Abstract
We sought to describe maternal satisfaction with childbirth among women planning either cesarean or vaginal birth. We enrolled primiparous women planning cesarean birth and a comparison group planning vaginal birth. After delivery, the maternal subjective experience was assessed with a visual analogue satisfaction scale and the Salmon questionnaire, with scale scores for these aspects of the maternal experience of birth: fulfillment, distress, and difficulty. The sample included 160 women planning vaginal birth and 44 women planning cesarean. Eight weeks postpartum, women planning cesarean reported higher satisfaction ratings (p = 0.023), higher scores for fulfillment (p = 0.017), lower scores for distress (p = 0.010), and lower scores for difficulty (p <0.001). The least favorable scores were associated with unplanned cesarean (n = 48). Women planning cesarean reported a more favorable birth experience than women planning vaginal birth, due in part to low satisfaction associated with unplanned cesarean. Maternal satisfaction with childbirth may be improved by efforts to reduce unplanned cesarean, but also by support for maternal-choice cesarean.
Keywords: Cesarean, vaginal birth, maternal satisfaction
Maternal subjective experience of childbirth has been investigated as an important outcome of obstetric care. Most basically, satisfaction may be assessed as a single construct, using visual analogue scores or Likert scales.1–4 However, satisfaction with childbirth is likely a multidimensional construct and therefore may not be adequately described by a single scale. For example, it has long been recognized that childbirth is viewed by some women as a challenge and that their experience of childbirth may be dominated by a sense of fulfillment or achievement.1 Thus, childbirth might be perceived as simultaneously fulfilling and yet also difficult or painful.5,6
Several questionnaires have been developed to characterize the maternal experience in childbirth, including surveys that focus on support and control,7 satisfaction with obstetric care,3 or fear of childbirth.8 However, these scales have typically been applied to women’s experience with labor and vaginal birth. In contrast, there has been less attention to the experience of women who undergo cesarean without labor. The importance of exploring the maternal perspective on planned cesarean is highlighted by the rising incidence of cesarean delivery.9,10
In this study, we compared maternal satisfaction after birth among primiparous women planning primary cesarean with a comparison group of women planning vaginal birth. In both groups, we measured maternal satisfaction after childbirth using both a visual analog scale1,2 and a validated questionnaire.6,11 Our aim was to investigate whether planned route of delivery influences satisfaction with the birth experience. In addition, we investigated whether actual route of delivery influences maternal satisfaction. These questions have important implications in an era characterized by increasing consumer choice in obstetric practice.
MATERIALS AND METHODS
This was a National Institutes of Health–funded cohort study of maternal goals and attitudes toward childbirth. We enrolled pregnant women during the third trimester of a first pregnancy and followed them for 8 weeks postpartum. Recruitment was limited to women planning to deliver at a single hospital in suburban Baltimore. Ethics approval was obtained for this study, and informed consent was obtained from all participants.
All participants were recruited during the third trimester and before hospital admission for delivery. Exclusion criteria included conditions that may be considered clinical indications for cesarean, including known placenta previa, known fetal malpresentation, multiple gestation, prior myomectomy, and known fetal congenital anomalies. Finally, we excluded women who delivered prior to 37 weeks and those who were not able to complete a written questionnaire in English. All participants were enrolled between June 1, 2007, and March 31, 2009.
Primiparous women planning primary cesarean birth were identified by daily review of the surgical schedule in the labor and delivery unit. All women who were planning cesarean birth and who were found to be eligible were invited to participate in the study. Primiparous women planning a vaginal birth were recruited from the same obstetric practices at the time they participated in childbirth preparation classes. Each month, research team members attended randomly selected childbirth classes and approached all participants for enrollment. Those found to be ineligible (based on a screening questionnaire) were excluded.
