC screening; however, patients often felt that the providers were not recommending or offering screening due to a lack of financial incentive. One person stated “they probably don’t have the machinery that they can get paid a high price for to get it done.” In addition, if their insurance wouldn’t pay, they felt the test was not being recommended “they’re very picky about that. Can you afford it, because your insurance won’t cover it?”
Finally, as mentioned by providers, patients did not see the test as a priority given other more pressing health concerns or a general lack of prioritizing physician visits.
“Sometimes with me, it may be because I’m there with another problem and sort of in dire straits and I probably don’t catch them at a good time to suggest it…I more or less go to the doctor when I am sick.“
“That’s probably why I don’t get screening. I was raised; don’t go to the doctor unless you’re sick.”
Consistent with the provider focus groups, patients described how perceptions of the test itself undermined screening (discomfort of preparation, embarrassment, lack of conclusiveness). The most commonly cited barrier for patients was the procedure, including the preparation for the test and the embarrassment of having colonoscopy performed. As these patients indicate,
“I just dread the, getting ready for the test and then having the test…”
“You hear so many horror stories and from seeing the procedure done several, many times over myself, I know it can’t be pleasant.”
Because of the discomfort associated with the test itself, some persons were hoping that a less invasive test would soon be available. “I’ve been waiting for that new thing comes along. Where you could swallow it and it takes pictures of you…”
Limitations inherent in the health care delivery system compounded perceptions that the test is invasive and embarrassing due to the perceived lack of privacy in the rural Appalachian setting. Many patients suggested that this lack of privacy and the limited pool of health care providers increased the likelihood that someone you know might perform this awkward procedure. One person stated that although she could afford the test and knew she should have it done, she didn’t because “I have to see those people.” Another stated “It’s not that I’m really embarrassed to have it done. It’s just that I don’t want them seeing me” One woman stated, “…you’re laying on the table, not a stitch on anywhere. If I’d have had a bag to put over my head, I’d have put it on.”
There was also concern about the confidentiality of medical information in the community. One person described an experience with having a screening test done and waiting for the results.
“I worried all evening. I mean I can remember walking in and out of the hall, worrying about it and wondering what my results were going to be and I come to work the next morning and one of my coworkers told me all about my results.”
In addition, lack of provider recommendation played a crucial role in perceived need for screening. In one focus group of eleven persons, only one had a doctor who recommended screening. Many said that the doctor only recommended CRC screening if the patient had a family history or were symptomatic. In addition, CRC screening was not as commonly recommended as other tests:
“I do get letters from my doctor saying, you need the mammogram or your pap smear and you need your cholesterol checked but I have never gotten anything about colorectal cancer.”
“I’ll mention it to her (physician) and she’ll say, well if it’s not in your family and you’ve not had any problems…she’s not really said you need to go do that.”
“I just had my yearly checkup and she didn’t mention it. “
“If you had a family member that had colon cancer, they’d probably push it more.”
In sum, the patient/non-provider focus groups included three categories of challenges: patient characteristics, the screening test itself, and the provider or health care system. These concerns appeared to be additive—colonoscopy constitutes a little known and rarely recommended procedure that may prevent a relatively unknown cancer through an unpleasant, unavailable, costly, and inconvenient procedure. Non-providers expressed concern with issues surrounding the test itself, including privacy issues related to living in a close-knit community with few qualified specialists. Participants also emphasized a lack of screening advocacy on the part of providers, a concern amplified due to more pressing health concerns or even more frequently recommended screening tests such as mammography.
Discussion
The purpose of this study was to explore the factors that influence CRC screening, particularly colonoscopy, among rural Appalachian Kentuckians. The results from this study may help to improve our understanding of the unique factors and circumstances that impede or facilitate the adoption of colonoscopy in Appalachian Kentucky. To our knowledge, such insights have not been previously reported.
One of the most intriguing findings from these focus groups was the emphasis on colonoscopy as the predominant or even exclusive screening method for colorectal cancer, to the exclusion of other screening modalities. Without prompting by the focus group moderators, colonoscopy emerged as the predominant colorectal cancer screening test of interest. Few comments were directed toward any other screening modality. Providers noted that fecal occult blood testing (FOBT) is not considered to be a useful test because any positive result ultimately would need to be resolved with colonoscopy. Most of the providers indicated that they had been trained in flexible sigmoidoscopy and several had performed it in their practices in the past. They no longer provided flexible sigmoidoscopy for two reasons; (1) positive findings would require a referral for colonoscopy and (2) reimbursement rates are too low to make providing flexible sigmoidoscopy financially viable for their practices. However, this may not be a limitation in availability of screening since colonoscopy is the preferred endoscopic procedure.
Residents of rural Appalachia provided several important and unique insights regarding their challenges to CRC screening. As previous research has suggested, physician recommendation plays an important role in influencing CRC screening.13 While this finding was reinforced by the findings in this study there were also issues specific to Appalachia that emerged in this regard. Confusion regarding screening recommendations was clearly expressed, as it was not often not clear to patients that their providers recommended screening. This perceived ambiguity translated into a lack of prioritization of colonoscopy by the patients.
