This rare presentation of extrapulmonary tuberculosis in a previously fit and healthy 24-year-old man emphasizes the high level of clinical suspicion needed for the early diagnosis of tuberculosis involving the bones and joints.
Introduction
Tuberculosis remains a major health issue worldwide, with a growing incidence in the UK; 8500 new cases were reported in 2006.1 However, musculoskeletal involvement is still infrequently reported in the medical literature, especially in the developed world. The lack of familiarity with tuberculosis in general, as well as specific signs and symptoms of extrapulmonary involvement may be contributory factors to a delay in diagnosis of atypical presentations. The case presented, of a 24-year-old man with a 6-month history of worsening elbow pain and range of movement, illustrates the high level of clinical suspicion needed for the early diagnosis of tuberculosis involving the bones and joints.
Case report
A 24-year-old Asian man presented to his GP with a 2-month history of worsening right elbow pain. He was normally fit and well with no significant past medical history and not on any regular medication. There was no history of trauma. General examination was normal but examination of the right elbow revealed exquisite tenderness over the lateral epicondyle. A diagnosis of lateral epicondylitis was made and he was treated with a corticosteroid injection. However, this only provided symptomatic relief for two weeks. Before a second corticosteroid injection was administered, on this occasion with slightly longer pain relief, plain radiographs of the right elbow were requested. In addition, various blood tests including full blood count (FBC), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR) and blood cultures were arranged. The radiograph showed a small joint effusion. The CRP and ESR were both elevated at 80 mg/L and 40 mm/hr, respectively, FBC was normal and blood cultures negative at 48 h. Aspiration of the joint effusion was unsuccessful.
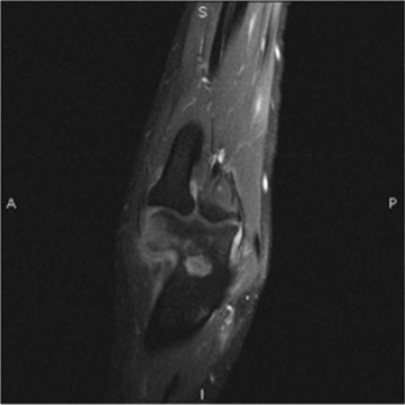
Three months after initial presentation, the patient was seen in the orthopaedic outpatient clinic as his right elbow pain had returned, together with a marked reduction in range of movement of the joint. On examination, he was still tender over the right lateral epicondyle, but there was also clinical evidence of synovial thickening on the lateral aspect of the right elbow together with a significant fixed flexion deformity of 30°. An MRI scan of the right elbow revealed a large joint effusion with marked marrow oedema and loss of cortex of the lateral epicondyle, highly suspicious of osteomyelitis (Figure 1). As a result, he underwent a right elbow synovial biopsy with debridement and washout of the joint under general anaesthetic six weeks later.
Figure 1.
MRI scan (STIR sequence) of the right elbow joint demonstrating inflammation involving the lateral condyle
The synovial biopsy results confirmed eroded bone and caseating granulomata, consistent with tuberculous osteomyelitis extending into soft tissue, with polymerase chain reaction (PCR) testing showing evidence of Mycobacterium Tuberculosis. Although Ziehl-Neelson (ZN) stains on the samples were negative, the culture grew fully sensitive Mycobacterium Tuberculosis. On further questioning, the patient denied any respiratory symptoms. Examination of the chest revealed no abnormalities. A chest radiograph was also requested, which showed no evidence of pulmonary tuberculosis. Relevant serological and haematological tests confirmed that the patient was not immunocompromised.
As a result of the culture and biopsy findings, the patient was commenced on anti-tuberculous therapy for six months with no complications. By the end of the treatment period, he regained full range of movement of his right elbow and was able to return to work and play squash regularly in his spare time with no complaints.