Study participants completed three questionnaires. The first questionnaire, completed during the third trimester, established planned route of delivery, demographic characteristics, and obstetric history. The second questionnaire (“postpartum questionnaire”) was completed within 4 days of delivery and focused on maternal impressions of birth, as described below. The third and final questionnaire was completed 8 weeks after delivery and was identical to the postpartum questionnaire. Women who did not return the mailed 8-week questionnaire were contacted by telephone and a second copy was sent in the mail. The obstetric chart of each participant was reviewed to determine the actual route of birth, the duration of labor, obstetric interventions (labor induction, epidural use, episiotomy, operative birth), and complications (maternal or neonatal). Complications that may have arisen after discharge were not assessed, as we did not have access to all outpatient records.
The postpartum and 8-week questionnaires focused on maternal subjective experience of childbirth. First, each woman was asked to rate her satisfaction with her childbirth experience. This rating was presented as a visual analogue scale1,2 with range of 0 (“completely dissatisfied”) to 100 (“completely satisfied”). In addition, each participant completed the Salmon Questionnaire,11 a 20-item, validated instrument that characterizes the maternal subjective experience of birth. This questionnaire consists of a series of items with the following instruction: “For each description below, please check the value from 1 to 5 that best describes how you felt during the whole birthing process, including the first hours after birth.” The 20 descriptors included “disappointed,” “enthusiastic,” “cheated,” “happy,” and other items.11 Each of these items is rated on a 5-point Likert scale (“not at all,” “a little bit,” “moderately,” “quite a bit,” or “extremely”). Based on the participant’s responses, three domain scale scores are calculated: fulfillment, distress, and difficulty. Each score is calculated by summing the standardized scores for relevant items. Scores are not calculated if more than one item from a scale is missing. Higher scores for fulfillment signify greater fulfillment. Similarly, higher scores for distress and difficulty signify greater degrees of distress and difficulty. In prior research, this measure of internal consistency has ranged from 0.54 to 0.83 for these scales,11,12 indicating moderate to high levels of internal consistency.
For each satisfaction measure, descriptive statistics were calculated, including mean and standard deviation or median and interquartile range. Differences between scores for the postpartum and 8-week questionnaires were compared with signed rank tests.
The primary goal of the study was to compare maternal satisfaction with the birth experience for women planning vaginal versus cesarean birth. This was achieved by comparing satisfaction measures between these two groups using Wilcoxon rank-sum test. In addition, we considered whether satisfaction differed by actual route of delivery. For this analysis, we considered four groups: planned cesarean, unplanned cesarean, spontaneous vaginal birth, and operative vaginal birth. Satisfaction measures for these four types of birth were compared using analysis of variance across birth groups. In addition, multivariate regression was used to compare satisfaction measures, controlling for other potential confounders.
Finally, we considered other characteristics that might influence the subjective birth experience, such as maternal age, maternal education, length of labor, labor induction, and obstetric or neonatal complications. We defined a composite definition for any maternal or neonatal complication, including the following: 5-minute Apgar score of 7 or lower, neonatal intubation or ventilation, admission to the neonatal intensive care unit, maternal transfusion, maternal febrile morbidity, or maternal return to the operating room. We specifically investigated whether these characteristics impacted any measure of maternal satisfaction using multivariate regression. Statistical analyses were performed using Stata 10.1 (StataCorp, College Station, TX).
RESULTS
Among 402 eligible women approached for this study, 204 (51%) agreed to participate. This included 44 of 113 women planning cesarean birth and 160 of 289 planning vaginal birth. Recruited participants represented all 19 obstetric groups practicing at this hospital. All 204 enrolled participants completed the enrollment questionnaire prior to childbirth. The postpartum questionnaire was returned by 196 participants (96%). The 8-week questionnaire was completed by 36/44 (81.8%) in the cesarean group and 132/160 (82.5%) in the vaginal birth group, with no difference in follow-up between groups.
Study population is described in Table 1. Women planning cesarean were less educated and less likely to be married. Of 160 women planning vaginal birth, 95 delivered by spontaneous vaginal birth, 17 by operative vaginal birth, and 48 by unplanned cesarean. Among women planning vaginal birth, labor induction was performed in 68 cases (42.5%). Episiotomy was performed in 42/85 (49.5%) of spontaneous vaginal births (with episiotomy data missing in 10 cases) and in 16/17 (94.1%) of operative vaginal births. The median duration of the first stage of labor was 10 hours but was missing in more than one-third of labors. The median second stage of labor was 1 hour and was missing for only one woman. Of the 44 women planning cesarean, only one woman delivered vaginally.