Previous research also points to embarrassment and fear as important barriers to colonoscopy from a patient perspective, especially among certain cultural groups. This finding, while evident in this population, is layered with the close-knit community structure that is present in much of rural Appalachia. Concerns about maintaining privacy in these communities is a commonly voiced concern.18,19 Persons worry that the provider is their friend or neighbor and that their privacy could be compromised by providers or their staff members.
Providers also listed a variety of barriers as reasons for patients not being screened, most of which focused on patient characteristics and the health care delivery system. Consistent with previous qualitative studies of general cancer screening in Appalachia, guidelines were an area of concern for providers.5, 6 Interestingly, few of the barriers providers cited described shortcoming in their own behaviors or practice patterns. Concerns were expressed among health care providers about whether certain procedures and counseling would be reimbursed.6
While there were several areas where providers and patients agreed in their perceptions about colorectal cancer screening in rural Appalachian, there were also marked differences in what each group perceived to be the primary barriers to screening.
Both groups expressed a variety of challenges to CRC screening, however, patients, unlike providers cited the most important barriers as those that had to do with the experiences they perceived to be associated with obtaining screening and with health care providers. Providers and non-providers alike both emphasized financial concerns as important factors hindering colorectal cancer screening. While patients’ financial concerns focused on whether physician practices would be reimbursed (if not, many maintained, they would be reluctant to recommend the screening), the financial concerns expressed by providers focused on the poverty of their patients and low rates of reimbursement. This divergence in financial concerns should prompt discussions between providers and patients regarding reimbursement issues, with providers being careful to clarify the reasons for their recommendations (or lack thereof) for care.
Another important area of divergence involved provider recommendation of CRC screening. Although providers reported that they routinely recommended colonoscopy, patients mentioned a lack of provider recommendation for screening. While patients reported that they received both oral and written recommendations and reminders to obtain other screening tests such as mammograms, they reported receiving few colorectal cancer screening recommendations. This emphasis on other screenings may have led to the assumption by patients that CRC screening is not really necessary. Since receiving physician recommendations is generally viewed as a key influence in the uptake of screening, this inconsistency or even lack of recommendation should be addressed both in enhanced research and clinical practice.20, 21
While both patients and providers agreed that CRC screening was a relatively low priority issue in the overall context of health care for this population, the reasons for its lack of importance were slightly different. Both groups agreed that more pressing health concerns often preclude focusing on screening, with patients suggesting that they are not encouraged to be screened for CRC unless they experience symptoms or have a family history of colorectal cancer. Providers, on the other hand, reported that they nearly always advised their patients to obtain colorectal cancer screening and that in the face of the other more pressing health concerns patients postponed or neglected CRC screening. Although having pressing health issues is indeed problematic at times, the presentation of persons with multiple morbidities could be seen as an opportunity to advocate for screening since patients are in the health care setting anyway. Providers should take this opportunity to discuss CRC screening and other preventive care measures with patients.
Although many of the challenges to screening reported here apply to other populations, several factors pertain specifically to rural and Appalachian populations such as health care professional shortages including a lack of accessibility of specialists trained to perform colonoscopy and concerns with privacy and anonymity in small close knit communities. Researchers and practitioners should be aware of these cultural considerations when developing plans of care and interventions designed to promote CRC screening among this unique population. Future studies should focus on practical solutions to address these issues.
The results from this study also suggest that in rural Appalachia there are marked differences between the perceptions of health care providers and patients regarding colorectal screening. These areas of agreement and disagreement present both opportunities and challenges for those concerned with increasing screening. Patients and providers seemed to agree that colorectal cancer is a salient health issue in Appalachian Kentucky and screening is an important objective. However, they disagreed regarding a critical issue: the strength and clarity of provider recommendation. Although the provider focus groups indicated that they recommend colonoscopy to their patients, the patient focus groups generally refuted this claim. Previous research on breast cancer screening suggests that clear messages from providers are necessary to increase mammography and we can assume the same applies for other types of cancer screening, such as that for CRC.22 Practitioners in this area should place special emphasis on discussions regarding CRC screening and be sure that the language being used is consistent with cultural norms. They should also listen carefully for cues from the patients that they are aware of the importance of CRC screening. Involving lay health workers or other community members in messaging may also provide help with this issue.
Finally, the emphasis on colonoscopy as THE screening test for colorectal cancer is problematic in Appalachian Kentucky. The limitation of recommendations to colonoscopy, arguably the most expensive and least available screening modality in Appalachian Kentucky, raises an important issue requiring additional research: Is screening with methods with lower sensitivity better than no screening at all? Or, are the human and financial costs associated with screening using an imperfect test too great to be justifiable?
We acknowledge several limitations. First, our sample size and selection approach limits the generalizability of our findings. Second, because data collection took place in rural Appalachian Kentucky, it is unclear whether our results reflect screening influences that are specific to Appalachia or simply to a rural environment. We suspect that the confluence of rural and Appalachia fosters additive challenges to obtaining screening. Finally, since we did not use medical records, we are unable to verify patients’ screening status and providers’ claims of having given their patients screening recommendations. Despite these limitations, our results provide among the first published insights on patient and provider perspectives on CRC screening in the highly burdened region of Appalachia.