Discussion
Tuberculosis is classified as either pulmonary or extrapulmonary, with bone and joint tuberculosis accounting for up to 35% of extrapulmonary tuberculosis.2 The spine is involved in half of all musculoskeletal cases (Pott's disease).3 In the remainder, osteoarticular tuberculosis usually affects weight-bearing joints, with 15% being polyarticular but non-weightbearing joints affected by tuberculosis, such as the elbow, are not frequently reported in the medical literature.3
Clinically, the diagnosis of osteoarticular tuberculosis can be difficult. The most consistent symptoms include a gradual onset of joint pain associated with swelling and a decreased range of motion.4 A recent case report has highlighted a progression to septic arthritis as a result of misdiagnosis.5 Systemic symptoms are usually absent in extrapulmonary tuberculosis4 and pulmonary disease is only seen on chest radiographs of 50% of patients presenting with musculoskeletal tuberculosis.3
Changes in plain film radiography of the affected joint may include non-specific changes including joint effusion (as in this case), soft tissue swelling, joint space narrowing, subchondral erosions and osteopenia.6 However, the changes may be absent and further imaging modalities will be required to aid diagnosis.7
The role of MRI is well-documented to provide further aid to the diagnosis. Features include bone marrow changes indicating either osteomyelitis or bone marrow oedema, chondral and sub-chondral bone erosions, synovial thickening, joint effusions and loss of joint space.8 T1- and T2-weighted MRI images demonstrate marrow changes as areas of low and high signal intensity, respectively, which are enhanced with administration of intravenous gadolinium contrast.6 A recent study shows synovial thickening associated with osteoarticular tuberculosis is hypointense on T2-weighted MRI images, distinguishing this from other proliferating synovial arthropathies.9 Computed tomography (CT) can be used to evaluate the degree of bone destruction, soft tissue extension and sequestrum formation.10
However, radiological findings in osteoarticular tuberculosis are non-specific and require aspiration or synovial biopsy for definitive diagnosis. Microscopy and cultures of synovial fluid yield positive results in up to 80% of patients with osteoarticular tuberculosis.7 The remainder are diagnosed through synovial, or bone biopsies, with positive mycobacterial culture and caseating granulomata on histology.7
Summary
Diagnosing osteoarticular tuberculosis clinically can be difficult and the clinician should always have a high index of suspicion. Not considering tuberculosis as a possibility in the differential diagnosis can delay definitive treatment by up to 10 years (with the mean being 16–19 months) leading to an increase in complications and loss of joint function.2 As this case illustrates, patients with extrapulmonary tuberculosis do not always have the classic systemic symptoms associated with pulmonary tuberculosis. In addition, radiographs of the joint may look essentially normal. However, it is important to realize that these ‘normal’ findings do not rule out disease. A history of exposure to, and risk factors for, tuberculosis especially in the presence of atypical osteoarticular disease should be considered always.
DECLARATIONS
Competing interests
None declared
Funding
None
Ethical approval
Written informed consent to publication was obtained from the patient or next of kin
Guarantor
AL
Contributorship
RSS performed the data collection, wrote up the case/discussions and revised the paper; AL revised all drafts of the paper; RS wrote up the discussion
Acknowledgements
None
Reviewer
Ming-Tzer Ling
References
- 1.Health Protection Agency Tuberculosis in the UK: Annual report on tuberculosis surveillance and control in the UK 2007 London: Health Protection Agency, 2007. See http://www.hpa.org.uk/web/HPAwebFile/HPAweb_C/1208763373323 [Google Scholar]
- 2.Grosskopf I, Ben DA, Charach G, Hochman I, Pitlik S Bone and joint tuberculosis – a 10-year review. Isr J Med Sci 1994;30:278–83 [PubMed] [Google Scholar]
- 3.Kramer N, Rosenstein ED Rheumatologic Manifestations of tuberculosis. Bull Rheum Dis 1997;46:5–8 [PubMed] [Google Scholar]
- 4.Golden MP, Vikram HR Extrapulmonary tuberculosis: an overview. Am Fam Physician 2005;72:1761–8 [PubMed] [Google Scholar]
- 5.Jung SS, Lee MK, Lim SH, Kwon YM, Choi SS Elbow pain proven to be tuberculous arthritis – a case report. Korean J Anesthesiol 2010;58:211–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Backer AI, Mortelé KJ, Vanhoenacker FM, Parizel PM Imaging of extraspinal musculoskeletal tuberculosis. Eur J Radiol 2006;57:119–30 [DOI] [PubMed] [Google Scholar]
- 7.Watts HG, Lifeso RM Tuberculosis of bones and joints. J Bone Joint Surg Am 1996;78:288–98 [DOI] [PubMed] [Google Scholar]
- 8.Hong SH, Kim SM, Ahn JM, Chung HW, Shin MJ, Kang HS Tuberculous versus pyogenic arthritis: MR imaging evaluation. Radiology 2001;218:848–53 [DOI] [PubMed] [Google Scholar]
- 9.Sanghvi DA, Iyer VR, Deshmukh T, Hoskote SS MRI features of tuberculosis of the knee. Skeletal Radiol 2009;38:267–73 [DOI] [PubMed] [Google Scholar]
- 10.Stäbler A, Reiser MF Imaging of spinal infection. Radiol Clin North Am 2001;39:115–35 [DOI] [PubMed] [Google Scholar]