Table 1.
Baseline Characteristics of Women in Planned Cesarean and Vaginal Birth Groups
| Characteristic | Planned Cesarean Birth (n = 44) | Planned Vaginal Birth (n = 160) | p Value |
|---|---|---|---|
| Age (y), mean (SD) | 31.9 (4.7) | 30.9 (4.5) | 0.186 |
| Primary race | 0.940 | ||
| White | 36 (81.8%) | 136 (85.0%) | |
| Black | 4 (9.0%) | 12 (7.5%) | |
| Asian | 2 (4.6%) | 6 (3.8%) | |
| Other | 0 | 6 (3.8%) | |
| Highest level of education | 0.046 | ||
| No college degree | 10 (22.7%) | 15 (9.4%) | |
| College degree | 18 (40.9%) | 67 (41.9%) | |
| Graduate degree | 16 (36.4%) | 78 (48.8%) | |
| Marital status | 0.045 | ||
| Married | 38 (86.4%) | 152 (95%) | |
| Unmarried | 6 (13.6%) | 8 (5.0%) |
Data are reported as n (%) unless otherwise noted. SD, standard deviation.
For the Salmon scale scores, Cronbach α, a measure of internal consistency for each scale score, was high for the fulfillment (0.90) and distress scales (0.83) and moderate for the difficulty scale (0.65). These findings were similar at both times. Comparing the postpartum and 8-week scores for each participant, there were no differences in visual analogue satisfaction (VAS) score or in any scale of the Salmon scale scores between time points. The 31 women who did not submit an 8-week questionnaire tended to report somewhat lower postpartum satisfaction scores, but the difference was not statistically significant.
All measures of maternal satisfaction suggested more favorable ratings among women planning cesarean compared with those planning vaginal birth (Table 2), although these differences were more pronounced 8 weeks after delivery. In the first few days after birth, the most significant differences were seen in the VAS satisfaction score, which was higher in the planned cesarean group (90.9 ± 8.5 versus 81.9 ± 19.1; p = 0.014), and in the Salmon score for difficulty, which indicated a less difficult birth experience for the cesarean group (−0.54 ± 0.89 versus 0.16 ± 0.98; p <0.001). Eight weeks later, women who had planned cesarean reported significantly higher median VAS scores (88.1 versus 81.8, p = 0.023), higher scores for fulfillment (0.32 ± 0.78 versus −0.09 ± 1.04; p = 0.017), and lower scores for distress (−0.37 ± 1.04 versus 0.10 ± 0.08; p = 0.010) and difficulty (−0.54 ± 1.05 versus 0.15 ± 0.94; p <0.001). Thus, 8 weeks after childbirth, women planning cesarean found their birth experience to be more satisfying, more fulfilling, less distressing, and less difficult than women planning vaginal birth.
Table 2.
Satisfaction Scores (Mean, Standard Deviation) by Planned Route of Delivery
| Postpartum |
8 Weeks |
|||||
|---|---|---|---|---|---|---|
| Satisfaction Measure | Planned Vaginal Birth (n = 152)* | Planned Cesarean Birth (n = 44) | p Value† | Planned Vaginal Birth (n = 132) | Planned Cesarean Birth (n = 36) | p Value† |
| VAS score | 81.9 ± 19.1 | 90.9 ± 8.5 | 0.014 | 81.8 ± 18.6 | 88.1 ± 16.3 | 0.023 |
| Fulfillment score | −0.08 ± 1.04 | 0.25 ± 0.79 | 0.058 | −0.09 ± 1.04 | 0.32 ± 0.78 | 0.017 |
| Distress score | 0.07 ± 0.99 | −0.24 ± 1.02 | 0.066 | 0.10 ± 0.08 | −0.37 ± 1.04 | 0.010 |
| Difficulty score | 0.16 ± 0.98 | −0.54 ± 0.89 | <0.001 | 0.15 ± 0.94 | −0.54 ± 1.05 | <0.001 |
The postpartum Salmon scores could not be calculated in two cases.