Acknowledgments
This work was supported by a grant from the National Cancer Institute # CA 11932
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The authors have nothing to disclose.
References
- 1.Cancer Facts & Figures. American Cancer Society; 2009. [Google Scholar]
- 2.Kentucky Cancer Registry. Age-Adjusted Cancer Mortality Rates in Kentucky. 2009 http://cancer-rates.info/ky/index_mort.php.
- 3.Centers for Disease Control. [Accessed September 20, 2008];Behavior Risk Factor Surveillance System Survey Data. 2007 http://www.cdc.gov/cancer/colorectal/statistics/screeningrates.htm.
- 4.Centers for Disease Control and Prevention. Screening for Colorectal Cancer - United States, 1997. 1999 February 19; [Google Scholar]
- 5.Wackerbarth SB, Peters JC, Haist SA. "Do we really need all that equipment?": factors influencing colorectal cancer screening decisions. Qual Health Res. 2005;15(4):539–554. doi: 10.1177/1049732304273759. [DOI] [PubMed] [Google Scholar]
- 6.Kelly KM, Phillips CM, Jenkins C, et al. Physician and staff perceptions of barriers to colorectal cancer screening in Appalachian Kentucky. Cancer Control. 2007;14(2):167–175. doi: 10.1177/107327480701400210. [DOI] [PubMed] [Google Scholar]
- 7.Behringer B, Friedell GH. Appalachia: where place matters in health. Prev Chronic Dis. 2006;3(4):A113. [PMC free article] [PubMed] [Google Scholar]
- 8.Appalachian Regional Commission. Report to the Appalachian Regional Commission. Washington D.C.: United States Government Print Office; 1966. [Google Scholar]
- 9.Biola H, Pathman DE. Are there enough doctors in my rural community? Perceptions of the local physician supply. J Rural Health. 2009;25(2):115–123. doi: 10.1111/j.1748-0361.2009.00207.x. [DOI] [PubMed] [Google Scholar]
- 10.Thompson MJ, Hagopian A, Fordyce M, et al. Do international medical graduates (IMGs) "fill the gap" in rural primary care in the United States? A national study. J Rural Health. 2009;25(2):124–134. doi: 10.1111/j.1748-0361.2009.00208.x. [DOI] [PubMed] [Google Scholar]
- 11.Basch CE. Focus group interview: an underutilized research technique for improving theory and practice in health education. Health Educ Q. 1987;14(4):411–448. doi: 10.1177/109019818701400404. [DOI] [PubMed] [Google Scholar]
- 12.Morgan D, editor. Designing focus group research. Newbury Park, CA: Sage; 1992. Tools for primary care. [Google Scholar]
- 13.Sabatino SA, Burns RB, Davis RB, et al. Breast cancer risk and provider recommendation for mammography among recently unscreened women in the United States. J Gen Intern Med. 2006;21(4):285–291. doi: 10.1111/j.1525-1497.2006.00348.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schwandt T. Dictionary of Qualitative Inquiry. Thousand Oaks, CA: Sage; 2001. [Google Scholar]
- 15.Friedemann-Sanchez G, Griffin JM, Partin MR. Gender differences in colorectal cancer screening barriers and information needs. Health Expect. 2007;10(2):148–160. doi: 10.1111/j.1369-7625.2006.00430.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Maxwell J. Qualitative Research Design: An Interactive Approach. 2nd ed. Thousand Oaks, CA: Sage; 2005. [Google Scholar]
- 17.Strauss ACJ. Basics of Qualitative Research: Grounded Theory Procedure and Techniques. Thousand Oaks, CA: Sage; 1990. [Google Scholar]
- 18.Allan J, Ball P, Alston M. 'You have to face your mistakes in the street': the contextual keys that shape health service access and health workers' experiences in rural areas. Rural Remote Health. 2008;8(1):835. [PubMed] [Google Scholar]
- 19.Leach CR, Schoenberg NE. The vicious cycle of inadequate early detection: a complementary study on barriers to cervical cancer screening among middle-aged and older women. Prev Chronic Dis. 2007;4(4):A95. [PMC free article] [PubMed] [Google Scholar]
- 20.Ye J, Xu Z, Aladesanmi O. Provider recommendation for colorectal cancer screening: examining the role of patients' socioeconomic status and health insurance. Cancer Epidemiol. 2009;33(3–4):207–211. doi: 10.1016/j.canep.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 21.Sarfaty M, Wender R. How to increase colorectal cancer screening rates in practice. CA Cancer J Clin. 2007;57(6):354–366. doi: 10.3322/CA.57.6.354. [DOI] [PubMed] [Google Scholar]
- 22.Schueler KM, Chu PW, Smith-Bindman R. Factors associated with mammography utilization: a systematic quantitative review of the literature. J Womens Health (Larchmt) 2008;17(9):1477–1498. doi: 10.1089/jwh.2007.0603. [DOI] [PubMed] [Google Scholar]