Signed rank test.
Data are shown separately for the postpartum and 8-week questionnaires. VAS, visual analogue satisfaction.
To investigate the impact of other measured covariates on maternal satisfaction, we considered the association between satisfaction scores and maternal characteristics (maternal age, maternal education) or obstetric characteristics (length of labor, labor induction, and obstetric or neonatal complications). Age and educational achievement were not associated with the VAS satisfaction score or with any of the Salmon scale scores. Neonatal or maternal complications were observed in only seven births (3.5%). Although complications were not significantly associated with either birth group (p = 0.62), higher distress scores were reported by women who experienced maternal or neonatal complications (p = 0.031). Among women who labored, induction of labor was associated with a marginally higher maternal distress score (p = 0.048), and a long second stage was associated with higher scores for difficulty (p = 0.005) and lower VAS scores (p = 0.033). None of the obstetric variables considered had a significant impact on fulfillment scores.
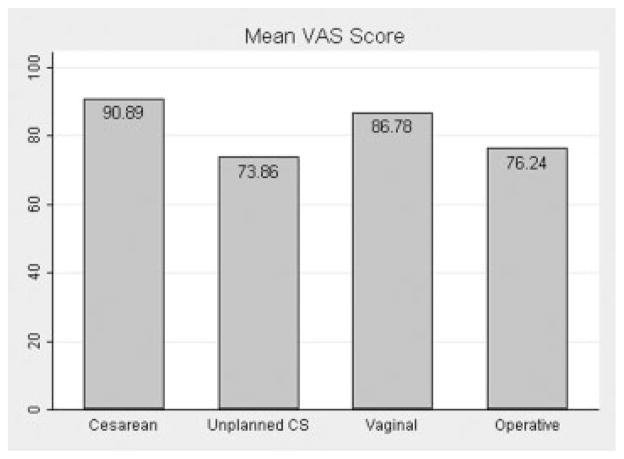
Comparing satisfaction by actual route of delivery (Fig. 1), we found that postpartum VAS scores differed significantly across birth groups (p <0.001). The highest mean VAS scores were seen among women delivered by planned cesarean (90.9 ± 8.5), with lowest scores among women who delivered by unplanned cesarean (73.9 ± 22.8) and by operative vaginal birth (76.2 ± 25.6). The VAS score reported by women who delivered by planned vaginal birth (86.8 ± 13.3) did not differ significantly from the VAS score for planned cesarean (p = 0.175). Controlling for delivery type, there was no significant association between mean VAS score and labor induction, length of labor, or morbidity. Results at 8 weeks were similar.
Figure 1.
Visual analogue satisfaction (VAS) scores, by actual route of delivery. Data are from the postpartum questionnaire. CS, cesarean delivery.
Postpartum Salmon scores by actual route of delivery are illustrated in Fig. 2. Fulfillment scores were lowest among women who delivered by unplanned cesarean (and similar between the other three birth groups). Distress was highest among women who delivered by unplanned cesarean (and similar between the other three birth groups). Scores for difficulty were significantly lower, indicating a less difficult birth experience, among women who delivered by planned cesarean as compared with the other groups. Planned cesarean was rated as less difficult than planned vaginal birth (p = 0.001). Conversely, the highest difficulty scores were reported by women who delivered by unplanned cesarean (p <0.001). Thus, women who delivered by unplanned cesarean had the lowest scores for fulfillment and the highest scores for both distress and difficulty. Controlling for delivery type, there was no significant impact of labor induction, length of labor, or morbidity on mean fulfillment score or distress score. However, duration of second stage was significantly associated with higher difficulty score (p = 0.028), controlling for these other factors. Results were similar at 8 weeks.
Figure 2.
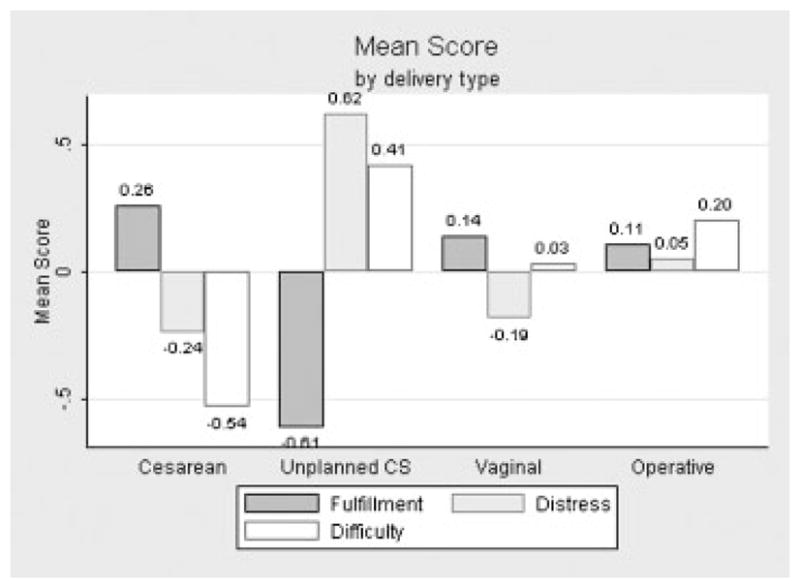
Salmon satisfaction scores, by actual route of delivery. Data are from the postpartum questionnaire. CS, cesarean delivery.
DISCUSSION
Our results suggest that maternal satisfaction is higher after planned cesarean compared with planned vaginal birth. Specifically, 8 weeks after childbirth, women who planned a cesarean delivery found their birth experience to be more fulfilling, less distressing, and less difficult than women who planned vaginal birth. This result is similar to Wiklund and colleagues,4 who found that childbirth was rated less favorably (using a single Likert scale) by women planning vaginal birth compared with those reporting cesarean. Our findings are particularly timely because obstetricians perceive an increase in maternal requests for planned cesarean birth.13 Currently, 2.1% of all U.S. deliveries are “truly elective” cesarean births,14 with a cesarean rate of 11% among primiparous women who present without a traditional indication for cesarean birth.10
Historically, vaginal birth has been viewed as more fulfilling than cesarean birth. However, one of the most interesting findings from this study was that women in the planned cesarean birth had higher scores for fulfillment than those who planned vaginal birth. Considering actual route of delivery, an important finding from this study is that women who achieved their planned route of birth experience found delivery equally fulfilling, regardless of whether they planned cesarean or vaginal birth. In contrast, in 1992, Salmon and colleagues reported that fulfillment was highest among British women who delivered vaginally and conversely was lowest among those delivering by cesarean.11 Nearly a decade later, Stadlmayr and colleagues found no association between mode of birth and fulfillment among German-speaking Swiss women.15 Differences between these studies and our results may suggest differences between populations studied or possibly changes in maternal attitudes over the past 30 years. Indeed, other researchers have found the current generation of parturients more accepting of technology and medical intervention than prior generations.16,17 We speculate that the modern, high-tech practice of obstetrics may leave women feeling more passive during labor, thereby rendering planned vaginal birth less fulfilling than it was in the past. The act of planning and achieving a planned cesarean birth might be equally fulfilling to women in that context.
At least some of the reduced satisfaction among our participants planning vaginal birth can be attributed to unplanned cesarean. The 48 of 160 women (30%) planning vaginal birth who delivered by unplanned cesarean were the least satisfied participants. These women reported lower satisfaction scores, lower fulfillment scores, and higher scores for distress and difficulty. Prior research has shown that women who deliver by unplanned cesarean are more likely to report a negative birth experience,3,15,18,19 although it is unclear whether this is related to the unanticipated route of delivery or to the events that led to unplanned cesarean. Nevertheless, the implications of this association are important. For example, low maternal satisfaction associated with unplanned cesarean might contribute to reluctance in subsequent pregnancies to consider trial of labor or vaginal birth after cesarean.19 A negative maternal birth experience has also been linked to postpartum depression.20 Therefore, women who experience unplanned cesarean might benefit from postpartum surveillance for this outcome.
We also noted that labor induction was associated with marginally higher distress scores. Although our population was not characterized by an unusually high incidence of labor induction compared with other U.S. hospitals,14 our results suggest that a lower rate of induction might potentially reduce maternal distress. Prior research has led to conflicting conclusions regarding whether labor induction negatively impacts the maternal experience of labor.11,15,19
These data were collected at a single institution; therefore our results may not be generalizable to other populations. We cannot judge whether unmeasured factors, such as the influence of the attitudes of the obstetricians, might have influenced maternal perceptions. In addition, our population had small numbers of women with certain outcomes, limiting our power for secondary analyses. This is particularly true of maternal and neonatal complications, which were fortunately low in this population. In addition, limited data regarding postpartum complications, such as mastitis or endometritis, may have reduced our ability to assess the influence of such complications on maternal satisfaction. Finally, the participation rate was 51%, and therefore we cannot rule out selection bias. However, by recruiting women before birth we believe we minimized the potential for selection bias. Also, participants in both groups were recruited from all 19 obstetric groups practicing at the hospital, suggesting that the study population is likely to be representative of women presenting for care at this institution.
A strength of this study is that the women were classified according to their planned route of delivery before childbirth. This allowed us to compare women by planned route of delivery (in addition to a comparison by actual route of delivery). An additional strength is the use of a multidimensional, validated measure of maternal perceptions of childbirth. Finally, the review of each obstetric record allowed us to investigate the impact of labor interventions and other obstetric variables on maternal satisfaction. This latter aspect of our data collection was facilitated by the conduct of this study at a single institution, with obstetric records available for review in all cases.
Our study raises an important question for obstetricians and others who care for pregnant women. Specifically, the question is how we can improve women’s experience with childbirth. A negative birth experience has been linked to an increased risk of postpartum depression,20 and therefore efforts to improve maternal satisfaction may also lead to improved clinical outcomes. Prior investigators have suggested that maternal satisfaction can be improved through enhanced maternal support during labor7 and by an improved sense of maternal control.19,21 Our results suggest that support for planned cesarean birth (including cesarean on maternal request) may also improve maternal satisfaction. However, from a public health perspective, because most women in the United States plan vaginal birth, efforts to decrease the probability of unanticipated cesarean birth are likely to have the greatest impact on maternal satisfaction with childbirth.
Acknowledgments
Supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development (R03 HD055216).
References
- 1.Morgan BM, Bulpitt CJ, Clifton P, Lewis PJ. Analgesia and satisfaction in childbirth (the Queen Charlotte’s 1000 Mother Survey) Lancet. 1982;2:808–810. doi: 10.1016/s0140-6736(82)92691-5. [DOI] [PubMed] [Google Scholar]
- 2.Capogna G, Alahuhtat S, Celleno D, et al. Maternal expectations and experiences of labour pain and analgesia: a multicentre study of nulliparous women. Int J Obstet Anesth. 1996;5:229–235. doi: 10.1016/s0959-289x(96)80042-2. [DOI] [PubMed] [Google Scholar]
- 3.Rijnders M, Baston H, Schönbeck Y, et al. Perinatal factors related to negative or positive recall of birth experience in women 3 years postpartum in the Netherlands. Birth. 2008;35:107–116. doi: 10.1111/j.1523-536X.2008.00223.x. [DOI] [PubMed] [Google Scholar]
- 4.Wiklund I, Edman G, Andolf E. Cesarean section on maternal request: reasons for the request, self-estimated health, expectations, experience of birth and signs of depression among first-time mothers. Acta Obstet Gynecol Scand. 2007;86:451–456. doi: 10.1080/00016340701217913. [DOI] [PubMed] [Google Scholar]
- 5.Christiaens W, Bracke P. Assessment of social psychological determinants of satisfaction with childbirth in a cross-national perspective. BMC Pregnancy Childbirth. 2007;7:26. doi: 10.1186/1471-2393-7-26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salmon P, Miller R, Drew NC. Women’s anticipation and experience of childbirth: the independence of fulfillment, unpleasantness and pain. Br J Med Psychol. 1990;63(Pt 3):255–259. doi: 10.1111/j.2044-8341.1990.tb01617.x. [DOI] [PubMed] [Google Scholar]
- 7.Ford E, Ayers S, Wright DB. Measurement of maternal perceptions of support and control in birth (SCIB) J Womens Health (Larchmt) 2009;18:245–252. doi: 10.1089/jwh.2008.0882. [DOI] [PubMed] [Google Scholar]
- 8.Wijma K, Wijma B, Zar M. Psychometric aspects of the W-DEQ; a new questionnaire for the measurement of fear of childbirth. J Psychosom Obstet Gynaecol. 1998;19:84–97. doi: 10.3109/01674829809048501. [DOI] [PubMed] [Google Scholar]
- 9.NCHS Dataline. Public Health Rep. 2006;121:208–210. [Google Scholar]
- 10.MacDorman MF, Menacker F, Declercq E. Cesarean birth in the United States: epidemiology, trends, and outcomes. Clin Perinatol. 2008;35:293–307. v. doi: 10.1016/j.clp.2008.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Salmon P, Drew NC. Multidimensional assessment of women’s experience of childbirth: relationship to obstetric procedure, antenatal preparation and obstetric history. J Psychosom Res. 1992;36:317–327. doi: 10.1016/0022-3999(92)90068-d. [DOI] [PubMed] [Google Scholar]
- 12.Stadlmayr W, Amsler F, Lemola S, et al. Memory of childbirth in the second year: the long-term effect of a negative birth experience and its modulation by the perceived intranatal relationship with caregivers. J Psychosom Obstet Gynaecol. 2006;27:211–224. doi: 10.1080/01674820600804276. [DOI] [PubMed] [Google Scholar]
- 13.Bettes BA, Coleman VH, Zinberg S, et al. Cesarean delivery on maternal request: obstetrician-gynecologists’ knowledge, perception, and practice patterns. Obstet Gynecol. 2007;109:57–66. doi: 10.1097/01.AOG.0000249608.11864.b6. [DOI] [PubMed] [Google Scholar]
- 14.Zhang J, Troendle J, Reddy UM, et al. Consortium on Safe Labor. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010;203:326, e1–e326, e10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Stadlmayr W, Schneider H, Amsler F, Bürgin D, Bitzer J. How do obstetric variables influence the dimensions of the birth experience as assessed by Salmon’s item list (SIL-Ger)? Eur J Obstet Gynecol Reprod Biol. 2004;115:43–50. doi: 10.1016/j.ejogrb.2003.12.015. [DOI] [PubMed] [Google Scholar]
- 16.Green JM, Baston HA. Have women become more willing to accept obstetric interventions and does this relate to mode of birth? Data from a prospective study. Birth. 2007;34:6–13. doi: 10.1111/j.1523-536X.2006.00140.x. [DOI] [PubMed] [Google Scholar]
- 17.Zwelling E. The emergence of high-tech birthing. J Obstet Gynecol Neonatal Nurs. 2008;37:85–93. doi: 10.1111/j.1552-6909.2007.00211.x. [DOI] [PubMed] [Google Scholar]
- 18.Schindl M, Birner P, Reingrabner M, Joura EA, Husslein P, Langer M. Elective cesarean section vs. spontaneous delivery: a comparative study of birth experience. Acta Obstet Gynecol Scand. 2003;82:834–840. doi: 10.1034/j.1600-0412.2003.00194.x. [DOI] [PubMed] [Google Scholar]
- 19.Waldenström U, Hildingsson I, Rubertsson C, Rådestad I. A negative birth experience: prevalence and risk factors in a national sample. Birth. 2004;31:17–27. doi: 10.1111/j.0730-7659.2004.0270.x. [DOI] [PubMed] [Google Scholar]
- 20.Ayers S, Pickering AD. Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth. 2001;28:111–118. doi: 10.1046/j.1523-536x.2001.00111.x. [DOI] [PubMed] [Google Scholar]
- 21.Goodman P, Mackey MC, Tavakoli AS. Factors related to childbirth satisfaction. J Adv Nurs. 2004;46:212–219. doi: 10.1111/j.1365-2648.2003.02981.x. [DOI] [PubMed] [Google Scholar]